Abstract
A 69-year-old man was transferred to our hospital for massive hemorrhage from a right hepatic artery pseudoaneurysm 5 months after surgery for gastric cancer. Stent-graft placement was planned to avoid fatal hepatic infarction, and a guiding sheath was advanced deeply into the tortuous and stenotic right hepatic artery beyond the pseudoaneurysm for safe deployment of a stent-graft. However, this advancement caused arterial dissection of the right hepatic artery. After the guiding sheath was pulled back, a Viabahn stent-graft was successfully advanced over a guidewire to exclude the pseudoaneurysm. We consider that a Viabahn stent-graft is more flexible than a guiding sheath and that advancing a Viabahn stent-graft directly from a proximally placed guiding sheath is safer than advancing a guiding sheath into a tortuous and stenotic abdominal artery.
Keywords: Stent-graft; Pseudoaneurysm, Arterial dissection
Introduction
Bleeding from a pseudoaneurysm is a serious complication after gastric surgery, and the effectiveness of transarterial embolization for postoperative bleeding has been reported [1]. As embolization of the hepatic artery in patients with occlusion or stenosis of the portal vein can cause life-threatening hepatic infarction, the usefulness of stent-graft placement to the hepatic artery has been also reported [2], [3]. Here, we report a case of successful stent-graft placement to the stenotic and tortuous hepatic artery after iatrogenic arterial dissection.
Case report
A 69-year-old man with gastric cancer underwent total gastrectomy, distal pancreatectomy, and splenectomy. An intraabdominal drain could not be removed due to persistent anastomotic leakage. Five months after surgery, he was transferred to our hospital for massive hemorrhage from the drain.
On admission, his vital signs were stable and hemorrhage from the drain had stopped. Contrast-enhanced CT demonstrated a pseudoaneurysm with a diameter of 30 mm at the proximal part of the right hepatic artery. CT also showed tight stenosis of the right hepatic artery adjacent to the pseudoaneurysm and tortuosity of the hepatic artery. Additionally, severe stenosis of the portal vein was observed. As the origin of the left hepatic artery was close to the pseudoaneurysm, embolization of the right hepatic artery alone was considered inadequate to stop the bleeding. We decided to perform stent-graft placement to the right hepatic artery to maintain the arterial blood flow to the liver because disruption of the hepatic arterial flow can cause fatal hepatic infarction.
Under local anesthesia, a 4-F 25-cm sheath was inserted via the right common femoral artery. The celiac artery was cannulated with a 4-F shepherd's hook catheter and celiac angiography was performed (Fig. 1). The proximal gastroduodenal artery and proximal left hepatic artery were embolized with microcoils to prevent hemorrhage due to backflow after stent-graft placement (Fig. 2). As the celiac artery arose steeply down from the aorta, a 7-F guiding sheath (Shuttle; Cook Medical, Bloomington, USA) was advanced from the left brachial artery for stent-graft placement. A 4-F flexible catheter (Fubuki; Asahi Intecc, Aichi, Japan) and 6-F guiding catheter were coaxially advanced into the common hepatic artery through the guiding sheath. The distal right hepatic artery was selected with a 0.014-inch floppy wire and a 2.0-F microcatheter that was advanced through the 4-F catheter. The 4-F catheter and 6-F guiding catheter were advanced coaxially into the right hepatic artery, crossing the stenotic proximal part (Fig. 3A). Then, the guiding sheath was advanced coaxially over the guiding catheter. Some resistance was felt when the guiding sheath crossed the stenosis. Straightening of the hepatic artery was revealed after advancement of the guiding sheath (Fig. 3B). Angiography from the guiding sheath demonstrated dissection of the right hepatic artery (Fig. 3C). Only the false lumen was opacified. The guiding sheath was carefully pulled back little by little, but it suddenly moved widely just proximal to the stenosis. The true lumen was selected by a 0.014-inch floppy wire and a 2.0-F microcatheter. Then, the floppy wire was exchanged with a 0.018-inch stiff wire (SV-5; Cordis, Miami Lakes, USA). Next, 25 mm × 6 mm and 50 mm × 7mm stent-grafts (Viabahn; Gore, Flagstaff, USA) were placed distally and proximally, respectively, with an overlap, while the guiding sheath was placed at the common hepatic artery. Some resistance was felt again when the stent-grafts crossed the stenosis, and slight straightening of the hepatic artery was revealed. Angiography revealed successful exclusion of the pseudoaneurysm and patent stent-grafts (Fig. 4).
Fig. 1.
Angiography of the celiac artery demonstrating a pseudoaneurysm (star) arising from the proximal part of the right hepatic artery (arrow). The origin of the pseudoaneurysm is close to the left hepatic artery (arrowhead) and gastroduodenal artery (curved arrow).
Fig. 2.
Angiography after embolization of the left hepatic artery and gastroduodenal artery demonstrating occlusion of both arteries (arrows). Severe stenosis of the right hepatic artery (arrowhead) is noted.
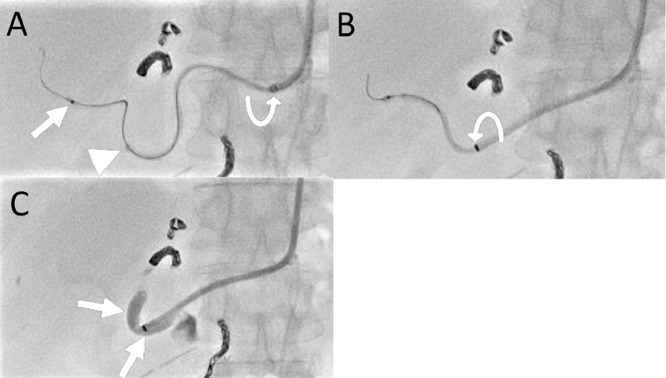
Fig. 3.
Abdominal X ray during advancement of a guiding catheter and a guiding sheath. (A) The tip of a 4-F catheter (arrow) and a 6-F diagnostic catheter (arrowhead) have passed the stenotic right proximal hepatic artery, while a 7-F guiding sheath is placed in the celiac artery. (B) After advancement of the guiding sheath (curved arrow) beyond the stenotic proximal part of the right hepatic artery, straightening of the tortuous hepatic artery is demonstrated. (C) Angiography from the guiding sheath demonstrates dissection of the right hepatic artery. Contrast medium (arrows) is pooled in the false lumen.
Fig. 4.
Angiography of the celiac artery after placement of 2 Viabahn stent-grafts (arrows) demonstrating successful exclusion of the pseudoaneurysm and the patent right hepatic artery.
Two months after the procedure, contrast-enhanced CT showed the patent stent-grafts and no hepatic ischemia. Bleeding did not recur for 3 months until death due to progression of recurrent gastric cancer.
Discussion
The Viabahn stent-graft is a highly flexible self-expandable stent-graft that is more suitable for tortuous abdominal arteries than a rigid balloon-expandable stent-graft [4]. Its usefulness for postoperative pseudoaneurysm of the abdominal arteries has been reported [5], [6]. The Viabahn stent-graft can be advanced to the hemorrhagic site after a guiding sheath or a guiding catheter has crossed the site [7], or it can be advanced over a guidewire while the sheath or catheter is placed proximally [4], [5], [6]. The latter strategy may not work in a patient with a very tortuous abdominal artery due to the lack of stability of the guiding sheath, and the former strategy may be needed. Another benefit of advancing a guiding sheath beyond the target site is that there is no risk of stent-graft dislodgement. Stent dislodgement is a serious issue when using a balloon-expandable stent, but the Viabahn stent-graft is self-expandable and the risk is expected to be very low.
In this case, we used a 4-F diagnostic catheter and a 6-F guiding catheter coaxially to safely advance a 7-F guiding sheath. However, this strategy resulted in dissection of the right hepatic artery, probably due to the stiffness of the guiding sheath, as demonstrated by straightening of the right hepatic artery after advancement of the guiding sheath. Dissection of an abdominal artery, such as the splenic artery or superior mesenteric artery has been reported in endovascular procedures using a guiding sheath or guiding catheter due to the large size and stiffness of the devices [4], [8].
We consider the Viabahn stent-graft to be more flexible and it can be advanced more safely than a guiding sheath in treatment of a pseudoaneurysm in a tortuous and stenotic abdominal artery. As mentioned above, this strategy may not work in some patients with tortuous vessels due to the lack of stability of the guiding sheath. More experience and additional techniques are needed to optimally treat these patients.
Conclusion
Placement of a Viabahn stent-graft can be achieved in a tortuous and stenotic abdominal artery. We consider advancing a Viabahn stent-graft from a guiding sheath placed proximally is safer than advancing a guiding sheath into a tortuous and stenotic abdominal artery beyond the hemorrhagic site.
Footnotes
Conflict of interest: The authors declare that they have no conflict of interest.
Funding: This study was not supported by any funding.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required.
Informed consent: Informed consent was obtained from the patient.
Consent for publication: Consent for publication was obtained for the patient's data included in the study.
References
- 1.Han K., Ahmed B.M., Kim M.D., Won J.Y., Lee D.Y., Kim G.M. Clinical outcome of transarterial embolization for postgastrectomy arterial bleeding. Gastric Cancer. 2017;20(5):887–894. doi: 10.1007/s10120-017-0700-2. [DOI] [PubMed] [Google Scholar]
- 2.Stoupis C., Ludwig K., Inderbitzin D., Do D.D., Triller J. Stent grafting of acute hepatic artery bleeding following pancreatic head resection. Eur Radiol. 2007;17(2):401–408. doi: 10.1007/s00330-006-0359-2. [DOI] [PubMed] [Google Scholar]
- 3.Wang M-Q. Stent-grafts placement for treatment of massive hemorrhage from ruptured hepatic artery after pancreaticoduodenectomy. World J Gastroenterol. 2010;16(29):3716. doi: 10.3748/wjg.v16.i29.3716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Venturini M., Marra P., Colombo M., Panzeri M., Gusmini S., Sallemi C. Endovascular repair of 40 visceral artery aneurysms and pseudoaneurysms with the viabahn stent-graft: technical aspects, clinical outcome and mid-term patency. Cardiovasc Intervent Radiol. 2018;41(3):385–397. doi: 10.1007/s00270-017-1844-5. [DOI] [PubMed] [Google Scholar]
- 5.Ching K.C., Santos E., McCluskey K.M., Orons P.D., Bandi R., Friend C.J. Covered stents and coil embolization for treatment of postpancreatectomy arterial hemorrhage. J Vasc Interv Radiol. 2016;27(1):73–79. doi: 10.1016/j.jvir.2015.09.024. [DOI] [PubMed] [Google Scholar]
- 6.Pedersoli F., Isfort P., Keil S., Goerg F., Zimmermann M., Liebl M. Stentgraft implantation for the treatment of postoperative hepatic artery pseudoaneurysm. Cardiovasc Intervent Radiol. 2016;39(4):575–581. doi: 10.1007/s00270-015-1274-1. [DOI] [PubMed] [Google Scholar]
- 7.Golarz S.R., Gable D. Use of a Viabahn stent for repair of a common carotid artery pseudoaneurysm and dissection. Ann Vasc Surg. 2010;24(4):550. doi: 10.1016/j.avsg.2009.07.037. e11-3. [DOI] [PubMed] [Google Scholar]
- 8.Kawasaki R., Miyamoto N., Oki H., Yamaguchi M., Okada T., Sugimura K. Aspiration therapy for acute superior mesenteric artery embolism with an angled guiding sheath and guiding catheter. J Vasc Interv Radiol. 2014;25(4):635–639. doi: 10.1016/j.jvir.2013.11.015. [DOI] [PubMed] [Google Scholar]