Abstract.
The dengue situation in the urban setting of Hanoi city, Vietnam, is emerging, focusing on inner districts. Previous studies showed that a dengue vector control program in Hanoi was not effective because of the lack of adequate engagement of the local government authorities, health sector, and community. This implementation research aimed to explore barriers to implementing community engagement in a dengue vector control program in an urban district of Hanoi city. Ten in-depth interviews and 14 focus group discussions were conducted at Lang Thuong, Khuong Thuong, Tho Quan, and Kim Lien wards in Dong Da district, Hanoi city. Data collection was implemented from April to June 2017. All discussions were recorded and transcribed verbatim. Data were analyzed using the content analysis approach. Secondary data from the dengue vector control program reports were used to support the qualitative evidence. We found that the barriers to implementing effective community engagement were as follows: 1) lack of interest and an attitude of dependency on action from the health sector of local people’s committee, 2) lack of enthusiasm of mass organizations and community leaders, 3) overburdened workloads and lack of communication skills from health sector, 4) low awareness and readiness from community, 5) lack of detailed policy guidelines and low enforcement of related policy, and 6) limited budget. Recommended actions should be made to improve the community engagement in the current resource-limited context of Vietnam by both top-down and bottom-up approaches.
INTRODUCTION
Dengue is a global public health threat. A recent study estimated that 390 million individuals are infected by dengue yearly in more than 100 countries.1 Approximately half a million people were hospitalized with dengue hemorrhagic fever and about 2.5% of those died.2 These morbidity and mortality rates correspond to an enormous total annual cost of dengue illness of 8–9 billion USD globally.3
Dengue fever (DF) is a vector-borne disease caused by the dengue virus. Dengue virus are arboviruses that are transmitted to humans by infected Aedes mosquitoes. The WHO proposed five strategies for reduction of dengue burden worldwide, including diagnosis and case management, integrated surveillance and outbreak preparedness, sustainable vector control, future vaccine implementation, and basic operational and implementation research. Although a vaccine is in the trial phase, vector control is seen as the best measure for dengue prevention by controlling Aedes mosquitoes.4 The householders and communities will take responsibility to reduce the number of potential breeding sites routinely supported by education, social mobilization, and community engagement from the health sector and local authorities.
The term “community engagement” is increasingly promoted in international health research and practices. Community engagement, defined as an ongoing relationship between citizens, health-care providers, and other community members and organizations to improve health through dialog, is a process rather than an end point.5 More specifically, this term is defined as “the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people. It is a powerful vehicle for bringing about environmental and behavior changes that will improve the health of the community and its members. It often involves partnerships and coalitions that help mobilize resources and influence systems, change relationships among partners, and serve as catalysts for changing policies, programs, and practices.”6 An effective and sustained dengue vector control program requires intersectoral collaboration and coordination. Dengue vector control programs need to build partnerships between diverse government ministries (health, environment, education, etc.); municipal and local authorities; public and private sectors; and professional, religious, and community representatives.4,7 Many studies have shown that dengue vector control activities are not successful without the participation and action of the community.8–11 To achieve a successful and sustained dengue vector control program, community engagement with optimum ownership of the program from the community is necessary.12
There has been an increasing trend of community-based participatory interventions using integrated community engagement strategies in the recent decades.13–17 However, findings from a systematic review indicated that the evidence-based community engagement in dengue vector control programs was still weak.18 Also, multi-entity coordination and partnership between relevant stakeholders in most dengue programs have been limited.9,16 This lack of community engagement in dengue vector control services is especially seen in developing countries, including Vietnam.19
Vietnam is a dengue-endemic country in the Asia–Pacific region. Even though Vietnam has successfully reduced the case fatality rate of dengue to less than one per 1,000 cases since 2005, the number of dengue cases remains high.20 The dengue control program in Vietnam is organized vertically with a top-down approach from the national level to the provincial, district, and community/ward levels. However, program activities were varied depending on local custom, society, and budget. According to the official guidelines on surveillance, prevention, and control of DF of the Ministry of Health, the activities are focused on vector control and larval eradication with the active engagement of each household and a whole community. The local government and health sector are responsible for reminding and urging the stakeholders and the participation of political and social organizations. Some typical activities consisted of 1) preventing mosquitoes from accessing egg-laying habitats by environmental management and modification at home and through cleanup campaigns; 2) disposing of solid waste properly and removing artificial man-made habitats; 3) covering, emptying, and cleaning of domestic water storage containers on a weekly basis; 4) applying appropriate insecticides to water storage outdoor containers; and 5) using biological control agents (predatory copepods or fish) and health information, education, with appropriate communication concerning DF.
Hanoi, the capital and second most populous city in Vietnam, is an endemic area. In the largest recorded dengue outbreak in 2009, 16,263 DF cases were confirmed in Hanoi, which accounted for 87% of total DF cases in the Northern area of Vietnam.21 The 2015 dengue outbreak recorded 90% in total, of the 16,913 cases in the Northern region lived in Hanoi.22 Of those dengue cases, 77.2% of the total cases were concentrated in urban areas during the period of 2006–2011.23 Other studies showed similar results that DF cases were mostly found in inner-city districts.21,24 Some recent research implemented in urban districts in Hanoi concluded that the less effective dengue vector control programs were related to the lack of community engagement.25–27 This implementation research aimed to explore the barriers to the implementation of community engagement in a dengue vector control program in an urban district of the Hanoi city.
METHODS
Study settings and period.
Hanoi city has 12 urban districts, of which Dong Da is the one in the inner-city districts with the highest prevalence of DF in recent years.28,29 Dong Da district also has a high population density, with around 352,000 citizens living crowded in an area of 9.96 km2. Among 21 wards across the district, four wards were also selected purposively based on the latest data on the incidence rate in 2017 of Hanoi Preventive Medicine Center including Lang Thuong (384,65/100,000), Khuong Thuong (353,44/100,000), Kim Lien (192,52/100,000), and Tho Quan (104,18/100,000).30
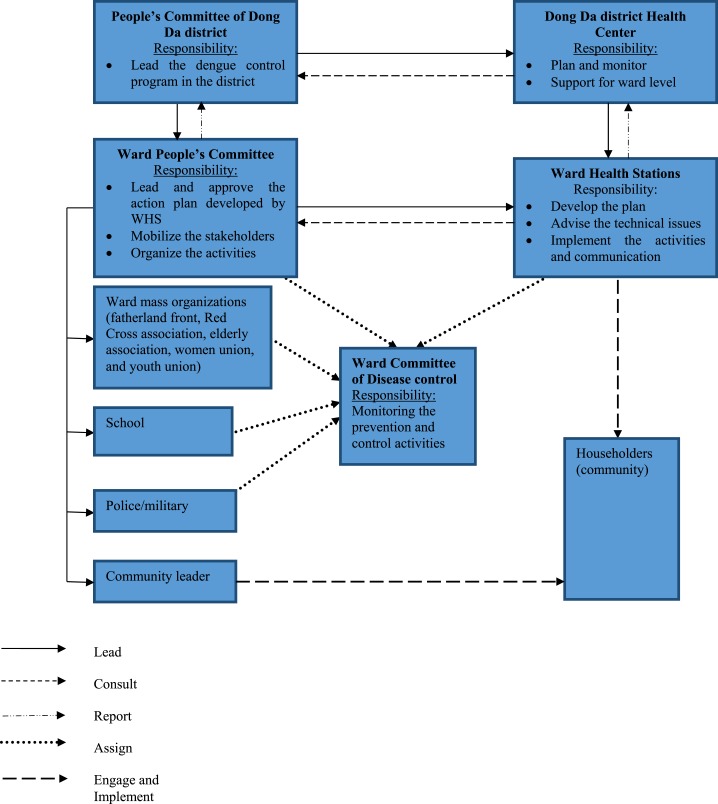
Figure 1 summarizes the organization of stakeholders in our research site.
Figure 1.
Organization of stakeholders in dengue control program. This figure appears in color at www.ajtmh.org.
The People’s Committee at the ward level is the main actor that leads and manages all the community engagement activities. The other key actor in mobilizing stakeholders in the program is the ward health station (WHS), which is the first formal point of health-care contact in the government health-care system. They are responsible for making an action plan and supporting all dengue-related technical prevention and control issues. Besides, there is also a network of mass organizations/unions whose functions are supported by the Socialist Party, and which represent strong stakeholders in Vietnam with branch offices established at all administrative levels and are under the management of the People’s Committee and with large proportions of the population as members including fatherland front, women union, youth union, veteran association, elderly association, and the International Red Cross association. Another workforce group with the aforementioned actors and other stakeholders also formed to assist in the dengue vector control program and implement the community engagement was the ward committee of disease control with the duty of monitoring the activities. The research was conducted from January to August 2017.
Study design.
This implementation research was a qualitative study involving all relevant stakeholders including responding entities in the health sector, local authorities, and community. Qualitative data and program-related secondary data were collected.
There were 10 in-depth Interviews (IDIs) and 14 focus group discussions (FGDs) conducted in the study, as follows:
1. Two IDIs with an officer of the Hanoi city Preventive Medicine Center and an officer of the Dong Da District Health Center
2. Four IDIs with the representatives of WHSs
3. Four IDIs with the representatives of ward People’s Committee (WPC)
4. Four FGDs with 22 ward health staff
5. Three FGDs with 19 representatives from school, police/military/civil defense forces, and head of residency cluster and mass organizations
6. Seven FGDs with 40 householders
Health officers who were responsible for dengue prevention and control program at the Hanoi city Preventive Medicine Center and the Dong Da District Health Center and had stayed at their position for at least 2 years were purposively invited for interview. In each ward, representatives of WPC who were responsible for medical work and had stayed at their position for at least 2 years were also invited to participate in the research. Health staff who were working at the WHS actively joined the research. The group of representatives from schools, police/military/civil defense forces, head of the residency cluster, and representatives from mass organizations were invited through the suggestions of WPC and WHS if they were not absent at the interview time. In case of absence, another one was substituted by WPC’s nomination. For those who were the householder, quota sampling was used to recruit based on the inclusion criteria to allow exploration of differences in groups from different experiences with DF. They were living in the research area and were the one with a range of past experiences with dengue (some with dengue infections in their family and others without). The large diversity of participants provided a broad range of views on the research topic. To ensure the quality of results, data were triangulated to allow comparison across sources and different types of respondents. The IDIs and FGDs reached the data saturation criteria, where no new information was uncovered.
Data collection and analysis.
In-depth interviews and FGD guidelines were developed by the researchers to collect information. In-depth Interview and FGDs were conducted at WHS and WPC meeting halls which ensured the privacy and convenience for the participants. These interviews were performed in Vietnamese. For IDIs, the principal investigator (PI) was the interviewer and notetaker as well. After the IDIs, the interviewer asked for the documents related to the topic. These documents were action plans and reports of program activities from the provincial to ward level that were read, and extracted the related information for supplementing the qualitative data. For FGDs, the PI was the moderator, and a research assistant took notes. Both the PI and research assistant worked in the public health field and had experience in qualitative interviewing. The PI was familiar with the context of Hanoi city, and this could reduce the credibility of the results; therefore, the PI only assisted the two coauthors in the data analysis to increase the trustworthiness and validity of the study.
All discussions lasted approximately 30–45 minutes and started with an introduction to the topic and the purpose of the study. The importance of active participation, contributions from all participants, and the freedom to make any statement were emphasized. Participants were interviewed on the factors affecting the community engagement of stakeholders in dengue vector control programs such as socioeconomic concerns, cultural aspects, geography, environment, policies, resources, community readiness, commitment, and active participation. All interviews were tape-recorded with permission from participants. The recorded files were then relistened to check the quality of the probes, and transcribed within 24 hours. All discussions were recorded and transcribed verbatim into an Microsoft Word Office 2013 document. Notes taken by the moderator and notetaker supplemented the audio-taped transcripts to collect and confirm details from the discussion. Content analysis was performed by organizing all interview text into key themes. Based on the transcripts, a list of codes was progressively established and structured. Related interview texts were coded systematically, and the most appropriate themes were chosen to illustrate the findings regarding the participants’ perceptions about barriers to the implementation in community engagement in dengue vector control programs. Only these related quotations were translated into English for research purposes.
RESULTS
Barrier from WPC.
Rely too much on WHS.
It can be deduced that the distribution of responsibility on disease control between two important sides of WPC and WHS was not balanced. As mentioned earlier, WPC should take the lead and organize the dengue vector control activities under the consultation of WHS. However, the WPC handed over almost all work related to health protection to the WHS.
“Respondent hesitated to share”. Their role is very important but they haven’t done well enough to their importance. They are the organizer. Actually; the ward health station is only the consultant, and they have to lead and organize but it’s truly a reserve position (FGD with health staff of WHS 2)
To tell the truth, the PC sometimes still said that this work belongs to health station. So, it’s very hard for us (FGD with health staff of WHS 1)
Lack of interest in dengue vector control program.
The Hanoi Preventive Medicine Centre’s dengue control program report in 2016 stated that the participation of local government authorities in dengue vector control programs was limited. The interest for medical work of WPCs was not sufficient, depending on the leadership of the WPC chairman.
When a new chairman of WPC takes up the duty, everything has changed. He said that there is no need to do this work (dengue vector control program) (FGD with health staff of WHS 2)
Barrier from WHS.
Overburdened workloads.
The health staff at WHS face work overload. A WHS with only about 10 staff was responsible for around 30 national health programs.
We not only spend time to eradicate the larval breeding sites and implement dengue control program; but we also need to do a lot of things such as examination, immunization etc., or go training and making reports. We are overburdened (FGD with health staff of WHS 3)
Secondary data also indicated that the ward health staff were overburdened with the dengue vector control activity workloads. Their duty was only to instruct and monitor the community behavior. However, they reported that they need to directly find and exterminated the larval breeding sites by themselves in each household because the householder did not do that after several times of communication and hand-on training. So even when they efficiently used the time, efforts, and human resources available, they still certainly do not have enough capacity to go to all households.
Furthermore, the health sector was still perceived as the responsible party for all dengue vector control and larval eradication efforts by both local authorities and the community. This means that they did not believe they had to share the burden of this work—hence not providing relief to the health staff.
The community leaders still said that this work is for health station…Many times in the field for larval eradication, they (community) said we must tip off the things. So, it’s very difficult for us to provide health education…You can think that how to help them clean the stuffs in many residency clusters with only six health staff (FGD with health staff of WHS 1)
Lack of communication skill.
Another point to be mentioned is that the health staff at the grassroots level need to strengthen their communication skills, focusing on persuading and working with communities because the report from the Hanoi Preventive Medicine Center also pointed out that health workers at the ward level were new with little experience. Through observation and qualitative data, the health staff were perceived to be too young to have experience in convincing communities to implement larval eradication regularly.
The ward health force is young, most of them are young. They are very enthusiastic, however, when they come to work with people in the community, it’s hard to convince them…The health workers need to have qualification and being trained to improve the persuading skills while working with community. When the health staff can show off their authority, it will be valuable at that time (IDI with the vice chairman of WPC 1)
Barrier from mass organizations and community leaders.
The mass organizations and community leaders are lacking in enthusiasm. Although they played a role as a supportive force in the dengue vector control program, however, their contribution in that role was insignificant.
Frankly speaking, the role of mass organizations, for example women’s union, youth union in some wards is still only doing for show as a movement. They haven’t promoted their active role (IDI with health staff of Dong Da district health centre).
According to the report of the Dong Da district health centre, some community leaders have not been enthusiastic to cooperate actively with the health staff. They also have not promoted their responsibility in dengue vector control programs. However, in fact, this lack of support is because of the low incentive for them while participating in the dengue vector control program and their concurrent responsibilities.
I think the caring with community leaders on allowance and spiritual issues is lacking, so they were unenthusiastic. The community leaders are retired elderly and have other works like meetings with WPC or caring their grandchildren whereas they complained about lot of overlapping works. For sure the allowance is too low for them (FGD with health staff of WHS 3)
Barrier from community.
The secondary and qualitative results showed the low awareness and readiness of the citizens. This lack of knowledge and preparedness also has been the result of ineffective community engagement, even though the respondents reported that citizens’ current knowledge about DF has improved compared with the past.
They knew that dengue fever is a very dangerous disease. Therefore, the people’s awareness in the community has been improved. In the past, their awareness was low but now it’s high (FGD with health staff of WHS 2)
Low awareness and bad practice.
Based on the results, it can be deduced that community awareness is not perceived to be at an adequate level. Some parts of communities still have low awareness on prevention methods of DF. They are mainly the short-term residents who come to Dong Da district for working and studying.
For those who are permanent residents in the ward; their participation is very positive and supportive but in contrast, the cooperation of temporary residents or students who rent the house to live has not been well on preventive activities (IDI with vice chairman of WPC 2).
They spend time for learning and doing other activities and have no time for regular cleaning.
I’m their neighbour but I haven’t ever met them. They go out all days. When they return, they close the door immediately. They also don’t know who I am so that I can remind them. I also don’t have responsibility, even I talk to them but I don’t know whether they listen and do it or not… Maybe they know about that but they don’t notice. They think they only live temporarily (FGD1 with the citizen of ward 1)
In addition, most immigrants with half-urban half-rural characteristics gather in the urban area and spend most of their time earning. They were also usually not available when health staff tried communicating. Hence, subjects such as these are considered to have not kept their personal hygiene well and not worried about dengue vector control. According to the Dong Da district health center’s official report on the dengue control program in the first 5 months of 2017, more than half (84/165) of dengue cases belonged to the student groups, whereas the other tenants accounted for 13% (21 cases) in total. The other cases which accounted for 36% were from the groups of officials, construction workers, retired people, and children. Among them, one group with a high percentage of dengue infection of 25% was that of officials with a high level of education (41 cases). This group also still has risky behaviors such as using water containers that can cause larvae to grow, growing vegetables or raising poultry on the terrace, and planting many bonsai and rockery.
There has a lot of rich families who planted the bonsai. But they left the caring work for their caretaker. Therefore, the larvae were born from the water of bonsai rockery without fishes. A lot of them didn’t use fish (IDI with vice chairman of WPC 3)
Furthermore, some community’s attitude on dengue vector control was still subjective, neglected, and dependent on the health staff. They personally think that if they live in a clean house with less breeding sites, they will not get the disease. Or they know that the WHS will come to their home for spraying every year before the dengue season, so they do not take any preventive measures for DF.
They said to us that I do whatever I like in my house. If I get the disease, I will suffer it myself (FGD with health staff of WHS 4)
The people still wait for the clean-up campaigns or when the outbreaks occur and the health staff will come to implement larval eradication for them…Their awareness is not changed. They don’t want to do the measures for larval extermination (IDI with health staff of Dong Da district health centre).
They also have not cooperated and followed the health staff’s instructions for dengue vector control.
For example, in recent clean-up campaign, there was one family that has 20 water tanks containing the larvae but they didn’t cooperate and let the dog out to bite my health staff. We must run away…We educated them a lot but they didn’t follow. They weren’t scared. When we talked to them, they agreed to do it. But when we return for surveillance, they still didn’t do so (IDI with head of WHS 1)
Lack of readiness and activeness.
Also, people in the community did not have mutual responsibility with the thought of “everybody’s business is nobody’s business”
In a tenancy, many persons use the same uncovered water tank, so nobody has a sense of responsibility thoroughly (IDI with former vice chairman of WPC 1).
Secondary data indicated that Dong Da district is an inner district with a variety of construction projects from both public and private builders such as apartments for tenants or public hospitals and even aerial railway. During the construction process, besides the lack of awareness and knowledge on sanitation and hygiene of workers who normally come from other provinces, some families would move away from the public construction projects and leave their unused things. Furthermore, the big public construction projects also contained many kinds of wastes. Hence, it became the ideal place for larval breeding sites during the rainy season.
The families that went away right after the public constructions’ compensation are the area consisting of waste or water containers for their daily use. So now, no one cleans the water containers and no one collects the wastes for larval extermination (IDI with health staff of Hanoi Preventive Medicine Centre)
Moreover, there were existing public places such as cemeteries with empty vases on the graves inside residential areas (Lang Thuong ward) or temples, pagodas with many vases and bonsai trees, or abandoned houses (Lang Thuong and Khuong Thuong wards) that lack human resources to eliminate potential breeding sites.
The specific characteristics of Dong Da district at the present are the existing of a graveyard in the middle of residency area; each tomb has a vase stuck by cement to avoid the thief. When it rains, the vase was filled up with water and nobody took care of it. The next factor is that Dong Da has numerous temples and pagodas with hundreds of vases or the bonsai or rockery (Hòn non bộ). People come for religious practice (including put flowers and water into the vases) a lot, especially in the first and fifteenth day of lunar month. So, if those temples or pagodas didn’t clean up after that by themselves, our health staff aren’t adequate to do that work for them (IDI with health staff of Dong Da district health centre).
There are several abandoned houses like a house next to mine. There was nobody living and it locked for almost ten years. Hence it couldn’t be entered whereas there are many dirty wastes in the garden. It’s a spot everyone forgot that is difficult to control (FGD 1 with the citizen of ward 3).
These are the main reasons why all stakeholders were cooperating in dealing with these difficulties of dengue vector control and proposing specific community engagement strategies to address the issue together. But some people tend to accept the situation. In addition, qualitative results showed that communication on dengue vector control was not extensive and novel enough to attract serious attention from the communities.
The residency clusters don’t go to check regularly, so, the dengue outbreaks still exist for years. Due to the high population density in our ward with populous tenants, the communication work of health station has not been thorough to each cluster or tenancy. Even some families have many rental rooms, therefore, the communication work on dengue control haven’t been penetrated for those families and their tenants (FGD 1 with citizen of ward 3)
Using loudspeakers was the only way to spread health information frequently; however, it seemed that this did not work properly. Other methods would be implemented when the dengue season approached. Hence, information coverage was not broad enough for the large scale of the population.
The loudspeakers broadcast continuously but I can’t hear it clearly (FGD 1 with citizen of ward 1)
People asked that many houses can’t listen. Sometimes the loudspeakers were broken. The common problems that people complained were less loudspeakers and unclear sound… The communication by loudspeakers is bad (FGD with health staff of WHS 1)
Besides, the communication measures were not new, leading the community to be disinterested with the repeated messages.
If communication was only conducted in normal way, it will be very boring. So, I think that we can organize the game, for example, whoever collect the wastes most will be exchanged into gifts like the fish for placing into the water tanks… (FGD 2 with citizen of ward 3)
Barrier on budget.
One of the most important barriers for community engagement is the limited budget. The budget was allocated at the central level of the health sector and then allocated to lower levels. However, it is usually low and perceived as inadequate to undertake the duties required.
Those communication sessions (for community leaders and citizen) organized by budget of district health centre. We need the allocated budget for implementation (FGD with health staff of WHS 3)
Although the WPC also assists the WHS and mass organizations on financial matters, however, it is only a small amount. Shortage of money led to the limitations of necessary sources for prevention, such as chemistry of Abate or fishes and community communication materials.
Of course, there is available budget for this activity from upper level but it’s very limited amount of money, so I have to tell that the WPC still support the finance, but it is only used for essential works. If it is utilized for working months by months, it will be a lot of troubles (IDI with the vice chairman of WPC 4).
The respondents also pointed out that allowance for people participating in dengue vector control events is too low for health staff and the members of mass organizations and relevant stakeholders.
Actually; the members of steering committee have worked very hard but in the payment aspect, it is called only a tiny allowance…For instance, a head of residency cluster who goes to 100 households in 3 days is paid 30.000 VND (1.32$), it means the money is very not worth (IDI with vice chairman of WPC 3).
If the budget increases, the interaction between WPC and the stakeholders will be better. The participants work hard but the allowance is too little, therefore, nobody certainly feel happy. The health staff only receive 50.000 VND (2.19$) per working day in clean-up campaign (IDI with head of WHS 2).
Barrier on policy environment.
Lack of detailed guidelines.
In the dengue vector control program, although policy documents were promulgated quite adequately by the Ministry of Health and other relevant partners, the guidelines of policies was not detailed and clear enough.
For dengue fever, Ministry of Health had the Decision number 3711 on dengue prevention and control and there is one Circular on financial matter. These are two backbones beside many directive documents that were issues monthly. The policy system is quite well. It will be good if the regulations of MOH were implemented well; however, those regulations still have some issues on unclear guidelines. Policy document need to be ensured that 100 people understand the same but in reality, the Southern apply in one way and the Northern apply in other way. It is general and debatable (IDI with health staff of Hanoi Preventive Medicine Centre).
Low enforcement effort.
Without the detailed guidelines, the policy enforcement on dengue vector control programs is also weak. For example, the Decree number 176/2013 of the Vietnamese Government on sanctioning of administrative violation in the health domain indicated that those who refuse carrying out or have not carried out the preventive measures for personal protection on disease control according to health staff’s instructions will be warned or punished with fines. Nevertheless, this drastic measure was not implemented until now, and not everyone knew about this. Also, most of the respondents admitted that enacting the punishment is very hard and unnecessary.
For penalty, there was no detailed policy. It should be mainly based on health communication and mobilization. The punitive implementation is hard because there has no clear policy document on disease control and dengue control is a communication work (IDI with the vice chairman of WPC 2)
For instance, when the people throw the waste on the sidewalk not inside the home bin; and from those wastes, when it rains, the larval and mosquitos were born. So, it is very hard… People shouldn’t be punished if they throw the waste wrongly because it is also a difficult process (FGD 2 with the citizen of ward 3).
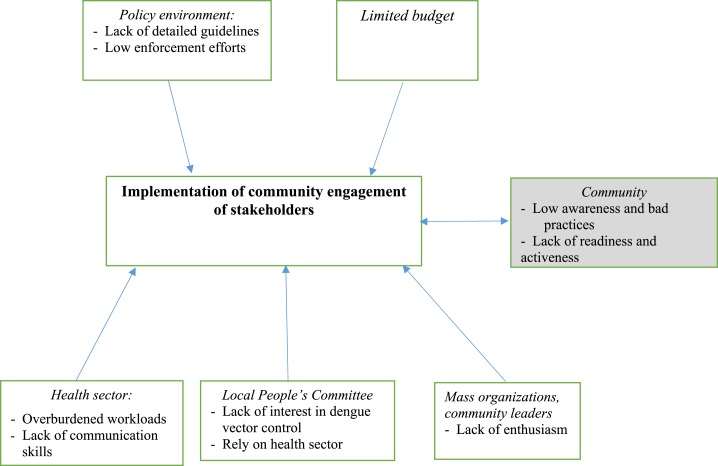
In summary, the barriers affecting the implementation of community engagement in a dengue vector control program in Dong Da district is shown in Figure 2.
Figure 2.
Barriers to effective community engagement activities in a dengue vector control program in Dong Da district. This figure appears in color at www.ajtmh.org.
DISCUSSION
The study findings showed that barriers to effective community engagement were varied from stakeholders and policies to the budget and resources. These barriers were quite similar with those found in Cuba, one of the world’s last remaining socialist republics with a political system like that in Vietnam. In Cuba, community engagement was also the decisive strategy to achieve the success of dengue vector control programs.12,31,32 Despite Cuba’s success in community participation in dengue vector control programs, the Andrade’s analysis still showed similar barriers of low awareness of community and lack of commitment and budget from the government.32 The community empowerment intervention in Cuba focused on five participatory processes: capacity building, community dengue surveillance, social communications, behavioral change, and participatory evaluation.31 For this research in Hanoi city, the dengue vector control programs conducted were lacking in the important parts of behavioral change and participatory evaluation. This finding can be explained by the unchanged practices in dengue vector control in the communities in our study. This issue was perceived as the most important factor affecting the community engagement activities of stakeholders. In addition, there is a prominent difference between our study population and Cuba’s study population that can influence behavior change in dengue vector control. Their routine Aedes aegypti control programs involved the enforcement of mosquito control legislation through the use of fines.8 Singapore also enacted anti-Aedes legislation for vector control.4 However, in our study setting and in the context of Vietnam in general, it had not been implemented and enforced strongly. Policy environment is a vital part to support all partners in any health program to complete their functioned roles. It will be the foundation for stakeholders to get involved in the joint work. So, these findings suggest that the policymakers should develop detailed guidelines to better support the enforcement of the policy environment. Regarding the lack of government commitment, Andrade’s analysis emphasized the political will of shared responsibility of local governments and citizens. It became the motivation to foster intersectoral collaboration and mobilize the participation of numerous stakeholders in community-based intersectoral initiatives for the control and prevention of dengue, including an integrated health-care system with effective models of family doctors, the network of mass organizations (Committees for the Defense of the Revolution, Federation of Cuban Women, Popular Councils, and Municipal Assemblies), school boards, and community leaders. This cooperative approach demonstrated that vector-borne disease such as DF cannot be seen as the exclusive responsibility of the health sector.32 The small task forces were created and scaled up in many study settings, namely, “community working groups,” to control A. aegypti by promoting specific behavioral change and reducing environmental risks through social communication strategies and intersectoral local government activities. The local task forces including all stakeholders at the neighborhood level were evaluated to be good and led to effective government–community partnership in dengue vector control activities.12,33 Besides Cuba, Wai et al.’s study in Myanmar, Ibarra et al.’s study in Ecuador, and Ladner et al.’s recent qualitative study in Brazil indicate that there needs to be more support for dengue outbreak prevention programs from the government because political commitment from government authorities was determined as an essential condition.14,34,35 And the government authorities were evaluated as important actors in the dengue vector control program. In Vietnam, it was mentioned in Nam et al.’s36 case study when they started implementing a new project with an integrated approach of community mobilization, behavior change, and biological control for dengue. In fact, a government leader was the head of health programs at all administrative levels. If they are truly concerned about health protection for the community, they would engage effectively in health activities with other stakeholders. Therefore, our findings recommend that government authorities need to be more responsible for this work with active support from relevant stakeholders, especially in the health sector. In terms of the barriers of enthusiasm of people from mass organizations and relevant stakeholders, there was a different finding between our study and Sanchez’s case study in Cuba; it was the activeness of community leaders. Their role in the study sites of Cuba was important although they delivered the information to community members and assisted in the establishment for communication and social mobilization at local levels.16 This finding was contrary to our result as the community leaders were not enthusiastic to participate in the dengue vector control programs. In fact, some of them were dengue collaborators in the past, but they concurrently took on other responsibilities in their family and society. In addition, they were normally the elderly who were too old to do the work which required them to travel a lot in their area, and also did not have enough financial support or reasonable allowance. Therefore, this situation is understandable.
As we know that dengue vector control is affected by complicated epidemiological elements such as rapid urbanization, high population density and immigration, and climate change, these elements need a long-term synchronized plan with multi-sector effort to resolve the problem. It could make the dengue vector control program become harder to successfully implement; therefore, it leads to ignorance of stakeholders as they accept that it cannot be dealt with soon. These factors were reported in previous articles.34,37 Only the factor of complex areas, such as cemeteries with empty vases on the grave inside residential areas or temples and pagodas with many vases, is quite unique because of the traditions and customs of most Vietnamese people who follow Buddhism. With the economic development, people in Vietnam follow the trend of decorating their house with bonsai, but they have not taken care of the negative impacts which bonsai can bring. Therefore, a warning about transmission of dengue from this habit is required in the communication campaigns.
From to Cuba’s experience, the active mobilization of the community should start with local identification of problems and needs.9 Although the researchers tried to figure out the community needs and expectations to improve the effectiveness of community engagement strategies for the promotion of behavior change in vector control, still in the FGDs with the communities in our study, the participants could not identify clearly what they expected to improve the dengue situation for themselves and the community in general. The response reflected more on how to support the communication strategies that make people in the community change their bad behavior. However, when we asked about the needed communication measures, they only mentioned the old ones that dengue vector control program had carried out already. Such top-down communication and deployment on dengue and its vector without active community involvement does not result in a behavioral change.6 The communication channels about DF in Dong Da district are varied, including direct communication from ward health staff, integrated meetings of PC and mass organizations/unions, distribution of leaflets to households, and use of loudspeakers. Among the communication channels, the most effective one is direct consultation of health staff. The use of loudspeakers is not good enough to improve coverage nor raise the awareness of citizens. Because of its ineffectiveness, the speaker system could be a supporting measure for health communication. However, there was a necessity to find better measures to improve knowledge and practice on dengue vector control activities of people in the community. Therefore, we recommend a series of studies to explore the community needs and the adoption of new communication methods , such as using a social media platform with the highest number of users in Vietnam, to deliver dengue information or for the pupils or students; it is more interesting for them to participate in the program by collecting waste in exchange for gifts like fishes to put it in jars and water tanks. Furthermore, using text messages to remind householders about dengue vector control activities at their home every week can be a good measure for behavior change in the community. Also, there is a need to improve community skills for problem identification by themselves.
The shortage of financial support in a health problem might be the most difficult factor to deal with. It is a great concern in many other countries.14,15,19,36,38,39 In our study context, health staff or people from mass organizations and relevant stakeholders normally had a low basic wage. They would not receive more allowance even if work harder to fulfill their tasks in the dengue vector control program. Therefore, they would do their job in a regular way; no more no less, with the little budget from WPC and WHS. This matter is different with Toledo’s research in Cuba, where community working groups consisting of 10–20 family doctors received no financial incentives,10,31 but with high trust and high wage in their study context. Therefore, it is proposed that some strategies related to a resource mobilization approach should be applied to adapt the hard situation in developing countries such as Vietnam. Besides, other ways to inspire the stakeholders’ participation in dengue vector control program need to be carried out such as handing over the certificate of recognition for active citizenship to people from mass organizations and relevant stakeholders to encourage their spirit in tackling the mutual concerns of their community.
This study has several limitations. The findings may not be generalizable to other parts of Vietnam as this was an urban setting. The data collected in the rural communities may give different results compared with the data collected in the urban wards. The results can also differ between districts in one city, between provinces in one country, and between countries. It may be generalized to urban settings in Hanoi city and other cities in Vietnam or countries with similar context of political structures. As mentioned before, some stakeholders such as ward health staff and representatives of mass organizations have not openly expressed their views on the WPC’s role. However, we attempted to minimize this bias by conducting more unstructured interviews with several ward health staff unofficially to get better validity of answers. In addition, there is a gap between what the community perceives as important and what the efforts needed to effectively control the dengue vector, leading to unawareness of other possible options. For example, monitoring and evaluation are important aspects in dengue vector control, but they seemed to underestimate this component. Weak monitoring and evaluation at local levels could present significant barriers leading to difficulties in community engagement strategies.17
To sum up, the study showed many barriers to engage communities in dengue vector control programs in the urban area of Hanoi city. Those negative factors include the lack of interest and dependent attitude in the health sector on the local People’s Committee; lack of enthusiasm of mass organizations and community leaders; overload and lack of communication skills from the health sector; low awareness and readiness from the community; lack of detailed policy guidelines and low enforcement of related policy; and a limited budget. It is recommended that creating some programs and communication campaigns with resource mobilization will be needed to improve the awareness and participation of stakeholders, especially the challenged communities in the current resource-limited context of developing countries, focusing on immigrants and people having high risk behaviors of planting bonsai. The health staff also need more training on soft skills of behavioral change communication to easily convince the community members. Detailed guidelines should be developed with a feasible punitive policy related to DF. This punitive policy should be carefully discussed and a consensus with the community developed on its type, feasibility, and enforcement before issue to hopefully make people change their behaviors that cause DF risks. Moreover, investing more budget from the government is also needed to motivate the WPC workers more efficiently and mobilize others to join dengue vector control programs. The encouragements also need to be done to motivate the active participation of stakeholders of mass organizations and heads of residency clusters. Further studies and experiments should be conducted in a variety of settings, both urban and rural, to explore more on novel communication methods to improve community engagement.
Acknowledgments:
The American Society of Tropical Medicine and Hygiene assisted with publication expenses.
REFERENCES
- 1.Bhatt S, et al. 2013. The global distribution and burden of dengue. Nature 496: 504–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO , 2014. Dengue. Available at: http://www.wpro.who.int/mediacentre/factsheets/fs_09032012_Dengue/en/. Accessed January 30, 2017.
- 3.Shepard DS, Undurraga EA, Halasa YA, Stanaway JD, 2016. The global economic burden of dengue: a systematic analysis. Lancet Infect Dis 16: 935–941. [DOI] [PubMed] [Google Scholar]
- 4.WHO , 2012. Global Strategy for Dengue Prevention and Control 2012–2020. Geneva, Switzerland: World Health Organization, 43 Available at: https://entity/denguecontrol/9789241504034/en/index.html. Accessed January 30, 2017. [Google Scholar]
- 5.Saskatoon Health Region , 2012. A Framework for Community Engagement in Primary Health. Available at: https://www.saskatoonhealthregion.ca/locations_services/Services/Primary-Health/Documents/SHR%20framework%20for%20community%20engagement.pdf. Accessed January 30, 2017. [Google Scholar]
- 6.Clinical Translational Science Awards Consortium , 2011. Principles of Community Engagement. Rockville, MD: US Goverment Printing Office. [Google Scholar]
- 7.Parks W, Lloyd L, 2004. Planning Social Mobilization and Communication for Dengue Fever Prevention and Control: A Step-by-Step Guide. Geneva, Switzerland: World Health Organization, 138. [Google Scholar]
- 8.Toledo ME, Baly A, Vanlerberghe V, Rodríguez M, Benitez JR, Duvergel J, Van der Stuyft P, 2008. The unbearable lightness of technocratic efforts at dengue control. Trop Med Int Health 13: 728–736. [DOI] [PubMed] [Google Scholar]
- 9.Toledo ME, Vanlerberghe V, Baly A, Ceballos E, Valdes L, Searret M, Boelaert M, van der Stuyft P, 2007. Towards active community participation in dengue vector control: results from action research in Santiago de Cuba, Cuba. Trans R Soc Trop Med Hyg 101: 56–63. [DOI] [PubMed] [Google Scholar]
- 10.Vu Sinh N, Marchand R, Tran Van T, Nguyen Van B, 1997. Dengue vector control in Viet Nam using Mesocyclops through community participation. Dengue Bull 21: 96–104. [Google Scholar]
- 11.Pérez-Guerra CL, Zielinski-Gutierrez E, Vargas-Torres D, Clark GG, 2009. Community beliefs and practices about dengue in Puerto Rico. Rev Panam Salud Pública 25: 218–226. [DOI] [PubMed] [Google Scholar]
- 12.Toledo Romani ME, Vanlerberghe V, Perez D, Lefevre P, Ceballos E, Bandera D, Baly Gil A, Van der Stuyft P, 2007. Achieving sustainability of community-based dengue control in Santiago de Cuba. Soc Sci Med 64: 976–988. [DOI] [PubMed] [Google Scholar]
- 13.Tana S, Umniyati S, Petzold M, Kroeger A, Sommerfeld J, 2012. Building and analyzing an innovative community-centered dengue-ecosystem management intervention in Yogyakarta, Indonesia. Pathog Glob Health 106: 469–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wai KT, Htun PT, Oo T, Myint H, Lin Z, Kroeger A, Sommerfeld J, Petzold M, 2012. Community-centred eco-bio-social approach to control dengue vectors: an intervention study from Myanmar. Pathog Glob Health 106: 461–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin H, et al. 2016. Community involvement in dengue outbreak control: an integrated rigorous intervention strategy. PLoS Negl Trop Dis 10.8: e0004919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sanchez L, Perez D, Pérez T, Sosa T, Cruz G, Kouri G, Boelaert M, Van der Stuyft P, 2005. Intersectoral coordination in Aedes aegypti control. A pilot project in Havana city, Cuba. Trop Med Int Health 10: 82–91. [DOI] [PubMed] [Google Scholar]
- 17.Toledo ME, et al. 2011. Evidence on impact of community-based environmental management on dengue transmission in Santiago de Cuba. Trop Med Int Health 16: 744–747. [DOI] [PubMed] [Google Scholar]
- 18.Heintze C, Garrido MV, Kroeger A, 2007. What do community-based dengue control programmes achieve? A systematic review of published evaluations. Trans R Soc Trop Med Hyg 101: 317–325. [DOI] [PubMed] [Google Scholar]
- 19.Horstick O, Runge-Ranzinger S, Nathan MB, Kroeger A, 2010. Dengue vector-control services: how do they work? A systematic literature review and country case studies. Trans R Soc Trop Med Hyg 104: 379–386. [DOI] [PubMed] [Google Scholar]
- 20.WHO , 2016. Vietnam. Dengue Factsheet. Available at: http://www.wpro.who.int/vietnam/topics/dengue/factsheet/en/. Accessed January 30, 2017. [Google Scholar]
- 21.Minh An DT, Rocklöv J, 2014. Epidemiology of dengue fever in Hanoi from 2002 to 2010 and its meteorological determinants. Glob Health Action 7: 23074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Thuy NTT, Linh NN, Quyen PD, Thu LTH, Cam NN, Mai LTQ, 2016. Dengue sitution in Hanoi, Viet Nam, between 2000 to 2015. Vietnam J Prev Med 26: 83. [Google Scholar]
- 23.Duong TN, Cam NN, Duoc VT, 2013. Epidemiological situation of dengue hemorrhagic fever in Ha Noi, 2006–2011. Vietnam J Prev Med 23: 58. [Google Scholar]
- 24.Hanh DTK, Binh NTT, Anh NTL, Cam NN, 2016. Epidemiological characteristics of dengue fever in Hanoi from 2004 to 2014. Vietnam J Prev Med 26: 25. [Google Scholar]
- 25.Hoan DB, Cam NN, 2012. Status and Related Factors of Dengue Outbreak Control in Hanoi City. Master thesis, Hanoi University of Public Health. [Google Scholar]
- 26.Huyen NP, Anh LTK, 2015. Knowledge, Attitude and Practice on Dengue Prevention and Difficulties in Vector Control in Cau Giay District, Hanoi, 2015. Master thesis, Hanoi University of Public Health. [Google Scholar]
- 27.Thuy D, Anh LTK, 2012. Activities of Health Collaborators and Challenges in Dengue Fever Surveillance in Dong Da District, Ha Noi. Master thesis, Hanoi University of Public Health. [Google Scholar]
- 28.Toan DTT, Hu W, Quang Thai P, Hoat LN, Wright P, Martens P, 2013. Hot spot detection and spatio-temporal dispersion of dengue fever in Hanoi, Vietnam. Glob Health Action 6: 18632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Dengue Control Program in Northern Region , 2014. Surveillance Results of Dengue Fever in Northern Area in 2013. Available at: http://www.tapchiyhocduphong.vn/tin-tuc/thong-bao-dich/2014/07/81E2105F/ket-qua-giam-sat-sot-xuat-huyet-dengue-khu-vuc-mien-bac-nam-2013/. Accessed January 30, 2017. [Google Scholar]
- 30.Hanoi Preventive Medicine Center , 2017. Proposal on Dengue Control Program in Hanoi in 2017. Hanoi, Vietnam: Hanoi Preventive Medicine Center. [Google Scholar]
- 31.Sanchez L, Perez D, Cruz G, Castro M, Kourí G, Shkedy Z, Vanlerberghe V, Van der Stuyft P, 2009. Intersectoral coordination, community empowerment and dengue prevention: six years of controlled interventions in Playa municipality, Havana, Cuba. Trop Med Int Health 14: 1356–1364. [DOI] [PubMed] [Google Scholar]
- 32.Andrade R, 2007. The Role of Community Participation in the Prevention of Dengue: A Case Study from Cuba. Spring Available at: http://summit.sfu.ca/item/2664. Accessed January 30, 2017.
- 33.Vanlerberghe V, Toledo ME, Rodríguez M, Gomez D, Baly A, Benitez JR, Van der Stuyft P, 2009. Community involvement in dengue vector control: cluster randomised trial. BMJ 338: b1959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Stewart Ibarra AM, Luzadis VA, Borbor Cordova MJ, Silva M, Ordoñez T, Beltrán Ayala E, Ryan SJ, 2014. A social-ecological analysis of community perceptions of dengue fever and Aedes aegypti in Machala, Ecuador. BMC Public Health 14.1: 1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ladner J, Rodrigues M, Davis B, Besson MH, Audureau E, Saba J, 2017. Societal impact of dengue outbreaks: stakeholder perceptions and related implications. A qualitative study in Brazil, 2015. PLoS Negl Trop Dis 11: e0005366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nam VS, Kay B, Yen NT, Ryan P, Bektas A, 2004. Community mobilization, behaviour change and biological control in the prevention and control of dengue fever in Viet Nam. Dengue Bull 28: 57–61. [Google Scholar]
- 37.Chang MS, Christophel EM, Gopinath D, Abdur RM; 2011. Challenges and future perspective for dengue vector control in the western Pacific region. Western Pac Surveill Response J 2.2: 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khun S, Manderson L, 2008. Community participation and social engagement in the prevention and control of dengue fever in rural Cambodia. Dengue Bull 32: 145–155. [Google Scholar]
- 39.Badurdeen S, et al. 2013. Sharing experiences: towards an evidence based model of dengue surveillance and outbreak response in Latin America and Asia. BMC Public Health 13.1: 607. [DOI] [PMC free article] [PubMed] [Google Scholar]