Abstract.
A high probability of another outbreak of communicable disease exists in sub-Saharan African countries, after the Ebola virus disease outbreak of 2014. Thus, health-care facility (HCF) preparedness for a prompt and effective response to disease outbreaks needs to be ascertained. In this study, Nigerian health-care workers’ (HCWs) knowledge of preparedness, perception of the level of preparedness existing in these HCFs, militating factors, and possible ways to improve, were evaluated through qualitative data collection, using focus group discussion and in-depth interview. Among the 193 HCWs which participated in the study, the perception of 190 (98.4%) was that their HCFs were insufficiently equipped to respond to disease outbreaks. None of the facilities had an emergency operation unit (EOU). Most HCWs perceived preparedness as observation of universal precautions. Other aspects of preparedness, such as training, routine emergency drills, disease surveillance, waste management, and design and location of HCFs were minimally mentioned. None of the participants had undergone any form of emergency drill training. Among the suggestions of how to improve on preparedness were immunization of staff, improved inter-departmental communication within the HCF, and routine training. The overall poor level of preparedness which exists in the HCFs means that they cannot prevent or contain a communicable disease outbreak. There is a need to improve universal precautions, communication within the HCFs, and routine interpretation of surveillance data by epidemiologists. There is also a need for the establishment of EOU in every HCF, a system that responds to, and manages emergency response to disease outbreaks, which also must be functional during non-outbreak periods.
INTRODUCTION
There have been repeated outbreaks of communicable diseases in Nigeria and most sub-Saharan African countries within the past 5 years1–3 and the occurrence of another outbreak is a matter of time. The last outbreak of Ebola virus disease (EVD) in West Africa was unprecedented4 and in the category of public health emergency of international concern.5,6 The cost was huge both financially and in human lives.7,8 It prompted a massive government and international donor organization emergency response aimed at halting regional spread of the disease. One factor that contributed to the multi-national epidemic was the sub-optimal healthcare system (HCS) and the unpreparedness of health-care workers (HCWs) in the affected countries.9,10 Being prepared and having a culture of safe health-care practices that can prevent and control the dissemination of pathogens is key to coping with disease outbreaks.11,12 A health-care facility (HCF) without a culture of safe practices will be exposed not only to disruption of the HCS, but also to increased risk of exposure of HCWs to communicable diseases.
By the end of November 2015, the WHO declared an end to the EVD outbreak. Given the time period since the declared end to EVD, now is a good time to reflect on the response to the EVD outbreak and to look for answers to the question: Are our health systems better prepared to anticipate and manage disease outbreaks? It would be optimistic to think that the EVD outbreak of 2014 would be the last communicable outbreak. It may not be another Ebola virus but another communicable disease outbreak, and it is almost impossible to predict with accuracy when it will occur, or its magnitude. Hence, the need to shift from reactive emergency responses to proactive focused approaches where the daily activities in the HCFs are adequate to contain potential outbreaks.
An extensive literature search revealed that the level of preparedness of HCFs have not been evaluated since the last outbreak of EVD, with the exception of one study in Ghana which focused on preparedness of HCWs.13 This dearth of information led us to assess the level of preparedness of our HCS and the knowledge of preparedness for emergency response to communicable disease outbreaks among HCWs in Nigeria.
MATERIALS AND METHODS
Ethical considerations.
The ethical approval to conduct this study was obtained from the Health Research Ethics Committee of the University of Nigeria, Teaching Hospital Enugu (Enugu, Nigeria). An information sheet was distributed to the participants before the study to explain its aims. Individuals who agreed to participate gave written consent before the interview commenced. To ensure anonymity, the location and designation of the respondents were omitted while reporting their responses in the result section.
Study design and setting.
The study design and setting have been presented in detail in reference 14 The study took place in public HCFs located in three states in Nigeria, of which only one reported EVD during the 2014 outbreak. All states had reported case(s) of other communicable diseases, including Lassa fever previously. The study was conducted in the major cities of these states and each of the study states has the three tiers of health-care delivery: primary, secondary, and tertiary. According to the national census of 2009, the population of the study states ranges from 2.8 million to 15 million individuals.
The study design was a qualitative cross-sectional study. Health-care workers were selected by a simple random method from both secondary and tertiary HCFs. The participants were doctors, pharmacists, nurses, laboratory scientists, physiotherapists, and other allied workers in the HCFs. Eligible participants were randomly selected for focus group discussions (FGDs). A total of 15 FGDs were conducted and each session involved 8–12 participants. In addition, 17 in-depth interviews (IDIs) were conducted, with participants derived from heads of departments or divisions within the HCFs.
Data collection in the study.
The interviews were conducted in English using an interview guide. The guides were designed to obtain information on HCWs’ facility evaluation, knowledge on preparedness, practice of universal precautions, and existence of emergency plans, stockpiling, and suggestions on how the level of preparedness for emergency response to disease outbreak could be improved. The universal precautions are the basic level of infection control precautions which are to be used as a minimum in the care of all patients with hand hygiene, and use of personal protective equipment as major components. Before any session of FGD, each participant was asked to fill and sign a biodata form. The biodata form was a small form that has brief description of the study, and space to fill-in the age, gender, occupation, place of residency, and space for signing of consent. Thereafter, each of the participants was assigned a number which they were asked to mention before responding to any question. This was for easy linkage of responses to the source and to enable quantitative analysis of certain responses. The respondents’ perceptions of their HCFs on preparedness were obtained individually. They were also asked to rate the performance of their HCFs, using a scale of 1–10, where 10 is the highest and 1 the lowest from their individual perception.
Data analysis.
Data were analyzed using a framework approach.15 The audio recordings of the IDIs and FGDs were transcribed verbatim into Microsoft Word documents (Microsoft, Redmond, WA) for analysis. To ensure transcription quality, all transcripts were independently checked against the original audio recordings and grammar errors were corrected. The transcripts were anonymized. A deductive approach was used to ensure that the analysis captured the main themes in the WHO preparedness conceptual framework checklist: facility evaluation, knowledge, and preparedness of HCW. An inductive approach was used for issues that were not anticipated during the research design but were explored in depth as they arose during the interview. The coding of the transcripts was performed by two independent coders and inconsistences were resolved by consensus. Thematic headings: knowledge on preparedness, evaluation of facility preparedness, militating factors, and suggestions on how it can be improved were used to develop the parent nodes and child nodes that were imported into NVivo software (QSR International, Melbourne, Australia). The information extracted through the coding framework was then analyzed. Frequency and percentages were calculated for few of the direct questions asked, such as competency of their facilities to handle disease outbreak and the rating of the level of preparedness. The responses of the HCWs to the rating of the level of preparedness of their HCFs were categorized, using Likert scales of 5: “very poor” (1–2), “poor” (3–4), “fair” (5–6), “good” (7–8), and “very good” (9–10). The Likert scale is an ordered scale of options which aligns with the views of the respondents on an issue.16 Odd-numbered response categories was adopted to allow evenly graded views of the respondents’ perspective of the level of preparedness of their facilities. The proportion of individual responses to each question was used to calculate the percentage. The three sites where the study were conducted were coded Site A, B, and C to ensure anonymity.
RESULTS
Population characteristics.
A total of 193 HCWs participated in the 15 FGDs and 17 IDIs; 32.6% (63/193) were male and 67.4% (130/193) were female. Their mean age was 37.7 years with range from 24 to 65 years (Table 1).14
Table 1.
Sociodemographic characteristics of the respondents
| Variables | |||
|---|---|---|---|
| Locality | Site A | Site B | Site C |
| Total participants (n = 193) | 66 (34.2%) | 61 (31.6%) | 66 (34.2%) |
| Age | |||
| Mean (SD) | 36.3 (5.44) | 31.1 (4.65) | 38.8 (7.83) |
| Range | 26–65 | 24–45 | 28–56 |
| Gender | |||
| Male | 21 (31.8%) | 27 (44.8%) | 15 (22.7%) |
| Female | 45 (68.2%) | 34 (55.2%) | 51 (77.3%) |
| Designation | |||
| Doctors | 22 (33.3%) | 19 (31.2%) | 31 (47.0%) |
| Nurses | 18 (27.3%) | 20 (32.8%) | 13 (19.7%) |
| Physiotherapists | 6 (09.1%) | 18 (29.5%) | 12 (18.2%) |
| Laboratory scientists | 3 (04.5%) | 2 (03.3%) | 3 (04.5%) |
| Pharmacists | 3 (04.5%) | 1 (01.6%) | 0 |
| Others | 14 (21.2%) | 1 (01.6%) | 7 (10.6%) |
| Years of practice | |||
| Mean (SD) years | 11.85 (9.45) | 5.25 (5.12) | 12.17 (8.55) |
| Range | 2.5 months–35 years | 1 month–24 year | 2 months–34 years |
Modified from Esangbedo et al.14
Health-care workers’ knowledge on preparedness.
The participants’ knowledge of preparedness was elicited from their responses to the question, How prepared is your health-care facility to handle any outbreak of infectious diseases? What the participants described as being prepared and what they stated was missing were identified.
The components mentioned in their description of preparedness by the 193 respondents were: use of hand sanitizer, availability of running water, use of latex gloves, face masks, and protective gowns. A few participants were concerned about the design of the HCF, waste management, training-and-retraining of HCWs, drill on emergency management, and disease surveillance. These statements were captured in some of their responses:
“No, we don’t have towels, napkins, and functional hand-free water tap. We have the regular hand gloves, that’s all. The regular face masks are made available only when needed” (Nurse, Teaching Hospital)
“There are functional water taps here, but no soap solution or soap bar. There are gloves and face masks, but not all the time.” (Doctor, Federal Medical Centre)
“Once you have the protective garments and hand sanitizers, I don’t think there is any other thing required…” (Doctor, Secondary Healthcare Facility)
Health-care workers rating of the preparedness of their HCFs.
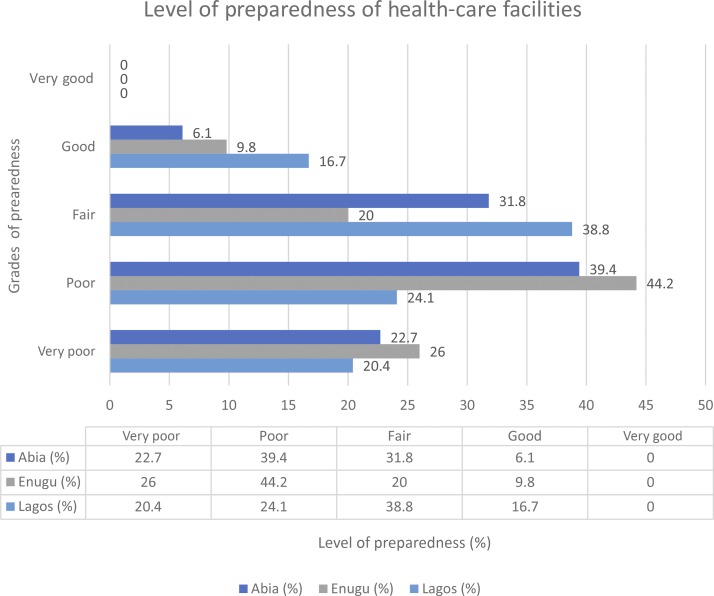
Table 2 shows the levels of preparedness of the HCFs to respond to an outbreak. In the HCW’s response to the question: Is your health facility sufficiently ready to handle and manage outbreaks? Of the 193 respondents, 98.4% (190/193) said “no,” when asked to rate the competence of their HCFs to handle an outbreak on a Likert scale of “1” to “10” where “1” is the lowest and “10” is the highest, 58.6% (113/193) rated the level of preparedness of their HCFs to be either 1 and 2, or 3 and 4, which signifies very poor or poor, whereas 58.6% (113/193) rated their HCFs to be either 5 and 6 or 7 and 8 (fair or good). None considered their facilities to be very good (see Figure 1).
Table 2.
Preparedness of the health-care facilities for an outbreak
| Variables | ||||
|---|---|---|---|---|
| Locality | Site A | Site B | Site C | |
| Total participants (n = 193) | 66 (34.2%) | 61 (31.6%) | 66 (34.2%) | |
| Whether their health-care facilities are competent to handle outbreak | ||||
| Yes | 3 (1.6%) | 2 (3.0%) | 0 (0.0%) | 1 (1.5%) |
| No | 190 (98.4%) | 64 (97.0%) | 61 (100%) | |
| Rate | ||||
| Very poor | 44 (22.8%) | 13 (20.4%) | 16 (26.0%) | 15 (22.7%) |
| Poor | 69 (35.8%) | 16 (24.1%) | 27 (44.2%) | 26 (39.4%) |
| Fair | 59 (30.5%) | 26 (38.8%) | 12 (20.0%) | 21 (31.8%) |
| Good | 21 (10.9%) | 11 (16.7%) | 6 (9.8%) | 4 (6.1%) |
| Very good | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) |
Figure 1.
Level of preparedness of health-care facilities. This figure appears in color at www.ajtmh.org.
Health-care worker’s evaluation of components and preparedness of their facilities.
There were variations in the evaluation of their HCF with regard to being suitable to control the spread of infection. These were extracted from their responses to the question, “Are your healthcare facilities sufficiently ready to handle and manage outbreaks? Some of the comments they made were as follows:
“All patients are just in an open place.” (Doctor, Teaching Hospital)
“If there is an outbreak, there is supposed to be an isolation room that is far away from the ward, but presently, I don’t think there is anywhere that they can isolate patients” (Nurse, Secondary Healthcare facility)
“I want to talk on waste management and waste disposal. We noticed that the way they dispose waste is not right. The safety measures and water are not there.” (Physiotherapist Teaching Hospital)
“The design of the healthcare facilities is wrong because of the entrance. We have one entrance here in the hospital. You know, normally there are supposed to be three or four entrances, but in this hospital, we just have one. When patients are coming into the hospital, they meet people at the single entrance. The same entrance serves for removal of corpses and other people doing all sorts of things, and this is very, very bad for disease and infection control.” (Nurse, Secondary Healthcare facility)
“During the Ebola outbreak, we were able to wash hands, we had functional taps. Sanitizers were all over the hospital. Face masks and soap were readily available as well. We were a lot more conscious and indeed better. All that has gone down a bit and a lot of people have regressed.” (Pharmacist, Secondary Healthcare Facility)
“At least, when there was Ebola, everybody was always conscious while working and wearing ward coats, but now that there is no more Ebola, everything has gone back to what it was.” (Doctor, Teaching Hospital)
“Our emergency response is very low, and we tend to have this panicky attitude.” (Physiotherapist, Federal Medical Centre)
Some affirmative responses on facility preparedness.
Some respondents did however provide positive commentary of the preparedness of the facilities in which they worked. For example:
“Very well; we had training on Ebola virus, where everybody was educated on the preventive measures particularly wearing of face masks and gloves.” (Nurse, Primary Healthcare facility)
“HIV Unit is well trained on antiseptic techniques. So we are very particular about sterilization. After washing the instrument, you still use sodium hypochlorite to soak our instrument before we autoclave them; that is standard practice.” (Laboratory Scientist, Secondary Healthcare Facility)
Factors that militate against facility preparedness.
Beyond preparedness, the respondents were also asked to mention some of the factors that militate against having an optimal level of preparedness. Among the factors mentioned were: lack of funds, lack of space and poor design of the hospitals, low level of awareness, and lack of collaboration between different disciplines in health care. Some of their comments that capture these were as follows:
“First and foremost is funds. We do not generate fund. Treatment here is free and we survive on the subvention from the government. This constrains the hospital from achieving its objectives towards provision of universal precautions.” (Pharmacist, Secondary Healthcare Facility)
“When I say education, we went for training where we were taught how to wear ideal WHO outfit and all that, but, then, they were basically videos, and there was no hands-on training. We were supposed to come back to step down the training to other members of staff. That didn’t happen because we didn’t have the outfit to practice with.” (Nurse, Secondary Healthcare Facility)
Suggestions on how to improve preparedness.
The respondents’ suggestions on the measures needed to improve preparedness of their HCFs were also elicited. Among the interventions mentioned were immunization of staff, especially the newly employed staff, implementation of continuous education and training, relocation or renovation of old facilities to a more suitable location and designs that enhance service delivery, allowing some level of autonomy for departments to fashion out their own preparedness programme, training-and-retraining of staff, as well as educating patients to know the basic level of precautionary measures expected of both themselves and HCWs.
“I will have to say immunization because I remember when I was doing my house officer rotation, we all had to be immunized.” (Doctor, Teaching Hospital)
“Continuous education and surveillance, so that we are not caught unawares.” (Physiotherapist, Teaching Hospital)
“Probably, supply to healthcare facilities should be taken over centrally and supply to each unit on a regular basis instead of each unit having to request for it. All hospitals should be supplied centrally, probably from the Ministry of Health. It will not be the issue of hospitals providing from their revenue or the allocated funding of the hospital. Some hospitals are better equipped than others. We are a bit sustained here because we have been receiving donations and funding.” (Pharmacist, Federal Medical Centre)
DISCUSSION
This study revealed that most HCWs lack adequate knowledge on preparedness for emergencies and response to communicable disease outbreak. The study also revealed that HCFs were not prepared to manage outbreaks of communicable diseases. This was similar to what has been reported previously.17,18 The HCWs’ knowledge on preparedness was limited to availability and use of universal precautions. Only a few talked about training as part of preparedness,19 routine drills and rehearsal on the handling of emergency situations, and the design and location of infrastructure. The proportion of the respondents that mentioned disease surveillance20 and immunization21 as components of preparedness was insignificant, probably because of a lack of understanding of their role/importance in outbreaks management. The overall knowledge of HCWs on preparedness is very vital in the control of any disease outbreak.22 This knowledge should be comprehensive for prompt, effective, and efficient response to communicable disease outbreak.
Universal precautions alone cannot prevent or contain a communicable disease outbreak. Adequate universal precautions should be practiced in well-designed HCFs, where proper documentation and communication between various units are optimal. The poor knowledge in preparedness contrasted with what was expected in areas that just experienced a major EVD outbreak. This underscores the poor efforts toward improvements in the HCS to avert inadequacies in the management of future communicable disease outbreaks. Preparedness is a process with multiple components, and if there were changes in the capacities of the HCS to handle disease outbreaks, the HCWs would have noticed the impact on the standard operating procedures in the delivery of their services. A study that reported high knowledge of preparedness among HCWs focused on aseptic precautions and preferred the use of antiseptics during outbreaks23 shared similar finding with this study. The level of preparedness of HCFs cannot be complete without improvement of the knowledge and skills of HCWs. Thus, regular training and re-training of staff on preparedness is of paramount importance.
Looking beyond the last EVD outbreak, there has been a long history of other infectious disease outbreaks.3,24,25 In the past decade, cholera, Lassa fever, monkey pox, HIV/AIDS, and other strains of viruses have affected millions of people in Nigeria.3,24,25,26 Fortunately, none transformed into a major epidemic or worse still, a pandemic of global scale. However, the threat persists, and the existing poorly designed HCFs and non-implementation of adequate disease surveillance are reflected in the poor ratings of the facilities presented in the findings. The need for a coordinated restoration of basic health services that includes immunization of HCWs, provision of universal precautions, implementation of control programmes, disease surveillance, and infrastructural and human resource development, which have been ignored over time, is an urgent requirement. To achieve this, every HCF requires the establishment of a system that responds to emergencies and manages such response in the form of an emergency operation unit (EOU). An EOU is a hospital-based version of a WHO public health Emergency Operations Centre.27 It will be an important component of emergency preparedness with multi-departmental coordination and response to a variety of health-related hazards and disease outbreaks. The EOU in the HCFs should have a physical space and dedicated staff with the ability to monitor events, using different sources of data, improve on communication between public health and emergency management personnel, facilitate coordination with multiple response partners, and provide space for members of the incident command team to gather and work. The EOU should be able to function during non-outbreak periods, and surveillance data should routinely be interpreted by an epidemiology unit. This will facilitate the rapid transition to response mode during outbreaks and improve the cost-effectiveness of investment in the infrastructure. The routine use of EOUs during outbreaks and during non-outbreak periods helps to ensure sustained technical capacity for data analyses, interpretation, and visualization tools and equipment, as well as the knowledge to analyze and interpret incoming health information.27–29
There is also a lack of financial investment in the area of preparedness. During the recent EVD outbreak in West Africa, government and international agencies spent millions of dollars in containing the outbreaks, and there were huge losses of lives, as well as in regional economy.30 When compared with the resources devoted to mitigating already occurred outbreaks, the investment required for infectious disease outbreak preparedness is strikingly little and cost-effective. The advocacy by health-care groups should include the articulation of the loss of lives and the economic losses due to an outbreak to attract the urgently needed political will for the establishment of a preparedness programme for communicable disease outbreaks.
Although funds are required for implementation of any intervention, the problem is not only due to lack of funds, but the need to show transparency and diligence in the disbursement of funds and the timeliness of the release of funds. This is very important, considering that resource mobilization is always difficult. Good cost-effectiveness evaluation could improve the funding of HCS. According to a report by the Commission on the Global Health Risk Framework, it will cost less than $5 billion annually to implement robust preparedness measures, which is far less than the cost of a major disease outbreak or pandemic.31 Thus, if the money can be made available during an outbreak, it will be wiser to release a significantly less amount for preparedness. There is a need to avoid the vicious cycle of panic, fire-brigade-resource-wasting approach that leads to huge investment of resources during outbreaks with a resultant lack of interest and dwindled investments in preparedness. The outbreak-driven responses are both ill planned and capital intensive and should be discouraged. The health-care managers should allow diffusion of innovations through the understudy of the military and other law enforcement agencies, to understand the factors that guarantee their level of alertness and prompt responses to emergencies, because both share the same denominator of protection and safeguard of lives and properties (catastrophic health expenditures).
It is also necessary to continually evaluate the design and location of HCFs in view of containing the spread of any outbreak. Some of the existing HCFs were strategically located when they were built, but with an increase in population and dynamics of urban development, the design and space provided for the HCFs have been encroached upon by residential and commercial buildings. Some of these facilities have exceeded their capacity in terms of HCWs, caregivers, and the patients they handle on a daily basis with very limited space to deliver services effectively and efficiently. Some formerly designated isolation areas have been taken over by wards, offices, and other ancillary services. With the recent emergence of outbreaks of infectious disease that require isolation areas/wards, it is difficult to find isolation space for such. There is lack of space in between beds in wards for effective infection control.32 Patients suffering from both communicable and non-communicable diseases are routinely nursed in the same open wards. This is a practice that should be discouraged if the preparedness of HCFs must improve.
One limitation in this study is not including patients in the evaluation of the level of preparedness of HCFs because it is the responsibility of both the HCWs and the patients to contain the spread of the infection; the perspective of the patients may have revealed more areas that need intervention and improvement. Furthermore, the conduct of this study exclusively on government-owned HCFs is another limitation. Inclusion of private HCFs would have given this study an overall view on the level of preparedness of the entire HCS. Although getting information on the level of preparedness from HCWs in private HCFs can be a daunting task, effort should be made in future studies to include private HCFs. The fact that this study was conducted in different states and involved different cadres of HCWs, made the findings of this study a good representation of the existing level of preparedness of most HCFs in Nigeria, toward prevention of disease outbreak.
CONCLUSION
The overall poor level of knowledge in preparedness by HCWs and low standard of disease prevention and surveillance which exists in most HCFs cannot effectively contain the spread of communicable disease outbreaks. Efforts should be made to improve knowledge in preparedness through regular hands-on trainings and routine emergency preparedness drills. Health-care facilities should look beyond the provision of universal precautions to inclusion of improved inter-departmental communication and information sharing, and regular interpretation of surveillance data by epidemiologists and establishment of EOU in every health institute. An EOU should respond to emergencies and manage the same, and have the capacity to function during non-outbreak periods and facilitate rapid transition to response mode during outbreaks.
Acknowledgments:
We thank all individuals who made this study possible. Our special thanks go to the Lagos State Health Services Commission (Lagos, Nigeria) for the approval to conduct the study in Lagos. The American Society of Tropical Medicine and Hygiene (ASTMH) assisted with publication expenses.
REFERENCES
- 1.Otu A, Ameh S, Osifo-Dawodu E, Alade E, Ekuri S, Idris J, 2017. An account of Ebola virus disease outbreak in Nigeria: implications and lessons learnt. BMC Public Health 18: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization , 2018. Nigeria Battles its Largest Lassa Fever Outbreak on Record. Available at: www.afro.who.int. Accessed March 15, 2018. [Google Scholar]
- 3.Adagbada AO, Adesida SA, Nwaokorie FO, Niemogha MT, Coker AO, 2012. Cholera epidemiology in Nigeria: an overview. Pan Afr Medl J 12: 59. [PMC free article] [PubMed] [Google Scholar]
- 4.Joshi RM, 2014. Ebola virus disease (EVD): an unprecedented major outbreak in west Africa. Clin Microb 3: e119. [Google Scholar]
- 5.Ughasoro MD, Esangbedo DO, Tagbo BN, Mejeha IC, 2015. Acceptability and willingness-to-pay for a hypothetical Ebola virus vaccine in Nigeria. Plos Negl Trop Dis 9: e0003838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization , 2014. Statement on the 1st Meeting of the IHR Emergency Committee on the 2014 Ebola Outbreak in West Africa. Geneva, Switzerland: WHO; Available at: www.who.int. Accessed April 14, 2018. [Google Scholar]
- 7.CDC , 2016. 2014 Ebola Outbreak in West Africa-Case Counts. Available at: https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html. Accessed February 16, 2018. [Google Scholar]
- 8.Centers for Disease Control and Prevention , 2016. Cost of the Ebola Epidemic. Available at: https://www.cdc.gov. Accessed November 14, 2018. [Google Scholar]
- 9.Oladimeji AM, et al. 2015. Ebola virus disease–gaps in knowledge and practice among healthcare workers in Lagos, August 2014. Trop Med Int Health 20: 1162–1170. [DOI] [PubMed] [Google Scholar]
- 10.Olowookere SA, Adioye-Kuteyi EA, Adepoju OK, Esan OT, Adeolu TM, Adeoye TK, Adepoju AA, Aderogba AT, 2015. Knowledge, attitude, and practice of health workers in a tertiary hospital in Ile-Ife, Nigeria, towards Ebola viral disease. J Trop Med 2015: 431317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.World Health Organization , 2012. Emergencies Preparedness, Response. Infection Prevention and Control in Health Care for Preparedness and Response to Outbreaks. Available at: www.who.int. Accessed April 14, 2018. [Google Scholar]
- 12.Balajee S, et al. 2017. Sustainable model for public health emergency operations centers for global settings. Emerg Infect Dis 23 10.3201/eid2313.170435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Annan AA, Yar DD, Owusu M, Biney EA, Forson PK, Okyere PB, Gyimah AA, Owusu-Dabo E, 2017. Health care workers indicate ill-preparedness for Ebola virus disease outbreak in Ashanti region of Ghana. BMC Public Health 17: 546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Esangbedo DO, Ughasoro MD, Tagbo BN, Olowu A, Anikene C, Iwegbulam CC, 2016. Health-care workers’ perspective on Ebola virus vaccine: a focus group and in-depth interview interventional study. Am J Trop Med Hyg 95: 658–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Braun V, Clarke V, 2013. Successful Qualitative Research: A Practical Guide for Beginners. London, United Kingdom: Sage; Available at: http://eprints.uwc.ac.uk/21156. Accessed February 10, 2017. [Google Scholar]
- 16.Losby J, Wetmore A, 2012. CDC Coffee Break: Using Likert Scales in Evaluation Survey Work. National Center for Chronic Disease Prevention and Health Promotion; Available at: https://www.cdc.gov/dhdsp/pubs/docs/CB_February_14_2012.pdf. Accessed March 18, 2018. [Google Scholar]
- 17.Yayi A, Laing V, Govule P, Onzima RADDM, Rogers Ayiko, 2015. Performance of epidemic prevention, preparedness and response in West Nile region, Uganda. Int J Public Health Res 3: 228–233. [Google Scholar]
- 18.Daugherty EL, Carlson AL, Perl TM, 2010. Planning for the inevitable: preparing for epidemic and pandemic respiratory illness in the shadow of H1N1 influenza. Clin Infect Dis 50: 1145–1154. [DOI] [PubMed] [Google Scholar]
- 19.Hsu EB, Thomas TL, Bass EB, Whyne D, Kelen GD, Green GB, 2006. Healthcare worker competencies for disaster training. BMC Med Educ 6: 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pilot E, Roa R, Jena B, Kauhi B, Krafft T, Murthy GVS, 2017. Towards sustainable public health surveillance in India: using routinely collected electronic emergency medical service data for early warning on infectious diseases. Sustainability 9: 604. [Google Scholar]
- 21.Hinman AR, Orenstein WA, Schuchat A, 2011. Vaccine-preventable diseases, immunizations, and the epidemic intelligence service. Am J Epidemiol 174 (11 Suppl): S16–S22. [DOI] [PubMed] [Google Scholar]
- 22.Martins SO, Osiyemi AO, 2017. Hand hygiene practices post-Ebola virus disease outbreak in a Nigerian Teaching Hospital. Ann Ib Postgrad Med 15: 16–22. [PMC free article] [PubMed] [Google Scholar]
- 23.Tour EA, Traor EF, Sako F, Delamou A, Tonguino F, Sylla D, Bangoura M, Barry M, Cisse M, Vanhems P, 2016. Knowledge, attitudes, and practices of healthcare workers on Ebola virus disease in Conakry, Guinea: a cross-sectional study. J Public Health Epidemiol 8: 12–16. [Google Scholar]
- 24.Shaoor S, Mir F, Zaidi AKM, Zafar A, 2015. Hospital preparedness in community measles outbreaks-challenges and recommendations for low-resource settings. Emerging Health Threats J 8: 24173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ajayi NA, Nwigwe CG, Azuogu BN, Onyire BN, Nwonwu EU, Ogbonnaya LU, Onwe FI, Ekaete T, Gunther S, Ukwala KN, 2013. Containing a Lassa fever epidemic in a resource-limited setting: outbreak description and lessons learned from Abakaliki, Nigeria (January–March 2012). Int J Infect Dis 17: e1011–e1016. [DOI] [PubMed] [Google Scholar]
- 26.World Health Organization Monkey Pox–Nigeria, Emergencies Preparedness, Response. https://www.who.int/csr/don/05-october-2018-monkeypox-nigeria/en/. Accessed November 18, 2018. [Google Scholar]
- 27.Centers for Disease Control and Prevention , 2016. Emergency Operations Centers: CDC Emergency Operations Center (EOC). Available at: https://www.cdc.gov/phpr/eoc.htm. Accessed January 17, 2018. [Google Scholar]
- 28.World Health Organization , 2015. Framework for a Public Health Emergency Operations Center. Available at: http://apps.who.int/iris/bitstream/10665/196135/1/9789241565134_eng.pdf. Accessed January 17, 2018. [Google Scholar]
- 29.World Health Organization , 2013. A Systematic Review of Public Health Emergency Operations Centers (EOC). Available at: http://apps.who.int/iris/bitstream/10665/99043/1/WHO_HSE_GCR_2014.1_eng.pdf. Accessed January 17, 2018. [Google Scholar]
- 30.Centers for Disease Control and Prevention (CDC) , 2016. 2014–2016 Ebola Outbreak in West Africa. Available at: https://www.cdc.gov. Accessed April 4, 2016. [Google Scholar]
- 31.Sands P, Shah CM, Dzau VJ, 2016. The neglected dimension of global security. A framework to counter infectious disease crises. N Engl J Med 374: 1281–1287. [DOI] [PubMed] [Google Scholar]
- 32.Ughasoro MD, Okanya OC, Uzochukwu B, Onwujekwe OE, 2017. An exploratory study of patients’ perceptions of responsiveness of tertiary health-care services in southeast Nigeria: a hospital-based cross-sectional study. Niger J Clin Pract 20: 267–273. [DOI] [PubMed] [Google Scholar]