Introduction
Cutaneous B-cell lymphoma consists of either a primary cutaneous disease (PCBCL) or a secondary manifestation of stage IV lymphoma (SCBCL). Secondary cutaneous metastasis of a disseminated lymphoma is rare and is reported in 3% to 5% of cases.1, 2 When they occur, secondary metastases present with pink to violaceous plaques, papules, and nodules with a predilection for the scalp, face, trunk, and back.3, 4 We present a rare manifestation of SCBCL as ill-defined erythematous macules coalescing into reticular patches over the scalp and forehead. There is only 1 other report of such presentation in the published literature. In a case series of 13 patients by Massone et al,5 2 patients with secondary follicular B-cell lymphoma presented with “partly hypochromic, partly erythematous ill-defined macules over the head and forehead.” In the latter case series, the existence of disseminated lymphoma was unknown at presentation, and the patients were given the wrong clinical diagnoses before biopsy specimens were obtained. These patients were diagnosed with androgenic alopecia because of the location of patches over frontoparietal regions and associated hair loss.5 We aim to alert clinicians of this rare presentation of disseminated follicular lymphoma because it may pose a diagnostic challenge and therefore early recognition can affect clinical management.
Case report
A 62-year-old woman with a history of stage IV grade 1 to 2 follicular B-cell lymphoma diagnosed 3 years earlier presented to the dermatology clinic with a mildly pruritic patch over her frontoparietal scalp and forehead that had not changed for 3 months (Fig 1, A). She was followed regularly by hematologists at our institution, had stable disease, and was managed on a “watch and wait” protocol with no treatment. The physical examination revealed an approximately 10 cm × 15 cm ill-defined erythematous reticular patch with blanchable telangiectasias. The patient reported using clobetasol 0.05% solution twice daily on the affected area for 2 weeks, which she stopped using 1 week before presentation because of a lack of response. Because of the blanchable telangiectasias, there was a question of whether the skin findings were caused by topical steroid use; however, the duration of use did not fit the classic timeline of steroid-induced telangiectasias. In addition, the patient reported no change in the morphology of the rash with topical steroid use. Given her medical history, the presence of cutaneous lymphoma was high on the differential and a punch biopsy specimen was obtained from the frontal scalp.
Fig 1.
A, Patient at her initial visit with ill-defined erythematous macules and reticular patches with areas of blanchable telangiectasias over frontoparietal forehead. B, Patient at the 6-month follow-up visit after 4 cycles of systemic rituximab.
Histopathology and immunohistochemistry
At lower magnification, dense lymphocytic nodular infiltrates with follicular growth pattern were seen in the dermis extending into the superficial subcutaneous fat (Fig 2). These follicles were of variable size and shape, were poorly defined, and had attenuated or absent mantle zones. At higher magnification, the follicles were noted to have many centrocytes and few centroblasts. Most of the lymphocytes within follicles were CD20+ (Fig 3), CD21+, CD 10+, BCL2+, and BCL6+, and about 20% were Ki-67+. Together, the histologic and immunohistochemical findings confirmed a diagnosis of grade 1 to 2 follicular B-cell lymphoma, likely metastatic given the CD10 and BCL2 copositivity (Fig 4). The immunohistologic phenotype of cutaneous lymphoma was also nearly identical to the lymphoma seen in the patient's axillary lymph node biopsy specimen at the time of her diagnosis 3 years earlier.
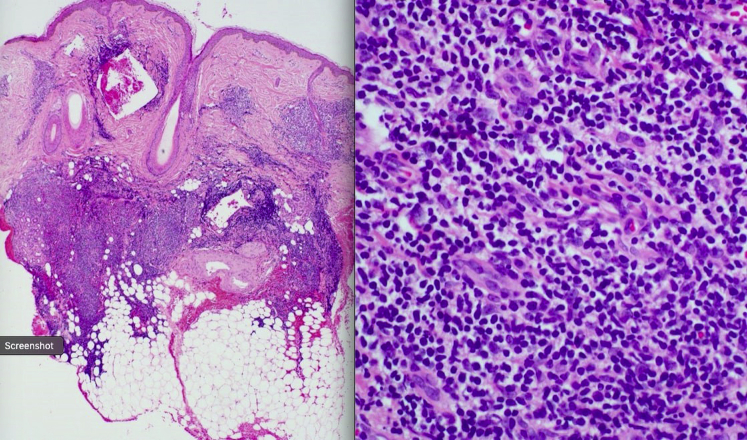
Fig 2.
Hematoxylin–eosin staining of a punch biopsy specimen at ×5 magnification showing dense nodular lymphocytic infiltrates in the dermis and superficial subcutaneous fat.
Fig 3.

CD20+ positive lymphocytic nodules (follicles) consistent with follicular B-cell lymphoma.
Fig 4.
A, CD10+ cells are seen within the follicles that are also (B) BCL2+. (Original magnification, ×5.)
Follow-up
Following the results of the cutaneous biopsy procedure, the patient was started on systemic rituximab by her hematologist. As mentioned, she had not received any form of treatment up to that point. At the 6-month follow-up visit, she had completed 4 cycles of rituximab with near complete resolution of the frontal forehead patch (Fig 1, B). She had not used any adjunct topical medications. Despite this initial treatment success, at the following visit 3 months later, she presented with a new reticular patch over her right cheek similar to the one at the time of her initial presentation. She is currently scheduled to undergo additional cycles of rituximab.
Discussion
We present a rare manifestation of SCBCL that has been reported in 1 other case series.5 This presentation is comprised of ≥1 ill-defined erythematous macule(s) coalescing into reticular patches over the forehead and scalp, which may be challenging to recognize, especially if the presence of lymphoma is unknown. In a case of a known lymphoma, recognition and subsequently obtaining a skin biopsy specimen may alter the course of treatment. As in our patient's case, disseminated follicular cell lymphoma may be managed without any treatment until systemic B symptoms or other evidence of progression occur.1 After cutaneous spread was confirmed from the biopsy procedure, the patient was started on a systemic treatment because the new cutaneous lesions represented disease progression.
In addition, the presence of cutaneous metastases may signal transformation to aggressive lymphoma subtypes.2, 6, 7 Examples of these include diffuse large B-cell lymphoma and double hit lymphoma. Double hit lymphoma is defined by presence of 2 activating translocations of BCL2 and c-MYC, which often occurs in the setting of previous low-grade lymphoma. This subtype is characterized by a resistance to most chemotherapeutics, fast systemic spread to the central nervous system and visceral organs, and a predilection to present in the skin.6, 7, 8, 9 Therefore, when the biopsy specimen is questionable for transformation, fluorescence in situ hybridization analysis can be performed, which may provide additional information on the presence of activating mutations or translocations. This was not done in our case, given the identical morphology and immunophenotype to that of the initial diagnosis from the patient's axillary lymph node biopsy specimen.
Unlike primary cutaneous lymphoma, which has a 10-year survival upwards of 90%, disseminated follicular lymphoma has a 10-year survival of 30% to 70%.1, 2 Treatment for disseminated follicular lymphoma and its cutaneous metastases is not curative, but rather meant to alleviate symptoms and disease burden. When symptoms develop and signs of progression appear, anti-CD20 therapy (rituximab) is preferred.
Rituximab with or without chemotherapy has shown to increase survival in patients with disseminated lymphoma in a systematic Cochrane review.10 As seen in our patient, cutaneous lesions are poorly responsive to topical steroids in reported cases. On the other hand, treatment of the underlying lymphoma caused the resolution of cutaneous lesions in most cases, although recurrence is common.10
Footnotes
Funding sources: None.
Conflicts of interest: None disclosed.
References
- 1.Pinter-Brown L.C. Diagnosis and management of cutaneous B-cell lymphoma. Dermatol Clin. 2015;33:835–840. doi: 10.1016/j.det.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 2.Franco R., Fernández-Vázquez A., Mollejo M. Cutaneous presentation of follicular lymphomas. Mod Pathol. 2001;14:913–919. doi: 10.1038/modpathol.3880411. [DOI] [PubMed] [Google Scholar]
- 3.López Aventín D., García M., Pedro C., Pujol R.M., Gallardo F. Miliary and agminated papules as clinical presentation of a secondary cutaneous follicular lymphoma. J Am Acad Dermatol. 2012;67:e195–e196. doi: 10.1016/j.jaad.2012.01.014. [DOI] [PubMed] [Google Scholar]
- 4.Ozaki S., Funasaka Y., Shimizu A. Follicular lymphoma presenting follicular papules in the skin: a case report. J Dermatol. 2016;44:111–113. doi: 10.1111/1346-8138.13441. [DOI] [PubMed] [Google Scholar]
- 5.Massone C., Fink-Puches R., Cerroni L. Atypical clinical presentation of primary and secondary cutaneous follicle center lymphoma (FCL) on the head characterized by macular lesions. J Am Acad Dermatol. 2016;75:1000–1006. doi: 10.1016/j.jaad.2016.05.039. [DOI] [PubMed] [Google Scholar]
- 6.Magro C.M., Wang X., Subramaniyam S., Darras N., Mathew S. Cutaneous double-hit B-cell lymphoma. Am J Dermatopathol. 2014;36:303–310. doi: 10.1097/DAD.0b013e31829beaa7. [DOI] [PubMed] [Google Scholar]
- 7.Khelfa Y., Lebowicz Y. Cutaneous presentation of double hit lymphoma. J Investig Med High Impact Case Rep. 2016;4 doi: 10.1177/2324709616642592. 2324709616642592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyaoka M., Kikuti Y.Y., Carreras J. Clinicopathological and genomic analysis of double-hit follicular lymphoma: comparison with high-grade B-cell lymphoma with MYC and BCL2 and/or BCL6 rearrangements. Mod Pathol. 2018;31:313–326. doi: 10.1038/modpathol.2017.134. [DOI] [PubMed] [Google Scholar]
- 9.Pham-Ledard A., Cowppli-Bony A., Doussau A. Diagnostic and prognostic value of BCL2 rearrangement in 53 patients with follicular lymphoma presenting as primary skin lesions. Am J Clin Pathol. 2015;143:362–373. doi: 10.1309/AJCP4SUBR4NPSPTN. [DOI] [PubMed] [Google Scholar]
- 10.Schulz H., Bohlius J., Skoetz N. Chemotherapy plus rituximab versus chemotherapy alone for B-cell non-Hodgkins lymphoma. Cochrane Database Syst Rev. 2007;4:CD003805. doi: 10.1002/14651858.CD003805.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]