Abstract.
Feeding of infant formula using contaminated bottles may be an important transmission pathway of enteric pathogens during early life. Determinants of suboptimal bottle hygiene and the feasibility and acceptability of intervention strategies have not been well assessed. We evaluated the extent of bottle contamination, its contributing factors, and options for promoting improved bottle hygiene in a Peruvian shantytown. During Phase 1, we sampled from bottles and caregiver hands (n = 48) and processed for enumeration of total coliform and Escherichia coli colony-forming units. A semi-structured questionnaire captured bottle use and hygiene practices. Phase 2 involved the identification of candidate practices to recommend to caregivers. Phase 3 consisted of a behavioral trial in which 14 caregivers were educated about improved practices for bottle disinfection and later reported on their experiences implementing them. Fecal bacteria were detected in 43.8% of bottles sampled during Phase 1 and in 21.7% of hands. Caregivers overall did not use effective methods for disinfecting bottles, displayed misunderstandings surrounding hygienic practices, and few had ever discussed bottle hygiene with a health provider. Findings from the behavioral trial indicated that the improved practice of brushing the bottle with dish detergent for 30 seconds after every use is preferable to boiling the bottle for several minutes daily as caregivers reported that the brush was simple to use, efficient, and practical. The promotion of a bottle brush and detergent is a feasible and acceptable intervention strategy in peri-urban settings, and future research should evaluate its long-term effectiveness for reducing bottle contamination.
INTRODUCTION
Repeated exposure to enteric pathogens during infancy is an important cause of growth stunting in developing countries.1,2 Stunting is not only a leading risk factor for childhood morbidity but also carries lifelong consequences such as cognitive impairments and decreased economic productivity.3–8 In Peru, as in most resource-poor settings, stunting tracks closely with poverty: Whereas stunting affects only 3.7% of children in the highest wealth quintile, it affects 34.0% of Peruvian children in the lowest wealth quintile.9 As a result, the long-term sequelae of stunting may reinforce the economic disadvantages experienced by those who are most vulnerable to chronic malnutrition in early life.
Infants who are not exclusively breastfed are more susceptible to diarrhea and asymptomatic enteric infections.10–13 This risk may be attributed in part to the transmission of infectious agents during bottle-feeding. High levels of fecal bacterial contamination have been found in the lacteal contents of bottles,14–19 as well as on bottles and nipples themselves.20–23 Studies that have recovered specific pathogens from bottles identified enteropathogenic Escherichia coli and Staphylococcus aureus as the most common bacteria.20,21,23 In peri-urban Peru, as early as 1989, a study found 35% of bottle nipples and 23% of bottles to be contaminated with E. coli—higher than any other household item sampled.24
Current trends toward increased formula feeding for infants less than 6 months of age in Peru pose serious risks for enteric infections.9,25 Although Peru’s exclusive breastfeeding rates improved considerably during the 1980s and 1990s, this progress has slowed since 2004. In turn, the use of infant formula and bottles has increased.26–28 According to Peru’s Demographic and Health Survey, in 2014, the rate of bottle use among infants < 2 months of age had returned to levels seen in 1992 (30.4%), after falling to a low of 18.3% in 2004.9,25,29
Bacterial outgrowth in feeding bottles is facilitated by the tendency of formula or milk to become a culture medium and by the difficulty of adequately cleaning bottles. Several studies have postulated relationships between bacterial counts and self-reported bottle-cleaning practices, yet several have failed to demonstrate significant associations. In Brazil, no differences were observed in median coliform counts between bottles that were reportedly washed or disinfected and those that were not, and in the United Kingdom, bacterial contamination (> 5 colonies/mL) was found in 54% of bottles that were self-reported to be sterilized through boiling.16,22
Such findings point to the need to better explore patterns of bottle contamination, caregivers’ perceptions of bottle-cleaning practices, and the barriers to effective disinfection. In addition, research is needed on opportunities for changing behaviors within the home. An understanding of these factors is critical to developing intervention strategies that may reduce infants’ exposure to pathogens through bottle-feeding.
We conducted this study to explore the determinants of suboptimal bottle hygiene in peri-urban Peru and to identify realistic strategies to improve those practices. The study had three objectives: 1) to quantify fecal contamination in bottles and current bottle-feeding and bottle-cleaning practices; 2) to identify effective bottle disinfection practices using local resources; and 3) to evaluate the acceptability and feasibility of improved practices for bottle care.
MATERIALS AND METHODS
This study involved three sequential phases of data collection to first explore the parameters of bottle contamination and then develop and evaluate measures to improve bottle hygiene (Table 1). Data collection was carried out in Villa El Salvador, a coastal, peri-urban district on the southern outskirts of Lima, Peru. Most of the approximately 380,000 inhabitants of this shantytown (pueblo joven) are first- or second-generation migrants from the Andean region, and have settled the area through a series of “invasions” in which families stake out plots of unauthorized land, build homes, and over time seek recognition and infrastructure from the local government.30 Data were collected from four of Villa El Salvador’s 10 sectors. The district has an altitude of 1,550 m.
Table 1.
Data collection methods, goals, and participants by study phase
| Data collection method | Goal of method | Number of participants |
|---|---|---|
| Phase 1: assessment of current landscape | ||
| Sample collection from bottles and hands | Estimate levels of fecal bacterial contamination in bottles and hands | 48 |
| Semi-structured questionnaire | Explore bottle-cleaning practices and barriers to optimal bottle hygiene | 48 |
| Phase 2: development of improved practices | ||
| Bottle-cleaning trial | Identify efficacious practices to promote during TIPs | NA (six replicates under controlled conditions) |
| Phase 3: TIPs | ||
| Semi-structured interviews | Assess feasibility and acceptability of improved practices | 14 |
NA = not applicable; TIPs = trial of improved practices.
Participants and sampling.
This study is nested within a larger cohort study on viral diarrhea in which infants less than 6 months of age have an average of 0.26 diarrhea episodes per child-month. All participants were recruited from households enrolled in the cohort study. A purposeful sampling scheme ensured that participants represented all four sectors comprising the cohort study’s field site as they differed in terms of socioeconomic status and water and sanitation access.31 A minimum of eight participants were recruited from each sector. In addition, we attempted to recruit caregivers with considerable variation regarding characteristics that may be relevant to infant feeding practices, such as education level and marital status.
Cohort study field workers conduct daily surveillance of infant health and caregiving behaviors, including breastfeeding status, and thus their records were used to identify potential participants for the present study. Caregivers were eligible to participate if they were currently bottle-feeding an infant younger than 9 months of age. “Caregiver” was defined as any member of the family who dedicated significant time (> 4 hours/day) to caring for and feeding the infant during the day.
For the third phase of the study, a subset of participants was selected from the initial sample based on results from the first study phase. Again, participants were recruited from distinct areas of the community to maximize geographic and socioeconomic diversity of the group.
Data collection.
Phase 1: assessment of current landscape.
Phase 1 (January–March 2017) consisted of sample collection from bottles and caregiver hands and the administration of a semi-structured questionnaire. Samples were collected during home visits by a trained field worker and the first author. Before collecting the sample, the field worker asked if the infant’s bottle was currently being used or was hypothetically ready to be used. Because the goal of this method was to quantify the fecal bacteria that may be transmitted via bottle-feeding, we did not sample from bottles that were considered dirty and not ready for use at the time of the visit.
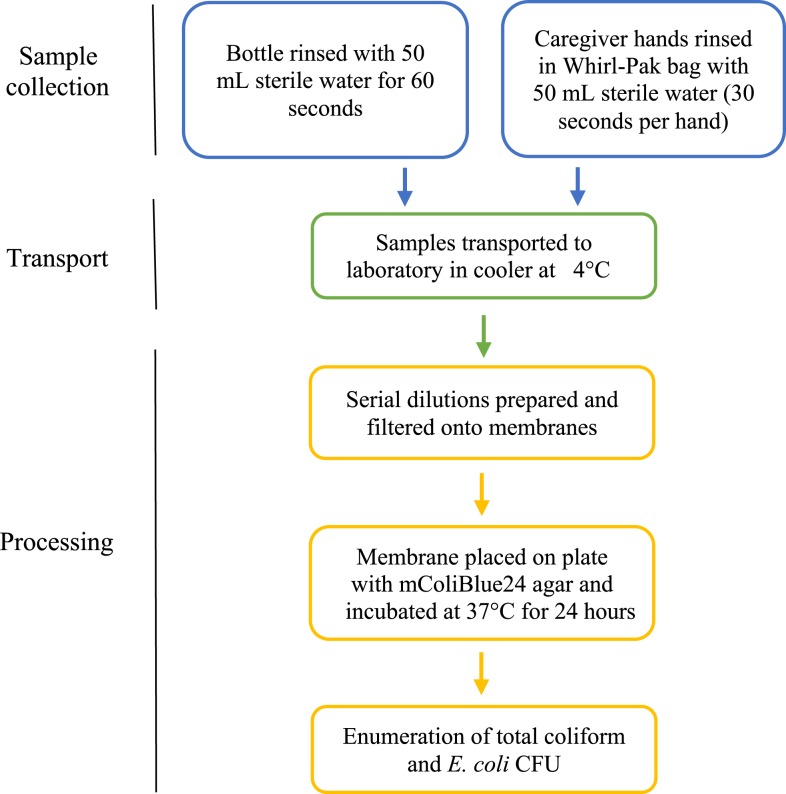
Bottle samples were collected aseptically by rinsing the bottle with 50 mL of sterile water for 60 seconds. Hand samples were collected by asking the caregiver to rinse each hand for 30 seconds in a sterile Whirl-Pak bag filled with 50 mL of sterile water. Each 50-mL sample was then placed in a sterile falcon tube, labeled, and stored in an insulated cooler with ice packs until being transported to the laboratory for processing (Figure 1). Controls of sterile water prepared in the field were sent to the laboratory on the first and last days of sampling each week to ensure that the water was not contaminated during any step of the procedure. Sampling took place during the summer months (January–March 2017) when the mean daily temperature was 24.2°C. All samples were collected between 9:15 am and 11:30 am to allow for same-day processing.
Figure 1.
Procedures for sample collection and processing. This figure appears in color at www.ajtmh.org.
Bottle and hand samples were analyzed for total coliform and E. coli, a reliable proxy indicator of fecal bacterial contamination.32 As illustrated in Figure 1, two serial dilutions were prepared for each sample, which were then filtered through a 47-mm-diameter, 0.45-µm-pore size filter and incubated on m-ColiBlue24 agar at 37°C for 24 hours, in accordance with the manufacturer’s instructions (Hach Company, Loveland, CO). Total coliform and E. coli colonies were enumerated based on the number of red and blue colonies, respectively. Coliform density was determined by dividing the number of colonies counted by the volume of rinse filtered after accounting for the dilution, producing a value of colony-forming units (CFUs) per mL. Averages were taken between multiple dilutions to determine the estimate for each sample. If there were more than 200 colonies of all types, results were reported as “too numerous to count” per the manufacturer’s instructions, and the other dilution prepared for the sample was used to determine coliform density. The presence of E. coli was confirmed through colorimetric biochemical assays (triple sugar iron, lysine iron agar, Simmons’ citrate agar, and sulfide indole motility) of representative colonies picked from the agar plates. All processing took place at the Universidad Peruana Cayetano Heredia in Lima, Peru, within 6 hours of sampling.
The field worker administered a semi-structured questionnaire in Spanish at the time of sample collection to record information about bottle characteristics, usage, and cleaning methods. The use of detergent, a bottle brush, and boiling were of particular interest as these disinfection practices are recommended by the WHO.33 Participants’ sources of information regarding formula and bottle hygiene were also explored. The questionnaire was informed by the Integrated Behavioral Model for Water, Sanitation, and Hygiene (IBM-WASH), which identifies psychosocial, technology, and contextual determinants of WASH behaviors that operate across several ecological levels.34 Most questions had discrete response options, yet open-ended questions were included to allow participants to elaborate on their experiences and the challenges to bottle disinfection. The questionnaire was translated from English to Spanish by the first author and then reviewed during a workshop with field workers to ensure that all phrasing would be comprehensible among the study population. Finally, it was back-translated to English by another bilingual member of the research team to confirm the accuracy of the translation, resulting in minor changes to the Spanish version.
During the administration of the questionnaire, responses to open-ended questions were digitally audio-recorded. At the end of the home visit for Phase 1, caregivers were informed that the laboratory results would be shared within 2 months. Sociodemographic information about each participant and household living conditions had been previously collected on enrollment into the parent cohort study.
Phase 2: development of improved practices.
Phase 2 (March 2017) involved a small laboratory trial comparing bottle-cleaning methods to inform the content of the behavioral trial in Phase 3. Methods assessed were derived from international guidelines for the safe handling of infant formula, which recommend that “Where feeding bottles are used, clean bottle and teat brushes should be used to scrub inside and outside of bottles and teats.”33 Thus, the trial sought to evaluate the relative efficacy of a set of bottle-cleaning procedures using a nylon-bristle bottle brush purchased in the field site, under controlled conditions.
A solution of 1,000 CFU/mL was prepared by isolating E. coli colonies from previously plated samples and culturing with tryptic soy agar. This was used to contaminate six new plastic bottles with 15 mL of the solution each, and the bottles were agitated for 60 seconds and then left for 15 minutes. One contaminated bottle served as the baseline measure of contamination, and the remaining five bottles were each subjected to one of five cleaning procedures. The procedures were 1) rinsing twice with water, 2) brushing with water for 30 seconds, 3) brushing with water for 60 seconds, 4) brushing with water and Ayudin (the local dish detergent) for 30 seconds, and 5) brushing with water and Ayudin for 60 seconds. Rinse was defined as filling the bottle with 90 mL of previously boiled (and then cooled to room temperature) water, closing with the nipple, swirling three times until the water reached the top of the bottle, and then inverting three times. Brush was defined as filling the bottle with 90 mL of previously boiled water and brushing the interior of the bottle in an up-and-down motion for the specified period of time, and then brushing the nipple for an equal period of time. The research team deemed the use of boiled water as feasible for households because all cohort study households had reported boiling water for drinking in the sociodemographic questionnaire administered on cohort study enrollment.
Bottle samples were collected and processed according to the same procedures used for field samples (described previously). Six replicates of this trial were conducted. A colony reduction to < 5 CFU/100 mL was set as the acceptable level of contamination. Colony reductions were calculated by comparing the average value of the results of each cleaning method with the average baseline sample.
Phase 3: trial of improved practices (TIPs).
The final study phase (March–April 2017) entailed a TIPs to assess the feasibility and acceptability of two demonstrated practices for improved bottle hygiene. Trials of improved practices, also known as behavioral trials, are a formative research method in which community members are treated as consultants to explore their perceptions and experiences with recommended activities, with the goal of informing future intervention design and implementation.35 In our study context, the first improved practice—“boil the bottle by removing the nipple and keeping the bottle and nipple on the stove at a rolling boil for several minutes at least once per day”—was selected based on existing evidence.33 The second improved practice was identified from the results of the controlled trial and consisted of “brush the bottle with Ayudin for 30 seconds after every use.”
The TIPs was conducted over a 2-week period with a subset of participants for Phase 1. Two household visits were conducted by a team consisting of a nurse-field worker and the first author. On the first visit, the team shared the results from the household’s sample collection, discussed the risks associated with bottles that are not fully disinfected, and explained one of the two improved bottle disinfection practices. A nylon-bristle brush and small container of Ayudin (310 g) were provided to each caregiver for whom the brushing practice was recommended. In addition, the nurse-field worker provided live demonstrations of the recommended practice if permitted and provided an opportunity for the caregiver to ask questions to ensure that all steps were understood. Caregivers were asked to implement the recommended practices for at least 1 week, or until the field worker returned for the follow-up visit.
Within 7–10 days of the initial visit, follow-up semi-structured interviews were completed and audio-recorded to explore caregiver experiences and attitudes surrounding the recommended practices. The team assessed how and with what frequency the caregiver had disinfected the bottle over the past week, motivating factors, and barriers and facilitators to the recommended practice.
Data analysis.
Data entry and statistical analyses.
Data were entered and analyzed using Visual FoxPro and Stata Statistical Software version 13 (StataCorp LP, College Station, TX). The presence or absence of bacterial contamination in the samples was measured as a dichotomous variable: neither the sterile water controls nor negative samples contained any detectable CFU. The range of CFU/mL in the positive samples was measured as a continuous variable. We calculated descriptive statistics of bottle characteristics and feeding and hygiene practices, and explored their associations with bottle contamination through chi-squared tests for significance; Fisher’s exact test was also used when the number of items in any group was less than five. Rates of contamination in the bottle and hand samples were compared using McNemar’s test.
Qualitative data analysis.
Native Spanish speakers transcribed the audio recordings of the textual data collected through Phase 1’s questionnaire and Phase 3’s home visits verbatim. The first author coded the transcripts directly from Spanish by hand and analyzed them using directed content analysis, with a focus on factors affecting caregivers’ capacity to practice appropriate bottle disinfection.36 Starting with dimensions from the IBM-WASH ecological framework, the first author identified key concepts related to psychosocial, technological, and contextual factors which served as the initial codes.34 After reviewing and refining the coding scheme with two other members of the research team, the first author applied the codes to all transcripts and organized them into categories and eventually into broader themes.
Ethical approval.
The study protocol was approved by the institutional review boards from Johns Hopkins Bloomberg School of Public Health (Baltimore, MD) and Asociación Benéfica Proyectos en Informática, Salud, Medicina, y Agricultura (Lima, Peru). Written informed consent was obtained from all caregivers or from the infant’s grandmother if the mother was < 18 years old (n = 2).
RESULTS
We integrated findings from our three study phases to estimate bottle contamination, understand its contributing factors, and assess strategies for reducing such risks. In the following paragraph, we begin with an overview of participant sociodemographic characteristics. Next, we present the quantitative findings from Phase 1, including the microbiological results of bottle and hand samples, bottle characteristics, and practices related to bottle use and hygiene. We then present findings from Phase 2’s laboratory trial. Finally, we discuss our qualitative findings related to barriers to bottle disinfection (Phase 1) and factors influencing the uptake of improved practices (Phase 3), drawing on illustrative quotations when appropriate.
Participant characteristics.
Forty-eight caregivers provided samples and completed the questionnaire during the first phase of the study (Table 2). The majority (54.2%) of mothers had at least 12 years of formal education, and only one was illiterate. Nearly half of all mothers were younger than 25 years (range 14–41 years), and 44 (91.7%) infants were younger than 6 months (range 1–8 months). Nineteen participating households did not have a land title and, therefore, lived on property not formally recognized by the municipality, yet most households had reasonable living conditions with access to piped drinking water, a flush toilet, and a cement or provisional cement floor. Piped water was generally regarded as unsafe for drinking, and all households reported boiling water before drinking or using for food preparation.
Table 2.
Sociodemographic characteristics of participants in Phases 1 and 3
| Phase 1: sample collection and questionnaire (N = 48), N (%) | Phase 3: behavioral trial (N = 14), N (%) | |
|---|---|---|
| Maternal age (years) | ||
| < 25 | 23 (47.9) | 7 (50.0) |
| 25–29 | 8 (16.7) | 2 (14.3) |
| 30–34 | 10 (20.8) | 2 (14.3) |
| > 34 | 7 (14.6) | 3 (21.4) |
| Maternal educational attainment | ||
| Complete superior (> 12 years) | 2 (4.2) | 1 (7.1) |
| Complete secondary school (12 years) | 24 (50.0) | 4 (28.6) |
| Incomplete secondary school (6–11 years) | 17 (35.4) | 6 (42.9) |
| Incomplete primary school (< 6 years) | 5 (10.4) | 3 (21.4) |
| Age of infants (months) | ||
| < 2 months | 13 (27.1) | 1 (7.1) |
| 3–6 months | 31 (64.6) | 12 (85.7) |
| > 6 months | 4 (8.3) | 1 (7.1) |
| Property ownership | ||
| With land title | 29 (60.4) | 4 (28.6) |
| Without land title | 19 (39.6) | 10 (71.4) |
| Main source of drinking water | ||
| Piped connection to dwelling | 35 (72.9) | 7 (50.0) |
| Public tap | 7 (14.6) | 4 (21.4) |
| Provisional piped connection | 5 (10.4) | 3 (28.6) |
| Tanker truck | 1 (2.1) | 0 (0) |
| Toilet | ||
| Flush toilet | 37 (77.1) | 9 (64.3) |
| Latrine | 8 (16.7) | 2 (14.3) |
| Provisional flush toilet | 2 (4.2) | 2 (14.3) |
| No toilet in home | 1 (2.1) | 1 (7.1) |
| Floor material | ||
| Dirt/sand | 4 (8.3) | 1 (7.1) |
| Provisional cement | 17 (35.4) | 6 (42.9) |
| Cement | 23 (47.9) | 6 (42.9) |
| Wood | 4 (8.3) | 1 (7.1) |
| Refrigerator in home | ||
| Yes | 33 (68.8) | 7 (50.0) |
| No | 15 (31.3) | 7 (50.0) |
Sociodemographic characteristics of the caregivers recruited for the TIPs were overall similar to the larger group, yet the TIPs participants had slightly lower maternal education and a greater proportion did not have a land title (Table 2).
Bacterial contamination of bottle and hand samples.
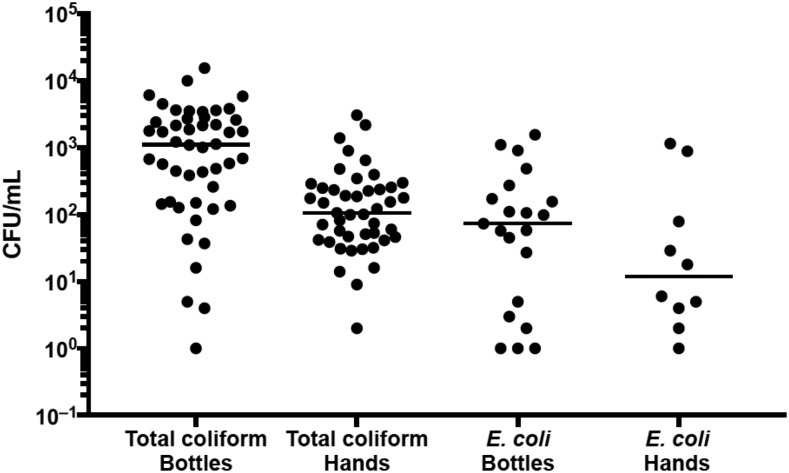
Total coliform was detected from all 48 bottle samples collected and from 45/46 (97.8%) of the hand samples collected (two participants declined to provide hand samples) (Table 3). As shown in Figure 2, the median total coliform count in positive bottle samples was 1.1 × 103 CFU/mL with a range of 1–1.5 × 104 CFU/mL. The median total coliform count in positive hand samples was 1.1 × 102 CFU/mL with a range of 2–3.1 × 103 CFU/mL. Escherichia coli was detected in 21 (43.8%) of 48 bottle samples and 10 (21.7%) of the 46 hand samples. The median E. coli in positive bottle samples was 7.3 × 101 CFU/mL with a range of 1–1.6 × 103 CFU/mL (Table 3). The median E. coli count in positive hand samples was 1.2 × 101 CFU/mL with a range of 1–1.2 × 103 CFU/mL. Bottles were significantly more contaminated than hands (P = 0.0075). Bottle-rinse colony counts were positively associated with hand-rinse colony counts in the same household (Spearman ρ = 0.42, P = 0.004).
Table 3.
Total coliform and Escherichia coli contamination in bottle and hand samples
| Bottles (N = 48), N (%) | Hands (N = 46), N (%) | |
|---|---|---|
| Total coliform | ||
| Negative | 0 | 1 (2.2) |
| Positive | 48 (100.0) | 45 (97.8) |
| Escherichia coli | ||
| Negative | 27 (56.3) | 36 (78.3) |
| Positive | 21 (43.8) | 10 (21.7) |
Figure 2.
Counts of total coliform and Escherichia coli colony-forming unit/mL in positive bottle and hand samples.
Bottle characteristics, usage, and hygiene practices.
Of the 48 participating households, 34 (70.8%) had a single bottle that was used continuously throughout the day. Thirty-six bottles (75.0%) had a cap at the time of sampling. Thirty (62.5%) were made of plastic, whereas 18 (37.5%) were glass. Most bottles (70.8%) were prepared by the infant’s mother, but other bottle handlers included the father, grandparents, and older children (Table 4). The number of times the bottle was prepared each day ranged from 1 to 15, with most caregivers (54.2%) preparing the bottle three to six times per day. This variation was likely due to the differing rates of mixed and partial breastfeeding among mothers and the handling of leftover feeds: Although 28 (58.3%) mothers reported that they discarded of leftover liquid feeds, 15 (31.3%) mothers kept them to be given to the infant later. Only five (10.4%) caregivers reported storing leftover feeds in the refrigerator (Table 4). Of 48 caregivers, 41 (85.4%) fed their infants formula, whereas seven (14.6%) used cow’s milk; nearly all of these products were sold as dehydrated powder.
Table 4.
Bottle characteristics, usage, and bottle hygiene practices (N = 48)
| N (%) | |
|---|---|
| Number of bottles in home | |
| 1 | 34 (70.8) |
| 2 | 12 (25.0) |
| 3 | 2 (4.2) |
| Bottle material | |
| Plastic | 30 (62.5) |
| Glass | 18 (37.5) |
| Bottle cap | |
| Yes | 36 (75.0) |
| No | 12 (25.0) |
| Bottle handler | |
| Mother | 34 (70.8) |
| Father | 5 (10.4) |
| Grandmother/grandfather | 5 (10.4) |
| Other child in home | 4 (8.3) |
| Average number of times bottle is prepared each day | |
| 1–2 | 10 (20.8) |
| 3–6 | 26 (54.2) |
| > 6 | 12 (25.0) |
| Handling of leftover feeds | |
| Discarded | 28 (58.3) |
| Stored at ambient temperature | 10 (20.8) |
| Stored in refrigerator | 5 (10.4) |
| Consumed by mother or another child | 5 (10.4) |
| Bottle contents | |
| Infant formula | 41 (85.4) |
| Cow’s milk | 7 (14.6) |
| Use of detergent to clean bottle | |
| No | 23 (47.9) |
| Yes | 25 (52.1) |
| Use of bottle brush to clean bottle | |
| No | 33 (68.8) |
| Brush with only water | 9 (18.8) |
| Brush with detergent | 6 (12.5) |
| Boiling bottle | |
| Never | 28 (58.3) |
| Less than daily basis | 9 (18.8) |
| Daily basis | 11 (22.9) |
According to caregiver self-report, the most common disinfection method was washing the bottle with dish detergent as slightly more than half (52.1%) of caregivers reported doing this regularly. Of those, six (12.5%) reported scrubbing the interior of the bottle with detergent and a bottle brush; another nine (18.8%) caregivers used a brush without detergent. Only 11 (22.9%) caregivers reported boiling their bottles on a daily basis. The majority of caregivers (58.3%) never boiled bottles (Table 4). High rates of fecal contamination were observed in bottles that were reportedly disinfected, including detergent use and daily boiling. Overall, we did not find any statistically significant associations between self-reported bottle disinfection and fecal contamination (Table 5). Additional covariates assessed, including bottle characteristics described in Table 4, also failed to demonstrate significant associations.
Table 5.
Bottle hygiene practices and Escherichia coli contamination of bottles
| Escherichia coli colonies not present (N = 27), N (%)† | Escherichia coli colonies present (N = 21), N (%)† | P-value* | |
|---|---|---|---|
| Use of detergent | 0.230 | ||
| No | 15 (65.2) | 8 (34.8) | |
| Yes | 12 (48.0) | 13 (52.0) | |
| Use of brush | 0.651 | ||
| No | 20 (60.6) | 13 (39.4) | |
| Brush with only water | 4 (44.4) | 5 (55.6) | |
| Brush with detergent | 3 (50.0) | 3 (50.0) | |
| Boiling | 0.082 | ||
| Never | 13 (46.4) | 15 (53.6) | |
| Less than daily basis | 8 (88.9) | 1 (11.1) | |
| Daily basis | 6 (54.6) | 5 (45.4) |
* Chi-squared or Fisher’s exact test.
† Parentheses are row percentages.
Trial of cleaning practices under controlled conditions.
Laboratory results indicated that the baseline contamination level after exposure to the E. coli solution was an average of 1.98 × 103 CFU/100 mL (SD: 302.4). As anticipated, the average reductions in E. coli increased as cleaning methods became more intensive in all six replicates of the trial. The only methods capable of reducing contamination levels to < 5 CFU/100 mL were brushing with water and detergent for 30 seconds and 60 seconds, which yielded an average of 2.3 (SD: 1.7) and 1 (SD: 2) CFU/100 mL, respectively. Given that the bacterial reductions from these two methods were nearly equivalent, the shorter duration was selected as the second improved practice to minimize the required time commitment for caregivers. For these reasons, “brush with Ayudin for 30 seconds after every use” was the second improved practice recommended to caregivers during the TIPs in Phase 3.
Identified barriers to optimal bottle disinfection.
Narratives that emerged during the administration of the Phase 1 questionnaire provided insight into obstacles to optimal bottle hygiene. Although caregivers expressed understandings consistent with the germ theory of disease, probing revealed a lack of understanding of the specific steps necessary for disinfection. For example, several caregivers described “boiling” a bottle as placing it in a bowl of hot water, rather than leaving it on the stove at a rolling boil for several minutes, as recommended by the WHO.33
The nutritionist told me that we have to boil the bottle…I do boil it, it’s quick—if I see that the water is boiling, I toss it in my bowl, I put [the bottle] in the boiled water, and right there the germs are killed.
(33-year-old mother with incomplete secondary school education; 6-month-old child)
Some participants reported submerging the entire bottle with the nipple attached into a bowl or pot to “boil,” whereas a number of other caregivers perceived rinsing the bottle with boiled water as adequate for purposes of disinfection.
Right when the water is boiling in the teapot, I take a bit out, and I start rinsing, washing everything…I rinse it with hot, boiled water to kill the germs—I’ve even burned my hand a few times!
(20-year-old mother with complete secondary school education; 7-month-old child)
Ownership of glass bottles generated additional barriers to appropriate bottle disinfection. Several caregivers worried that the glass bottle would crack if it were placed in boiling or hot water and chose not to take this risk because replacing it would be prohibitively expensive.
In addition, perceptions of detergent interfered with its effective use. Some caregivers avoided detergent because they viewed it as potentially harmful for an infant, as one 24-year-old mother stated, “[Detergent] leaves a smell and it’s strong. If a tiny little bit remains, then it can harm the baby’s stomach.” Others believed that using a brush to scrub the bottle interior obviated the need for detergent.
Health providers’ advice surrounding bottle hygiene.
Most caregivers did not receive any information or guidance regarding bottle cleaning from health providers, despite the fact that they often discussed infant feeding practices after delivery and during postnatal care visits. Out of 48, 29 (60.42%) caregivers had discussed formula use with an obstetrician or pediatrician, yet only eight (16.67%) had ever received information about bottle hygiene. Some caregivers received advice related to purchasing choices, such as to buy glass bottles instead of plastic and to regularly replace bottles and nipples. One caregiver recalled that “The nurse in the hospital told me that you always have to change the bottles—they should be changed after at most three months,” yet found it difficult to adhere to this suggestion given her household’s socioeconomic instability.
More commonly, nurses advised mothers to avoid bottles altogether and to spoon-feed their infants or use a cup instead. Yet, mothers generally did not heed these recommendations, citing how bottle-feeding saved time and helped infants consume greater volumes of formula. As one 41-year-old mother said of her 8-month-old son, “With the cup he gets desperate and he spills on himself…the quickest for me is the bottle.”
Uptake of practices recommended during the TIPs.
Fourteen caregivers were selected for participation in the TIPs based on the detection of E. coli in their bottles during Phase 1 (median of 42.4 CFU/mL). Eleven TIPs participants were mothers, one was a father, and two were grandmothers. During the first round of household visits, the boiling practice was assigned to six caregivers and the brushing practice was assigned to eight. During the follow-up visits, all caregivers who received the recommendation to brush the bottle with Ayudin implemented this practice at home, yet two did so less frequently than recommended. Three of six caregivers reported adhering to the recommendation of boiling the bottle on a daily basis (one stopped boiling altogether and two modified the frequency and duration).
Caregivers generally expressed enthusiasm for the improved practices. All but two of the caregivers reported noting a difference in the appearance of the bottle after implementing the new disinfection methods; remarks included “it looked shiny, like it was new” and “it looks cleaner now, more hygienic.” Most caregivers reported sharing the recommendation with their partners, mothers, and other household members. Thirteen of 14 caregivers said they would plan to continue the recommended practice in the future.
Facilitators and challenges surrounding behavior change.
The IBM-WASH framework guided the identification of factors that influenced caregivers’ capacity to implement the improved practices. Within the technology dimension, caregivers were impressed with the relative convenience and ease of use of the brush.
It helps me because it’s quick. I could get everything out, even from the little nipple. Before, with the sponge, nothing would come out—I spent so much time trying to get everything out with the sponge!
(13-year old mother with incomplete primary school education; 4-month-old child)
By contrast, boiling was more time-consuming and less convenient and was associated with higher perceived costs because of the gas required for the stoves. For example, a 41-year-old caregiver attempted to boil her bottle by burning wood outdoors to conserve her tank of gas, explaining “Boiling every single day is a big expense, and we’re stretched for money these days.” When this proved too difficult, she decided to clean her bottle with bleach instead of boiling it.
In addition to technology-related factors, boiling bottles was also restricted by contextual factors such as the division of labor within the household. Given that mothers were often responsible for all household tasks, it was challenging to set aside 10–15 minutes to put water to boil and boil the bottle thoroughly, as was recommended for the TIPs.
Sometimes I lose track of time and I don’t do it…I think it’s possible to do but sometimes I forget, or sometimes I’m cooking, and I have to tend to the clothes, or I hear them crying, and I go running—that’s why.
(23-year-old mother with complete secondary school education; 5-month-old child)
During the follow-up interviews, caregivers shared how several aspects of the initial TIPs visits had motivated them to try out the improved practices. Receiving the results of the bottle testing heightened the “perceived threat” of dirty bottles, as described within the psychosocial domain of IBM-WASH. Caregivers were often surprised and dismayed when the nurse-field worker informed them that “germs that cause diarrhea” had been found inside their bottle. During the second visit, when asked about their reasons for implementing the new practices, the majority (9/14) mentioned their desire to prevent their child from having contact with germs or getting sick.
In addition, caregivers commonly mentioned the value of the TIPs demonstrations for both boiling and brushing as they clarified all steps in the process and corrected previous misconceptions. A particularly important aspect of the brushing demonstrations involved the bottle rinse at the end, during which the nurse-field worker showed how rinsing thoroughly two times would wash away all of the remaining detergent. This helped to alleviate concerns about detergent harming the infant, and two caregivers even developed their own strategy of smelling the bottle after rinsing to ensure that the detergent’s odor was gone.
DISCUSSION
Bottles for feeding formula or milk to infants in shantytown communities of Lima are important transmission routes for enteric pathogens because of inappropriate disinfection practices. Our first study phase revealed that bottles were highly contaminated with fecal bacteria at rates that were comparable with those found in previous studies.20,21,23 Importantly, rates of contamination in our population were far greater in bottles than in caregiver hands (43.8% and 21.7%, respectively). These findings align with the extensive evidence base for the dangers of bottle-feeding infants in low-resource settings, which include greater susceptibility to respiratory and enteric infections during childhood.37–40
The high levels of fecal contamination detected in the bottles may be attributable to biofilm formation on the interior walls of the bottles. Caregivers’ remarks at the shiny appearance of their bottles following execution of the TIPs recommendations suggest that macroscopic biofilm layers may have emerged in the absence of adequate cleaning practices. Many types of bacteria, including E. coli, have been found to thrive in biofilm communities, which tend to form at solid–liquid interfaces and are enclosed in an extracellular matrix.41,42 Given their structural integrity, biofilm-associated cells cannot be removed by gentle rinsing, and, therefore, may play a role in the need for more intensive disinfection methods to maintain clean bottles.41
Our data suggest several aspects of bottle use, which create risks for bacterial contamination. Because of socioeconomic constraints, most households use plastic bottles, which have been shown to harbor greater quantities of formula residue after a feeding as compared with glass bottles.43 The tendency to store prepared feeds for several hours and then re-use them, rather than discard costly formula, likely facilitates further bacterial outgrowth. Finally, the fact that most households have only one bottle may increase the need for their continuous use and decrease opportunities for thorough cleaning between feeds.
Once bottles have become contaminated, suboptimal cleaning practices preclude disinfection before their subsequent use. Data collected from Phase 1 highlight incomplete understandings of how to adequately disinfect bottles, which may explain the absence of significant associations between bottle contamination and hygiene practices. For example, although we might have expected that bottles boiled on a daily basis would be significantly less contaminated than those never boiled, we found that caregivers’ interpretation of “boiling” was to leave the bottle in a bowl of water that had been boiled in a kettle. This action differs greatly from what is recommended for the purposes of disinfection, and evidence suggests that several strains of pathogenic bacteria remain viable at a temperature below 65°C.44
These misconceptions may be related to the lack of communication surrounding appropriate bottle hygiene during their interactions with health providers. Recommendations that participants received from providers related to purchasing glass bottles or replacing bottle-feeding with spoon-feeding often proved difficult to implement and did not equip caregivers with the skills necessary to adequately disinfect the bottles. Postnatal and well-baby visits may represent an opportunity for health providers to discuss feasible bottle-cleaning methods with caregivers that have already decided to give formula or cow’s milk to their infants using bottles.
To our knowledge, this is the first study to develop and assess strategies for a bottle hygiene intervention based on a context-specific understanding of existing practices and their behavioral determinants. Theoretical frameworks such as IBM-WASH have underscored the importance of “enabling products” to encourage behavior change.34,45 Previous studies of bottle contamination at the community level have tended to focus on the need for health education and attitude shifts to improve practices,16,22 whereas other studies have exclusively examined the efficacy and efficiency of cleaning products in a controlled laboratory setting.43,46,47 Our study adds to this literature by using a TIPs to examine participants’ experiences with and perceptions of different technologies in a field setting. Specifically, we found the nylon-bristle bottle brush to have several advantageous attributes highlighted in the technology domain of IBM-WASH: it is easy to use, efficient, locally commercially available, and inexpensive (1 Peruvian sol or approximately 0.30 USD).
By comparison, when caregivers boiled their bottles, they often did so inadequately, and others found it overly costly and time-consuming to adhere to the suggested duration of boiling for several minutes. This finding reflects the conclusions of several other studies demonstrating the impracticality of boiling water in low-resource settings because of economic and indirect (time) costs.48–51 Furthermore, boiling introduces the additional risk of burns; several studies conducted in peri-urban Lima have identified scalding as the primary cause of burns in young children, with poverty and household crowding exacerbating such risks.52,53 For these reasons, although our controlled trial indicated that the use of a bottle brush and detergent did not eliminate 100% of the bacterial contamination, the advantages of this practice over the alternative disinfection procedure of boiling are substantial.
Our data also highlight key factors for adoption of improved bottle hygiene practices. After learning the results of their bottle testing, most caregivers cited their new awareness of this threat as motivation to try out the recommended practices. This indicates the value of increasing one’s “perceived susceptibility”—a theoretical construct identified by the Health Belief Model as necessary for successful behavior change.54,55 In addition, the social learning that occurred from the demonstrations provided during the initial household visit likely strengthened caregivers’ self-efficacy to practice bottle hygiene, although reducing the “perceived barriers” to such practices.54,56 Future interventions that address these behavioral determinants may prove more effective in promoting adoption of bottle hygiene behaviors.
This study was limited by several factors. First, data on bottle-feeding and bottle-cleaning practices during Phase 1 were collected via self-report rather than direct observations and, therefore, may have been subject to social desirability bias.57 Nevertheless, we triangulated both quantitative and qualitative methods to assess existing practices and facilitate an in-depth understanding of the most pertinent barriers to bottle disinfection that merit consideration during intervention development. The incorporation of formative research methods allowed for important insights into the uptake of recommended practices that leverage locally available resources. However, the short duration of the TIPs (one initial visit plus one follow-up visit) means that it cannot speak to the potential for long-term adoption. This will need to be determined through more extensive trials in the future. Finally, our study’s sample size was relatively small, and it is possible that a larger sample would allow for the observation of statistically significant associations between bottle contamination and hygiene practices.
Ultimately, the high rates of bottle contamination revealed by our study reinforce the importance of continuing to dedicate ample health sector resources toward the promotion of exclusive breastfeeding and regulations on the marketing of breast milk substitutes.58,59 Meanwhile, as upward trends of formula use in peri-urban settings continue to increase infants’ exposure to risks associated with dirty bottles, there may be a need for open discussion of bottle hygiene measures that are feasible and acceptable to caregivers. Future research should assess the effectiveness of promoting the use of a brush and detergent by testing E. coli levels in bottles before and after field implementation. In addition, further qualitative research may inform the specific messaging and delivery mechanisms for recommendations on bottle hygiene adapted to the local context.
Acknowledgments:
We gratefully acknowledge the study participants of Villa El Salvador for their engagement and sharing of experiences which made this research possible, and we thank members of the field team, including Nelly M. Briceño, Flor de Maria Pizarro, Mercedes Margarita Escobar, Blanca I. Delgado, Cristel M. Lizarraga, Leyda Murga, Erika M. Falcon, Cynthia Arriaga Diaz, Brigida Rosario Jimenez, and Omar Cabrera for their assistance and feedback during data collection, and Marco Varela, Giovanna Vivanco, Roxy K. Malasquez, and Pilar K. Sanchez for their assistance with data entry and management. We also acknowledge Francesca Schiaffino for her input on study design and methods and Maya P. Ochoa and Guillermo S. Rodríguez for their assistance with laboratory work.
REFERENCES
- 1.Katona P, Katona-Apte J, 2008. The interaction between nutrition and infection. Clin Infect Dis 46: 1582–1588. [DOI] [PubMed] [Google Scholar]
- 2.Dewey KG, Mayers DR, 2011. Early child growth: how do nutrition and infection interact? Matern Child Nutr 7 (Suppl 3): 129–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kar BR, Rao SL, Chandramouli BA, 2008. Cognitive development in children with chronic protein energy malnutrition. Behav Brain Funct 4: 31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkman DS, Lescano AG, Gilman RH, Lopez SL, Black MM, 2002. Effects of stunting, diarrhoeal disease, and parasitic infection during infancy on cognition in late childhood: a follow-up study. Lancet 359: 564–571. [DOI] [PubMed] [Google Scholar]
- 5.Dewey KG, Begum K, 2011. Long-term consequences of stunting in early life. Matern Child Nutr 7 (Suppl 3): 5–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, Sachdev HS; Maternal, Child Undernutrition Study Group , 2008. Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371: 340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoddinott J, Maluccio JA, Behrman JR, Flores R, Martorell R, 2008. Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet 371: 411–416. [DOI] [PubMed] [Google Scholar]
- 8.Martorell R, Melgar P, Maluccio JA, Stein AD, Rivera JA, 2010. The nutrition intervention improved adult human capital and economic productivity. J Nutr 140: 411–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.INEI , 2015. Peru: Encuesta Demográfica y de Salud Familiar 2014. Lima, Peru: Instituto Nacional de Estadística e Informática. [Google Scholar]
- 10.Behar M, 1975. The role of feeding and nutrition in the pathogeny and prevention of diarrheic processes. Bull Pan Am Health Organ 9: 1–9. [PubMed] [Google Scholar]
- 11.Bullen CL, Willis AT, 1971. Resistance of the breast-fed infant to gastroenteritis. Br Med J 3: 338–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cushing AH, Anderson L, 1982. Diarrhea in breast-fed and non-breast-fed infants. Pediatrics 70: 921–925. [PubMed] [Google Scholar]
- 13.Lu R, Costello A, 2000. Failure to exclusively breastfeed and the risk of early infant mortality due to infectious disease in poor communities in Lima, Peru. J Trop Pediatr 46: 309–311. [DOI] [PubMed] [Google Scholar]
- 14.Surjono D, Ismadi SD, Suwardji, Rohde JE, 1980. Bacterial contamination and dilution of milk in infant feeding bottles. J Trop Pediatr 26: 58–61. [DOI] [PubMed] [Google Scholar]
- 15.Andresen E, Rollins NC, Sturm AW, Conana N, Greiner T, 2007. Bacterial contamination and over-dilution of commercial infant formula prepared by HIV-infected mothers in a Prevention of Mother-to-Child Transmission (PMTCT) Programme, South Africa. J Trop Pediatr 53: 409–414. [DOI] [PubMed] [Google Scholar]
- 16.Morais TB, Morais MB, Sigulem DM, 1998. Bacterial contamination of the lacteal contents of feeding bottles in metropolitan Sao Paulo, Brazil. Bull World Health Organ 76: 173–181. [PMC free article] [PubMed] [Google Scholar]
- 17.Imong SM, Jackson DA, Rungruengthanakit K, Wongsawasdii L, Amatayakul K, Drewett RF, Baum JD, 1995. Maternal behaviour and socio-economic influences on the bacterial content of infant weaning foods in rural northern Thailand. J Trop Pediatr 41: 234–240. [DOI] [PubMed] [Google Scholar]
- 18.Suthienkul O, Siripanichgon K, Promachot P, Echeverria P, Lexsomboon U, Rakue Y, 1999. Bacterial contamination of bottle milk in infants under 6 months in Children’s Hospital, Bangkok, Thailand. Southeast Asian J Trop Med Public Health 30: 770–775. [PubMed] [Google Scholar]
- 19.Gibson S, Sahanggamu D, Fatmaningrum D, Curtis V, White S, 2017. ‘Unfit for human consumption’: a study of the contamination of formula milk fed to young children in East Java, Indonesia. Trop Med Int Health. [DOI] [PubMed] [Google Scholar]
- 20.Cherian A, Lawande RV, 1985. Recovery of potential pathogens from feeding bottle contents and teats in Zaria, Nigeria. Trans R Soc Trop Med Hyg 79: 840–842. [DOI] [PubMed] [Google Scholar]
- 21.Elegbe IA, Ojofeitimi EO, Elegbe I, Akinola MO, 1982. Pathogenic bacteria isolated from infant feeding teats: contamination of teats used by illiterate and educated nursing mothers in Ile-Ife, Nigeria. Am J Dis Child 136: 672–674. [PubMed] [Google Scholar]
- 22.Anderson JA, Gatherer A, 1970. Hygiene of infant-feeding utensils. Practices and standards in the home. Br Med J 2: 20–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Redmond EC, Griffith CJ, Riley S, 2009. Contamination of bottles used for feeding reconstituted powdered infant formula and implications for public health. Perspect Public Health 129: 85–94. [DOI] [PubMed] [Google Scholar]
- 24.Black RE, Lopez de Romana G, Brown KH, Bravo N, Bazalar OG, Kanashiro HC, 1989. Incidence and etiology of infantile diarrhea and major routes of transmission in Huascar, Peru. Am J Epidemiol 129: 785–799. [DOI] [PubMed] [Google Scholar]
- 25.INEI , 2006. Peru: Encuesta Demográfica y de Salud Familiar. ENDES Continua 2004–2005. Informe Principal. Lima, Peru: Instituto Nacional de Estadística e Informática. [Google Scholar]
- 26.WHO , 2001. Global Strategy for Infant and Young Child Feeding. WHA54 A54/INF.DOC./4. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 27.INEI , 1988. Encuesta Demográfica y de Salud familiar (ENDES 1986). Informe General. Lima, Peru: Instituto Nacional de Estadística e Informática. [Google Scholar]
- 28.WHO , 2013. Protecting Breastfeeding in Peru. Geneva, Switzerland: World Health Organization. Available at: http://www.who.int/features/2013/peru_breastfeeding/en/. Accessed December 10, 2018. [Google Scholar]
- 29.INEI , 1992. Encuesta Demográfica y de Salud Familiar 1991/1992. Lima, Peru: Instituto Nacional de Estadística e Informática. [Google Scholar]
- 30.INEI , 2007. XI Censo de Población y VI de Vivienda. Lima, Peru: Instituto Nacional de Estadistica e Informatica. [Google Scholar]
- 31.Sandelowski M, 1995. Sample size in qualitative research. Res Nurs Health 18: 179–183. [DOI] [PubMed] [Google Scholar]
- 32.Doyle M, Erickson M, 2006. Closing the door on the fecal coliform assay. Microbe 1: 162–163. [Google Scholar]
- 33.WHO and Food and Agriculture Organization of the United Nations , 2007. Safe Preparation, Storage and Handling of Powdered Infant Formula: Guidelines. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 34.Dreibelbis R, Winch PJ, Leontsini E, Hulland KR, Ram PK, Unicomb L, Luby SP, 2013. The integrated behavioural model for water, sanitation, and hygiene: a systematic review of behavioural models and a framework for designing and evaluating behaviour change interventions in infrastructure-restricted settings. BMC Public Health 13: 1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dickin K, Griffiths M, 1997. Designing by Dialogue: A Program Planners’ Guide to Consultative Research for Improving Young Child Feeding. Washington, DC: Academy for Educational Development. [Google Scholar]
- 36.Hsieh HF, Shannon SE, 2005. Three approaches to qualitative content analysis. Qual Health Res 15: 1277–1288. [DOI] [PubMed] [Google Scholar]
- 37.Kim HY, Han Y, Pyun Y, Kim J, Ahn K, Lee SI, 2011. Prolonged bedtime bottle feeding and respiratory symptoms in infants. Asia Pac Allergy 1: 30–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Feachem RG, Koblinsky MA, 1984. Interventions for the control of diarrhoeal diseases among young children: promotion of breast-feeding. Bull World Health Organ 62: 271–291. [PMC free article] [PubMed] [Google Scholar]
- 39.Huttly SR, Morris SS, Pisani V, 1997. Prevention of diarrhoea in young children in developing countries. Bull World Health Organ 75: 163–174. [PMC free article] [PubMed] [Google Scholar]
- 40.Kramer MS, et al. 2001. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 285: 413–420. [DOI] [PubMed] [Google Scholar]
- 41.Donlan RM, 2002. Biofilms: microbial life on surfaces. Emerg Infect Dis 8: 881–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Watnick P, Kolter R, 2000. Biofilm, city of microbes. J Bacteriol 182: 2675–2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kuan WH, Chen YL, 2016. Bottle material and cleansing procedures of infant feeding bottles. Southeast Asian J Trop Med Public Health 47: 142–151. [PubMed] [Google Scholar]
- 44.Spinks AT, Dunstan RH, Harrison T, Coombes P, Kuczera G, 2006. Thermal inactivation of water-borne pathogenic and indicator bacteria at sub-boiling temperatures. Water Res 40: 1326–1332. [DOI] [PubMed] [Google Scholar]
- 45.Devine J, 2010. Beyond tippy-taps: the role of enabling products in scaling up and sustaining handwashing. Waterlines 29: 304. [Google Scholar]
- 46.Ma L, Zhang G, Swaminathan B, Doyle M, Bowen A, 2009. Efficacy of protocols for cleaning and disinfecting infant feeding bottles in less developed communities. Am J Trop Med Hyg 81: 132–139. [PubMed] [Google Scholar]
- 47.Redmond E, Griffith CJ, 2009. Disinfection methods used in decontamination of bottles used for feeding powdered infant formula. J Fam Health Care 19: 26–31. [PubMed] [Google Scholar]
- 48.Gilman RH, Skillicorn P, 1985. Boiling of drinking-water: can a fuel-scarce community afford it? Bull World Health Organ 63: 157–163. [PMC free article] [PubMed] [Google Scholar]
- 49.Clasen T, McLaughlin C, Nayaar N, Boisson S, Gupta R, Desai D, Shah N, 2008. Microbiological effectiveness and cost of disinfecting water by boiling in semi-urban India. Am J Trop Med Hyg 79: 407–413. [PubMed] [Google Scholar]
- 50.Oswald WE, Lescano AG, Bern C, Calderon MM, Cabrera L, Gilman RH, 2007. Fecal contamination of drinking water within peri-urban households, Lima, Peru. Am J Trop Med Hyg 77: 699–704. [PubMed] [Google Scholar]
- 51.Psutka R, Peletz R, Michelo S, Kelly P, Clasen T, 2011. Assessing the microbiological performance and potential cost of boiling drinking water in urban Zambia. Environ Sci Technol 45: 6095–6101. [DOI] [PubMed] [Google Scholar]
- 52.Delgado J, Ramirez-Cardich ME, Gilman RH, Lavarello R, Dahodwala N, Bazan A, Rodriguez V, Cama RI, Tovar M, Lescano A, 2002. Risk factors for burns in children: crowding, poverty, and poor maternal education. Inj Prev 8: 38–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Donroe J, Gilman RH, Brugge D, Mwamburi M, Moore DA, 2009. Falls, poisonings, burns, and road traffic injuries in urban Peruvian children and adolescents: a community based study. Inj Prev 15: 390–396. [DOI] [PubMed] [Google Scholar]
- 54.Rosenstock IM, Strecher VJ, Becker MH, 1988. Social learning theory and the health belief model. Health Educ Q 15: 175–183. [DOI] [PubMed] [Google Scholar]
- 55.Janz NK, Becker MH, 1984. The health belief model: a decade later. Health Educ Q 11: 1–47. [DOI] [PubMed] [Google Scholar]
- 56.Bandura A, 1977. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84: 191–215. [DOI] [PubMed] [Google Scholar]
- 57.Stanton BF, Clemens JD, Aziz KM, Rahman M, 1987. Twenty-four-hour recall, knowledge-attitude-practice questionnaires, and direct observations of sanitary practices: a comparative study. Bull World Health Organ 65: 217–222. [PMC free article] [PubMed] [Google Scholar]
- 58.WHO , 1981. International Code of Marketing of Breast-Milk Substitutes. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 59.WHO , 2014. Comprehensive Implementation Plan on Maternal, Infant and Young Child Nutrition. Geneva, Switzerland: World Health Organization. [DOI] [PMC free article] [PubMed] [Google Scholar]