Abstract
Background:
To describe and analyze the involvement of fentanyl and fentanyl analogs (FAs) in drug-related deaths in West Virginia (WV), United States.
Methods:
Retrospective analyses of all WV drug-related deaths from 2005–2017 were performed, including comparisons of demographic and toxicological characteristics among total deaths, deaths in which fentanyl/FAs were present, deaths in which they were absent, heroin-related deaths, and prescription opioid-related deaths.
Results:
Most of the 8813 drug-related deaths were overdoses, with about 11% resulting from transportation/other injuries in which drugs were contributors. Prescription opioid presence (without fentanyl) decreased by 75% from 2005–14 to 2015–17 (3,545 deaths to 859 deaths, respectively), while fentanyl involvement in the deaths increased by 122% between these periods (487 to 1082 deaths). Ten FAs were identified (427 instances) after 2015. Alprazolam and ethanol were among the top five most frequently identified substances across years. Fentanyl, heroin and cocaine replaced oxycodone, diazepam and hydrocodone in the top five beginning in 2015. Few decedents had a prescription for fentanyl after 2015, with fewer prescriptions also present for other controlled substances identified.
Conclusions:
Fentanyl, rapidly emerging FAs, and other illicit drugs in recent years pose a serious health threat even though prescription opioid-related deaths decreased over the same time period.
Keywords: fentanyl, fentanyl analog, death, illicit drug, prescription opioid
1. Introduction
Opioid-related deaths continue to increase in the United States, resulting in a substantial public health burden of about five years of life lost per 1,000 population (Gomes et al., 2018). Fentanyl and fentanyl analog (FA)-related deaths have increased dramatically with much of the fentanyl identified consisting of illicitly manufactured fentanyl (IMF) (Armenian et al., 2017; Suzuki and El-Haddad, 2017; Centers for Disease Control and Prevention [CDC], 2018). Greater difficulty obtaining prescription opioids along with ready heroin availability may have contributed to increased IMF use (Hempstead and Yildirim, 2014). Potent FAs such as carfentanil (veterinary drug) and furanyl fentanyl maintain fentanyl’s pharmacologic effects while being difficult to detect with standard toxicological testing (Armenian et al., 2017; Suzuki and El-Haddad, 2017). Since fentanyl is about 50–100 times and carfentanil approximately 10,000 times more potent than morphine, they and other illicit FAs pose serious health threats (Armenian et al., 2017; Suzuki and El-Haddad, 2017).
Fentanyl/FAs have been found in adulterated prescription drugs and in heroin, cocaine, and methamphetamine (Arens et al., 2016; Mars et al., 2017; McCall Jones et al., 2017; CDC, 2018), resulting in deaths of individuals misusing or abusing these substances (Frank and Pollack, 2017). Combining IMF/FAs with other opioids increases the overdose danger by potentiating respiratory and central nervous system depression, often resulting in rapidly occurring death(Fox et al., 2018; Slavova et al., 2017).
West Virginia (WV), which is predominantly rural, has the highest per capita drug overdose mortality in the United States (Hedegaard et al., 2017). Although heroin and synthetic opioids such as fentanyl contribute to an increasing number of drug-related deaths nationally (Rudd, 2016), studies have suggested that fentanyl overdoses might be more common in urban and suburban areas (Marshall et al., 2017). The objective of this study was to compare fentanyl and FA-related deaths to drug-related deaths not involving fentanyl/FAs in West Virginia.
2. Methods
A forensic drug database (FDD) was created in 2005 in collaboration with the West Virginia Office of the Chief Medical Examiner (WVOCME) to compile data from all WV drug-related deaths. West Virginia uses a centralized medical examiner system and the WVOCME maintains files for WV deaths. Drug-related death data are available from 2005 through 2017 (a total of 78 [7%] of 2017 deaths were not available for entry at time of this manuscript). Each FDD case includes demographic information (e.g., age, sex, race, weight, height, date of death, zip code of residence), cause and manner of death, toxicology findings (e.g., drugs identified, concentrations, postmortem interval), whether a prescription was present within the past 30 days for controlled substances, autopsy findings, and medical history. Sources used by the OCME data entry personnel to compile the FDD data included the death certificate, autopsy report, external examination, investigator reports, medical records, police reports, toxicology reports, the West Virginia Controlled Substances Monitoring Program (WV CSMP), and any other relevant information in the decedent’s file. Medical history information was obtained using a variety of sources, including county MEs, scene investigations, prescription records, autopsy reports, and medical records when available.
Deaths were defined as fentanyl or FA-related if one or more of these substances was found during postmortem toxicology testing and identified as a cause of or contributor to death in Parts I or II of the death certificate. Deaths included those in which overdose was the immediate cause of death, or a transportation-related or other injury (e.g., motor vehicle, ATV, drowning, etc.) was the immediate cause of death but drugs were believed to be significant contributors to death (e.g., fentanyl and heroin present during confirmatory toxicology in vehicle operator’s death).
Drug screening is routinely performed on all deaths investigated by the WV OCME, with confirmative toxicology tests conducted for most positive screens. Blood and/or tissue samples are screened for volatile compounds using gas chromatography with flame ionization detection and drugs of abuse using automated enzyme immunoassays. This latter test includes the following drugs/drug classes: amphetamines, barbiturates, benzodiazepines, buprenorphine, cocaine, fentanyl/fentanyl analogs, methadone, opiates (morphine, codeine, hydrocodone, hydromorphone, oxycodone, oxymorphone), and marijuana. In addition to the opiate immunoassay, a second immunoassay is specifically used to detect oxycodone and oxymorphone. Drugs or drug classes, including many therapeutic and nonprescription drugs, which screen positive undergo confirmation testing and quantitation. Fentanyl analogs were tested beginning in 2013 to coincide with national reports. Heroin was considered to have been used when the drug or its metabolite 6-monoacetylmorphine (6-MAM) was identified in any sample tested. Frequently 6-MAM is detectable in vitreous fluid or urine when no longer detectable in blood. The femoral or subclavian blood concentration ratio of morphine to codeine was also considered when heroin involvement in the death was suspected (Harruff et al., 2015). In a small number of cases, heroin was listed on the death certificate as a cause of or contributor to death on the basis of a compelling death scene investigation with toxicology reports identifying morphine (metabolite of 6-MAM) and small amounts to undetectable codeine.
Descriptive analyses were used to characterize the drug-related deaths. T-tests and Chi-square tests were used for continuous and categorical data comparisons, respectively. Co-intoxicants in fentanyl and FA-related deaths were compared between the 2005–2014 and the 2015–2017 time periods because the number of fentanyl and FA-related deaths did not increase substantially until 2015. The number of drugs with a valid prescription (defined as a prescription present within 30 days prior to death) was determined through use of the WV CSMP. Comorbidities identified through autopsy reports and other information in decedents files were defined as follows: cardiovascular (cardiomyopathy, cardiomegaly, hypertrophy, hypertensive cardiovascular disease, ischemic heart disease, atherosclerotic coronary artery disease, cardiac disease, heart failure, myocardial infarction), psychiatric other than substance abuse disorder (Alzheimer’s disease, anxiety disorder, attention deficit hyperactivity disorder, bipolar affective disorder, chronic fatigue, delusional disorder, dementia, depression, mania, mental/behavioral disorders, obsessive-compulsive disorder, panic attacks, posttraumatic stress disorder, psychosis, schizophrenia, suicide attempts/ideation, self-mutilation behavior), pulmonary (asthma, sleep apnea, chronic obstructive pulmonary disease, pneumoconiosis), hepatic (hepatitis, cirrhosis, alcoholic/other liver disease, hepatic necrosis, hepatic failure), pain (ankylosing spondylitis, migraine/headache syndromes, arthritis/polyarthritis/rheumatoid arthritis/osteoarthritis, systemic lupus, systemic sclerosis, neuropathy pain, acute pain, chronic pain, fibromyalgia, pancreatitis, systemic lupus, hip fracture), and history of substance abuse (drug, alcohol or other substance).
All analyses were performed using SAS 9.4 (SAS Institute, Cary, NC). A P value of less than 0.05 was considered statistically significant.
3. Results
A total of 8813 WV drug-related deaths from 2005 to 2017 were analyzed. Five data sources were reviewed on average per death, with toxicology, investigation and autopsy reports, and death certificates used most frequently. Of the 5924 drug-related deaths from 2005 to 2014, fentanyl was identified in 487 deaths (8.2%), most of which involved co-intoxicants with only one FA found (Table 1). Of the 2889 drug-related deaths from 2015 to 2017, 1082 (37.5%) involved fentanyl and/or FAs. The mean decedent age in fentanyl and/or FA-related deaths was significantly lower (~ seven years) compared to deaths involving prescription opioids. Overall, most decedents were male, with about 87% of deaths classified by the OCME as unintentional. Body mass index (BMI) did not differ between fentanyl/FA-related and prescription opioid deaths from 2005–2014, although BMI was slightly but statistically significantly lower compared to prescription opioid deaths during 2015 – 2017. Drug overdose was the primary cause of death across years and was significantly higher in the fentanyl/FA-related cases (99%) compared to prescription opioid or total drug deaths. A transportation-related accident or other injury (e.g., impaired/intoxicated individual hit by vehicle or falling) was the primary cause of death in approximately 11%, with one or more drugs considered contributors.
Table 1.
Changes in fentanyl, fentanyl analog, heroin, and non-fentanyl prescription opioid-related deaths in West Virginia, 2005–2017 (n = 8813).
| 2005 – 2014 | 2015 – 2017 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Totalf | 5924 (NA) | 487 (8.2) | 508 (8.6) | 3545 (59.8) | NA | 2889 (NA) | 1082 (37.5) | 290 (10.0) | 857 (29.7) | NA |
| Age (mean, SD) | 41.6 (118) | 39.7 (113) | 36.1 (10.7) | 41.3 (11.4) | 0.0039 | 42.1 (12.3) | 39.2 (112) | 38.2 (112) | 46.4 (11.4) | <0.0001 |
| Male | 3921 (66.2) | 313 (64.3) | 402 (79.1) | 2240 (63.2) | 0.6386 | 1952 (67.6) | 766 (70.8) | 202 (69.7) | 515 (60.1) | <0.0001 |
| BMI (mean, SD) | 28.9 (7.6) | 29.2 (6.9) | 28.4 (6.6) | 29.6 (7.9) | 0.2544 | 28.4 (7.8) | 28.1 (7.0) | 28.9 (7.7) | 29.3 (8.4) | 0.0010 |
| Number of drugs present | ||||||||||
| Single drug | 1320 (22.3) | 48 (9.9) | 97 (19.1) | 366 (10.3) | 664 (23.0) | 140 (12.9) | 59 (20.3) | 74 (8.6) | ||
| 2 drugs | 1539 (26.0) | 126 (25.9) | 164 (32.3) | 967 (27.3) | 833 (28.8) | 309 (28.6) | 123 (42.4) | 235 (27.4) | ||
| 3 drugs | 1354 (22.9) | 138 (28.3) | 129 (25.4) | 941 (26.6) | 0.8711 | 659 (22.8) | 302 (27.9) | 63 (21.7) | 237 (27.7) | 0.0018 |
| 4 drugs | 895 (15.1) | 97 (19.9) | 66 (13.0) | 651 (18.4) | 409 (14.2) | 202 (18.7) | 24 (8.3) | 161 (18.8) | ||
| 5 or more drugs | 816 (13.8) | 78 (16.0) | 52 (10.2) | 620 (17.5) | 324 (112) | 129 (119) | 21 (7.2) | 150 (17.5) | ||
| Number of drugs present by sex (mean, SD) | ||||||||||
| Female | 3.2 (1.7) | 3.3 (1.6) | 3.1 (1.7) | 3.5 (1.7) | 0.2543 | 3.0 (1.6) | 3.1 (1.4) | 2.6 (1.5) | 3.5 (1.7) | 0.0013 |
| Male | 2.6 (1.4) | 3.1 (1.3) | 2.6 (1.4) | 3.0 (1.4) | 0.3451 | 2.5 (1.4) | 2.9 (1.3) | 2.4 (1.1) | 3.0 (1.5) | 0.0246 |
| Total | 2.8 (1.6) | 3.2 (1.5) | 2.7 (1.4) | 3.2 (1.5) | 0.8893 | 2.7 (1.5) | 2.9 (1.3) | 2.4 (1.3) | 3.2 (1.6) | <0.0001 |
| Manner of death | ||||||||||
| Unintentional | 4982 (84.1) | 455 (93.4) | 499 (98.2) | 3141 (88.6) | 2670 (92.4) | 1068 (98.7) | 284 (97.9) | 762 (88.9) | ||
| Suicide | 517 (8.7) | 8 (1.6) | 8 (1.6) | 175 (4.9) | 0.0015 | 118 (4.1) | 8 (0.7) | 0 (0.0) | 44 (5.1) | <0.0001 |
| Other (Could not be determined, homicide) | 425 (7.2) | 24 (4.9) | 1 (0.2) | 229 (6.5) | 101 (3.5) | 6 (0.6) | 6 (2.1) | 51 (6.0) | ||
| Cause of death by category | ||||||||||
| Overdose | 5292 (89.3) | 480 (98.6) | 506 (99.6) | 3401 (95.9) | 2568 (88.9) | 1072 (99.1) | 284 (97.9) | 787 (91.8) | ||
| Transportati on (occupant, pedestrian, etc.) | 197 (3.3) | 2 (0.4) | 1 (0.2) | 40 (1.1) | 0.0165 | 223 (7.7) | 5 (0.5) | 4 (1.4) | 50 (5.8) | <0.0001 |
| Other injuries (fall, firearm, drowning, etc.) | 435 (7.3) | 5 (1.0) | 1 (0.2) | 104 (2.9) | 98 (3.4) | 5 (0.5) | 2 (0.7) | 20 (2.3) | ||
NA: not applicable.
Includes deaths involving any drug or alcohol.
2005–2014 included only 1 fentanyl analog identified in 1 death.
Any death involving heroin with no fentanyl and/or analogs.
Any death involving buprenorphine, codeine, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, diphenoxylate, propoxyphene, meperidine or tramadol; no fentanyl and/or analogs or heroin.
Comparison between fentanyl and/or analogs and prescription opioid(s).
Total drug-related deaths during time period.
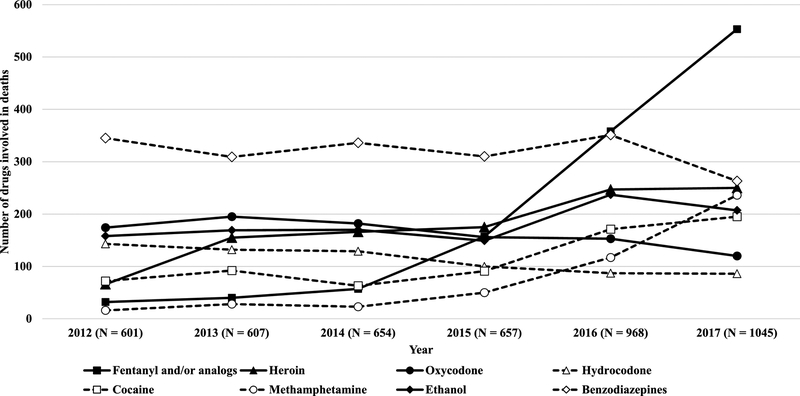
Multiple drug use was common (77.5%) among drug-related deaths (Table 1). A slight but statistically significantly greater number of co-intoxicants was identified in prescription opioid-related deaths during 2015–2017 (mean = 3.2) compared to fentanyl/FA-related deaths (mean = 2.9). Females tended to have only a slightly higher average number of co-intoxicants present than males. Involvement of fentanyl/FAs in the deaths increased dramatically during 2015–2017 (Figure 1) while prescription opioid-related deaths, still a considerable problem, decreased (Table 1). From 2012 to 2017, the largest increases in the drugs identified were: fentanyl (1325%), methamphetamine (1375%), heroin (279%), and cocaine (171%), with most increases occurring from 2015 to 2017. Prescription opioids (not including fentanyl) were present in about 30% of 2015–2017 deaths compared to almost 60% of 2005–2014 deaths. Only age, manner of death, and cause of death were statistically significantly different between fentanyl/FA-related deaths and prescription opioid deaths from 2005–2014, with all characteristics compared significantly different during 2015–2017 (Table 1).
Figure 1.
Fentanyl ± FAs and other drug involvement in unintentional drug-related deaths in West Virginia, 2012 – 2017.
Alprazolam, oxycodone, ethanol, diazepam, and hydrocodone comprised the top five identified substances in unintentional deaths from 2005–2014, while fentanyl, heroin, ethanol, alprazolam, and cocaine were the most common substances in 2015–2017 (Table 2). During 2015–2017, the most frequent co-intoxicants found together with fentanyl/FAs were heroin (36.3%), cocaine (19.9%), alprazolam (15.5%), ethanol (15.1%), and methamphetamine (14.7%). Only methamphetamine was found with similar frequency regardless of whether fentanyl/FAs were present or absent (p = 0.6430). Of the 1196 unintentional heroin-related deaths from 2005–2017, 6-MAM was identified in 1061 cases (88.7%) and morphine was present in all remaining cases (n = 135). A morphine/codeine concentration ratio in femoral or subclavian blood could be calculated in 29 (21.5%) of these latter deaths; the ratio was greater than 1 in all cases and greater than 3 in 28 of the 29 cases (96.6%). Scene investigations also helped determine the likelihood of heroin involvement in these deaths.
Table 2.
Drugs most frequently present in total, 2005–2014, and in total and fentanyl ± fentanyl analog-related unintentional deaths in West Virginia, 2015–2017 (n = 7652).
| 2005–2014 (n = 4982) | 2015–2017 (n = 2670) | |||||
|---|---|---|---|---|---|---|
| Alprazolam | 1551 (31.1) | Fentanyl | 899 (33.7) | NA | NA | NA |
| Oxycodone | 1430 (28.7) | Heroin | 672 (25.2) | 388 (36.3) | 284 (17.7) | <0.0001 |
| Ethanol | 1262 (25.3) | Ethanol | 593 (22.2) | 161 (15.1) | 432 (27.0) | <0.0001 |
| Diazepam | 1244 (25.0) | Alprazolam | 495 (18.5) | 166 (15.5) | 329 (20.5) | 0.0011 |
| Hydrocodone | 1029 (20.7) | Cocaine | 457 (17.1) | 213 (19.9) | 244 (15.2) | 0.0015 |
| Methadone | 783 (15.7) | Oxycodone | 429 (16.1) | 95 (8.9) | 334 (20.8) | <0.0001 |
| Cocaine | 730 (14.7) | Methamphetamine | 403 (15.1) | 157 (14.7) | 246 (15.4) | 0.6430 |
| Heroin | 524 (10.5) | Diazepam | 368 (13.8) | 116 (10.9) | 252 (15.7) | 0.0003 |
| Morphine | 520 (10.4) | Hydrocodone | 273 (10.2) | 60 (5.6) | 213 (13.3) | <0.0001 |
| Fentanyl | 454 (9.1) | Gabapentin | 248 (9.3) | 30 (2.8) | 218 (13.6) | <0.0001 |
| Oxymorphone | 402 (8.1) | Clonazepam | 217 (8.1) | 63 (5.9) | 154 (9.6) | 0.0006 |
| Clonazepam | 358 (7.2) | Morphine | 207 (7.8) | 114 (10.7) | 93 (5.8) | <0.0001 |
| Citalopram | 301 (6.0) | Buprenorphine | 189 (7.1) | 46 (4.3) | 143 (8.9) | <0.0001 |
| Diphenhydramine | 299 (6.0) | Oxymorphone | 145 (5.4) | 20 (1.9) | 125 (7.8) | <0.0001 |
| Tramadol | 214 (4.3) | Methadone | 95 (3.6) | 22 (2.1) | 73 (4.6) | 0.0006 |
NA: not applicable; F: fentanyl; FA: fentanyl analogs.
Total drug-related unintentional deaths during time period (excludes cases with other manners of death).
Comparison between deaths in which F and/or FA were present or absent.
Since 2015, fentanyl/FA deaths outpaced those of other prescription opioids identified in unintentional deaths. The number of fentanyl/FA-related deaths exceeded those from other substances since 2016 and rose dramatically in 2017 (Figure 1). Methamphetamine involvement has also rapidly increased from 2015 (7.6%) to 2017 (22.6%). Ethanol continues to maintain a significant presence in drug-related deaths each year (19.8% in 2017). Benzodiazepines were commonly found across years but decreased in 2017.
Ten different FAs were identified in any death from 2015 to 2017 (427 instances) (Table 3), with a single FA identified prior to 2015. The FAs identified include (in decreasing frequency): carfentanil, furanyl fentanyl, para-fluoro(iso)butyryl fentanyl, acetyl fentanyl, acryl fentanyl, cyclopropyl fentanyl, butyryl fentanyl, 3-methyl fentanyl, methoxyacetyl fentanyl, and tetrahydrofuran fentanyl. They were often identified with co-intoxicant fentanyl, heroin, benzodiazepines, cocaine or other FAs. Fentanyl was a co-intoxicant in about 31–35% of deaths involving carfentanil and furanyl fentanyl, 87.5% of deaths involving acetyl fentanyl, and 61.3% of deaths involving para-fluoro(iso)butyryl fentanyl. Among a total of 317 cases with at least one FA present, heroin and benzodiazepines were identified in 121 (38.2%) and 87 (27.4%), respectively, with other prescription opioids less commonly found (81 cases; 25.6%).
Table 3.
Fentanyl analogs idenified in drug-related deaths in West Virginia, 2015 – 2017 (n = 2889).
| Characteristic | Carfentaniln (%) | Furanyl fentanyl n (%) |
Para-fluoro(iso) butyryl fentanyl n (%) |
Acetyl fentanyl n (%) |
Acryl fentanyl n (%) |
Cyclopropyl fentanyl n (%) |
Butyryl fentanyl n (%) |
3-Methyl fentanyl n (%) |
Methox yacetyl fentanyl n (%) |
Tetrahyd rofuran fentanyl n (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Total No. of cases | 117 | 104 | 75 | 56 | 29 | 20 | 10 | 8 | 7 | 1 |
| First identified date | 2016/Aug | 2015/Jan | 2015/Jan | 2013/Jan | 2015/Jan | 2017/Jun | 2016/Dec | 2016/Sept | 2017/Sept | 2017/Apri 1 |
| Age (mean, SD) | 38.8 (11.7) | 40.1 (11.2) | 40.9 (11.3) | 37.4 (9.7) | 35.0 (9.2) | 39.6 (11.6) | 44.1 (8.6) | 33.6 (10.2) | 43.4 (14.2) | 26.0 (.) |
| Male | 75 (64.1) | 69 (66.3) | 60 (80.0) | 35 (62.5) | 20 (69.0) | 17 (85.0) | 10 (100.0) | 6 (75.0) | 5 (71.4) | 0 (.) |
| Number of drugs present (mean, SD) | 3.2 (1.6) | 3.9 (1.4) | 4.1 (1.3) | 3.8 (1.4) | 3.5 (1.3) | 3.2 (1.6) | 4.7 (1.8) | 2.4 (0.5) | 4.4 (1.9) | 4 (.) |
| Single drug | 16 (13.7) | 2 (1.9) | 1 (1.3) | 1 (1.8) | 2 (6.9) | 4 (20.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| 2 drugs | 27 (23.1) | 14 (13.5) | 9 (12.0) | 8 (14.3) | 5 (17.2) | 3 (15.0) | 1 (10.0) | 5 (62.5) | 1 (14.3) | 0 (0.0) |
| 3 drugs | 28 (23.9) | 26 (25.0) | 12 (16.0) | 17 (30.4) | 9 (31.0 | 5 (25.0) | 2 (20.0) | (37.5) | 1 (14.3) | 0 (0.0) |
| 4 drugs | 24 (20.5) | 32 (30.8) | 29 (38.7) | 17 (30.4) | 7 (24.1) | 4 (20.0) | 2 (20.0) | 0 (0.0) | 2 (28.6) | 1 (100.0) |
| 5 or more drugs | 22 (18.8) | 30 (28.8) | 24 (32.0) | 13 (23.2) | 6 (20.7) | 4 (20.0) | 5 (50.0) | 0 (0.0) | 3 (42.9) | 0 (0.0) |
| Cases with concurrent | ||||||||||
| Fentanyl | 41 (35.0) | 32 (30.8) | 46 (61.3) | 49 (87.5) | 14 (48.3) | 9 (45.0) | 6 (60.0) | 1 (12.5) | 6 (85.7) | 0 (0.0) |
| Other fentanyl analog(s) | 28 (23.9) | 31(29.8) | 41 (54.7) | 1 (1.8) | 15 (51.7) | 5 (25.0) | 5 (50.0) | 2 (25.0) | 3 (42.9) | 1 (100.0) |
| Other prescriptio n opioid(s)a | 28 (23.9) | 25 (24.0) | 14 (18.7) | 20 (35.7) | 3 (10.3) | 2 (10.0) | 3 (30.0) | 2 (25.0) | 2 (28.6) | 1 (100.0) |
| Heroin | 26 (22.2) | 48 (46.2) | 42 (56.0) | 29 (51.8) | 17 (58.6) | 6 (30.0) | 5 (50.0) | 1 (12.5) | 2 (28.6) | 1 (100.0) |
| Benzodiaze pine(s)b | 34 (29.1) | 39 (37.5) | 19 (25.3) | 15 (26.8) | 3 (10.3) | 4 (20.0) | 3 (30.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) |
| Ethanol | 13 (11.1) | 18 (17.3) | 9 (12.0) | 10 (17.9) | 2 (6.9) | 0 (0.0) | 2 (20.0) | 0 (0.0) | 1 (14.3) | 0 (0.0) |
| Methamph etamine | 28 (23.9) | 13 (12.5) | 5 (6.7) | 4 (7.1) | 6 (20.7) | 6 (30.0) | 2 (20.0) | 1 (12.5) | 4 (57.1) | 0 (0.0) |
| Cocaine | 19 (16.2) | 20 (19.2) | 22 (29.3) | 12 (21.4) | 3 (10.3) | 6 (30.0) | 3 (30.0) | 4 (50.0) | 2 (28.6) | 0 (0.0) |
| Most frequently occuring analog cointoxicant | Furanyl fentanyl, 17 (14.5) | Para-fluoro(iso)buty ryl/butyryl fentanyl, 32 (30.8) | Furanyl fentanyl, 32 (42.7) | Furanyl fentanyl, acryl fentanyl, para-fluoro(iso) butyryl fentanyl, 1 (1.8) | Furanyl fentanyl, 13 (44.8) | Para-fluoro(iso) butyryl fentanyl, Butyryl fentanyl, 2 (10.0) | Para-fluoro(iso) butyryl fentanyl, 5 (50.0) | Carfentanil, Furanyl fentanyl, 1 (12.5) | Carfentanil, 2 (28.6) | Carfentanil, 1 (100.0) |
Any death involving buprenorphine, codeine, hydrocodone, hydromorphone, methadone, morphine, oxycodone, oxymorphone, diphenoxylate, propoxyphene, meperidine or tramadol; no fentanyl or heroin
Benzodiazepines include alprazolam, clonazepam, chlordiazepoxide, diazepam, lorazepam, oxazepam, temazepam.
The percentage of controlled substances for which decedents had a prescription decreased overall from 2005–2014 to 2015–2017, but the percentage steadily increased by age, from 9.8%of decedents aged 18–24 years to 42% of those 65 years and older. Fewer decedents had a prescription for hydrocodone (51.4% vs. 38.8%), oxycodone (39.3% vs. 37.3%), morphine (19.9% vs. 9.7%), alprazolam (44.5% vs. 34.5%), and diazepam (28.9% vs. 22.6%) during 2015–2017 compared to the earlier period. Very few decedents had a prescription for methamphetamine. For deaths involving methadone, commonly used in medication-assisted treatment for opioid abuse, a prescription was found with slightly higher frequency during 2015–2017 compared to earlier years (31.2% to 24.2%, respectively), although the number of methadone-related deaths was much lower recently. Most notable was the recent decline in the percentage of decedents who had a prescription for identified fentanyl (23.9% to 1.7%).
Medical records were accessed for 25.6% (2259/8813) of all deaths (Table 4). Of these, a history of substance abuse (drugs and/or alcohol) was significantly higher in unintentional deaths involving fentanyl/FAs compared to deaths in which they were absent (87.6% vs. 67.8%), while co-morbid cardiovascular (41.1% vs. 50.3%) and pulmonary diseases (17.0% vs. 25.5%) were significantly less common in fentanyl/FA-related deaths. There were no significant differences in co-morbid psychiatric, pain, or hepatic conditions between deaths with or without fentanyl/FAs, with percentages in all groups relatively low (less than 20%).
Table 4.
Comorbid medical conditions in unintentional drug-related deaths (n = 7652) - fentanyl + FAs vs. non-fentanyl + FAs in West Virginia, 2005–2017.
| Medical Conditions | Total Deaths n (%) |
Fentanyl and/or Analogs Present n (%) |
Fentanyl and/or Analogs Absent n (%) |
p- valueb |
|---|---|---|---|---|
| Totala | 6837 | 1420 | 5417 | - |
| Cardiovascular | 3306 (48.4) | 584 (41.1) | 2722 (50.3) | 0.0001 |
| Psychiatric | 1342 (19.6) | 299 (21.1) | 1043 (19.3) | 0.128 |
| Pulmonary | 1622 (23.7) | 241 (17.0) | 1381 (25.5) | 0.0001 |
| Hepatic | 660 (9.7) | 142 (10.0) | 518 (9.6) | 0.6192 |
| Pain | 738 (10.8) | 154 (10.9) | 584 (10.8) | 0.9447 |
| History of Abuse | 4915 (71.9) | 1244 (87.6) | 3671 (67.8) | <0.0001 |
Total cases with available medical history data; percentages calculated using total number as denominator.
Comparsion between fentanyl and/or analogs present vs. fentanyl and/or analogs absent.
4. Discussion
Drug-related deaths continue to rise in the United States (Armenian et al., 2017; Frank and Pollack, 2017; O’Donnell et al., 2017; Suzuki and El-Haddad, 2017; CDC, 2018). Fentanyl-related WV deaths have continued unabated since 2015, with a steep recent increase. Drug involvement in the deaths has also changed, from predominantly prescription opioids to illicit drugs, generally with co-intoxicants. This recent shift from predominantly prescription opioids to illicit drugs suggests that programs to reduce prescription opioid deaths, e.g., prescription drug monitoring programs (PDMPs), are decreasing fatal intoxications from such opioids. However, when prescription opioids are less readily available, drug users often switch to cheaper, illicit substitutes (Alexander et al., 2016; Fink et al., 2018; Nam et al., 2017; Pergolizzi et al., 2018; Seth et al., 2018; Slavova et al., 2017). Our finding of fewer decedents with prescriptions for identified controlled substances is consistent with these reports. Although a recent review found that PDMPs appeared to reduce overdose deaths, albeit based on low-strength evidence (Compton and Wargo, 2018), they have continued to increase in WV. This increase might also be explained in part by geographical isolation, poverty, limited medical resources, heavy economic burdens, and social obstacles that could exacerbate the fentanyl problem in rural areas (Jozaghi and Marsh, 2017).
Similar to other reports (Hayashi et al., 2018), the mean decedent age was significantly younger in fentanyl/FA-related deaths compared to other drugs or those involving prescription opioids. Compared to non-fentanyl prescription opioids, fentanyl/FA-related deaths in 2015–2017 had a significantly greater proportion of males, lower BMI, and were more likely to be unintentional in nature. Thus, it is important that efforts to reduce fentanyl abuse encompass the younger male population.
Characterizing the co-intoxicants involved in fentanyl-related deaths is important. Fentanyl or a FA was present as a single drug in a minority of deaths (12.9%), although to a significantly greater extent than single drug prescription opioids (9% of deaths). Co-intoxicants identified prior to 2015 were predominantly benzodiazepines and prescription opioids; more recently, they were likely to be illicit although benzodiazepine involvement continues to be high. Heroin, cocaine, and methamphetamine were present in 36.3%, 19.9%, and 14.7% of all unintentional fentanyl/FA-related deaths during 2015–2017, respectively, consistent with reports describing regular heroin and cocaine use as risks for fentanyl overdose (Baldwin et al., 2018; Hayashi et al., 2018; Mars et al., 2017; McCall Jones, et al., 2017; Rubin, 2017). Crystal methamphetamine use has been significantly associated with fentanyl identification (Amlani et al., 2015; Baldwin et al., 2018; Hayashi et al., 2018), with fentanyl/FAs found to an increasing extent in confiscated methamphetamine (CDC, 2018). Methamphetamine was present to a similar extent in WV fentanyl/FAs present or absent deaths.
Fentanyl-related deaths with multiple co-intoxicants might partly result from the use of fentanyl-laced or counterfeit heroin, cocaine, opioids and benzodiazepines (CDC, 2016a; Marinetti and Ehlers, 2014; Unick and Ciccarone, 2017; CDC, 2018). This could help explain the rapid rise in fentanyl-related deaths in WV, a state with traditionally high prescription opioid deaths. A prescription was present in a very small percentage of our recent fentanyl deaths, indicating predominantly IMF use or diversion.
Heroin was identified in over a third of fentanyl/FA-related deaths during 2015–2017 but can be difficult to detect due to its very rapid metabolism to 6-monoacetylmorphine, which has a slightly longer but still relatively short half-life (Harruff et al., 2015). Thus, the morphine/codeine concentration ratio can assist in identifying heroin involvement in deaths. Codeine in small concentrations is often present in illicit heroin batches. A morphine/codeine ratio greater than three likely indicates that heroin use was the source of codeine present, while a ratio smaller than one typically indicates codeine ingestion (Harruff et al., 2015). In cases where 6-MAM was present in our study, all had a ratio greater than one, with most having a morphine/codeine ratio above three. Similar results were found in suspected heroin deaths in which 6-MAM was absent and a morphine/codeine ratio could be determined. Thus, only a relatively small number of 6-MAM-negative deaths might be falsely attributed to heroin, although some cases with heroin involvement could be missed.
The rapid increase in FA deaths represents an unprecedented public health threat (CDC, 2018), with prescription opioids and benzodiazepines still contributing to a significant number of deaths. Although relatively new to WV, FAs were identified for several years in other areas of the country (Hibbs et al., 1991). A total of ten different FAs were identified in WV deaths during 2015–2017, usually with co-intoxicant fentanyl, heroin, benzodiazepines, cocaine or other FAs. Carfentanil and furanyl fentanyl were present most often, but new FAs continue to be identified.
Additional trends from the more recent drug-related deaths deserve special mention. Recent increases in methamphetamine involvement is of particular concern, particularly with the prevalence of cardiovascular disease in WV (CDC, 2016b). Heroin and cocaine were infrequently involved in WV deaths in past years but now constitute serious health threats. Alcohol should not be overlooked since it has consistently been among the top substances identified in WV drug-related deaths, present in almost a quarter of such deaths.
About 89% of WV drug deaths represented overdoses. Deaths were also included in which a transportation-related accident or other injury was the immediate cause of death, but drugs and/or alcohol were contributors. While not classified as overdoses, these deaths might have been avoided if the person was unimpaired. A total of 953 deaths between 2005 and 2017 fell into transportation or other injury categories (e.g., falling, drowning, choking/suffocating, being hit by trains or cars, ATV or other vehicular accidents) influenced by the presence of one or more substances. Of 321 such deaths from 2015–2017, fentanyl was found in 10 (3%) and prescription opioids were contributors in 70 (22%) (Table 1). By preventing overdose deaths, substance-related injury deaths might also be reduced. Further studies should explore trauma-related deaths directly or indirectly attributed to impairment.
Most study decedents had a history of drug and/or alcohol abuse, a known risk factor for opioid-related mortality (Webster, 2017). This history was significantly more common in fentanyl/FA associated deaths, consistent with the illicit nature of FAs and the very low percentage of prescriptions present for fentanyl in the recent deaths. However, significantly lower rates of co-morbid cardiovascular and pulmonary conditions, also reported as risk factors for opioid-related death (Webster, 2017), were found in WV decedents with fentanyl/FAs present. Existing diagnoses of psychiatric conditions and pain, reported to be risk factors for opioid mortality (Webster, 2017), were found in about 20% and 11%, respectively, of our decedents’ files. Since comprehensive medical histories were not available in most cases, these figures are likely incomplete. Further studies involving direct linkages with medical records are needed to examine the association of underlying medical conditions with drug mortality risk.
Most drug-related death reports have focused on overdoses based on ICD-10 codes (O’Donnell et al., 2017; Unick and Ciccarone, 2017). A particular strength of this study is the use of multiple data sources, including death certificates, autopsy reports, CSMP information, and toxicology analyses that allow individual opioids and drug combinations involved to be identified. A centralized medical examiner system in WV enables fairly complete decedent data to be compiled.
This study also has potential limitations. Accurately determining intent for manner of death (i.e., unintentional vs. suicide) is difficult postmortem. The WV OCME certifies deaths with the understanding that the potential for under-reporting suicides is substantial, and the number of suicides related to drug overdose deaths are likely underestimated (Rockett et al., 2018). Relevant data might be missing or incorrectly entered in the case file or FDD. However, data were checked for inconsistencies or missing values, with follow-up to the extent possible. Heroin can be difficult to identify in decedents due to rapid metabolism, so heroin in some cases might be missed. When fentanyl was found as a co-intoxicant, it cannot be determined whether the decedent used fentanyl in addition to heroin/other drugs or if heroin/other drugs were taken that unknowingly contained fentanyl. Due to the frequency in which new FAs are appearing in the deaths, it is possible that as yet unknown analogs were not detected. A small number of drug-related deaths from 2017 were not yet entered into the FDD at the time of this study. However, preliminary review of these cases found that 31 (39.7%) had fentanyl present. Finally, West Virginia is a rural state with a high per capita drug overdose death rate. Although these findings might not be representative of other geographic areas, they are consistent with reports of increasing FA deaths in several states (CDC, 2018).
The substances involved in drug-related deaths must be closely monitored to ensure that appropriate harm reduction strategies are used. The frequency at which new FAs and IMF are appearing is particularly concerning since controlled substances monitoring programs cannot track these substances. Routine toxicological detection of FAs is difficult, and clandestine laboratories can easily modify fentanyl and its derivatives. Expanded access to addiction treatment and ready availability of naloxone to treat acute opioid overdoses are needed (Frank and Pollack, 2017; Klebacher et al., 2017; Samet and Kertesz, 2018; Thomson et al., 2017; CDC, 2018). Multifaceted fentanyl outbreak identification, prevention, harm reduction, and expanded treatment strategies that consider social, economic, and other contributing factors are needed to address the opioid and illicit drug crisis (Dasgupta et al., 2018; CDC, 2018). Education and training of health providers, public health professionals, and health professions students are necessary to implement such strategies (Frank and Pollack, 2017; Samet and Kertesz, 2018; Thomson et al., 2017). Public health, law enforcement, and other government agencies must work in collaboration to halt the production and supply of IMF, FAs and other illicit drugs.
5. Conclusions
Fentanyl involvement increased substantially over time in WV drug-related deaths from 2005 to 2017, with ten different FAs identified since 2015. Prescription opioid presence decreased by about half with fentanyl, heroin, ethanol, alprazolam and cocaine constituting the top five identified drugs in these deaths since 2015. Alprazolam and ethanol were consistently among the top five drugs identified since 2005, with methamphetamine involvement increasing. In contrast, the presence of a prescription for most controlled substances identified in the deaths has been decreasing. Deaths involving fentanyl and newly identified FAs could represent the “tip of the iceberg” since fentanyl derivatives are often not readily detected.
Highlights.
89% of drug deaths were overdoses; 11% had injuries as immediate cause of death
Prescription opioid involvement in deaths decreased by half in 2015–2017
Fentanyl, heroin and cocaine now in top five drugs involved in 2015–2017 WV deaths
Ten different fentanyl analogs identified (total 427 times) from 2015–2017
Increasing recent involvement of methamphetamine in deaths is also of concern
Role of the Funding Sources
This work was supported in part by the following awards: National Institute of General Medical Sciences (2U54GM104942-02.), National Institute of Drug Abuse (1R21DA040187 and 1UG3DA044825), and Centers for Disease Control and Prevention (R49CE002109). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Centers for Disease Control and Prevention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest
No conflict declared.
References
- Alexander RT, Hedrick CW, Alexander SD, Jufer-Phipps R, Fowler DR, 2016. Epidemic fentanyl deaths in Maryland: A public health intervention involving Geographic Information Systems and collaboration with the Drug Enforcement Administration. Acad. Forensic Pathol 6, 301–314. 10.23907/2016.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amlani A, McKee G, Khamis N, Raghukumar G, Tsang E, Buxton JA, 2015. Why the FUSS (Fentanyl Urine Screen Study)? A cross-sectional survey to characterize an emerging threat to people who use drugs in British Columbia, Canada. Harm Reduct. J 12, 54 10.1186/s12954-015-0088-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arens AM, van Wijk XM, Vo KT, Lynch KL, Wu AH, Smollin CG, 2016. Adverse effects from counterfeit alprazolam tablets. JAMA Intern. Med 176, 1554–1555. 10.1001/jamainternmed.2016.4306. [DOI] [PubMed] [Google Scholar]
- Armenian P, Olson A, Anaya A, Kurtz A, Ruegner R, Gerona RR, 2017. Fentanyl and a novel synthetic opioid U-47700 masquerading as street “Norco” in central California: A case report. Ann. Emerg. Med 69, 87–90. 10.1016/j.annemergmed.2016.06.014. [DOI] [PubMed] [Google Scholar]
- Baldwin N, Gray R, Goel A, Wood E, Buxton JA, Rieb LM, 2018. Fentanyl and heroin contained in seized illicit drugs and overdose-related deaths in British Columbia, Canada: An observational analysis. Drug Alcohol Depend. 185, 322–327. 10.1016/j.drugalcdep.2017.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC), 2016a. Influx of fentanyl-laced counterfeit pills and toxic fentanyl-related compounds further increases risk of fentanyl-related overdose and fatalities. Accessed 6.6.18 https://emergency.cdc.gov/han/han00395.asp.
- Centers for Disease Control and Prevention (CDC), 2016b. Stats of the state of West Virginia. accessed 6.1.18 https://www.cdc.gov/nchs/pressroom/states/westvirginia/westvirginia.htm.
- Centers for Disease Control and Prevention (CDC), 2018. Health Alert Network (HAN) 00413. Rising numbers of deaths involving fentanyl and fentanyl analogs, including carfentanil, and increased usage and mixing with non-opioids. Accessed 14 July 2018 https://emergency.cdc.gov/han/han00413.asp.
- Compton WM, Wargo EM, 2018. Prescription drug monitoring programs: Promising practices in need of refinement. Ann. Intern. Med 168, 826–827. 10.7326/M18-0883. [DOI] [PubMed] [Google Scholar]
- Dasgupta N, Beletsky L, Ciccarone D, 2018. Opioid crisis: No easy fix to its social and economic determinants. Am. J. Public Health 108, 182–186. 10.2105/AJPH.2017.304187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fink DS, Schleimer JP, Sarvet A, Grover KK, Delcher C, Castillo-Carniglia A, Kim JH, Rivera-Aguirre AE, Henry SG, Martins SS, Cerdá M, 2018. Association between prescription drug monitoring programs and nonfatal and fatal drug overdoses. Ann. Intern. Med 168, 783–790. 10.7326/M17-3074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fox LM, Hoffman RS, Vlahov D, Manini AF, 2018. Risk factors for severe respiratory depression from prescription opioid overdose. Addiction 113, 59–66. 10.1111/add.13925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank RG, Pollack HA, 2017. Addressing the fentanyl threat to public health. N. Engl. J. Med 376, 605–607. 10.1056/NEJMp1615145. [DOI] [PubMed] [Google Scholar]
- Gomes T, Tadrous M, Mamdani MM, Paterson JM, Juurlink DN, 2018. The burden of opioid-related mortality in the United States. JAMA Netw. Open 1, e180217–e180217. 10.1001/jamanetworkopen.2018.0217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harruff RC, Couper FJ, Banta-Green CJ, 2015. Tracking the opioid drug overdose epidemic in King County, Washington using an improved methodology for certifying heroin related deaths. Acad. Forensic Pathol. 5, 499–506. 10.23907/2015.055. [DOI] [Google Scholar]
- Hayashi K, Milloy MJ, Lysyshyn M, DeBeck K, Nosova E, Wood E, Kerr T, 2018. Substance use patterns associated with recent exposure to fentanyl among people who inject drugs in Vancouver, Canada: A cross-sectional urine toxicology screening study. Drug Alcohol Depend. 183, 1–6. 10.1016/j.drugalcdep.2017.10.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hedegaard H, Warner M, Minino AM, 2017. Drug overdose deaths in the United States, 1999–2016. NCHS Data Brief 294, 1–8. [PubMed] [Google Scholar]
- Hempstead K, Yildirim EO, 2014. Supply-side response to declining heroin purity: Fentanyl overdose episode in New Jersey. Health Econ. 23, 688–705. 10.1002/hec.2937. [DOI] [PubMed] [Google Scholar]
- Hibbs J, Perper J, Winek CL, 1991. An outbreak of designer drug-related deaths in Pennsylvania. JAMA 265, 1011–1013. 10.1001/jama.1991.03460080081037. [DOI] [PubMed] [Google Scholar]
- Jozaghi E, Marsh S, 2017. Missing the trends in the fentanyl overdose crisis: The need for immediate intervention in small and rural communities. Can. J. Public Health 108, 457, 10.17269/cjph.108.6480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klebacher R, Harris MI, Ariyaprakai N, Tagore A, Robbins V, Dudley LS, Bauter R, Koneru S, Hill RD, Wasserman E, Shanes A, Merlin MA, 2017. Incidence of naloxone redosing in the age of the new opioid epidemic. Prehosp. Emerg. Care 21, 682–687. 10.1080/10903127.2017.1335818. [DOI] [PubMed] [Google Scholar]
- Marinetti LJ, Ehlers BJ, 2014. A series of forensic toxicology and drug seizure cases involving illicit fentanyl alone and in combination with heroin, cocaine or heroin and cocaine. J. Anal. Toxicol 38, 592–598. 10.1093/jat/bku086. [DOI] [PubMed] [Google Scholar]
- Mars SG, Ondocsin J, Ciccarone D, 2017. Sold as heroin: Perceptions and use of an evolving drug in Baltimore, MD. J. Psychoactive Drugs 50, 1–10. 10.1080/02791072.2017.1394508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marshall BDL, Krieger MS, Yedinak JL, Ogera P, Banerjee P, Alexander-Scott NE, Rich JD, Green TC, 2017. Epidemiology of fentanyl-involved drug overdose deaths: A geospatial retrospective study in Rhode Island, USA. Int. J. Drug Policy 46, 130–135. 10.1016/j.drugpo.2017.05.029. [DOI] [PubMed] [Google Scholar]
- McCall Jones C, Baldwin GT, Compton WM, 2017. Recent increases in cocaine-related overdose deaths and the role of opioids. Am. J. Public Health 107, 430–432. 10.2105/AJPH.2016.303627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nam YH, Shea DG, Shi Y, Moran JR, 2017. State prescription drug monitoring programs and fatal drug overdoses. Am. J. Manag. Care 23, 297–303. [PubMed] [Google Scholar]
- O’Donnell JK, Gladden RM, Seth P, 2017. Trends in deaths involving heroin and synthetic opioids excluding methadone, and law enforcement drug product reports, by census region - United States, 2006–2015. MMWR Morb. Mortal. Wkly. Rep 66, 897–903, 10.15585/mmwr.mm6634a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pergolizzi JV Jr., LeQuang JA, Taylor R Jr., Raffa RB, 2018. Going beyond prescription pain relievers to understand the opioid epidemic: The role of illicit fentanyl, new psychoactive substances, and street heroin. Postgrad. Med 130, 1–8. 10.1080/00325481.2018.1407618. [DOI] [PubMed] [Google Scholar]
- Rockett IR, Caine ED, Connery HS, D’Onofrio G, Gunnell DJ, Miller TR, Nolte KB, Kaplan MS, Kapusta ND, Lilly CL, Nelson LS, Putnam SL, Stack S, Värnik P, Webster LR, Jia H, 2018. Discerning suicide in drug intoxication deaths: Paucity and primacy of suicide notes and psychiatric history. PLoS One 13, e0190200 10.1371/journal.pone.0190200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R, 2017. Illicit fentanyl driving opioid overdose deaths. JAMA 318, 2174 10.1001/jama.2017.18602. [DOI] [PubMed] [Google Scholar]
- Rudd RA, 2016. Increases in drug and opioid-involved overdose deaths—United States, 2010–2015. MMWR Morb. Mortal. Wkly. Rep 65, 1445–1452. 10.15585/mmwr.mm655051e1. [DOI] [PubMed] [Google Scholar]
- Samet JH, Kertesz SG, 2018. Suggested paths to fixing the opioid crisis: Directions and misdirections. JAMA Netw. Open 1, e180218–e180218. 10.1001/jamanetworkopen.2018.0218. [DOI] [PubMed] [Google Scholar]
- Seth P, Rudd RA, Noonan RK, Haegerich TM, 2018. Quantifying the epidemic of prescription opioid overdose deaths. Am. J. Public Health 108, 500–502. 10.2105/AJPH.2017.304265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavova S, Costich JF, Bunn TL, Luu H, Singleton M, Hargrove SL, Triplett JS, Quesinberry D, Ralston W, Ingram V, 2017. Heroin and fentanyl overdoses in Kentucky: Epidemiology and surveillance. Int. J. Drug Policy 46, 120–129. 10.1016/j.drugpo.2017.05.051. [DOI] [PubMed] [Google Scholar]
- Suzuki J, El-Haddad S, 2017. A review: Fentanyl and non-pharmaceutical fentanyls. Drug Alcohol Depend. 171, 107–116. 10.1016/j.drugalcdep.2016.11.033. [DOI] [PubMed] [Google Scholar]
- Thomson E, Lampkin H, Maynard R, Karamouzian M, Jozaghi E, 2017. The lessons learned from the fentanyl overdose crises in British Columbia, Canada. Addiction 112, 2068–2070. 10.1111/add.13961. [DOI] [PubMed] [Google Scholar]
- Unick GJ, Ciccarone D, 2017. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int. J. Drug Policy 46, 112–119. 10.1016/j.drugpo.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster LR, 2017. Risk factors for opioid-use disorder and overdose. Anesth. Analg 125, 1741–1748. 10.1213/ANE.0000000000002496. [DOI] [PubMed] [Google Scholar]