Abstract.
In 2012, approximately 5.6 million Zambians did not have access to improved sanitation and around 2.1 million practiced open defecation. The Zambia Sanitation and Hygiene Program (ZSHP), featuring community-led total sanitation, began in November 2011 to increase the use of improved sanitation facilities and adopt positive hygiene practices. Using a pre- and post-design approach with a population-level survey, after 3 years of implementation, we evaluated the impact of ZSHP in randomly selected households in 50 standard enumeration areas (representing 26 of 65 program districts). We interviewed caregivers of children younger than 5 years old (1,204 and 1,170 female caregivers at baseline and end line, respectively) and inspected household toilet facilities and sites for washing hands. At end line, 80% of households had access to improved sanitation facilities versus 64.1% at baseline (prevalence ratio [PR] = 1.25; 95% CI: 1.18–1.31) and 14.1% did not have a toilet facility compared with 19.4% at baseline. At end line, 10.6% of households reported living in an open defecation-free certified village compared with 0.3% at baseline (PR = 32.0; 95% CI: 11.9–86.4). In addition, at end line, 33.4% of households had a specific place for washing hands and 61.4% of caregivers reported handwashing with a washing agent after defecation or before preparing food compared with 21.1% (PR = 1.59; 95% CI: 1.39–1.82) and 55.2% (PR = 1.11; 95% CI: 1.04–1.19) at baseline, respectively. Community-led total sanitation implementation in Zambia led to improvements in access to improved sanitation facilities, reduced open defecation, and better handwashing practices. There is however a need for enhanced investment in sanitation and hygiene promotion.
INTRODUCTION
Zambia was not able to reach the Millennium Development Goal (MDG) 7c for water and sanitation, that is, halving the proportion of people without sustainable access to safe drinking water and basic sanitation by 2015, despite creating a comprehensive policy environment to guide the development and management of sanitation and water sectors with specific policy measures, such as community-based approaches, promotion of appropriate technology, and capacity building.1 The Sustainable Development Goals (SDGs),2 also known as the global goals, are now complementing and improving on the goals initially outlined under the MDGs. Sustainable Development Goal 6, which builds on MDG 7, has as one of its targets achieving access to adequate and equitable sanitation and hygiene for all, and ending open defecation by 2030, while paying special attention to the needs of women and girls and those in vulnerable situations.
The people of Zambia have one of the lowest levels of access to sanitation and hygiene services on the African continent. The 2012 WHO/UNICEF Joint Monitoring Program Report indicated that approximately 5.6 million Zambians did not have access to improved sanitation and around 2.1 million practiced open defecation.3 In 2012, it was estimated that only 34% of rural inhabitants in Zambia had access to improved sanitation facilities as compared with 56% in urban areas.4 Zambia loses an estimated $194 million, equivalent to 1.3% of gross domestic product, every year because of poor sanitation.5
To address the high burden of sanitation- and hygiene-related morbidity and mortality, especially in rural areas, the Zambian government, through the Ministry of Local Government and Housing (now Ministry of Water Development, Sanitation, and Environmental Protection), in partnership with UNICEF, the U.K. Department for International Development, and other line ministries such as the Ministry of Health, Ministry of General Education, and Ministry of Chiefs and Traditional Affairs started implementing the Zambia Sanitation and Hygiene Program (ZSHP) in 2011.6 The purpose of the ZSHP has been to contribute to the achievement of the MDG 7c (and SDG 6) targets in Zambia, with an additional 3 million people consistently using improved sanitation facilities and adopting hygiene practices (e.g., handwashing with soap or ash). Zambia Sanitation and Hygiene Program features community-led total sanitation (CLTS) as its core activity, but it also comprises a package of activities, including supporting enabling environments, sanitation marketing, school-led total sanitation, and national behavior change communication. There was a major focus on institutional strengthening and accountability of the key line ministries.
Community-led total sanitation uses participatory methods to eliminate the practice of open defecation in rural communities and promote latrine construction. At the local level, selected villagers are trained to facilitate a process in communities, known as triggering.7 The triggering is designed to convince villages to form a sanitation committee, build (and use) their own latrines without subsidies, and improve their personal hygiene. Triggered villages are followed by facilitators until they attain open defecation-free (ODF) status and are formally certified. Sanitation marketing was given a top priority in the ZSHP because of its ability to build sustainable capacity of the private sector to increase the demand for sanitation products and services to support the building of low-cost latrines.8 A recent systematic review of the quality and impact of CLTS found that this intervention consistently resulted in latrine ownership and decreased open defection.9 However, latrine quality varied and there were inconsistent impacts on self-reported diarrhea prevalence. The review suggested that the evidence base is relatively weak for the effectiveness of this intervention and noted a need for further, high-quality research.
To assess the effects of the CLTS-oriented program on sanitation and hygiene practices, an impact evaluation was conducted, covering Phase I of the ZSHP. The objective was to measure the key performance, impact, outcome, and input indicators to track changes over time, and to examine and explain the extent the program has contributed to the observed impact, outcome, and input indicators. This article presents the effect of implementing CLTS on sanitation and hygiene indicators in populations targeted to benefit from this package of interventions.
METHODS
Design.
We used a pre- and post-intervention design. We measured study outcomes at baseline, allowed 36 months for program implementation to proceed, and then conducted end line measurements. The baseline survey was conducted in June to August 2013 and end line survey in June to August 2016. These months corresponded to the middle of the dry season in Zambia. A household population–level survey tool, adapted from standard relevant modules of the multiple indicator cluster survey and Demographic Health Survey, was the main data collection tool used to measure outcomes. The end line tool was slightly modified from the tool used in the baseline survey, by adding more details of the features of pit latrines with slabs in training data collectors, as requested by the UNICEF water, sanitation, and hygiene (WASH) team. Key stakeholders, especially UNICEF and the steering committee members, provided input in the design and development of the data collection tools.
Study site and population.
The study was conducted from selected standard enumeration areas (SEAs) from all the 65 districts in eight of the 10 provinces of Zambia where the ZSHP was being implemented. To avoid selecting urban districts, the impact evaluation did not include Lusaka and Copperbelt provinces because these included several urban and peri-urban districts. To have a more precise estimate of change in our study outcomes, data were collected from the same SEAs at baseline and end line. Female caregivers with children younger than 5 years old (0–59 months) who were permanent residents (living in the area for at least 6 months) in the study area (selected SEAs) were interviewed for the household survey.
Sample size and sampling.
The sample was designed to provide estimates of the proportion of households with children younger than the age of 5 years meeting WASH indicators for rural Zambia. The sample design did not have power to allow for any outcome to be studied in subgroup analyses. Our primary sampling unit (cluster) was the SEA. We chose to use SEAs because 1) they are approximately the same size, so each household would have a similar probability of being selected; 2) they are geographically defined, which allowed us to identify all the households within the borders of the sampling frame; and 3) they are a manageable size to survey, with only 130 households on average.
We estimated a sample size of 1,250 households in 50 clusters (SEAs) based on the following assumptions: 1) 50% of households meeting WASH indicators, 2) margin of error of ±4% with a 95% CI, 3) design effect of 1.7 based on a review of design effects from household surveys conducted in sub-Saharan Africa,10–12 and 4) 88% response rate of households and eligible individuals based on our previous work.
We selected the representative sample of 1,250 households using a two-stage design. We received a list of all SEAs for districts in the eight provinces where the program was being implemented from the Central Statistics Office (CSO). The SEA list included the number of households in each SEA. In the first stage of sampling, 50 SEAs were selected using systematic stratified sampling with probability proportion to size, with the SEAs stratified by province and district to ensure complete geographical coverage. In the second stage of sampling, because of the variable number of households in each SEA, we selected an average of 25 households (range 11–49) from each SEA proportionate to the number of households for each SEA. To minimize variation, we sampled households in the same SEAs for both the baseline and end line surveys, but we did not attempt to visit the same households at each time point. Household was defined as consisting of one or more people who live in the same dwelling and also share at meals or living accommodation, consistent with the CSO definition. The 50 SEAs selected were located in 26 of the 65 districts where the ZSHP was being implemented. We obtained maps of the selected SEAs from CSO. In each SEA, the data collectors identified the center of the SEA and spun a bottle to determine the direction to select the first house. They selected an integer “n” from 1 to 9 and selected the nth house along the ray as the first house. The next house selected was the one with the door nearest to the previous house. They continued until the number of survey participants for the SEA was achieved. In each house, the first household to be contacted was selected; and in each household if there were two caregivers, the older was selected.
Data collection.
Trained interviewers interviewed caregivers in their homes after obtaining informed consent in the participants’ local language. They explained the purpose and rationale of the study and informed the participants that they would not be paid for participating, they were not obliged to participate, and they could refuse to answer any question. They were assured of confidentiality regarding any information they provided. They were asked to sign, mark, or thumbprint the consent form, and offered a copy of the consent form. Participants were interviewed only after written informed consent was provided. No eligible caregiver refused to participate, and we did not have anyone refuse to respond after providing informed consent, although a few caregivers refused to respond to some questions.
Information collected included knowledge and good hygiene practices, household water treatment practices, understanding of the link between diseases and poor hygiene and sanitation, access to and use of improved sanitation, handwashing practices, source and storage of drinking water, and any barriers encountered in accessing these services (end line household survey, Supplemental Material). Sociodemographic characteristics of respondents and family were also collected. We asked about expenditure on the construction and maintenance of latrines and handwashing materials. Dates of latrine construction were also collected. We asked about sources of information on sanitation and hygiene, any contact with the program, and participation in program activities. In addition, toilet facilities for the household, water storage containers, and sites for washing hands were inspected. The data collectors used a pictorial guide to ascertain the type of sanitation facility during the end line survey. The data collectors also checked whether there was soap or ash available for handwashing.
To understand how the program was implemented, the study team held discussions with program implementers and reviewed relevant program documents, including annual, semi-annual, and annual reports; field progress and monitoring reports; reports of annual reviews by the funder; publications; and related documents. Open defecation-free and CLTS triggering status data were extracted from program documents.
Data collection quality control.
Data collectors were recruited from a pool of experienced field staff that our research team has used over the years to conduct similar field activities. They received a 5-day training to ensure that they had the appropriate training and skills necessary to the overall conduct of the study, safety of research subjects, and quality of the resulting data. We used three data collection teams: each team made up of three data collectors and a supervisor. During daily contact with the data collectors, the supervisor collected and checked forms to ensure that they were completed properly and there were no missing responses. The supervisor also made both scheduled and unscheduled visits to data collectors during interviews.
Data management.
The data collection tools were designed in TeleForms®. The Teleforms enabled handwritten text to be translated to computer-readable files, and data are then transferred into a Microsoft® Access 14 database. As Teleforms included a data verification system, there was no need for double data entry. The paper forms were scanned and imported as faxed forms into the computer, and all fields were verified through the TeleForms system. Data checking took place with verification of the Access database with the paper forms by the office-based data manager. Data cleaning involved logic checks, range, missing data, and missing form checks.
Data analysis.
Using data from the baseline and end line surveys, supplemented with data from implementing partners and government sources, we ascertained whether changes occurred during the project. Because sampling was population-proportional, sampling weights were not needed. We used SAS version 9.4 software (SAS Institute, Cary, NC). We used frequency counts for dichotomous outcomes and means and medians for continuous outcomes. The main outcome was household access to improved toilet facility, which is defined as toilet facility that separates the waste from human contact and includes flush toilets, ventilated improved pit latrines, traditional pit latrines with slab, and composting toilets.
To test the differences in outcome variables between pre- and post-intervention surveys to detect the impact and effect of the intervention, we used generalized estimating equation models using an exchangeable correlation matrix to calculate prevalence ratios (PRs) and 95% CI adjusting for clustering by SEA. Because we sampled from matched SEAs in the baseline and end line surveys at the same proportion, we treated the survey as a self-weighting sample.
Ethical approval.
Ethical approval was obtained from the Boston University Institutional Review Board (IRB) and a local Zambian IRB (Excellence in Research Ethics and Science [ERES] Converge), authorized to review and approve studies of this nature. We also received Zambian Ministry of Health approval. All consent forms were developed in accordance with the BU and ERES Converge IRB guidelines. Consent forms were translated into the major local languages spoken in the study districts (Bemba, Nyanja, and Tonga). These translations were validated and attested for their accuracy. Validation was performed by retranslating the consent forms in the local languages into English and certified by an expert who completed an attestation form.
RESULTS
Characteristics of respondents and households.
We interviewed 1,204 and 1,170 female caregivers of children aged 0–59 months in the baseline and end line household surveys, respectively. The characteristics of respondents and their households were similar in both surveys, although a higher proportion of respondents were older than 35 years (23.0% versus 18.5%; PR = 1.24, 95% CI: 1.06–1.46) and self-employed (10.2% versus 4.9%; PR = 2.07, 95% CI: 1.53–2.80), whereas slightly fewer male heads of households and a smaller proportion of farmers and households with fewer than four persons (14.1% versus 17.8%; PR = 0.79, 95% CI: 0.66–0.96) were observed in the end line survey compared with the baseline survey (Table 1). There was also lower use of adequate water treatment methods at end line relative to baseline. Most women interviewed were in the age group of 20–35 years, had at least primary education, and self-identified as farmers, and a little more than two-fifths were from Bemba or Tonga ethnic groups. The head of households was, in most cases, the husband or partner of the respondent, and about half of the households had a household size of four to six (Table 1).
Table 1.
Sociodemographic characteristics of respondents and households
| Characteristic | Baseline survey | End line survey | PR (95% CI)* |
|---|---|---|---|
| Number of households surveyed | 1,204 | 1,170 | |
| Age (years) | |||
| < 20 | 9.9% (116/1,173) | 9.1% (103/1,134) | 0.92 (0.71–1.18) |
| 20–35 | 71.6% (840/1,173) | 67.9% (770/1,134) | 0.95 (0.89–1.00) |
| > 35 | 18.5% (217/1,173) | 23.0% (261/1,134) | 1.24 (1.06–1.46) |
| Highest level of education | |||
| No education | 10.2% (123/1,204) | 10.8% (126/1,170) | 1.05 (0.83–1.33) |
| Primary | 67.4% (812/1,204) | 65.8% (770/1,170) | 0.98 (0.92–1.03) |
| Secondary | 21.8% (263/1,204) | 22.8% (267/1,170) | 1.04 (0.90–1.21) |
| College and higher | 0.5% (6/1,204) | 0.6% (7/1,170) | 1.20 (0.40–3.56) |
| Main occupation | |||
| Housewife | 3.2% (38/1,201) | 4.4% (52/1,169) | 1.40 (0.93–2.12) |
| Farmer | 87.1% (1,046/1,201) | 80.6% (942/1,169) | 0.93 (0.89–0.96) |
| Business/self-employed | 4.9% (59/1,201) | 10.2% (119/1,169) | 2.07 (1.53–2.80) |
| Civil servant | 0.6% (7/1,201) | 0.3% (4/1,169) | 0.59 (0.17–2.00) |
| Unemployed | 1.9% (23/1,201) | 1.6% (19/1,169) | 0.85 (0.46–1.55) |
| Others* | 2.3% (28/1,201) | 2.8% (33/1,169) | 1.21 (0.74–1.99) |
| Marital status | |||
| Single/not married | 9.1% (109/1,203) | 7.8% (91/1,169) | 0.86 (0.66–1.12) |
| Married | 82.0% (986/1,203) | 81.7% (955/1,169 | 0.99 (0.96–1.04) |
| Separated/divorced | 6.4% (77/1,203) | 6.7% (78/1,169) | 1.04 (0.77–1.41) |
| Widowed | 2.6% (31/1,203) | 3.8% (45/1,169) | 1.49 (0.95–2.34) |
| Ethnic group/tribe affiliation | |||
| Bemba | 27.1% (323/1,192) | 25.9% (302/1,167) | 0.96 (0.83–1.09) |
| Tonga | 17.4% (208/1,192) | 16.7% (195/1,167) | 0.96 (0.80–1.14) |
| Tumbuka | 6.8% (81/1,192) | 6.8% (79/1,167) | 0.99 (0.74–1.34) |
| Lozi | 4.2% (50/1,192) | 6.0% (70/1,167) | 1.43 (1.00–2.04) |
| Others | 44.5% (530/1,192) | 44.6% (521/1,167) | 1.00 (0.92–1.10) |
| Head of household | |||
| Respondent | 11.3% (136/1,203) | 13.4% (156/1,168) | 1.18 (0.95–1.47) |
| Husband/partner | 81.1% (976/1,203) | 77.3% (903/1,168) | 0.95 (0.91–0.99) |
| Female relative | 3.7% (45/1,203) | 5.0% (58/1,168) | 1.32 (0.90–1.94) |
| Male relative | 3.8% (46/1,203) | 4.4% (51/1,168) | 1.14 (0.77–1.69) |
| Household size (persons) | |||
| < 4 | 17.8% (214/1,204) | 14.1% (165/1,168) | 0.79 (0.66–0.96) |
| 4–6 | 47.3% (569/1,204) | 48.8% (570/1,168) | 1.03 (0.95–1.12) |
| > 6 | 35.0% (421/1,204) | 37.1% (433/1,168) | 1.06 (0.95–1.18) |
| Water sources | |||
| Improved (protected) water source | 34.7% (418/1,204) | 51.9% (607/1,170) | 1.50 (1.36–1.65) |
| Water treatment | |||
| Use adequate water treatment method | 32.3% (389/1,204) | 24.6% (288/1,170) | 0.76 (0.67–0.87) |
Prevalence ratios presented in bold are all significant at P < 0.05.
* Prevalence ratio (PR) was calculated as the ratio of end line to baseline.
Household use of sanitation facilities.
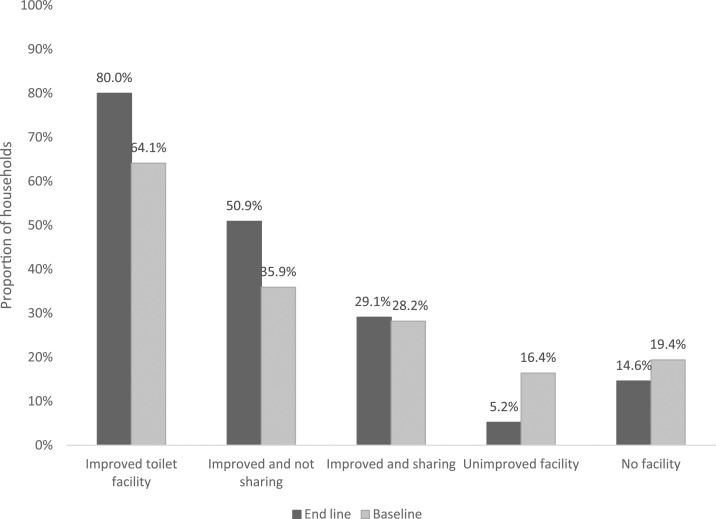
The most commonly used sanitation facility reported by households in both end line and baseline was a pit latrine with a slab, with coverage of 78.2% and 63.5%, respectively (Table 2). Fewer households in the end line survey (14.6%) reported not having a toilet facility than those in the baseline (19.4%). At end line, 80.0% (936/1,170) of households reported using an improved toilet facility as compared with 64.1% (772/1,204) in the baseline (Figure 1) (PR = 1.25, 95% CI: 1.19–1.31). A little more than half (50.7%; 595/1,170) of the households in the end line survey reported using an improved unshared toilet facility as compared with 35.9% (432/1,204) in the baseline survey (PR = 1.42; 95% CI: 1.29–1.56).
Table 2.
Household sanitation facilities at baseline and end line
| Characteristic | Baseline survey | End line survey | PR (95% CI)*† |
|---|---|---|---|
| Number of households surveyed | 1,204 | 1,170 | |
| Pit latrine with slab | 63.5% (765/1,204) | 78.2% (915/1,170) | 1.41 (1.33–1.49) |
| Ventilated improved pit latrine | 0.6% (7/1,204) | 1.6% (19/1,170) | 2.78 (1.18–6.67) |
| Flush/pour toilet | 0.0% (0/1,204) | 0.2% (2/1,170) | – |
| Pit latrine without slab | 16.4% (198/1,204) | 5.2% (61/1,170) | 0.32 (0.24–0.42) |
| No facility | 19.4% (234/1,204) | 14.6% (171/1,170) | 0.76 (0.63–0.90) |
Prevalence ratios presented in bold are all significant at P < 0.05.
* Clustered adjusted prevalence ratio (PR) and 95% confidence interval.
† Prevalence ratio was calculated as the ratio of end line to baseline.
Figure 1.
Household using improved sanitation facilities at baseline and end line.
Household defecation practices and status.
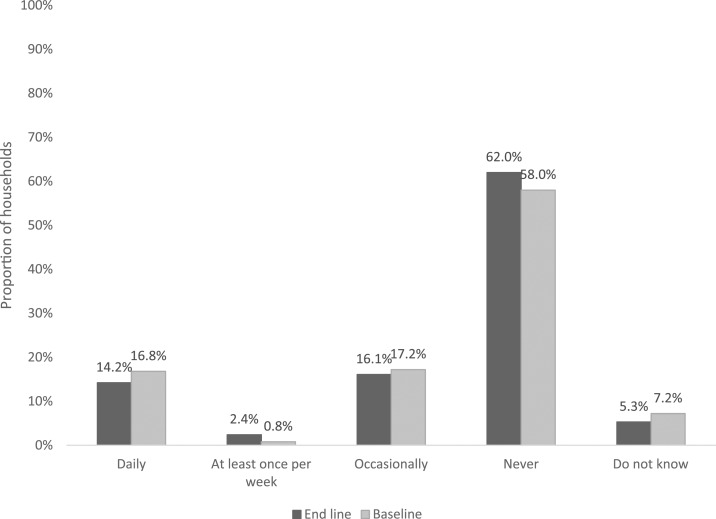
At end line, 62.0% of households responded that no member of their households had ever practiced open defecation compared with 58.0% at baseline (PR = 1.07; 95% CI: 1.00–1.14), and 14.2% of households in the end line survey as compared with 16.8% at baseline reported that a member of their households practiced open defecation on a daily basis (Figure 2). In the end line survey, 10.6% responded that they lived in an ODF-certified village as compared with 0.3% in the end line, a significant difference (PR = 32.0; 95% CI: 11.9–86.4). The program implementation data confirmed the ODF status of 832 households (of the 1,170 households surveyed during the end line survey), of which 83 representing 10.0% lived in an ODF-certified village. The ODF status as reported at end line (10.6%) was similar to the ODF status documented in the program data (10.0%).
Figure 2.
Household member practicing open defecation at baseline and end line.
Handwashing practices and knowledge.
The caregivers’ report of practicing washing hands before preparing food or after using the toilet was high in both the baseline and end line surveys (87.3% versus 94.0%; PR = 0.92; 95% CI: 0.90–0.95), but fewer caregivers reported washing hands with water and washing agents. For both handwashing and washing hands with water and washing agent, the proportion at end line was significantly higher than that at baseline (Table 3). The availability of having a specific place for washing hands and the presence of water and washing agent onsite were significantly higher at end line than those at baseline. The proportion of households with an improved unshared toilet facility with handwashing station with water and washing agent available was relatively low overall, although it was significantly higher at end line than at baseline (Table 3). Knowledge about critical times to wash hands and association between WASH practices and disease risk were similar at both baseline and end line.
Table 3.
Handwashing practices at baseline and end line
| Characteristic | Baseline survey | End line survey | PR (95% CI)*† |
|---|---|---|---|
| Number of households surveyed | 1,204 | 1,170 | |
| Reported washing hands before preparing food or after defecation | 87.3% (1,038/1,189) | 94.0% (1,092/1,162) | 1.09 (1.05–1.11) |
| Reported washing hands with water and washing agent | 55.2% (665/1,204) | 61.4% (718/1,170) | 1.11 (1.04–1.19) |
| Observed having specific place for washing hands | 21.1% (254/1,204) | 33.4% (391/1,170) | 1.59 (1.39–1.82) |
| Observed having place for washing hands near or close to the toilet area | 13.6% (164/1,204) | 20.7% (242/1,170) | 1.52 (1.27–1.82) |
| Observed specific place of washing hands has water and soap available | 13.3% (160/1,204) | 18.2% (213/1,170) | 1.39 (1.15–1.69) |
| Have improved unshared sanitation facility with handwashing facility with water and washing agent available | 5.4% (65/1,204) | 14.3% (167/1,170) | 2.70 (2.00–3.45) |
Prevalence ratios presented in bold are all significant at P < 0.05.
* Clustered adjusted prevalence ratio (PR) and 95% confidence interval.
† Prevalence ratio was calculated as the ratio of end line to baseline.
Triggering status and WASH outcomes.
Program implementation data confirmed the triggering status of 777 households (of the 1,170 households surveyed during the end line survey), of which 93, representing 12.0%, lived in a village that had not been triggered. Key WASH outcome indicators for households living in triggered villages to those living in non-triggered village were not significantly different with two exceptions—knowledge of at least four critical times to wash hands and recent handwashing with soap/detergent or ash, both of which were significantly higher in the triggered households (Table 4).
Table 4.
Water, sanitation, and hygiene outcomes by triggering status
| Indicator | Households in triggered villages (n = 684) | Households in non-triggered villages (n = 93) | Adjusted prevalence ratio (95% CI) |
|---|---|---|---|
| Improved toilet facility | 537 (78.5%) | 76 (81.7%) | 0.96 (0.87–1.07) |
| Improved toilet facility (not shared) | 323 (47.2%) | 59 (63.4%) | 0.75 (0.64–0.89) |
| No facilities—use bush or field | 113 (16.5%) | 15 (16.1%) | 1.03 (0.63–1.67) |
| Appropriate disposal of child feces* | 563 (87.3%) | 74 (87.1%) | 1.02 (0.93–1.12) |
| Household has specific place for washing hands | 245 (35.8%) | 29 (31.2%) | 1.11 (0.83–1.48) |
| Site for washing hands has water and soap/detergent or ash available | 132 (19.3%) | 11 (11.8%) | 1.64 (0.92–2.91) |
| Knowledge of all six critical times to wash hands | 43 (6.3%) | 1 (1.1%) | 5.91 (0.82–42.5) |
| Knowledge of at least four critical times to wash hands | 192 (28.1%) | 12 (12.9%) | 2.20 (1.28–3.78) |
| Recent handwashing with soap/detergent or ash | 473 (69.2%) | 44 (47.3%) | 1.47 (1.18–1.83) |
| Improved toilet facility and handwashing station with water and washing agent | 105 (15.4%) | 11 (11.8%) | 1.31 (0.73–2.34) |
Adjusted prevalence ratios presented in bold are all significant at P < 0.05.
*Child used toilet facility or child feces put/rinsed into toilet facility or child feces buried.
DISCUSSION
This impact evaluation of CLTS in rural Zambia demonstrated improvements in sanitation and hygiene measures between the baseline survey conducted in 2013 and the end line survey in 2016. Notable findings include a significant increase in the availability of improved sanitation, fewer households reporting open defecation, and improvements in handwashing with soap or ash and handwashing at critical times. However, overall knowledge of appropriate times to wash hands did not improve between the baseline and end line time periods, although two measures of handwashing were significantly higher in triggered households relative to those that were not triggered.
An increase in improved sanitation use and reductions in open defecation have been demonstrated in other African countries, including Ghana, Tanzania, and Mali, where CLTS interventions led to increased latrine coverage and use.13–15 In contrast to Mali, where CLTS resulted in roughly a doubling of the percentage of households with a private latrine,14 the ZSHP resulted in a smaller relative increase in this parameter, although this change was similar to that in the studies conducted in Ghana and Tanzania. Similarly, the Mali study found a larger decrease in reported open defecation at end line (about 24 percentage points) relative to the small change in this important sanitation parameter in Zambia (four percentage points). By contrast, an evaluation in Ethiopia that compared conventional CLTS facilitated by health workers and local leaders, as was performed in the Zambia program, with CLTS led by teachers, found that conventional CLTS resulted in greater reductions in open defecation (decrease of 15 percentage points), although there was no change in improved sanitation.16 In Indonesia, CLTS combined with sanitation marketing has also resulted in increased latrine ownership and reduced open defecation (six percentage points lower).17 By contrast, combining CLTS with subsidies proved more effective than community motivation alone for increasing latrine ownership in rural Bangladesh.18 Differences in baseline ODF status, timing of data collection in relation to programmatic interventions, variations in how the CLTS programs were implemented, and local sociocultural differences are likely to account for the differential impact of these different sanitation programs on ODF.
Like the Tanzanian and Indonesian studies, sanitation marketing, which developed the capacity of private sector players such as artisans to provide sanitation services that fulfilled the need for stronger longer lasting toilets at affordable prices, contributed to increased latrine coverage and use.13,17 A recent meta-analysis found that CLTS was one of a handful of sanitation interventions, along with latrine subsidy/provision interventions, sewage interventions, and sanitation education interventions that had the greatest impact on latrine use and coverage.19
There appeared to be knowledge sharing in the implementation of the project. Households living in villages that had not been triggered had similar access to improved sanitation facilities to those in triggered villages, as well as regional interventions like collaboration with local chiefs. Spillover of the intervention into nearby untriggered villages is an important potential collateral benefit because this and similar programs may not have to trigger all villages, as nearby untriggered villages may be motivated to organize themselves to ensure that they use improved toilets; this may help with program sustainability.
One of the CLTS goals is to eliminate the practice of open defecation in rural communities.20,21 Although the impact of the ZSHP on open defecation practice and status was lower than anticipated, there were significant improvements in ODF status and practices at end line compared with baseline. There were many more households at end line whose members did not practice open defecation and lived in ODF-certified villages. It has been noted that even when high latrine coverage levels are achieved, open defecation is often still practiced. Users may still choose to openly defecate, and that decision is likely influenced by a number of social, cultural, and behavioral factors, such as opportunity to leave the house and socialize with community members.22
This WASH strategy has the potential to reduce problems associated with open defecation, which threaten human health, including sanitation-related diseases such as cholera, dysentery, and typhoid, and the spread of zoonotic parasites such as helminths, and their contributions to childhood malnutrition and stunting.23,24 Community-led total sanitation interventions have had mixed effects on the prevalence of diarrhea and other health outcomes, with some studies showing reductions in self-reported diarrhea prevalence but others showing no change.9
There was a significant increase in the proportion of caregivers who reported washing hands before preparing food or after defecation. Not using soap or ash decreases the effectiveness of handwashing, which leads to the recommendation to put more emphasis of the program on using detergent. Knowledge around handwashing did not increase between baseline and end line in this evaluation. However, about a third of those who reported washing their hands did not wash with water and washing agent. Despite the likely positive health benefits of handwashing, it is poorly practiced in Zambia and globally.25 If the bottleneck was not knowledge in Zambia, the causes for a limited increase in handwashing require further investigation. There are a number of different contextual and psychosocial factors that can have an influence on handwashing practices. A study in Burundi found that household wealth, amount of water per person, and having a designated place for handwashing all significantly predicted the frequency of handwashing.26 Psychosocial factors including remembering to wash one’s hands, self-efficacy, and action planning were all important contributors to the variance in self-reported handwashing frequency.
This impact evaluation has a number of limitations. First, in some SEAs, the program had started before the baseline survey; hence, their data were not truly pre-intervention data. Furthermore, some villages may have been affected by regional interventions such as collaboration with a chief, although the village was not triggered. However, this would result in a bias toward the null and any differences found would be underestimates. Second, we relied on respondents’ self-reporting for handwashing and defecation behaviors. Consequently, these results are subject to potential reporting biases, which may have resulted in either over or under estimation of indicators. Third, there may have been misclassification of improved sanitation at baseline during observations of toilet facilities by the data collectors. We addressed this challenge by carefully reviewing all types of improved latrines during the end line data collector training and by providing each data collector with a laminated pictorial atlas demonstrating examples of unimproved and improved latrines that were used during end line data collection. Fourth, government ODF certification data were incomplete and not available for all surveyed households. For those areas where we had complete data, there was good agreement between self-report of ODF status by households and local ODF verification data. Finally, because this was a nationwide program that had already begun implementation by the time of the baseline survey, it was not possible to perform this study with a control or comparison group. Even though there was no control group, the rigorous selection of rural households for the survey and comparison of the same SEAs after a 3-year period of program implementation allowed us to demonstrate temporal changes associated with the ZSHP.
This impact evaluation demonstrated improvements in sanitation and hygiene measures associated with the ZSHP. The reasons for a limited increase in handwashing require further investigation. The major focus on institutional strengthening and accountability of the key line ministries coupled with building capacity of governance structures in both the public and private sector, as well as at the community level, has been essential for the sustainability and expansion of the program. Sanitation marketing, an integral part of the program, appeared to contribute to the generation of sanitation demand and strengthening the supply of sanitation products and services. In addition, engagement of traditional leaders and the use of a mobile-to-web program that allowed real-time tracking of improved sanitation by traditional leaders and feedback to their communities were unique aspects of the program in Zambia that contributed to increased impact of the ZSHP.27 Continued programmatic activities including support for community-level sanitation training and capacity strengthening by the Zambian government may result in sustained benefits of this program, as has been found in Ghana and Ethiopia.28
Supplementary Material
Acknowledgments:
We would like to thank the caregivers and their children who took part in the study and the data collectors and supervisors. We would also like to acknowledge the kind assistance we received from the UNICEF Lusaka WASH team. We appreciate the helpful technical input of the Project Steering Committee. We are also grateful to the Lusaka Central Statistics Office for providing the standard enumeration area maps and the program implementation partners for providing us with details of their programmatic activities. We also would like to thank the Ministry of Local Government (and Housing) and Ministry of Health staff at district and provincial offices, and community champions and volunteers of the program from the sites where we collected data for their support during the data collection.
Note: Supplemental materials appear at www.ajtmh.org.
REFERENCES
- 1.National Water Supply and Sanitation Council (NWASCO) , 2012. 2013–2015 Strategic Plan. Lusaka, Zambia: NWASCO. [Google Scholar]
- 2.United Nations Sustainable Development Goals. Available at: https://www.un.org/sustainabledevelopment/sustainable-development-goals/. Accessed July 26, 2018.
- 3.WHO/UNICEF 2013. WHO/UNICEF Joint Monitoring Programme (JMP) for Water Supply and Sanitation. Estimates for the Use of Improved Sanitation Facilities Updated March 2012 for Zambia. New York, NY. [Google Scholar]
- 4.WHO/UNICEF , 2014. Progress on Sanitation and Drinking Water. Geneva, Switzerland: World Health Organization. [Google Scholar]
- 5.Water and Sanitation Program (WSP) Economic Impacts of Poor Sanitation in Africa: Zambia 2012. Available at: https://www.wsp.org/sites/wsp.org/files/publications/WSP-ESI-Zambia.pdf. Accessed March 6, 2018. [Google Scholar]
- 6.Real-Time Monitoring or Rural Sanitation at Scale in Zambia Using Mobile-to-Web Technology. Available at: https://www.unicef.org/esaro/WASH-Field-M2W-low-res.pdf. Accessed November 18, 2018. [Google Scholar]
- 7.Lawrence JJ, Yeboah-Antwi K, Biemba G, Ram PK, Osbert N, Sabin LL, Hamer DH, 2016. Beliefs, behaviors, and perceptions of community-led total sanitation and their relation to improved sanitation in rural Zambia. Am J Trop Med Hyg 94: 553–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Barrington DJ, Sridharan S, Shields KF, Saunders SG, Souter RT, Bartram J, 2017. Sanitation marketing: a systematic review and theoretical critique using the capability approach. Soc Sci Med 194: 128–134. [DOI] [PubMed] [Google Scholar]
- 9.Venkataraman V, Crocker J, Karon A, Bartram J, 2018. Community-led total sanitation: a mixed-methods systematic review of evidence and its quality. Environ Health Perspect 126: 026001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Planning Office, Evaluation and Research Office, Programme Division , 1995. Monitoring Progress toward the Goals of the World Summit for Children: A Practical Handbook for Multiple-Indicator Surveys. New York, NY: UNICEF. [Google Scholar]
- 11.Lê TN, Verma VK, 1997. An Analysis of Sample Designs and Sampling Errors of the Demographic and Health Surveys. DHS Analytical Reports No. 3. Calverton, MD: Macro International. [Google Scholar]
- 12.United Nations Statistics Division , 2005. Designing Household Survey Samples: Practical Guidelines. New York, NY: Statistics Division of the Department of Economic and Social Affairs of the United Nations. [Google Scholar]
- 13.Briceño B, Coville A, Gertler P, Martinez S, 2017. Are there synergies from combining hygiene and sanitation promotion campaigns: evidence from a large-scale cluster-randomized trial in rural Tanzania. PLoS One 12: e0186228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pickering AJ, Djebbari H, Lopez C, Coulibaly M, Alzua ML, 2015. Effect of a community-led sanitation intervention on child diarrhoea and child growth in rural Mali: a cluster-randomised controlled trial. Lancet Glob Health 3: e701–e711. [DOI] [PubMed] [Google Scholar]
- 15.Crocker J, Abodoo E, Asamani D, Domapielle W, Gyapong B, Bartram J, 2016. Impact evaluation of training natural leaders during a community-led total sanitation intervention: a cluster-randomized field trial in Ghana. Environ Sci Technol 50: 8867–8875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crocker J, Geremew A, Atalie F, Yetie M, Bartram J, 2016. Teachers and sanitation promotion: an assessment of community-led total sanitation in Ethiopia. Environ Sci Technol 50: 6517–6525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cameron L, Shah M, Olivia S, 2013. Impact Evaluation of a Large-Scale Rural Sanitation Project in Indonesia. World Bank Policy Research Working Paper No. 6360. Washington, DC: World Bank; Available at: 10.1596/1813-9450-6360 Accessed November 18, 2018. [DOI] [Google Scholar]
- 18.Guiteras R, Levinsohn J, Mobarak AM, 2015. Encouraging sanitation investment in the developing world: a cluster-randomized trial. Science 348: 903–906. [DOI] [PubMed] [Google Scholar]
- 19.Garn JV, Sclar GD, Freeman MC, Penakalapati G, Alexander KT, Brooks P, Rehfuess EA, Boisson S, Medlicott KO, Clasen TF, 2017. The impact of sanitation interventions on latrine coverage and latrine use: a systematic review and meta-analysis. Int J Hyg Environ Health 220: 329–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sigler R, Mahmoudi L, Graham JP, 2015. Analysis of behavioral change techniques in community-led total sanitation programs. Health Promot Int 30: 16–28. [DOI] [PubMed] [Google Scholar]
- 21.Zimba R, et al. 2016. Chiengi district, Zambia open defecation free after 1 year of community-led total sanitation. Am J Trop Med Hyg 95: 925–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Routray P, Schmidt WP, Boisson S, Clasen T, Jenkins MW, 2015. Socio-cultural and behavioural factors constraining latrine adoption in rural coastal Odisha: an exploratory qualitative study. BMC Pub Health 15: 880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merchant AT, Jones C, Kiure A, Kupka R, Fitzmaurice G, Herrera MG, Fawzi WW, 2003. Water and sanitation associated with improved child growth. Eur J Clin Nutr 57: 1562–1568. [DOI] [PubMed] [Google Scholar]
- 24.Mara D, Lane J, Scott B, Trouba D, 2010. Sanitation and health. PLoS Med 7: e1000363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Freeman MC, et al. 2014. Hygiene and health: systematic review of handwashing practices worldwide and update of health effects. Trop Med Int Health 19: 906–916. [DOI] [PubMed] [Google Scholar]
- 26.Seimetz E, Boyayo AM, Mosler HJ, 2016. The influence of contextual and psychosocial factors on handwashing. Am J Trop Med Hyg 94: 1407–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markle L, Maganani A, Katooka O, Tiwari A, Osbert N, Larsen DA, Winters B, 2017. A mobile platform enables unprecedented sanitation uptake in Zambia. PLoS Negl Trop Dis 11: e0005131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Crocker J, Saywell D, Bartram J, 2017. Sustainability of community-led total sanitation outcomes: evidence from Ethiopia and Ghana. Int J Hyg Environ Health 220: 551–557. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.