Abstract
We reviewed survey data deposited in the Global Neglected Tropical Diseases database and many other articles on the prevalence and distribution of Schistosoma haematobium in Nigeria. Schistosoma haematobium surveys conducted over the period of 50 years under review using different diagnostic tools revealed that Ogun State has the highest prevalence, followed by Ekiti state, while the lowest prevalence was recorded in Adamawa. No incidence of Schistosoma haematobium was recorded for states such as Akwa Ibom, Bayelsa, Nasarawa, Jigawa and Gombe. In terms of endemicity, this review has shown that Nigeria is divided into four zones: hyperendemic, moderately endemic, low endemic, and no endemic zones. A survey of 47 (15%) of the 323 dams in Nigeria revealed that 45 out of the 47 dams are located in the hyperendemic zone, while the remaining two are located in the moderately endemic zone. Twenty (43%) of the total surveyed dams harboured Bulinus globosus and/or Biomphalaria pfeifferi, the local intermediate hosts of schistosomes, and 18 of these are located in the hyperendemic zone, while the other two are in the moderately endemic zone. We conclude that there is an urgent need to carry out a nationwide survey to help in planning, coordinating, and evaluating schistosomiasis control activities.
Keywords: Schistosomiasis, Schistosoma haematobium, Epidemiology, Snails, Morbidity, Praziquantel
Abstract
Nous avons examiné les données recueillies dans la base de données mondiale sur les maladies tropicales négligées et de nombreux autres articles sur la prévalence et la répartition de Schistosoma haematobium au Nigéria. Les enquêtes sur S. haematobium menées au cours des 50 dernières années à l’aide de différents outils de diagnostic ont révélé que l’État d’Ogun avait la prévalence la plus élevée, suivi de l’état d’Ekiti, la plus faible prévalence ayant été enregistrée à Adamawa. Aucune incidence de S. haematobium n’a été enregistrée dans des États comme Akwa Ibom, Bayelsa, Nasarawa, Jigawa et Gombe. En termes d’endémicité, cette revue a montré que le Nigéria est divisé en quatre zones: hyper endémique, modérée, basse et sans endémie. L’enquête menée auprès de 47 (15 %) des 323 barrages au Nigeria a révélé que 45 des 47 barrages sont situés dans la zone d’hyperendémie, tandis que les 2 restants sont situés dans une zone d’endémie modérée. Parmi les barrages étudiés, 20 (43 %) hébergeaient Bulinus globosus et/ou Biomphalaria pfeifferi, les hôtes intermédiaires locaux des schistosomes, et 18 d’entre eux sont situés dans la zone d’hyperendémie tandis que les 2 autres se trouvent dans la zone d’endémie modérée. Nous concluons qu’il est urgent de mener une enquête à l’échelle nationale pour faciliter la planification, la coordination et l’évaluation des activités de lutte contre la schistosomiase.
Introduction
Urinary schistosomiasis caused by Schistosoma haematobium is endemic in the sub-Saharan region of Africa, including in Nigeria [9, 10]. About 200 million people in some 74 countries are infected worldwide and at least 600 million are at risk of infection [27]. An estimated 120 million suffer severe consequences of the infection with an estimated annual mortality rate of about 20,000 worldwide [28]. An estimated 30 million Nigerians need to be treated annually for the disease [2]. In most endemic areas, the highest intensities of infection are found in children between 5 and 15 years of age [28]. In sub-Saharan Africa alone, it is estimated that 70 million individuals experience haematuria, 32 million difficulty in urinating (dysuria), 18 million bladder-wall pathology, and 10 million major hydronephrosis from infections caused by S. haematobium annually. The mortality rate due to non-functioning kidneys (from S. haematobium) and haematemesis has been estimated to be 150,000 per year [25]. The above figures show that urinary schistosomiasis is an important public health problem in sub-Saharan Africa, second only to malaria in morbidity [26]. Urinary schistosomiasis has been reported to increase the risk of HIV infection among women due to the fact that this parasite causes genital lesions and sandy patches [13]. Up to 75% of women infected with urinary schistosomiasis develop irreversible lesions in their vulva, vagina, cervix and uterus, creating a lasting entry point for HIV [20]. The planorbid snail Bulinus spp. is the intermediate host in the transmission of vesical schistosomiasis. The distribution of the disease is focal and its effects are more common in rural areas in the tropics where the population uses natural fresh water for their domestic water supply, recreational activities, and agricultural production. Hence, disease transmission is contingent on the presence of infected water, the primary snail host, and contact with the human population [17]. Extreme poverty, lack of knowledge of the risks, an inadequacy or total lack of public health facilities along with the unsanitary conditions in which millions of people live their daily lives, especially in the rural areas of developing tropical countries, are all factors contributing to the risk of infection [15, 29].
Although there is no current estimate for the disease in Nigeria, past estimates have calculated infection rates of about 25 million people and 101 million at risk of infection [7]. In terms of urinary schistosomiasis endemicity, Nigeria has been divided into three zones: a hyperendemic zone, a moderately endemic zone, and a zone with low or no endemicity [8].
Our review followed a very encompassing approach, covering half a century (1961–2011) of urinary schistosomiasis in Nigeria. Topics of interest were prevalence, disease burden, risk factors, effects of global health policies in terms of World Health Organization (WHO) programmes on schistosomiasis control and the federal government’s approach to disease surveillance, control of transmission, and the road map to morbidity control and elimination. Special reference was made to the effects of dams, lakes and other water bodies in Nigeria impacting the spatial and temporal distribution of S. haematobium and the future success of disease control programmes. The Nigerian government’s efforts towards morbidity control through primary healthcare policies over the last 50 years in line with the WHO’s eradication road map were highlighted.
The presence of two forms of human schistosomiasis, caused either by Schistosoma haematobium or by Schistosoma mansoni, in Nigeria has been known since 1881. A report by the WHO in 1987 indicated that the urinary form of the disease (caused by S. haematobium) is widespread throughout Nigeria, while intestinal schistosomiasis (caused by S. mansoni) is less prevalent and was not reported in the south-eastern and some south-western parts of Nigeria [1]. As a result, this review is restricted to S. haematobium.
Methods
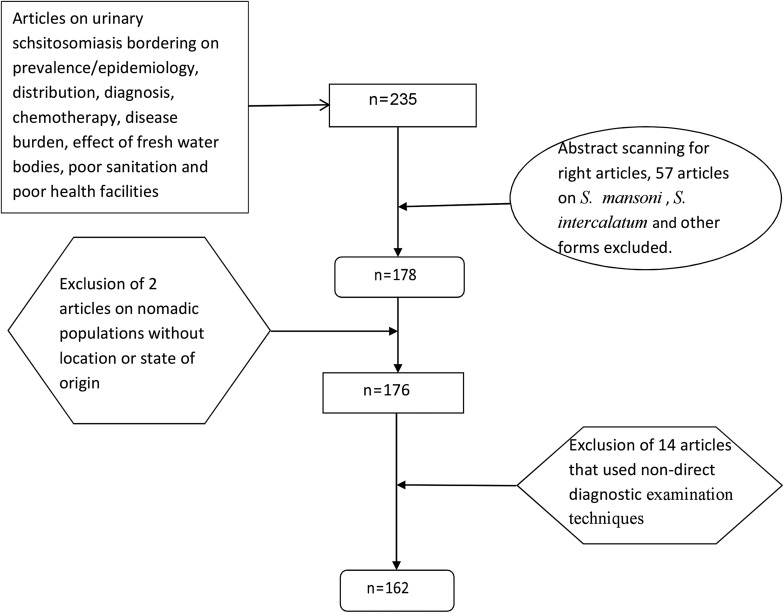
This review adapted in parts the methods of Hotez and Kamath [11] (2009) and the modified version of Schur et al. [21] (2011) as a framework outlined in the following steps (Fig. 1).
Figure 1.
Article selection flow chart.
Location, screening and selection of relevant publications
The literature search was done using an online literature database from 1961 to 2011, with urinary schistosomiasis listed as a neglected tropical disease on the PLoS Neglected Tropical Disease Website (http://www.gntd.org). This database collates general information about the type of publication, authors, and publication year, as well as study-specific information about the survey population, survey period, schistosome species, diagnostic test employed, and the number of infected individuals among those examined, stratified by age and sex (if available). We also examined all the journals related to S. haematobium epidemiology listed on African Journals Online (AJOL). The reference lists of identified articles and reviews were also searched manually, as were databases from the WHO, including the Weekly Epidemiological Record. All other publications on urinary schistosomiasis outside the mentioned databases were also included if they met the inclusion criteria.
Publications selection/inclusion criteria
The review focused on 50 years of Nigeria’s existence from 1961, exactly a year after Nigeria gained independence to the last date in 2011 and as such, all articles on urinary schistosomiasis concerning prevalence/epidemiology, distribution, diagnosis, chemotherapy, disease burden, effect of fresh water bodies, poor sanitation and poor health facilities within the set dates were included. The search procedure yielded 235 articles. However, abstracts were scanned to determine whether or not the articles were valid and all independent articles on other species of schistosomes such as S. mansoni and S. intercalatum were excluded, giving 178 articles. Moreover, all articles on nomadic populations without the exact state of origin within the Nigerian Federation were excluded, as well as articles with conflicting figures. This left a total of 176 articles. Articles reporting non-direct diagnostic examination techniques, such as immunofluorescence tests and antigen detections, or publications reporting on questionnaire data alone were excluded, and these final exclusion criteria yielded 162 articles deemed relevant.
Data extraction
The following information was extracted and recorded: general information about the type of publication, authors, publication year, as well as study-specific information about the survey population, the survey period, Schistosoma species (those other than S. haematobium were excluded), the diagnostic test employed, and the number of infected individuals among those examined stratified by age and sex (if available). These data formed the basis of the analysis.
Study areas
The studied areas where surveys and sample collections were carried out within Nigeria were recorded as geographical coordinates in latitudes and longitudes. Almost all articles showed the coordinates of their survey points or delineated them in area maps. However, some survey point geographical coordinates were not provided at the year of study or publication. Therefore Google Earth map link tele-atlas, 2012 was used to obtain their coordinates. Nonetheless, there are cases of interstate surveys that cannot be represented in clear coordinates, but the prevalence data for each state were used.
Sample collection
All articles indicated the time of urine sample collection as between 10 a.m. and 2 p.m. This is the time of midstream urine when all S. haematobium eggs shedding from patients were highest. All community-based surveys ensured pre-survey education of their volunteers before sample collection, while school-based surveys relied on school administrators to ensure accurate sample collection. Hospital-based survey used patients’ urine that presented haematuria/the eggs in diagnosis. All survey types took the precaution of ruling out menstruating female volunteers. Hence, all sample collections were reported to have followed standard urine sample collection procedures and conditions, and ensured the quality of the sample container. Ethical considerations were reported in each case, and ethical clearance was obtained from appropriate authorities.
Urine analysis
The urine samples were reported to be analysed almost immediately after sample collections, except in a few cases where the survey points were very far from points of analysis. However, reports indicated that adequate provisions were made beforehand to forestall the time lag before analysis in terms of urine sample preservation. This was done by transporting the specimen in a cold box containing ice blocks to laboratories where they were analysed. Some articles reported immediate use of reagent strips in the field to determine haematuria and subsequent sedimentation/centrifugation or filtration before microscopy. There were many cases of negative haematuria with positive egg results in many urine samples. The infection intensity was defined as the number of S. haematobium eggs contained in a 10 mL urine sample and S. haematobium eggs were identified as having a terminal spine in microscopy.
Results
Prevalence and geographical distribution
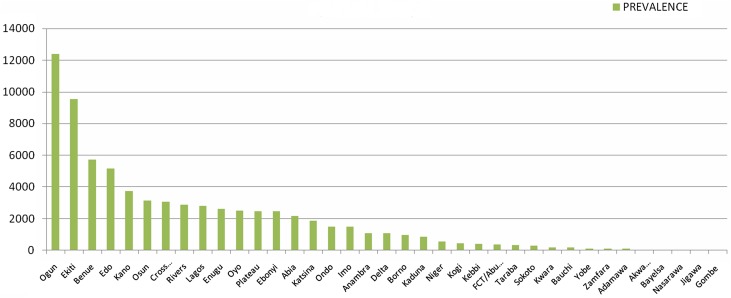
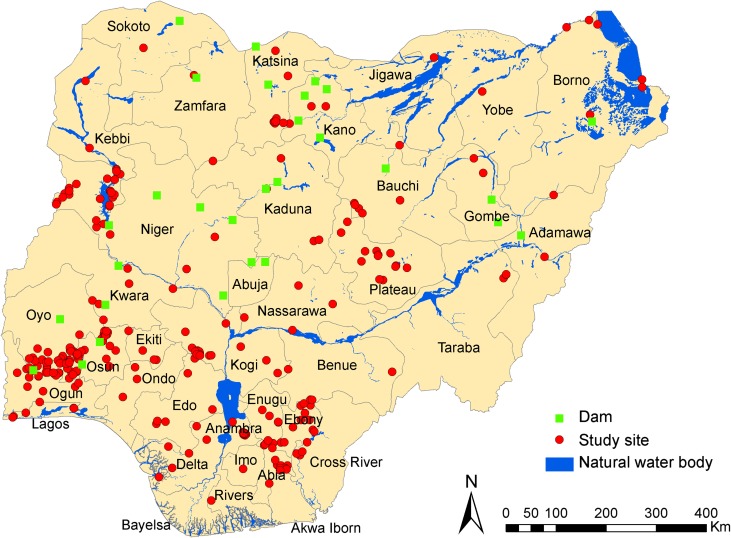
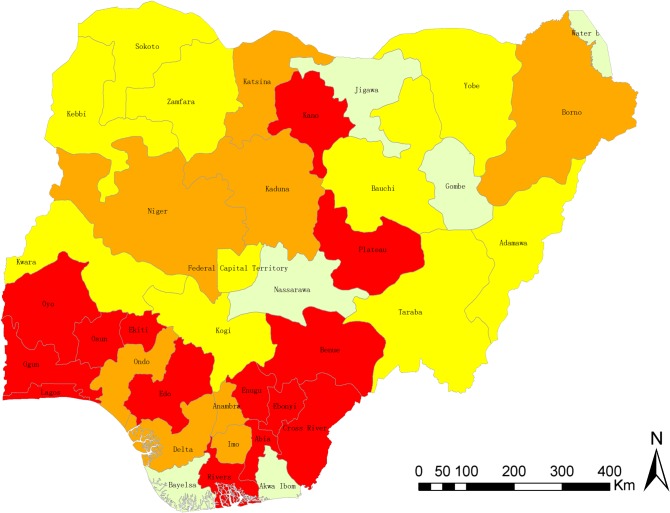
The exact degree of prevalence of urinary schistosomiasis in Nigeria is not known. The distribution and the prevalence level of the survey locations are shown in Figures 2–3 as well as Table 1, while ranking of the endemicity by state is shown in Table 2. An overview of the number of surveys with details given regarding sampling period, diagnostic technique, survey type, and prevalence, stratified by state is given in Table 1. Figure 2 is the bar chart representation of disease prevalence per state in Nigeria. Figure 3 is a map of Nigeria showing prevalence (cases per 100,000 inhabitants) and distribution of urinary schistosomiasis, while Figure 4 is a map of Nigeria showing the levels of endemicity of S. haematobium. These figures and tables are simply cumulative representations of various research work’s output included in this review. There are no baseline data or nationwide surveys carried out to serve as a reference point. It is known that states with low prevalence or without reports may be highly endemic with either S. mansoni or S. intercalatum, or have high prevalence of S. haematobium that is unreported. There are generally very few research reports on schistosomiasis in Nigeria. If we factor figures in Chitsulo et al. [7] (2000) and those at risk of infection and re-infection since the publication of the article into the prevalence, then Figure 3 will show a near real description of the geographical distribution of urinary schistosomiasis in Nigeria.
Figure 2.
Summary of the prevalence of Schistosoma haematobium across the 36 states of Nigeria including FCT.
Figure 3.
Map of Nigeria, showing location of study sites, dams, and natural water bodies.
Table 1.
Overview of the survey data included in the analysis stratified by state.
| Location |
Survey year |
Diagnostic technique |
Survey type |
Prevalence | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Unique | 1960s | 1970s | 1980s | 1990s | 2000+ | RS | SD | FT | DT | CB | SB | HB | ||
| Ogun | 45 | 41 | 0 | 1 | 0 | 5 | 9 | 4 | 9 | 1 | 1 | 8 | 7 | 0 | 12,400 |
| Ekiti | 18 | 12 | 0 | 0 | 0 | 0 | 4 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 9464 |
| Benue | 19 | 9 | 0 | 0 | 1 | 0 | 4 | 0 | 4 | 1 | 0 | 3 | 1 | 1 | 5735 |
| Edo | 50 | 10 | 0 | 0 | 0 | 1 | 8 | 1 | 8 | 0 | 0 | 7 | 2 | 0 | 5174 |
| Kano | 7 | 6 | 0 | 0 | 1 | 0 | 3 | 1 | 3 | 0 | 0 | 2 | 2 | 0 | 3731 |
| Cross River | 11 | 1 | 0 | 0 | 0 | 5 | 7 | 1 | 4 | 7 | 0 | 3 | 8 | 1 | 3168 |
| Osun | 21 | 20 | 0 | 1 | 2 | 2 | 7 | 2 | 5 | 5 | 0 | 4 | 7 | 1 | 3138 |
| Rivers | 5 | 4 | 0 | 0 | 0 | 1 | 3 | 1 | 3 | 0 | 0 | 3 | 1 | 0 | 2868 |
| Lagos | 15 | 10 | 2 | 2 | 5 | 0 | 2 | 3 | 4 | 3 | 1 | 3 | 8 | 0 | 2809 |
| Enugu | 22 | 17 | 0 | 0 | 1 | 2 | 3 | 2 | 1 | 3 | 0 | 2 | 4 | 0 | 2626 |
| Oyo | 18 | 15 | 2 | 5 | 0 | 3 | 6 | 1 | 14 | 1 | 0 | 7 | 8 | 1 | 2517 |
| Plateau | 14 | 10 | 0 | 0 | 0 | 2 | 4 | 1 | 5 | 0 | 0 | 4 | 2 | 0 | 2476 |
| Ebonyi | 40 | 39 | 0 | 0 | 0 | 0 | 9 | 2 | 6 | 1 | 0 | 3 | 5 | 1 | 2471 |
| Abia | 31 | 23 | 0 | 0 | 1 | 2 | 2 | 1 | 3 | 1 | 0 | 3 | 2 | 0 | 2162 |
| Katsina | 6 | 4 | 0 | 5 | 0 | 0 | 0 | 0 | 4 | 1 | 0 | 3 | 2 | 0 | 1863 |
| Ondo | 19 | 18 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 2 | 0 | 0 | 1508 |
| Imo | 28 | 22 | 0 | 0 | 0 | 0 | 4 | 2 | 3 | 0 | 0 | 4 | 0 | 0 | 1485 |
| Anambra | 8 | 6 | 0 | 0 | 0 | 3 | 3 | 0 | 4 | 2 | 1 | 2 | 4 | 0 | 1100 |
| Delta | 41 | 16 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 0 | 2 | 0 | 1085 |
| Borno | 3 | 2 | 0 | 0 | 1 | 0 | 2 | 1 | 3 | 0 | 0 | 0 | 2 | 0 | 983 |
| Kaduna | 9 | 5 | 0 | 1 | 2 | 1 | 3 | 1 | 5 | 1 | 0 | 3 | 2 | 3 | 868 |
| Niger | 13 | 8 | 0 | 0 | 1 | 0 | 3 | 1 | 4 | 0 | 0 | 1 | 3 | 0 | 543 |
| Kogi | 22 | 18 | 1 | 0 | 0 | 0 | 1 | 1 | 2 | 0 | 0 | 1 | 1 | 0 | 450 |
| Kebbi | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 406 |
| FCT | 6 | 5 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 360 |
| Taraba | 3 | 2 | 0 | 0 | 0 | 0 | 2 | 0 | 2 | 0 | 0 | 1 | 1 | 0 | 327 |
| Sokoto | 5 | 3 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 296 |
| Kwara | 1 | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 193 |
| Bauchi | 4 | 2 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 181 |
| Yobe | 2 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 1 | 0 | 1 | 127 |
| Zamfara | 6 | 3 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 117 |
| Adamawa | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 0 | 101 |
| Akwa Ibom | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Bayelsa | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Nasarawa | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Jigawa | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Gombe | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
Table 2.
Ranking of endemicity by state.
| Endemicity | States |
|---|---|
| Hyperendemic zone (>50%) | Abia, Ebonyi, Enugu,Osun, Ogun, Lagos, Rivers, Cross Rivers, Edo, Benue, Kano, Oyo, Ekiti, Plateau |
| Moderately endemic zone (10%–50%) | Anambra, Ondo, Imo, Delta, Borno, Kaduna, Niger, Katsina |
| Low endemic zone (1%–10%) | Kogi, Taraba, Adamawa, Kebbi, Sokoto, Bauchi, Yobe, Kwara, Zamfara, Abuja |
| No report | Gombe, Akwa Ibom, Jigawa, Nasarawa, Bayelsa. |
Figure 4.
Map of Nigeria, showing the level of endemicity of urinary schistosomiasis by state. Red: highly endemic (>50%); brown: moderately endemic (10–50%); yellow: low endemic (1–10%); grey: no report of urinary schistosomiasis.
Table 3.
The distribution of the snail host and human schistosomiasis in investigated artificial lakes/dams in Nigeria.
| S/N | Name of dam | Location | Size | Purpose | Year | Snail | Human infection |
|---|---|---|---|---|---|---|---|
| 1 | Kubani | Kaduna | Medium | WS | 1975 | Positive | NI |
| 2 | Kangimi | Kaduna | Large | WS, IR | 1977 | Positive | NI |
| 3 | Bagoma | Kaduna | Large | WS, IR | 1974 | Positive | NI |
| 4 | Zaria | Kaduna | Large | MP | 1974 | Positive | NI |
| 5 | Baugauda | Kano | Large | MP | 1970 | Positive | NI |
| 6 | Karaye | Kano | Large | MP | 1971 | Negative | NI |
| 7 | Tiga | Kano | Large | MP | 1975 | Positive | Positive |
| 8 | Jakara | Kano | Large | MP | 1976 | Negative | NI |
| 9 | Ruwan Kanya | Kano | Large | MP | 1976 | Positive | NI |
| 10 | Tomas | Kano | Large | MP | 1976 | Positive | Positive |
| 11 | Kafin Chiri | Kano | Large | MP | 1977 | Negative | NI |
| 12 | Tudun Wada | Kano | Large | MP | 1977 | Negative | NI |
| 13 | Gari | Kano | Large | MP | 1980 | Negative | NI |
| 14 | Marashi | Kano | Large | MP | 1980 | Negative | NI |
| 15 | Pada | Kano | Large | MP | 1980 | Negative | NI |
| 16 | Watari | Kano | Large | MP | 1980 | Negative | NI |
| 17 | Magaga | Kano | Large | MP | 1990 | Positive | NI |
| 18 | Challawa Gorge | Kano | Large | MP | 1992 | Negative | NI |
| 19 | Kango | Kano | Large | MP | UC | Negative | NI |
| 20 | Warwade | Kano | Large | MP | NA | Negative | Negative |
| 21 | Birmin Kudu | Kano | Small | MP | 1970 | Negative | NI |
| 22 | Rimin Gado | Kano | Small | WS,RC | 1978 | Positive | Positive |
| 23 | Dogwala | Kano | Small | FL | NA | Negative | NI |
| 24 | Duduvum | Kano | Small | FL | NA | Negative | NI |
| 25 | Gata | Kano | Small | FL | NA | Negative | NI |
| 26 | Garanga | Kano | Small | FL | NA | Negative | NI |
| 27 | Rugunsana | Kano | Small | FL | NA | Negative | NI |
| 28 | Gulka | Kano | Small | FL | NA | Negative | NI |
| 29 | Iggi | Kano | Small | FL | NA | Negative | NI |
| 30 | Guzu Guzu | Kano | Small | FL | NA | Negative | NI |
| 31 | Kefin Gana | Kano | Small | FL | NA | Negative | NI |
| 32 | Kiwia | Kano | Small | FL | NA | Negative | NI |
| 33 | Kiyako | Kano | Small | FL | NA | Negative | NI |
| 34 | Kara Dumba | Kano | Small | FL | NA | Negative | NI |
| 35 | Malumfashi | Katisina | Large | MP | NA | Positive | Positive |
| 36 | Zobe | Katisina | Large | MP | NA | Positive | Positive |
| 37 | Kainji | Niger | Large | MP | 1968 | Positive | Positive |
| 38 | Oyan | Ogun | Large | MP | NA | Positive | Positive |
| 39 | Opa | Osun | Large | WS | 1980 | Positive | Positive |
| 40 | Eleiyele | Oyo | Large | WS | 1942 | Positive | NI |
| 41 | Oba | Oyo | Large | WS | 1964 | Positive | NI |
| 42 | Opeki | Oyo | Large | WS | 1967 | Positive | NI |
| 43 | Wurno | Sokoto | Small | MP | 1960 | Positive | Positive |
| 44 | Goronyo | Sokoto | Large | MP | 1983 | Negative | Negative |
| 45 | Bakolori | Zamfara | Large | MV | 1982 | Positive | Positive |
Notes: MP = Multipurpose use, WS = Water supply, RC = Recreation, IR = Irrigation, NA = Not available, NI = Not investigated, FL = Flood control, UC = Under construction, S/N = Serial number, Nil = Not detected.
Large dams are all dams >15 m high or all dams with height 10–15 m having length of crest >500 m and/or reservoir capacity >1 million m3. Medium dams are all dams with height 8–10 m; and Small dams are all dams <8 m high.
Disease burden
Nigeria ranks highest in terms of schistosomiasis burden among the countries in sub-Saharan Africa (SSA) [11]. Of the 192 million cases estimated in SSA by Steinmann et al. [22], Nigeria alone has 29 million cases. The disease burden, i.e., Disability-Adjusted Life Year (DALYs) in sub-Saharan Africa resulting from schistosomiasis is estimated to be 1.6–4.2 million, which is 93% of estimated global disease burden in DALYs, put at 1.7–4.5 million [11]. Of this estimate, Nigeria ranks highest as of 2006. Urinary schistosomiasis accounts for more than 90% of all schistosomiasis cases in Nigeria, suggesting that the DALYs in Nigeria resulting from schistosomiasis are mainly from urinary schistosomiasis.
Control measures
Currently, there is no separate control measure applicable in Nigeria other than the measures the Federal Ministry of Health outlined in its Primary Health Policy covering all infectious diseases. However, Nigeria has adopted the WHO’s strategy for schistosomiasis control but there is an apparent gap in policy making and implementation. Recently, the Carter Center-assisted programme in Nigeria provided health education and schistosomiasis treatment to communities in four states – Plateau, Delta, Edo, and Nasarawa – where the burden of the disease is high, and as of 2011, the programme has assisted by providing more than 6 million cumulative praziquantel tablets which have been distributed primarily to children since 1999. The vast majority of these treatments were distributed during 2008–2011 alone, through a scale up of activities made possible through a donation to the Center from the World Health Organization and Merck KGaA (Germany) (http://www.cartercenter.org/health/schistosomiasis/index.html). The remaining 33 states and Federal Capital Territory are meant to be covered under the Mass Drug Administration (MDA) programmes of the WHO and the Federal Ministry of Health.
Discussion
There is currently no vaccine for schistosomiasis. Control measures rely on the use of a chemotherapeutic drug – praziquantel, which provides a safe and effective oral treatment against all human schistosome species. It is an essential tool that led to a shift in the global control strategy from transmission containment to morbidity control that occurred in the mid-1980s [19].
WHO has set a target to regularly treat 75% of school-aged children at risk of morbidity due to schistosomiasis by 2010, in support of the 54th World Health Assembly which passed a resolution urging member states to provide drug treatment to high-risk groups [6] and in 2002, a grant from the Bill and Melinda Gates Foundation (BMGF) to the Schistosomiasis Control Initiative (SCI), Imperial College of Science Technology and Medicine, enabled the initiation of country-wide control programmes in six African countries. The increasing expansion of international initiatives to reduce the disease burden of helminth infections in the developing world has been catalysed by “funding from the BMGF, donations from several drugs companies, and the reduced price of praziquantel” [14]. But how would all these measures fare in Nigeria considering that there is no clear road map for schistosomiasis control in the country, no accurate national data on prevalence and distribution, treatment and the predisposing factors to re-infection after treatment?
In Nigeria, S. haematobium infection had been found in many parts of the country with varying intensities and prevalence rates, and incidence is believed to be on the increase [19]. The true epidemiological data appear difficult to determine in developing nations because of inadequate research and no epidemiological control/information centre on tropical diseases, despite its relevance in planning for control in any locality. It is known that schistosomiasis affects up to 50% or more of people in some areas of Nigeria, but the total number of affected persons is unknown. Endemicity may be linked to behaviour, lack of education, public health facilities, very poor sanitary conditions and poverty in this part of the world [24]. The prevalence of this disease like many other endemic diseases is affected by the socio-cultural characteristics of Nigeria. As a result, the prevalence of this disease is also affected by these characteristics and accounts for the obvious difference in the distribution of the disease between southern and northern parts of the country [30]. Even within the same geographical area, such differences are likely to exist between different age groups. Although the prevalence of urinary schistosomiasis is found not to be uniform over the five decades in the states studied, the distribution among sexes was similar in that more males were infected than females, and this finding is statistically significant (p < 0.05) [4, 17, 23]. However, some studies in the southern parts of Nigeria showed that females have a higher prevalence of urinary schistosomiasis than males [3, 16]. The reason for this is that women are mostly involved in activities known to favour infection due to their gender-assigned responsibilities.
Socio-cultural factors like washing, fishing and recreational activities in fresh water harbouring infected snails facilitate the transmission of the disease. These practices are very common in the rural areas of northern Nigeria and many other villages in the western and eastern parts of the country. The construction of earth dams for dry season farming contributes to the high prevalence and distribution of the disease in this part of the country. Also, communities around most fresh water bodies show very high prevalence (Fig. 4). A total of 47 (15%) of the 323 dams in Nigeria have been surveyed for the presence of the snail intermediate host species of schistosomiasis, taking into consideration its distribution and ecology. The survey revealed that 45 of the 47 dams are located in the hyperendemic zone, while the remaining two are located in the moderately endemic zone. Results show that 20 (43%) of the total surveyed dams harboured Bulinus globosus and/or Biomphalaria pfeifferi, the local intermediate host of the Schistosoma parasite. Eighteen of these are located in the hyperendemic zone, while the other two are in the moderately endemic zone. Fifteen of them are in the northern part of the country and the remaining five are in the southwest [18]. Since the intermediate host of schistosomiasis breeds in slow-flowing/stagnant water, reservoirs of dams provide favourable conditions for year-round transmission of the disease, even in areas where snail distribution used to be seasonal [5]. Imevbore et al. [12] showed that within the reservoirs, distribution is focal and is confined to human contact sites, especially along their shallow vegetative shore, not more than a few meters from the shores or deep into the water. The endemicity ranking by state (Table 2) shows some areas of contrast in that some well-known states classified by Cowper et al, 1965 as hyperendemic are now in moderately endemic or low endemic zones. Obviously, this is due to low research levels or survey data over the decades in review. Hence, Table 2 cannot really serve as a reference as the data forming the classification represented in the table are grossly insufficient owing to very low research levels and survey data. The information is nonetheless informative. The merging of data arising from the prevalence of urinary schistosomiasis predicted due to dams and the data in Table 2 give a better estimated prevalence of the disease over the last 50 years so far reported in Nigeria within the context of this review inclusion criteria. Therefore, Figure 3 represents the total known cases of urinary schistosomiasis reported in various surveys over the five decades. Conclusively, it is very clear that the Federal Ministry of Health should urgently carry out a national survey to guide the various programmes for schistosomiasis control. More research is needed to elucidate the transmission patterns of different species and as well an overall political will on the part of government to cut transmission through several measures: mass education, provision of potable water, and proper waste disposal facilities to all rural areas (especially settlements around dams), and adequate checks on sanitary conditions of residents and a continuous MDA programme.
Conclusion
We conclude that there is an urgent need to carry out a nationwide survey to help in planning, coordinating, and evaluating schistosomiasis control activities.
Competing interests
The authors declare that they have no competing interests.
Cite this article as: Ezeh CO, Onyekwelu KC, Akinwale OP, Shan L & Wei H. 2019. Urinary schistosomiasis in Nigeria: a 50 year review of prevalence, distribution and disease burden. Parasite 26, 19.
References
- 1.Anonymous. 1987. Atlas of the global distribution of schistosomiasis Nigeria. http://www.who.int/schistosomiasis/epidemiology/en/nigeria.pdf.
- 2.Anosike JC, Okere AN, Nwoke BE, Chukwu JU, Nwosu DC, Njoku-Tony RF, Oguwuike TU, Ezike MN, Okogun RA, Obasi CU, Ogbusu FI, Onyirioha CU, Ajero CM, Dike MU. 2003. Endemicity of vesical schistosomiasis in the Ebonyi Benue river valley, south eastern Nigeria. International Journal of Hygiene and Environmental Health, 206, 205–210. [DOI] [PubMed] [Google Scholar]
- 3.Anyagwe S, Njikan ONM, Kouemen L. 1992. Urinary schistosomiasis in women an anthropological descriptive study of Holo-endemic focus in Cameroun, OSLO, Norway.
- 4.Bello YM, Adamu T, Abubakar U, Muhammad AA. 2003. Urinary schistosomiasis in some villages around the Goronyo Dam, Sokoto state, Nigeria. Nigerian Journal of Parasitology, 24, 109–114. [Google Scholar]
- 5.Betterton C, Ndifon GT, Bassey SE, Tan RM, Oyeyi T. 1988. Schistosomiasis in Kano state, Nigeria. I. Human infections near dam sites and the distribution and habitat preferences of potential snail intermediate hosts. Annals of Tropical Medicine and Parasitology, 82, 561–570. [PubMed] [Google Scholar]
- 6.Brooker S, Whawell S, Kabatereine NB, Fenwick A, Anderson RM. 2004. Evaluating the epidemiological impact of national control programmes for helminths. Trends in Parasitology, 20, 537–545. [DOI] [PubMed] [Google Scholar]
- 7.Chitsulo L, Engels D, Montresor A, Savioli L. 2000. The global status of schistosomiasis and its control. Acta Tropica, 77, 41–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cowper SG. 1973. Bilharziasis (schistosomiasis) in Nigeria. Tropical and Geographic Medicine, 25, 105–118. [PubMed] [Google Scholar]
- 9.Edungbola LD, Asaolu SO, Omonisi MK, Aiyedun BA. 1988. Schistosoma haematobium infection among schoolchildren in the Babana district, Kwara state, Nigeria. African Journal of Medicine and Medical Sciences, 17, 187–193. [PubMed] [Google Scholar]
- 10.Ekejindu IM, Ekejindu GOC, Agbai A. 2002. Schistosoma haematobium infection and nutritional status of residents in Ezi-Anam, a riverine area of Anambra state, South-Eastern Nigeria. Nigerian Journal of Parasitology, 23, 131–138. [Google Scholar]
- 11.Hotez PJ, Kamath A. 2009. Neglected tropical diseases in sub-saharan Africa: review of their prevalence, distribution, and disease burden. PLoS Neglected Tropical Diseases, 3, e412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imevbore AMA, Ofoezie IE, Obot EA. 1986. Report on the study on snail and cyclopoid borne disease: problems of small scale water resources development projects in Nigeria. O. A.U., Ile-Ife, Nigeria: The Institute of Ecology.
- 13.Kjetland EF, Ndhlovu PD, Gomo E, Mduluza T, Midzi N, Gwanzura L, Mason PR, Sandvik L, Friis H, Gundersen SG. 2006. Association between genital schistosomiasis and HIV in rural Zimbabwean women. AIDS, 20, 593–600. [DOI] [PubMed] [Google Scholar]
- 14.Lammie PJ, Fenwick A, Utzinger J. 2006. A blueprint for success: integration of neglected tropical disease control programmes. Trends in Parasitology, 22, 313–321. [DOI] [PubMed] [Google Scholar]
- 15.Michaud CM, Gorden WS, Reich MR. 2003. The global burden of diseases due to schistosomiasis DCPP working paper. http://www.hsph.harvard.edu/schisto.
- 16.Nwaogu OC. 1992. Schistosomiasis and women in Amagunze, Southeastern Nigeria. Oslo, Norway: p. 6–8. [Google Scholar]
- 17.Nwosu DC, Anosike JC, Nwoke BEB, Uwaezouke JC. 2006. Epidemiological assessment of vesical schistosomiasis in Bende local government area of Abia state, Nigeria. Journal of Applied Sciences and Environmental Management, 10, 55–60. [Google Scholar]
- 18.Ofoezie IE. 2002. Human health and sustainable water resources development in Nigeria: schistosomiasis in artificial lakes. Natural Resources Forum, 26, 150–160. [Google Scholar]
- 19.Okon OE, Udoutun MF, Oku EE, Nta AI, Etim SE, Abraham JT, Akpan PA. 2007. Prevalence of urinary schistosomiasis in Abini community, Biase local government area, Cross River state, Nigeria. Nigerian Journal of Parasitology, 28, 28–31. [Google Scholar]
- 20.Olusegun AF, Ehis OC, Richard O. 2011. Proportion of urinary schistosomiasis among HIV-infected subjects in Benin city, Nigeria. Oman Medical Journal, 26, 175–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schur N, Hurlimann E, Garba A, Traore MS, Ndir O, Ratard RC, Tchuem Tchuenté LA, Kristensen TK, Utzinger J, Vounatsou P. 2011. Geostatistical model-based estimates of schistosomiasis prevalence among individuals aged ≤ 20 years in West Africa. PLoS Neglected Tropical Disease, 5, e1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steinmann P, Keiser J, Bos R, Tanner M, Utzinger J. 2006. Schistosomiasis and water resources development: systematic review, meta-analysis, and estimates of people at risk. Lancet Infectious Disease, 6, 411–425. [DOI] [PubMed] [Google Scholar]
- 23.Ude EA, Akinwale OP, Ukaga CN, Ajayi MB, Akande OD. 2009. Prevalence of urinary schistosomiasis in Umuowele, Agulu community, Anambra state, Nigeria. International Journal of Health Research, 2, 347–353. [Google Scholar]
- 24.Ukoli FMA. 1992. Prevention and Control of Parasitic Diseases in Tropical Africa. PLC Ibadan, Nigeria: University Press p. 32. [Google Scholar]
- 25.van der Werf MJ, de Vlas SJ, Brooker S, Looman CW, Nagelkerke NJ, Habbema JD, Engels D. 2003. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Tropica, 86, 125–139. [DOI] [PubMed] [Google Scholar]
- 26.WHO. 1993. The control of schistosomiasis: report of the WHO Expert Committee. Geneva, Switzerland: World Health Organization; Technical Report Series. [Google Scholar]
- 27.WHO. 1995. Identification of high-risk communities for control of schistosomiasis in Africa: a multi community study. Geneva, Switzerland: World Health Organization; Social and Economic Research Reports. [Google Scholar]
- 28.WHO. 1998. Guidelines for the evaluation of soil transmitted helminthiasis and schistosomiasis at community level: a guide for managers of control programmes. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 29.WHO. 2002. Prevention and control of schistosomiasis and soil transmitted helminthiasis. Geneva, Switzerland: World Health Organization; Technical Report Series. [PubMed] [Google Scholar]
- 30.Zoakah AI, Okoronkwo MA, Gajida AU. 2004. Urinary schstosomiasis in Katarko, Yobe state northeastern Nigeria. Nigerian Journal of Basic and Clinical Sciences, 1, 14–17. [Google Scholar]