Abstract
Objective:
Self-regulation interventions encouraging daily weighing prevent weight gain in young adults; however, concerns have been raised that such interventions may have undesirable effects on eating pathology, depression, and quality of life (HRQL). The present study examined whether self-regulation interventions and self-weighing frequency were associated with these indices in normal weight individuals and those with overweight or obesity.
Methods:
Young adults (n=599), 18–35 years with a body mass index (BMI) 21.0–30.9 kg/m2 were randomized to control (C), self-regulation with Small Changes (SC) or self-regulation with Large Changes (LC). Interventions taught frequent self-weighing to guide behavioral changes. SC prescribed daily small decreases in intake and increases in physical activity. LC prescribed a 5–10 pound weight loss to buffer against anticipated gains. Psychological indices were assessed at baseline and periodically over 2 years of follow-up.
Results:
There was no evidence that the interventions increased depressive symptoms or compensatory behaviors or decreased HRQL relative to C. LC increased flexible and rigid control and SC decreased disinhibition. Results did not differ by weight status with the exception of rigid control; here, differences between LC and the other conditions were smaller among those with BMI ≥ 25. Greater self-weighing frequency over time was associated with increases in flexible and rigid control, dietary restraint, and improvements in HRQL.
Conclusions:
The self-regulation interventions and increases in self-weighing had no untoward effects. Encouraging weight gain prevention in young adults through frequent weighing and self-regulation appears to be safe for normal weight young adults and those with overweight.
Keywords: weight gain prevention, psychological outcomes, emerging adults, self-weighing
Weight gain is common in young adults (Lewis et al., 2000; Mulye et al., 2009; Nelson, Story, Larson, Neumark-Sztainer, & Lytle, 2008) yet few evidence-based weight gain prevention approaches exist (Poobalan, Aucott, Precious, Crombie, & Smith, 2010). In the Study of Novel Approaches to Weight Gain Prevention (SNAP) Trial, we demonstrated that self-regulation interventions encouraging daily weighing, comparison of weight to a target, and corrective action can prevent long-term weight gain in young adults (Wing et al., 2016). Concerns persist, however, about whether the self-regulatory nature of weight control interventions, particularly frequent self-weighing, might result in untoward psychological consequences or unhealthy weight control practices in young adults such as depressed mood or compensatory behaviors, with the greatest concerns surrounding those who are normal weight (Benn, Webb, Chang, & Harkin, 2016; Pacanowski, Linde, & Neumark-Sztainer, 2015).
The self-weighing literature generally supports the notion that frequent self-weighing is an effective weight management strategy (Crain, Sherwood, Martinson, & Jeffery, 2017; Katterman, Butryn, Hood, & Lowe, 2016; LaRose et al., 2014; Linde, Jeffery, French, Pronk, & Boyle, 2005; Pacanowski & Levitsky, 2015; Rosenbaum, Espel, Butryn, Zhang, & Lowe, 2017; Steinberg et al., 2013) that does not increase depression or other psychological symptoms (LaRose et al., 2014; Steinberg et al., 2014; Wing et al., 2007). However, most studies have examined these relationships in treatment seeking samples with overweight or obesity. Largely absent are young adults who are historically underrepresented in weight management trials (Gokee-LaRose et al., 2009; Loria, Signore, & Arteaga, 2010). Thus, conclusions about the safety of self-weighing in this developmental period are more tentative with some studies even suggesting negative outcomes including lower levels of self-esteem and higher levels of stress (Benn et al., 2016; Pacanowski et al., 2015; Quick, Larson, Eisenberg, Hannan, & Neumark-Sztainer, 2012). In community samples, some observational studies suggest that self-weighing frequency in young adults may be associated with weight preoccupation (Klos, Esser, & Kessler, 2012) and the development of binge eating and unhealthy weight control behaviors (Neumark-Sztainer, van den Berg, Hannan, & Story, 2006), particularly in women but this remains largely untested in the context of weight management treatment. Moreover, little is known about the potential consequence of prescribing self-weighing in normal weight individuals (Ogden & Whyman, 1997; Pacanowski et al., 2015; Rosenbaum et al., 2017) as part of an intervention to prevent weight gain over time.
The SNAP Trial provides an opportunity to examine the psychological impact of self-regulation interventions encouraging daily weighing on young adults including those who were normal weight and overweight at study entry. The objective of this paper is to determine whether the SNAP self-regulation interventions had any undesirable effects on participants’ levels of restraint, disinhibition, binge eating and compensatory behaviors, depression, and health-related quality of life (HRQL) and whether increases in self-weighing frequency, particularly in those participants who were not weighing frequently at study entry, were associated with adverse psychological outcomes. The impact of the interventions and self-weighing on psychological outcomes were further examined by baseline weight status (normal weight vs. overweight). It was predicted that the interventions and increases in self-weighing would not be associated with adverse psychological outcomes and that these patterns would hold true for normal weight individuals and those who were overweight at study entry.
Methods
The SNAP Trial is a 3-arm randomized clinical trial designed to compare the effects of self-regulation with small daily behavior changes, self-regulation with large periodic behavior changes, and a minimal treatment control condition on mean weight gain over an average follow-up of 3 years. The study was funded by the National Heart Lung and Blood Institute and involved 2 clinical sites (Providence, RI and Chapel Hill, NC) and a coordinating center (Winston-Salem, NC) and was approved by each Institutional Review Board (Lifespan-The Miriam Hospital IRB; UNC Chapel Hill Non-Biomedical IRB). Informed consent was obtained from all participants and a data Safety Monitoring Board provided trial oversight. The protocol and primary findings have been previously published (Wing et al., 2013; Wing et al., 2016). A brief description of the study design and measures relevant to this report of secondary outcomes is provided below.
Participants
Women and men, ages 18–35 years with a BMI between 21.0–30.9 kg/m2, were recruited from 2 clinical sites (Providence, RI and Chapel Hill, NC). Exclusion criteria included: ≥ 10-pound weight loss in the past six months, bariatric surgery, hospitalization for depression or psychiatric disorder, history of bipolar disorder, manic depression or schizophrenia, past diagnosis or treatment for anorexia or bulimia nervosa, past diagnosis or current symptoms of alcohol or substance abuse, or currently pregnant or nursing within the past 6 months or planning to become pregnant within the next 6 months. Full inclusion and exclusion criteria are reported in Wing and colleagues (Wing et al., 2013) and recruitment methods are described elsewhere (Tate et al., 2014). Participants were primarily women (78%), non-Hispanic White (74%), with a baseline BMI of 25.4 kg/m2 (Table 1).
Table 1:
Characteristics of the SNAP participants who contributed psychological data during follow-up at the time of their enrollment by intervention assignment.
| Baseline Characteristics |
Control N=198 |
Small Changes N=195 |
Large Changes N=190 |
|---|---|---|---|
| Gender Female Male |
154 (77.8%) 44 (22.2%) |
152 (78.0%) 43 (22.0%) |
150 (79.0%) 40 (21.0%) |
| Age, years 18–24.9 25–35 |
52 (26.3%) 146 (73.7%) |
57 (29.2%) 138 (70.8%) |
52 (27.4%) 138 (72.6%) |
| BMI, kg/m2 <25 ≥25 |
94 (47.5%) 104 (52.5%) |
81 (41.5%) 114 (58.5%) |
92 (48.4%) 98 (51.6%) |
| Weight, kg Mean (SD) | 71.4 (10.2) | 71.8 (11.0) | 70.7 (10.8) |
| Employment status, No. (%) Employed full time Student full time1 Other |
154 (77.8%) 9 (4.6%) 35 (17.7%) |
151 (77.4%) 23 (11.8%) 21 (10.8%) |
167 (87.9%) 10 (5.3%) 13 (6.8%) |
| Race/ethnicity African-American Non-Hispanic White Other |
17 (8.6%) 146 (73.7%) 35 (17.7%) |
24 (12.3%) 144 (73.8%) 27 (13.8%) |
21 (11.0%) 140 (73.7%) 29 (15.3%) |
| Education Not college graduate College graduate |
38 (19.2%) 160 (80.8%) |
43 (22.0%) 152 (78.0%) |
30 (15.8%) 160 (84.2%) |
Notes: Mean (Standard Deviation) or Frequency (Percent) reported.
Participants who both worked full time and were full time students are classified as working full time.
SNAP Intervention arms
Participants were randomized to one of 3 conditions: Self-regulation with Small Changes (SC), Self-regulation with Large Changes (LC), or Self-guided (Control). In brief, participants in the Small and Large Changes conditions received a 4-month initial in-person intervention (weekly meetings for weeks 1–8, monthly meetings from weeks 9–16), followed by two optional 4-week online refresher courses each year over the duration of follow up. The interventions were grounded in self-regulation theory (Carver & Scheier, 1982), and participants were taught to use the scale to self-weigh daily to evaluate their progress and determine whether corrective action was necessary to prevent weight gain. In Small Changes, behavioral goals included increasing steps by 2000 steps per day and reducing intake by 100 kcal/day. If weight gain over baseline level was observed, SC participants were taught to add additional small changes to reverse these gains. In Large Changes, participants were encouraged to create a 5–10 pound weight loss buffer in the first 4 months of the program through a reduction of 500–1000 kcals/day and an increase in physical activity to ≥250 min/week of moderate-to-vigorous intensity PA (MVPA), which was designed to offset future anticipated weight gains. If weight exceeded their baseline weight at any time point, LC participants were advised to return to these calorie goals to reverse this gain. Participants in the Control group attended one in-person group session, where they received general information on weight gain in young adults and an overview and publicly available websites for both the Small and Large Changes approaches; they were encouraged to choose the approach that was best suited to their personal goals. All participants received a quarterly newsletter via email, and feedback on all assessment measures throughout the trial.
Measures
Participants were assessed by blinded research staff at baseline and over an average of 3 years of follow-up for the main trial; the full assessment battery is described elsewhere (Wing et al., 2013). This analysis focuses on measures of eating pathology (i.e., restraint, disinhibition, binge eating, compensatory behaviors,) psychological outcomes (i.e., depressive symptomatology, heath related quality of life), and self-weighing frequency that were collected at baseline, month 4, 1-year and 2-years; methods for assessing the constructs of interest are detailed below. Participants received a $50 honorarium for each follow-up assessment.
Restraint and disinhibition:
The Eating Inventory (TFEQ; Stunkard, 1988), a 51-item self-report instrument, was used to assess dietary restraint (e.g., degree of conscious control exerted over eating behaviors; range from 0–21) and disinhibition (e.g., susceptibility to loss of control over eating; range 0–16). Flexible and rigid control were also captured with these items (Westenhoefer, 1991). Flexible control is characterized by a balanced approach to eating (e.g., taking smaller portions to control weight, engaging in healthy compensation) and is associated with better weight management outcomes, while rigid control is characterized by an all-or-nothing inflexibility around dietary rules (e.g., strict calorie counting, with guilt following if calorie-dense foods are consumed) that is associated with poor weight outcomes and more binge eating (Westenhoefer, Stunkard, & Pudel, 1999).
Binge eating and compensatory behaviors:
Participants complete a questionnaire adapted from the Questionnaire on Eating and Weight Patterns (Spitzer, 1993) and used in Look AHEAD (Gorin et al., 2008) that assesses the frequency of binge eating episodes accompanied by loss of control. Additional questions assessed the frequency of compensatory behaviors including vomiting, diuretics, fasting, or exercising more than one hour to control weight.
Depressive symptomatology:
The 20-item Center for Epidemiologic Studies Depression Scale (CES-D; Turvey, Wallace, & Herzog, 1999), is a well-validated self-report questionnaire, with higher scores representing more depressive symptoms.
Health-related quality of life:
The General Health Index, a one-item question from the CDC’s Health-Related Quality of Life measure (Measuring Healthy Days, 2000) required participants to report whether in general their health is excellent (1), very good (2), good (3), fair (4), or poor (5).
Self-weighing frequency:
Frequency of self-weighing was assessed with a single item asking participants how frequently they weighed themselves. Response options include: several times a day, daily, a few times a week, weekly, once a month, less than once a month to never.
Analytic Approach
Analyses examined psychological indices over time by intervention group controlling for baseline level, clinic, time from randomization, gender, age, education, race/ethnicity, and baseline BMI. Mixed effects models were fitted to the longitudinal data over time and linear contrasts were used to compute means at 2 years, which were compared with Wald tests. The prevalence of binge eating and compensatory behaviors at 2 years was contrasted among groups using logistic regression with baseline prevalence added the above list of covariates. Tests of interactions were used to assess for differences in relationships among participants grouped by baseline BMI. Associations between daily weighing and the psychological indices over time were assessed using mixed effects models, with daily weighing included as a time-varying ordinal covariate. Inverse probability weighting was used to assess the sensitivity of results to missing data (Weuve et al., 2012). This was based on a logistic regression to predict missing data at year 2 with predictors drawn from baseline psychological measures and other characteristics we report.
Results
The present analyses include 583 (97%) of the 599 participants enrolled in the trial, excluding only 16 individuals who did not contribute psychological data during follow-up: 2.0% of the Control participants, 3.6% of the Large Changes participants, and 2.5% of the Small Changes participants (p=0.61). Overall, 91% and 87% provided at least some psychological data at years 1 and 2, respectively.
Psychological Symptoms at Baseline
At study entry, there were no significant differences on any of the psychological parameters among conditions (Table 2). Overall, participants reported low levels of depressive symptoms and judged their health to be in the very good to good range. Moderate levels of restraint and disinhibition were reported, consistent with other weight management trials (JaKa et al., 2015; Teixeira et al., 2015). Less than 8% of the sample endorsed having one or more binge episodes in the six months prior to the trial and few participants (6%) reported engaging in any compensatory behaviors. Sixteen participants met criteria for obesity (BMI≥30 kg/m2) and were equally distributed among treatment groups (p=0.68).
Table 2:
Psychological characteristics (at the time of their enrollment and change from baseline to 2 years) of the SNAP participants by intervention assignment.
|
Baseline Characteristics |
Intervention Assignment |
p-value |
||
|---|---|---|---|---|
| Control N=198 |
Small Changes N=195 |
Large Changes N=190 |
||
| CES-D symptoms Baseline Δ BL to 2 year |
5.67 (4.85) 1.68 (0.50) |
5.65 (5.20) 0.60 (0.51) |
5.94 (4.50) 1.73 (0.51) |
0.81 0.20 |
|
Eating Inventory Flexible Control Baseline Δ BL to 2 year Rigid Control Baseline Δ BL to 2 year Restraint Baseline Δ BL to 2 year Disinhibition Baseline Δ BL to 2 year |
6.49 (2.40) 0.39 (0.18)a 7.12 (3.07) 0.35 (0.21)a 10.49 (1.97) 0.61 (0.19) 9.34 (2.50) 0.07 (0.17)a |
6.45 (2.36) 0.59 (0.19)a 6.94 (2.77) 0.22 (0.21)a 10.57 (1.91) 0.53 (0.19) 9.55 (2.48) −0.78 (0.17)b |
6.56 (2.29) 1.27 (0.19)b 6.95 (3.05) 1.75 (0.21)b 10.31 (1.85) 1.16 (0.19) 9.07 (2.46) −0.03 (0.17)a |
0.91 0.002 0.80 <0.001 0.41 0.04 0.17 <0.001 |
| HRQL - General health index Baseline Δ BL to 2 year |
2.48 (0.78) 0.04 (0.06) |
2.46 (0.75) −0.04 (0.06) |
2.48 (0.72) −0.11 (0.06) |
0.95 0.24 |
| Binge episodes at least 1/week Baseline 2 year Compensatory Behaviors * Baseline 2 year |
7.6% 6.4% 7.6% 9.4% |
6.3% 3.8% 5.1% 1.2% |
9.2% 11.7% 4.2% 5.5% |
0.56 0.02 0.33 0.29 |
Notes: Mean (Standard Deviation) or Frequency (Percent) are reported with covariate-adjustment for baseline characteristics: age, body mass index, education, gender, race/ethnicity, and clinic.Subscripts are used to identify pairwise differences that reach Bonferroni-corrected p<0.05.
At least one of vomiting, use of medicines, fasting, or exercising>1 hour
Change in Psychological Symptoms over 2 Years for Intervention and Control Conditions
There was no evidence that either the SC or LC interventions increased depressive symptomatology or impacted health-related quality of life over the 2-year follow-up period (Table 2) relative to Control. Some differences did emerge between conditions in regards to restraint and disinhibition. Specifically, the Large Changes group experienced greater increases in both flexible and rigid control over time compared to both Small Changes and the Control group. In contrast, Small Changes experienced greater decreases in disinhibition over time compared to Large Changes and the Control group. There was some evidence that the three groups had different changes in restraint and binge eating over time, but none of the differences between pairs of intervention conditions were large enough to reach statistical significance under Bonferroni correction. Compensatory behaviors remained infrequent (less than 8%) with no differences over time between conditions (p=.29). The pattern of results did not differ by initial weight status with the exception of rigid control where differences between the Large Change versus other groups were smaller (yet in the same direction) among those with BMI ≥ 25 than those with BMI < 25 (interaction p=0.04 data not reported).
Relation between Self-Weighing and Psychological Symptoms
The association between frequency of self-weighing during the trial and psychological symptoms across conditions in those participants who were weighing once per week or less at study entry was examined. Greater weighing frequency during the trial was associated with increases in flexible and rigid control, restraint, and improvements in health-related quality of life (Table 3; Figure 1). There were no associations between self-weighing frequency and depression, disinhibition, binge eating, or compensatory behaviors and no differences in patterns between BMI groups (all interactions p>0.15). Inverse probability weighting was used to assess the sensitivity of Table 3 results to missing data: this did not alter the statistical significance of any relationships.
Table 3:
Relationship between concurrent daily weighing and psychological indices during follow-up in participants whose baseline self-weighing was once per week or less.
| Psychometric Indices |
Never (3.75%)* |
<1 per month (5.05%) |
<1 per week (7.76%) |
Once per week (11.97%) |
Several times per week (28.65%) |
≥ Once each day (42.82%)** |
P value for trend |
|---|---|---|---|---|---|---|---|
| CESD | 8.39 (0.83) | 6.78 (0.70) | 6.65 (0.55) | 6.70 (0.45) | 7.61 (0.35) | 6.10 (0.36) | 0.22 |
| Flexible Control | 6.22 (0.28) | 6.38 (0.23) | 7.00 (0.18) | 7.29 (0.15) | 7.59 (0.12) | 8.07 (0.12) | <0.001 |
| Rigid Control | 6.61 (0.32) | 7.14 (0.26) | 7.28 (0.21) | 7.38 (0.17) | 7.82 (0.14) | 7.99 (0.14) | <0.001 |
| Restraint | 10.49 (0.28) | 10.97 (0.23) | 11.10 (0.19) |
11.14 (0.15) | 11.37 (0.12) | 11.56 (0.12) | <0.001 |
| Disinhibition | 9.14 (0.27) | 8.66 (0.22) | 8.83 (0.17) | 8.76 (0.14) | 9.00 (0.11) | 8.84 (0.12) | 0.84 |
| General Health | 2.65 (0.10) | 2.57 (0.08) | 2.47 (0.06) | 2.40 (0.05) | 2.35 (0.04) | 2.18 (0.04) | <0.001 |
| Binge eating | 6.8% (3.1%)) | 6.2% (2.6%) |
8.9% (2.1%)) |
5.1% (1.7%) |
5.4% (1.3%) | 2.7% (1.3%) | 0.06 |
| Compensatory Behaviors | 6.4% (3.3%) | 3.3% (2.7%) |
5.0% (2.2%) |
5.5% (1.8%) |
6.7% (1.4%) | 6.5% (1.4%) | 0.41 |
Notes: Covariate adjustment for intervention group, baseline level, clinic, time from randomization, gender, age, race/ethnicity, education, and baseline BMI.
Percentage of visits over follow-up time among all participants providing reports on self-weighing
3.75% of participants reported weighing more than once per day.
Figure 1.
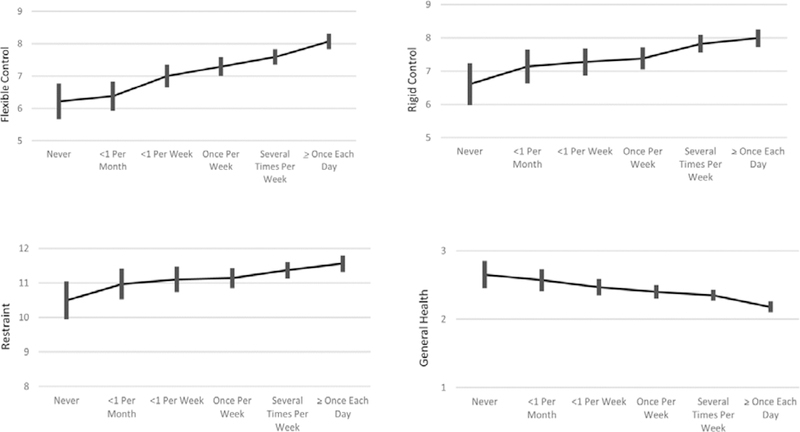
Relationship between concurrent daily weighing and psychological indices during follow-up in participants whose baseline self-weighing was once per week or less. Notes: Means +/− standard errors are presented with covariate adjustment for intervention group, baseline level, clinic, time from randomization, gender, age, race/ethnicity, education, and baseline BMI.
Discussion
This study examined whether participation in self-regulation interventions with an emphasis on self-weighing and corrective actions to prevent weight gain was associated with adverse psychological outcomes in young adults. Over a two-year follow-up period in the SNAP trial (Wing et al., 2016), there was no evidence that the self-regulation interventions exacerbated depressive symptoms or compensatory behaviors or had any other untoward effects on other psychological indices in either normal weight individuals or those who were overweight at baseline. Rather, the interventions tended to be associated with increases in restraint and improvements, not worsening, in disinhibition and binge eating behavior regardless of initial weight status. Only a few group differences emerged; these included greater increases in flexible and rigid control in the Large Changes intervention compared to both the Small Changes intervention and the Control group and greater decreases in disinhibition in Small Changes compared to the other two conditions. The Large Changes intervention encouraged periodic bouts of weight loss to buffer against anticipated weight gains over time, thus the higher levels of restraint that were observed in that condition likely reflect the emphasis on caloric restriction as a weight loss method. Such increases in restraint are common in weight loss trials (e.g, Gokee-LaRose, Gorin, & Wing, 2009) and high levels of restraint are associated with successful weight loss maintenance (e.g., LaRose, Leahey, Hill, & Wing, 2013). While these changes in restraint are believed to be positive consequences of the intervention, under certain conditions increases in rigid control and dietary restraint may lead to unhealthy weight control practices (e.g., Jacobi et al., 2004; Polivy, 1996). In contrast, the Small Changes condition promoted small daily changes a means of preventing weight gain. It is possible that participants perceived this approach to weight management as more flexible given the daily discrete changes as opposed to adherence to a calorie goal, which would be consistent with the smaller increases in control and greater decreases in disinhibition observed here.
The associations between self-weighing frequency and psychological outcomes mirrored the intervention effects; in those who were not weighing regularly at study entry, more frequent self-weighing during the follow-up period was associated with increases in restraint, flexible and rigid control, and health-related quality of life and had no impact on depressive symptoms, disinhibition, binge eating, or compensatory behaviors. These findings add to a growing literature suggesting that self-weighing is a beneficial self-regulatory strategy with no discernable negative consequences for individuals who are actively seeking to manage their weight and who do not have a history of anorexia or bulimia (LaRose et al., 2014; Steinberg et al., 2014; Wing et al., 2007). The present study extends this work by focusing on young adults and including both normal weight individuals and those who were overweight.
Limitations of the study include the use of self-report measures to assess psychological outcomes; these measures are well established and psychometrically sound but do not provide clinical diagnoses for conditions such as depression and binge eating. Moreover, study results should not be generalized to young adults who have a history of eating disorders as individuals who reported being diagnosed or treated for anorexia or bulimia were not eligible to participate in the trial. Individuals with a history of anorexia or bulimia may respond differently to self-weighing (Pacanowski et al., 2016) and the present study did not examine these risk factors. The sample was also predominantly female and non-Hispanic White; more research is needed to see if the same pattern of results is found in a more diverse sample. Also, while a major goal of both interventions was to teach and reinforce self-weighing as the cornerstone of a self-regulation approach, the study design does not allow attribution of psychological changes to self-weighing in isolation because this strategy was part of the overall intervention package. It is also worth noting that while the results largely confirmed the null hypothesis, it is possible that differences do exist that were not detected. Strengths of the study include a randomized design, the two-year follow-up period, and excellent retention rates. The focus on young adults fills an important gap in the obesity prevention literature, as does the inclusion of both normal weight individuals and those who are overweight.
In sum, study findings give increased confidence in the safety of using a self-regulation based weight gain prevention approach in young adults that encourages daily self-weighing and corrective action. That young adults can benefit from these intervention approaches not just in terms of weight gain and disease prevention (Wing et al., 2016; Wing et al., 2017) but also in regards to their quality of life and psychological outcomes should assuage concerns about putative negative effects of frequent self-weighing in this age group, particularly among those who are normal weight and without a history of anorexia or bulimia.
Acknowledgments
FUNDING:NIH/NHLBI U01HL090864, U01HL090875
Footnotes
DISCLOSURE: Dr. Tate is a member of the Scientific Advisory Board for Weight Watchers International.
CLINICAL TRIAL REGISTRATION: clinicaltrials.gov NCT 1183689
References
- Benn Y, Webb TL, Chang BP, & Harkin B (2016). What is the psychological impact of self-weighing? A meta-analysis. Health Psychol Rev, 10(2), 187–203. doi: 10.1080/17437199.2016.1138871 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carver CS, & Scheier MF (1982). Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull, 92(1), 111–135. [PubMed] [Google Scholar]
- Crain AL, Sherwood NE, Martinson BC, & Jeffery RW (2017). Mediators of Weight Loss Maintenance in the Keep It Off Trial. Ann Behav Med. doi: 10.1007/s12160-017-9917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Zwann M (2001). Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 25(Suppl 1), S51–5. [DOI] [PubMed] [Google Scholar]
- Gokee-LaRose J, Gorin AA, Raynor HA, Laska MN, Jeffery RW, Levy RL, & Wing RR (2009). Are standard behavioral weight loss programs effective for young adults? Int J Obes (Lond), 33(12), 1374–1380. doi: 10.1038/ijo.2009.185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokee-Larose J, Gorin AA, & Wing RR (2009). Behavioral self-regulation for weight loss in young adults: a randomized controlled trial. Int J Behav Nutr Phys Act. 16, 6:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Niemeier HM, Hogan P, Coday M, Davis C, DiLillo VG, . . . Yanovski SZ (2008). Binge eating and weight loss outcomes in overweight and obese individuals with type 2 diabetes: results from the Look AHEAD trial. Arch Gen Psychiatry, 65(12), 1447–1455. doi: 10.1001/archpsyc.65.12.1447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobi C, Hayward C, de Zwaan M, Kraemer HC, & Agras WS (2004). Coming to terms with risk factors for eating disorders: Application of risk terminology and suggestions for a general taxonomy. Psychological Bulletin, 130, 19–65. [DOI] [PubMed] [Google Scholar]
- JaKa MM, Sherwood NE, Flatt SW, Pacanowski CR, Pakiz B, Thomson CA, & Rock CL (2015). Mediation of Weight Loss and Weight Loss Maintenance through Dietary Disinhibition and Restraint. J Obes Weight Loss Ther, 5(2). doi: 10.4172/2165-7904.1000253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katterman SN, Butryn ML, Hood MM, & Lowe MR (2016). Daily weight monitoring as a method of weight gain prevention in healthy weight and overweight young adult women. J Health Psychol, 21(12), 2955–2965. doi: 10.1177/1359105315589446 [DOI] [PubMed] [Google Scholar]
- Klos LA, Esser VE, & Kessler MM (2012). To weight or not to weigh: the relationship between self-weighing behavior and body image among adults. Body Image, 9(4):551–4. doi: 10.1016/j.bodyim.2012.07.004. [DOI] [PubMed] [Google Scholar]
- LaRose JG, Fava JL, Steeves EA, Hecht J, Wing RR, & Raynor HA (2014). Daily self-weighing within a lifestyle intervention: impact on disordered eating symptoms. Health Psychol, 33(3), 297–300. doi: 10.1037/a0034218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- LaRose J, Leahey TM, Hill JO, & Wing RR (2013). Differences in motivations and weight loss behaviors in young adults and older adults in the National Weight Control Registry. Obesity, 21, 449–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis CE, Jacobs DR Jr., McCreath H, Kiefe CI, Schreiner PJ, Smith DE, & Williams OD (2000). Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol, 151(12), 1172–1181. [DOI] [PubMed] [Google Scholar]
- Linde JA, Jeffery RW, French SA, Pronk NP, & Boyle RG (2005). Self-weighing in weight gain prevention and weight loss trials. Ann Behav Med, 30(3), 210–216. doi: 10.1207/s15324796abm3003_5 [DOI] [PubMed] [Google Scholar]
- Loria CM, Signore C, & Arteaga SS (2010). The need for targeted weight-control approaches in young women and men. Am J Prev Med, 38(2), 233–235. doi: 10.1016/j.amepre.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Measuring Healthy Days. (2000). Atlanta, Georgia: Centers for Disease Control and Prevention [Google Scholar]
- Mulye TP, Park MJ, Nelson CD, Adams SH, Irwin CE, & Brindis CD (2009). Trends in Adolescent and Young Adult Health in the United States. Journal of Adolescent Health, 45(1), 8–24. doi: 10.1016/j.jadohealth.2009.03.013 [DOI] [PubMed] [Google Scholar]
- Nelson MC, Story M, Larson NI, Neumark-Sztainer D, & Lytle LA (2008). Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity (Silver Spring), 16(10), 2205–2211. doi: 10.1038/oby.2008.365 [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, van den Berg P, Hannan PJ, Story M. Self-weighing in adolescents: helpful or harmful? Longitudinal associations with body weight changes and disordered eating. J Adolesc Health. 2006;39:811–818 [DOI] [PubMed] [Google Scholar]
- Ogden J, & Whyman C (1997). The Effect of Repeated Weighing on Psychological State. European Eating Disorders Review, 5(2), 121–130. doi: [DOI] [Google Scholar]
- Pacanowski CR, & Levitsky DA (2015). Frequent Self-Weighing and Visual Feedback for Weight Loss in Overweight Adults. J Obes, 2015, 763680. doi: 10.1155/2015/763680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacanowski CR, Linde JA, & Neumark-Sztainer D (2015). Self-Weighing: Helpful or Harmful for Psychological Well-Being? A Review of the Literature. Current Obesity Reports, 4(1), 65–72. doi: 10.1007/s13679-015-0142-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacanowski CR, Pisetsky EM, Berg KC, Crosby RD, Crow SJ, Linde JA, . . . Peterson CB (2016). Self-weighing behavior in individuals with eating disorders. International Journal of Eating Disorders, 49(8), 817–821. doi: 10.1002/eat.22537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polivy J (1996). Psychological consequences of food restriction. Journal of the American Dietetic Association, 96(6): 589–92. [DOI] [PubMed] [Google Scholar]
- Poobalan AS, Aucott LS, Precious E, Crombie IK, & Smith WC (2010). Weight loss interventions in young people (18 to 25 year olds): a systematic review. Obes Rev, 11(8), 580–592. doi: 10.1111/j.1467-789X.2009.00673.x [DOI] [PubMed] [Google Scholar]
- Quick V, Larson N, Eisenberg ME, Hannan PJ, & Neumark-Sztainer D (2012). Self-weighing behaviors in young adults: tipping the scale toward unhealthy eating behaviors? J Adolesc Health, 51(5), 468–474. doi: 10.1016/j.jadohealth.2012.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum DL, Espel HM, Butryn ML, Zhang F, & Lowe MR (2017). Daily self-weighing and weight gain prevention: a longitudinal study of college-aged women. J Behav Med. doi: 10.1007/s10865-017-9870-y [DOI] [PubMed] [Google Scholar]
- Spitzer RY,S; Marcus M. (1993). The Questionnaire on Eating and Weight Patterns-Revised (QEWP-R). New York: New York: New York State Psychiatric Institute. [Google Scholar]
- Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, & Ward DS (2013). The efficacy of a daily self-weighing weight loss intervention using smart scales and e-mail. Obesity (Silver Spring), 21(9), 1789–1797. doi: 10.1002/oby.20396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg DM, Tate DF, Bennett GG, Ennett S, Samuel-Hodge C, & Ward DS (2014). Daily self-weighing and adverse psychological outcomes: a randomized controlled trial. Am J Prev Med, 46(1), 24–29. doi: 10.1016/j.amepre.2013.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stunkard AJM,S (1988). Eating Inventory Manual. New York: Psychological Corporation. [Google Scholar]
- Tate DF, LaRose JG, Griffin LP, Erickson KE, Robichaud EF, Perdue L, . . . Wing RR (2014). Recruitment of young adults into a randomized controlled trial of weight gain prevention: message development, methods, and cost. Trials, 15, 326. doi: 10.1186/1745-6215-15-326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teixeira PJ, Carraca EV, Marques MM, Rutter H, Oppert JM, De Bourdeaudhuij I, . . . Brug J (2015). Successful behavior change in obesity interventions in adults: a systematic review of self-regulation mediators. BMC Med, 13, 84. doi: 10.1186/s12916-015-0323-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turvey CL, Wallace RB, & Herzog R (1999). A revised CES-D measure of depressive symptoms and a DSM-based measure of major depressive episodes in the elderly. Int Psychogeriatr, 11(2), 139–148. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J (1991). Dietary restraint and disinhibition: is restraint a homogeneous construct? Appetite, 16(1), 45–55. [DOI] [PubMed] [Google Scholar]
- Westenhoefer J, Stunkard AJ, & Pudel V (1999). Validation of the flexible and rigid control dimensions of dietary restraint. Int J Eat Disord, 26(1), 53–64. [DOI] [PubMed] [Google Scholar]
- Weuve J, Tchetgen EJ, Glymour MM, Beck TL, Aggarwal NT, Wilson RS (2012). Accounting for bias due to selective attrition: the example of smoking and cognitive decline. Epidemiology, 23, 119–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate D, Espeland M, Gorin A, LaRose JG, Robichaud EF, . . . Lewis CE (2013). Weight gain prevention in young adults: design of the study of novel approaches to weight gain prevention (SNAP) randomized controlled trial. BMC Public Health, 13, 300. doi: 10.1186/1471-2458-13-300 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Espeland MA, Lewis CE, LaRose JG, Gorin AA, . . . Lang W (2016). Innovative Self-Regulation Strategies to Reduce Weight Gain in Young Adults: The Study of Novel Approaches to Weight Gain Prevention (SNAP) Randomized Clinical Trial. JAMA Intern Med, 176(6), 755–762. doi: 10.1001/jamainternmed.2016.1236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Garcia KR, Bahnson J, Lewis CE, & Espeland MA (2017). Improvements in Cardiovascular Risk Factors in Young Adults in a Randomized Trial of Approaches to Weight Gain Prevention. Obesity (Silver Spring), 25(10), 1660–1666. doi: 10.1002/oby.21917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL, & Machan J (2007). STOP regain: are there negative effects of daily weighing? J Consult Clin Psychol, 75(4), 652–656. doi: 10.1037/0022-006x.75.4.652 [DOI] [PubMed] [Google Scholar]


