Abstract
Septic hip arthritis is a rare but serious disease, which is often persistent, able to transform into a chronic infection, and difficult to cure. The present study aimed to compare the midterm outcomes between the staging of a total hip arthroplasty via the Girdlestone surgery (a resection of the head and neck) and the Girdlestone combined with a cement spacer in treating chronic septic hip arthritis, as well as to compare the postsurgery efficacy and complications between the two groups. A total of 13 patients (14 total hip joints) were enrolled and retrospectively analyzed. For the stage I surgery, four patients (five hips) underwent the resection of the head and neck, and nine patients (nine hips) underwent the resection of the head and neck combined with the implantation of a bone cement spacer. After the infection was fully controlled, the patients in both groups underwent cementless total hip arthroplasties as stage II surgeries. The mean follow-up period was 24.2 months. The curative effects and complications of the patients were recorded and compared. It was found that the application of the staging arthroplasty for treating a chronic septic hip was conducive to the complete clearance of lesions. Notably, the implantation of a bone cement spacer containing antibiotics in the stage I surgery prevented joint contracture caused by a head and neck resection, reducing the risk of infection recurrence between the two stages of the operation. This effectively maintained the length of the lower limbs, simplified the stage II complete hip arthroplasty and reduced operative hemorrhage, thus achieving improved recovery of joint function after the stage II arthroplasty. The results suggested that the implantation of a cement spacer at the stage I surgery was more effective in treating chronic septic hip arthritis.
Keywords: bone cement spacer, hip joint infection, septic arthritis, two-stage arthroplasty
Introduction
Septic arthritis of the hip joint may occur in adults with a debilitating disease or sepsis at other bodily sites, but the most common cause of a hip joint infection in the adult population is the incidence of a previous surgical procedure (such as an internal fixation of a fracture or the debridement of a lesion, excluding a hip arthroplasty) (1). This kind of disease is often persistent and recalcitrant. Due to the existence of articular cartilage damage and chronic osteomyelitis, the infection may transform into chronic septic arthritis (2,3) and has a high debridement failure rate (4), which is difficult to cure and is a challenge for orthopedists.
A Girdlestone surgery involves the complete removal of a lesion via a head and neck incision, as well as a thorough debridement, which is more effective in treating chronic septic arthritis of the hip compared with the general debridement surgery (5). Subsequently, a complete hip arthroplasty can be performed following the infection is effectively controlled. However, patients usually appear with shortened extremities, arthralgia, and other symptoms after the two-stage surgery due to a soft tissue contracture, which seriously affects their quality of life (6,7).
Usually, a surgical program including the removal of a prosthesis, a complete debridement, an implantation of an antibiotic cement spacer, and a subsequent total hip arthroplasty (THA) is effective for treating a periprosthetic joint infection (PJI) (7–10). Previous studies have adopted a similar staging surgical program (the incision of the head and neck combined with the implantation of a cement spacer) for treating refractory or chronic septic arthritides of the hip, which can maintain the length and function of the lower limbs and can prevent a muscle contracture prior to the stage II THA, thereby achieving excellent results (1,11–14). Nevertheless, all of the previous studies focused only on the outcomes of using a bone cement spacer in patients receiving a staging hip arthroplasty but did not compare the outcomes in patients receiving a THA after the Girdlestone procedure alone. Thus, these studies did not obtain direct evidence that proved the advantages of the spacer method over the Girdlestone surgery.
The present study aims to explore the midterm (followed-up for at least 1 year) efficacy of a two-stage THA in treating chronic septic arthritis of the hip, as well as to compare the outcomes between patients who received and did not receive a cement spacer after the incision of the femoral head and neck.
Materials and methods
Patient selection
Adult patients with chronic hip infections, who had each received a staging complete hip arthroplasty between January 2010 and January 2016 in the First Affiliated Hospital of Fujian Medical University, were retrospectively analyzed. These patients were initially diagnosed according to their disease history, clinical manifestations (local erythema, tenderness, exudation and pain) and imaging performances like disappearance of joint space and femoral head damage (Fig. 1A). All patients underwent a preoperative joint cavity puncture, as well as an intraoperative joint fluid and tissue culture. The inclusion criteria were as follows: i) A chronic sinus connected to the joint cavity; ii) the presence of pus in the joint puncture or pus and destruction of femoral head during the surgery; iii) increased (>20 mg/l) serum C-reactive protein (CRP) concentrations (detected using a Modular automated protein analyzer; IMMAGE800; Beckman Coulter, Inc., Brea, CA, USA) and positive frozen sections during the stage I surgery (numbers of white blood cells per high-power field >5); and iv) cultures of the joint punctures or intraoperative specimens yielding positive results. A positive result was considered when at least one culture yielded a strict pathogen (Staphylococcus aureus, Pseudomonas aeruginosa, Enterobacteriaceae and anaerobes) or when two cultures yielded a strain that was a skin commensal (including coagulase-negative staphylococci or Propionibacterium acnes) (15–17). The exclusion criteria were as follows: i) Patients with infections after a THA and ii) patients with incomplete clinical and laboratory information. Additionally, the following data of the patients were preoperatively collected: Cause of disease, causative organisms, comorbidities, CRP and erythrocyte sedimentation rate (ESR; detected using an Automatic ESR analyzer; Monitor-100; Vital, Puteaux, France).
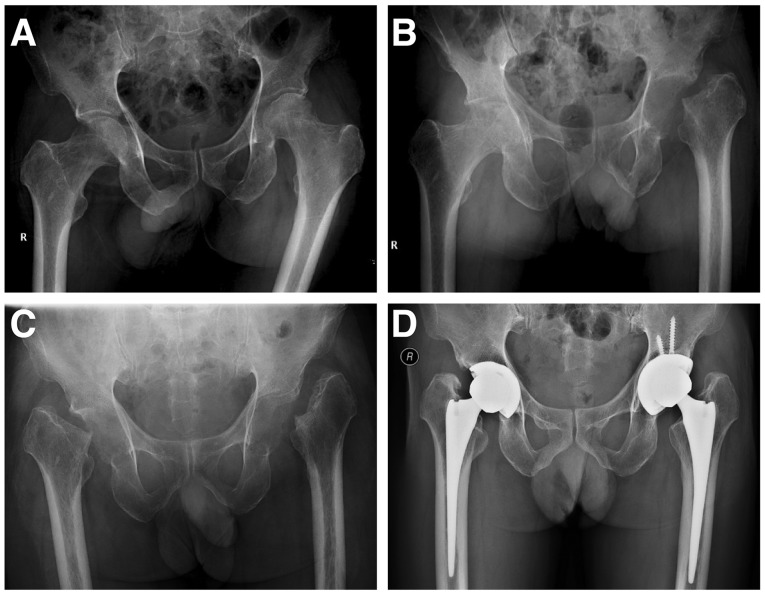
Figure 1.
Images of a patient receiving a femoral head and neck resection (case 1). (A) Male, 59 years old with bilateral hip joint pain and sinus present for 3 months, no improvement after receiving I&D and an antibiotic treatment. (B and C) The patient successively underwent resection of the head and neck of the left and right hips. Culture results revealed the presence of Burkholderia pseudomallei. After the surgery, the CRP did not decline to the normal level for a long period of time and the patient received prolonged course of antibiotics. (D) After 1 year the CRP returned to a normal level, the patient successively underwent a left and right total hip arthroplasty. During the operation it was found that soft tissue surrounding the hip joint was difficult to loosen; a large amount of scar hypertrophy and a severe operative hemorrhage were observed in the acetabulum. The postoperative bilateral lower limbs were shortened, and the hip joints had poor range of motion. CRP, C-reactive protein; I&D, incision and debridement.
Surgical procedures
All surgeries were performed using the same approaches and procedures as described below and by the same experienced surgeon. The stage I surgery was performed as follows: An incision was made at the posterolateral region of the hip joint. The purulent fluid was sucked out and sent for bacterial culture and drug sensitivity examinations. Subsequently, the articular capsule was cut open to fully expose the hip joint (the internal fixture was taken out, if present) and was followed by the removal of the destroyed head and neck of the femur. Subsequently, the proximal femur was unreamed to prevent inflammation from the reaming to the medullary cavity. The purulent pus, inflammatory tissue, detached articular surface, and scar tissue were removed. For the Girdlestone alone group, the incision was closed after the drainage tube was placed (Fig. 1B and C). For the cement spacer group, after debridement, 8 g vancomycin (Lilly, Indianapolis, IN, USA) was mixed with 80 g of bone cement (Refobacin; Zimmer Biomet, Warsaw, IN, USA), which was used to wrap two 4 mm Kirschner wire (Fig. 2B) or cement prostheses (Fig. 3) composed of a 28 mm femoral head, a 32 mm femoral neck and a 105 mm femoral stem (CM-CZ; AKMedical, Beijing, China) to make a spacer that matched the acetabular and femoral medullary cavities. The spacer was then implanted into the hip joint, which could help to maintain the normal eccentricity and tension of the gluteus medius. Finally, the incision was sutured after the drainage tube was fixed. After the surgery, the drainage tube was retained until a clear drainage fluid was observed and the drainage fluid volume was >20 ml in both groups. The selection of antibiotics was based on the preoperative or intraoperative cultures and the drug sensitivity results, while vancomycin was applied in patients without culture results. The courses of intravenous and oral administration of antibiotics depended on the clinical symptoms as well as the CRP decline. After the patients received intravenous antibiotics (Table II) for 2–4 weeks, they were switched to oral antibiotics, which included 0.6 g levofloxacin (Daiichi Sankyo Co., Ltd., Tokyo, Japan) once per day and 0.3 g rifampicin (Chengdu Tiantaishan Pharmaceutical Co., Ltd., Chengdu, China) twice per day for 1–2 months. The affected limbs were allowed to gradually perform flexion and extension activities, as well as partial loading.
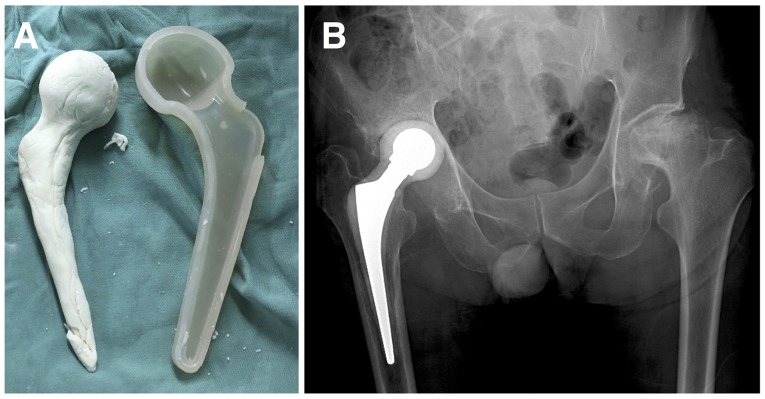
Figure 2.
Images of a patient undergoing a femoral head and neck resection and spacer treatment (Case 5): (A) Male, 62 years old, pain for 3 months after the surgical treatment of a left acetabulum fracture, with purulence found in I&D and no improvement observed after receiving antibiotics. (B) The patient underwent a head and neck resection and an implantation of a bone cement spacer after the internal fixation was removed. (C) The infection was controlled after 3 months, and the patient underwent a hip arthroplasty, with a lower degree of operative hemorrhage. After the surgery, the lengths of the lower limbs were recovered and the hip joints had a good range of motion.
Figure 3.
A small cement prosthetic was used as a skeleton to fabricate a spacer (case 6). (A) A spacer mold and (B) a fabricated spacer using a cement prosthesis as the skeleton was implanted into the body.
Table II.
Pathogen and stage I surgery.
| Case | Type of stage 1 surgery | Pathogen | Antibiotics administration after stage 1 (IV) | Length of antibiotic therapy after stage 1 (weeks) | Interval to normal CRP (weeks) | Interval to THA (months) |
|---|---|---|---|---|---|---|
| 1 | Girdlestone | Burkholderia pseudomallei | Meropenem Ceftazidime | L-24 | L-12 | L-12 |
| R-10 | R-7 | R-9.5 | ||||
| 2 | Girdlestone | Stenotrophomonas maltophilia | Meropenem | 12 | 12 | 33 |
| 3 | Girdlestone | Escherichia coli | Levofloxacin | 8 | 6 | 69 |
| 4 | Girdlestone | MRSA | Vancomycin | 6 | 5 | 24 |
| 5 | Spacer | Enterobacter cloacae | Meropenem | 6 | 4 | 3 |
| 6 | Spacer | Corynebacterium | Vancomycin meropenem Cefoperazone | 8 | 6 | 5.5 |
| 7 | Spacer | Negative | Vancomycin moxifloxacin | 8 | 4 | 4.5 |
| 8 | Spacer | Streptococcus | Vancomycin levofloxacin | 8 | 4 | 3 |
| 9 | Spacer | MSSA | Vancomycin cefuroxime | 6 | 4 | 4 |
| 10 | Spacer | Negative | Vancomycin levofloxacin | 12 | 12 | 3 |
| 11 | Spacer | MRSA | Vancomycinlinezolid | 12 | 10 | 3 |
| 12 | Spacer | MSSA | Vancomycin | 6 | 3 | 4 |
| 13 | Spacer | MSSA | Vancomycin | 6 | 5 | 6 |
L, left; R, right; CRP, C-reactive protein; THA, total hip arthroplasty; MRSA, Methicillin-resistant Staphylococcus aureus; MSSA, Methicillin-susceptible Staphylococcus aureus.
Indications for stage II surgery
When movement of the hip did not incur obvious pain and the soft tissue did not appear to be swollen, patients underwent a CRP and ESR review a total of three times, with each review occurring once every week and yielding normal results. The stage II surgery was conducted using the original approach. The antibiotic bone cement spacer was removed, followed by an intra-articular scar clearance and debridement. The patients in both groups underwent THA using bioprosthesis (Johnson & Johnson Services, Inc., New Brunswick, NJ, USA).
Evaluation indicators
Patients were assessed in terms of Harris hip scores (18) before the stage I surgery, between the two surgeries, and within the follow-up period (12.0–62.0 months; mean duration, 24.2±3.8 months) after the last surgery. The complications after the stage I surgery, the time of antibiotic applications after the stage I surgery, the interval between the stage I and stage II surgeries, the operation times, and the operative hemorrhage of the stage II surgery were recorded and the lengths of the lower extremities were postoperatively compared. In addition, the patients were reviewed using the inflammatory indicators (ESR and CRP) once every 3 months within the follow-up period, in order to monitor the recurrences of disease.
Statistical analyses
All of the data are presented as the mean ± standard error of the mean. A Mann-Whitney U test was performed to evaluate the differences between the Girdlestone alone group and the Girdlestone + cement spacer group for all of the indicators analyzed. The statistical significance threshold was set at P=0.05.
Results
Analysis of included cases
According to the inclusion criteria, 16 patients were eligible for the present study. Among these patients, three patients with incomplete clinical data were excluded. Therefore, a total of 13 patients (14 hip joints, with one case of a bilateral infection) were enrolled in the study, including 8 men and 5 women, mean age 59.3±4.3 years; range 19–79 years. The present study included 7 cases (8 hip joints) of primary hip infections, 5 cases of infections after the internal fixation of the hip fracture (4 cases were femoral neck fractures and one case was an acetabular fracture), and one case of a chronic infection after the focal cleaning of osteonecrosis of the femoral head. All of the patients complained of symptoms for >2 months (Table I). Ten patients had pain and swelling at the affected site, and two patients had pain symptoms and a sinus connected with the articular cavity. The symptoms of these patients lasted for 60–125 days (mean: 82.7±7.5 days) before the first surgery. Nine patients had a history of antibiotic use before the first surgery, while certain patients underwent incision drainages (cases 1, 3, 5, and 7) with no improvement in clinical manifestations (Table I). Beside the cases that were negative for the presence of bacterial cultures, half of the bacterial cultures of the two groups were comprised of gram-negative bacteria, which were different from the commonly found staphylococci and other positive cocci in PJI cases. On the basis of the bacterial culture results, the patients in both groups were given antibiotics, out of which two cases of negative cultures were given a combination of vancomycin and quinolones (levofloxacin; cases 7 and 10; Table II).
Table I.
Patient data (preoperative).
| Case | Age (years)/Sex | Cause of presentation | Duration of symptom (days) | Joint | Etiology | Comorbidities | Previous treatment for infection |
|---|---|---|---|---|---|---|---|
| 1 | 59/M | Pain, sinus | L-60; R-35 | Bilateral | Primary | Syphilis, osteoporosis | I&D, Cefradine |
| 2 | 54/M | Pain | 106 | Left | Primary | Gout | Aspiration |
| 3 | 61/M | Pain, sinus | 120 | Right | Femoral neck fracture ORIF | Eczema | I&D, Cefdinir |
| 4 | 67/M | Pain | 125 | Right | Primary | NIDDM | None |
| 5 | 62/M | Pain | 71 | Left | Acetabula fracture ORIF | Arterial hypertension, NIDDM | I&D, Moxifloxacin |
| 6 | 52/M | Sinus | 63 | Right | AVN focal cleaning | Cirrhosis | Cefradine |
| 7 | 55/M | Pain, sinus | 61 | Right | Femoral neck fracture ORIF | None | I&D, Cefradine |
| 8 | 77/F | Pain | 64 | Right | Femoral neck fracture ORIF | Arterial hypertension, NIDDM, PD | Cefdinir |
| 9 | 49/F | Pain | 123 | Left | Primary | None | Cefradine |
| 10 | 75/F | Pain | 100 | Right | Primary | None | Cefradine |
| 11 | 79/F | Pain | 60 | Left | Primary | None | None |
| 12 | 62/M | Pain | 90 | Right | Primary | NIDDM | None |
| 13 | 19/F | Pain | 80 | Right | Femoral neck fracture ORIF | None | Cefradine |
AVN, Avascular necrosis; F, female; I&D, incision and debridement; M, male; NIDDM, non-insulin-dependent diabetes mellitus; L, left; R, right; ORIF, open reduction internal fixation.
Pathogen and stage I surgery
For the stage I surgery, 4 patients (5 hips) underwent the resection of the head and neck (cases 1–4, hereafter referred to as the Girdlestone alone group), and 9 patients (9 hips) underwent the resection of the head and neck combined with the implantation of a bone cement spacer (cases 5–13, hereafter referred to as the spacer group). In the Girdlestone alone group, the highly pathogenic Burkholderia cepacia was cultured in one case (case 1, Fig. 1), which did not show significant complications after the stage I surgery but required a longer time duration for controlling the infection. One case had an incision sinus and infection recurrence after the surgery (case 3, Escherichia coli) and required a re-debridement and an extended anti-infective treatment. Another case had pneumonia, poor wound healing and other complications, and underwent a re-debridement (case 2, Stenotrophomonas maltophilia). The infection and complications in these three cases were under control and CRP levels were restored to a normal level after the stage I surgery in a mean of 8.4±1.5 weeks (range, 5–12 weeks). Among the patients undergoing a spacer implantation, two cases had complications. One case had a pneumonia and type I respiratory failure after the stage I surgery and was healed after treatment and underwent the stage II surgery successfully (case 6 with Corynebacterium). Another case had a spacer fracture after walking with weight loading at 3 months after the surgery and underwent the stage II surgery soon after (case 7). The mean time for CRP levels of the patients to decline to the normal level after the stage I surgery was 5.8±1.0 weeks (range 4–12 weeks), which was a shorter time period than that of the Girdlestone alone group. However, this difference was statistically insignificant. Additionally, two cases of the Girdlestone alone group who underwent a debridement after the stage I surgery suffered from poor wound healing again after the stage II surgery (cases 2 and 3) and were healed after receiving a debridement. However, all the patients in the spacer group were well healed. Signs of infection recurrence were not found in both groups until the end of the follow-up periods (Table II).
Comparison of stage II surgery and postoperative implications in two groups
After the stage I surgery, the patients in the Girdlestone alone and spacer groups were given antibiotics for 120±3.2 weeks and 8.0±0.8 weeks, respectively, but this difference in antibiotic treatment times was statistically insignificant. The mean time interval between the two surgeries was 4.0±0.4 months in the spacer group, which was a significantly shorter time interval than that in the Girdlestone alone group (29.5±10.7 months, P<0.01, Table II). The stage II arthroplasty was more difficult to perform in the Girdlestone alone group. The mean operation time was longer (124.0±13.6 vs. 105.6±7.9 min) and the incidence of a hemorrhage was increased more in the Girdlestone alone group (501.0±100.8 vs. 322.2±55.4 ml), but these differences were statistically insignificant. The Girdlestone alone group showed a more marked leg-length discrepancy after the stage II THA than the spacer group (2.8±0.6 vs. 0.8±0.2 cm, P<0.01; Table III).
Table III.
Patient data (stage II surgery and postoperative implications).
| Case | Operative hemorrhage of THA (ml) | Duration of THA operation (min) | Leg-length discrepancy after THA (cm) | Preoperative hip score | Interim hip score | Final hip score | Complication between stages | Complication after prosthesis implantation | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | L-200 | L-90 | L-2.0 | L-54 | L-74 | L-82 | 62 | ||
| R-400 | R-120 | R-2.2 | R-52 | R-72 | R-81 | ||||
| 2 | 500 | 150 | 2.2 | 51 | 75 | 84 | Pneumonia, hematosepsis, poor wound healing | Poor wound healing | 27 |
| 3 | 600 | 100 | 5.0 | 49 | 66 | 83 | Recurrence of infection, poor wound healing | Poor wound healing | 24 |
| 4 | 805 | 160 | 3.0 | 65 | 78 | 12 | |||
| 5 | 250 | 90 | 1.1 | 47 | 85 | 90 | 24 | ||
| 6 | 600 | 105 | 2.0 | 48 | 79 | 89 | Pneumonia, type-I respiratory failure | 28 | |
| 7 | 200 | 70 | 1.0 | 53 | 85 | 93 | 36 | ||
| 8 | 300 | 80 | 0.8 | 30 | 90 | 91 | Spacer fracture | 30 | |
| 9 | 200 | 147 | 0.7 | 45 | 91 | 84 | 16 | ||
| 10 | 150 | 115 | 0 | 35 | 75 | 78 | 17 | ||
| 11 | 500 | 116 | 1 | 42 | 79 | 94 | 13 | ||
| 12 | 500 | 127 | 0 | 20 | 95 | 93 | 14 | ||
| 13 | 200 | 100 | 0.5 | 25 | 88 | 88 | 12 |
L, left; R, right; THA, total hip arthroplasty.
All patients were followed up for >12 months after the stage II surgery (12.0–62.0 months), with a mean of 24.2±3.8 months (Girdlestone alone group: 31.3±10.8 months; spacer group: 21.1±2.9 months). No cases had an infection recurrence or emerging infection surrounding the prosthesis, and no cases had prosthesis loosening, a dislocation, or a fracture around the prosthesis during the follow-up periods. The mean Harris scores before the surgery were comparable between the two groups (47.8±2.5 vs. 40.7±3.1; Table IV). The Harris scores after the stage I replacement were 70.4±2.1 vs. 85.2±2.2 in the Girdlestone alone group and spacer group, respectively, which showed significant differences (P<0.01). At the last follow-up, the Harris score in the spacer group was also improved than that in the Girdlestone alone group (81.6±1.1 vs. 88.9±1.7, P<0.01; Table IV).
Table IV.
Comparison of the two surgical procedures.
| Surgical type | Operative hemorrhage of THA (ml) | Duration of THA operation (min) | Leg-length discrepancy after THA (cm) | Preoperative Harris hip score | Interim Harris hip score | Final Harris hip score |
|---|---|---|---|---|---|---|
| Girdlestone alone | 501.0±100.8 | 124.0±13.6 | 2.8±0.6 | 47.8±2.5 | 70.4±2.1 | 81.6±1.1 |
| Girdlestone + spacer | 322.2±55.4 | 105.6±7.9 | 0.8±0.2 | 40.7±3.1 | 85.2±2.2 | 88.9±1.7 |
| P-value | 0.1658 | 0.2812 | 0.0015 | 0.1783 | 0.0020 | 0.0175 |
THA, total hip arthroplasty.
Discussion
The present study evaluated the midterm efficacy of a staged complete hip arthroplasty in treating the refractory septic arthritis of the hip. The comparison of the results from the follow-up in patients undergoing different surgical procedures showed that the application of an antibiotic cement spacer in addition to a head and neck resection could better control the infection. It could also maintain the limb length more effectively, thus providing more favorable conditions for the stage II complete hip arthroplasty, compared with the head and neck resection alone.
Previous literature has reported the unsatisfactory efficacy of a head and neck resection (19). It is generally believed that the joint is unstable, shortened, and often painful after the surgery. Additionally, it is not guaranteed that there is a complete and thorough debridement (20,21). Rittmeister et al (19) reported 39 cases that underwent a head and neck resection of the hip joint and observed 67% incidence of complications and a repair rate of 44%. Charlton et al (22) found that the lower limb was shortened by an average of 30.5 mm after two resections of the head and neck; of these, 39 and 11.4% of the patients had a claudication and a dislocation after the stage II surgery, respectively.
The application of a spacer following a head and neck resection has been reported, wherein the spacer can be prefabricated or made by the surgeons during the surgery. Romanò et al (13) applied a prefabricated spacer made of gentamicin antibiotic loaded bone cement in 19 patients (20 hips). The authors found that hip arthroplasty was successfully implemented in all of the hips after a mean of 22 weeks, and only 1 case had infection recurrence during an average follow-up period of 56 months (13). Huang et al (23) used a variety of antibiotic bone cements to treat 14 cases (15 hips) with refractory septic hips and found an uncontrolled infection in only 1 case; no spacer-associated complications were observed. Among the 14 cases reported by Fleck et al (12), two died of other diseases, and two did not undergo the stage II surgery, while no case showed any sign of an infection recurrence. Shen et al (14) has questioned the traditional spacer method, they believed that an infection following hip trauma surgery was different from that of an infection following an arthroplasty. Since the infection might only involve the intra-articular soft tissue, cartilage, and subchondral bone, but not the proximal femur, the spacer with a femoral stem may lead to the involvement of the femoral medullary cavity and the spread of the infection. Thus, a spacer that does not need to be placed into the medullary cavity was used, and no infection recurrence and spacer associated complications were found during an average follow-up period of 39.6 months. Nonetheless, this kind of spacer could not achieve an axial and rotational stability that was similar to that of the traditional spacer; thus, this spacer had a higher risk of mechanical loosening and dislocation. Therefore, the conventional spacer was still adopted in the present study.
Two surgical methods were successfully used in the present study. It was found that, although the resection of the femoral head and neck could achieve a complete debridement, two patients had postoperative infection recurrences and poor wound healing, which greatly prolonged the time of antibiotic use and the interval between the two surgeries. The patients also suffered from shortened limbs and obvious dysfunctions, which may have led to great difficulties in the stage II hip arthroplasty. This may be because systemic medications did not help to achieve an effective concentration locally in patients with a poor blood supply, which led to a higher likelihood of an infection recurrence. Hsieh et al (24) used antibiotic beads locally after the Girdlestone surgery for treating a septic hip and achieved an improvement in the control of infection. For the implantation of an antibiotic bone cement spacer based on the stage I head and neck resection, a local release of antibiotics helped in controlling the infection and shortened the time of systemic application of the antibiotics. At the same time, the spacer was able to maintain the lengths and ranges of motion of the limbs (25,26). It was not necessary to loosen the scar tissue during the stage II surgery, which resulted in a lower degree of operative hemorrhage and a shortened operation time. Additionally, the postoperative limbs were shortened by no more than 1 cm, the function was fully recovered, and no joint dislocation was reported during the follow-up. The spacer, which constructed using the bone cement prosthesis, is simple and inexpensive, has improved mechanical stability (compared with the Kirschner wire as the skeleton), and enables patients to walk with weight loading in an earlier time period following surgery, thus making it conducive for a functional recovery. This was therefore used instead of Kirschner wire in the later phase.
The selection of the implant in the stage II surgery is still controversial (27). Theoretically, the loss of bone mass in the septic hip is less than that in the infection following a THA, which is beneficial to the fixation of the biological prosthesis. A cementless bioprosthesis has been reported to have a good efficacy in treating an infection following a THA (28,29). In addition, the use of a cement prosthesis has been reported to be insignificantly associated with an infection recurrence (27,30,31). Therefore, it is believed that a cementless prosthesis is a good choice for the stage II surgery for a septic hip. A bio-prosthesis was implemented in the stage II arthroplasty in most patients in this study. The results showed that the stability was immediately achieved during the surgery, no signs of loosening of the prosthesis were reported during the follow-up, and infections were well controlled in the patients. Other concerns in this study are the type and duration of antibiotic use. A systemic application of antibiotics is needed to not only control the primary foci but also prevent the hematogenous spread and infection metastasis. Despite reports that a short term application of intravenous antibiotics can also achieve the same effect as that of a long term application after spacer therapy for a refractory septic hip (23,32), retrospective studies exist that only have a small number of cases and insufficient evidence. The bacterial cultures in this study revealed mostly gram-negative bacteria. Because of insufficient data showing the ideal doses and duration of antibiotic use, the patients were given intravenous antibiotics for at least 4 weeks after the stage I surgery, and the extended application was determined according to the changes in the inflammatory indicators.
The strengths of the present study were as follows: (1) All the patients received follow-ups; (2) all the surgical procedures were performed by the same surgeon in a standard manner; and (3) two surgical methods were compared. Since the patients were selected at different time-points, those patients receiving treatment after an improvement in the prosthesis and surgical techniques may show higher efficacy (a spacer was used in the late phase), which was the limitations of the present study. Nevertheless, this was unlikely to affect the credibility of the results as the use of the spacer significantly reduced the duration of antibiotic use, improved the function of the hip joints during the surgery, and maintained the lengths of the lower limbs. This, thereby simplified the stage II surgery, achieving improved final clinical efficacy. These effects showed a significant difference between the two groups. Evidently, this study included a small number of samples and hence further statistical analysis could not be performed. Furthermore, this was a retrospective study, in which patients were not randomly grouped and received follow-ups for a relatively short time. Therefore, further studies, with more patients and a long-term follow-up period are needed to provide more convincing comparative data. In conclusion, the present study found that a staging arthroplasty was conducive for a complete debridement in treating a chronic septic hip. The implantation of a bone cement spacer containing antibiotics in the stage I surgery could effectively control infection, avoid a joint contracture caused by a head and neck resection, reduce the risk of an infection recurrence between the two stages of the surgery. It could also effectively maintain the lengths of the lower limbs, simplify the stage II complete hip arthroplasty, and reduce an operative hemorrhage. Thus, it was a more effective method for treating a chronic septic hip arthritis.
Acknowledgements
Not applicable.
Glossary
Abbreviations
- AVN
Avascular necrosis
- CRP
C-reactive protein
- ESR
erythrocyte sedimentation rate
- F
female
- I&D
incision and debridement
- M
male
- NIDDM
noninsulin-dependent diabetes mellitus
- ORIF
open reduction internal fixation
- PJI
Periprosthetic Joint Infection
- THA
total hip arthroplasty
Funding
The current study was funded by Fujian Youth Talents General Training Program (grant no. 2014-ZQN-JC-19) and the Key Clinical Specialty Discipline Construction Program of Fujian, P.R.C and the Key Clinical Discipline of Fujian Medical University (grant no. XK201106).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
WZ designed the current study. WL, XF, CZ and YX accumulated the data. WL, ZH, ZY and XF analysed the data. WL and XF drafted the manuscript. All authors read and approved the final version of the manuscript.
Ethics approval and consent to participate
This study was approved by the Ethics Committee and Institutional Review Board of The First Affiliated Hospital of Fujian Medical University (committee's reference number: [2014] 047). Informed consent was obtained from each patient before the data was collected.
Patient consent for publication
Consents regarding individual details, images, findings of physical examination and data of the surgery details were obtained from all patients.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Diwanji SR, Kong IK, Park YH, Cho SG, Song EK, Yoon TR. Two-stage reconstruction of infected hip joints. J Arthroplasty. 2008;23:656–661. doi: 10.1016/j.arth.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 2.Souza Miyahara Hd, Helito CP, Oliva GB, Aita PC, Croci AT, Vicente JR. Clinical and epidemiological characteristics of septic arthritis of the hip, 2006 to 2012, a seven-year review. Clinics (Sao Paulo) 2014;69:464–468. doi: 10.6061/clinics/2014(07)04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vukasinović Z, Spasovski D, Cobeljić G, Zivković Z. Septic arthritis of the hip in infancy-diagnostic and therapeutic possibilities. Srp Arh Celok Lek. 2006;134:77–81. (In Serbian) [PubMed] [Google Scholar]
- 4.Stutz G, Kuster MS, Kleinstück F, Gächter A. Arthroscopic management of septic arthritis: Stages of infection and results. Knee Surg Sport Traumatol Arthrosc. 2000;8:270–274. doi: 10.1007/s001670000129. [DOI] [PubMed] [Google Scholar]
- 5.Harrison MH. Robert Jones, Gathorne Girdlestone and excision arthroplasty of the hip. J Bone Joint Surg Br. 2005;87:1306. doi: 10.1302/0301-620X.16753. [DOI] [PubMed] [Google Scholar]
- 6.Malcolm TL, Gad BV, Elsharkawy KA, Higuera CA. Complication, survival, and reoperation rates following girdlestone resection arthroplasty. J Arthroplasty. 2015;30:1183–1186. doi: 10.1016/j.arth.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 7.Cui Q, Mihalko WM, Shields JS, Ries M, Saleh KJ. Antibiotic-impregnated cement spacers for the treatment of infection associated with total hip or knee arthroplasty. J Bone Joint Surg Am. 2007;89:871–882. doi: 10.2106/00004623-200704000-00026. [DOI] [PubMed] [Google Scholar]
- 8.Assmann G, Kasch R, Maher CG, Hofer A, Barz T, Merk H, Flessa S. Comparison of health care costs between aseptic and two stage septic hip revision. J Arthroplasty. 2014;29:1925–1931. doi: 10.1016/j.arth.2014.04.043. [DOI] [PubMed] [Google Scholar]
- 9.Kim YS, Bae KC, Cho CH, Lee KJ, Sohn ES, Kim BS. Two-stage revision using a modified articulating spacer in infected total knee arthroplasty. Knee Surg Relat Res. 2013;25:180–185. doi: 10.5792/ksrr.2013.25.4.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandiford NA, Duncan CP, Garbuz DS, Masri BA. Two stage management of the infected total hip arthroplasty. Hip Int. 2015;25:308–315. doi: 10.5301/hipint.5000265. [DOI] [PubMed] [Google Scholar]
- 11.Anagnostakos K, Duchow L, Koch K. Two-stage protocol and spacer implantation in the treatment of destructive septic arthritis of the hip joint. Arch Orthop Trauma Surg. 2016;136:899–906. doi: 10.1007/s00402-016-2455-3. [DOI] [PubMed] [Google Scholar]
- 12.Fleck EE, Spangehl MJ, Rapuri VR, Beauchamp CP. An articulating antibiotic spacer controls infection and improves pain and function in a degenerative septic hip. Clin Orthop Relat Res. 2011;469:3055–3064. doi: 10.1007/s11999-011-1903-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romanò CL, Romanò D, Meani E, Logoluso N, Drago L. Two-stage revision surgery with preformed spacers and cementless implants for septic hip arthritis: A prospective, non-randomized cohort study. BMC Infect Dis. 2011;11:129. doi: 10.1186/1471-2334-11-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shen H, Wang QJ, Zhang XL, Jiang Y. Novel articulating medullary-sparing spacer for the treatment of infectious hip arthritis. Orthopedics. 2013;36:e404–e408. doi: 10.3928/01477447-20130327-13. [DOI] [PubMed] [Google Scholar]
- 15.Osmon DR, Berbari EF, Berendt AR, Lew D, Zimmerli W, Steckelberg JM, Rao N, Hanssen A, Wilson WR, Infectious Diseases Society of America Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the infectious diseases Society of America. Clin Infect Dis. 2013;56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 16.Mirra JM, Amstutz HC, Matos M, Gold R. The pathology of the joint tissues and its clinical relevance in prosthesis failure. Clin Orthop Relat Res. 1976:221–240. [PubMed] [Google Scholar]
- 17.Spangehl MJ, Masri BA, O'Connell JX, Duncan CP. Prospective analysis of preoperative and intraoperative investigations for the diagnosis of infection at the sites of two hundred and two revision total hip arthroplasties. J Bone Joint Surg Am. 1999;81:672–683. doi: 10.2106/00004623-199905000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Mahomed NN, Arndt DC, McGrory BJ, Harris WH. The Harris hip score: Comparison of patient self-report with surgeon assessment. J Arthroplasty. 2001;16:575–580. doi: 10.1054/arth.2001.23716. [DOI] [PubMed] [Google Scholar]
- 19.Rittmeister M, Müller M, Starker M, Hailer NP. Functional results following Girdlestone arthroplasty. Z Orthop Ihre Grenzgeb. 2003;141:665–671. doi: 10.1055/s-2003-812402. (In German) [DOI] [PubMed] [Google Scholar]
- 20.Fenelon GC, Von Foerster G, Engelbrecht E. Disarticulation of the hip as a result of failed arthroplasty. A series of 11 cases. J Bone Joint Surg Br. 1980;62-B:441–446. doi: 10.1302/0301-620X.62B4.7430220. [DOI] [PubMed] [Google Scholar]
- 21.Petty W, Goldsmith S. Resection arthroplasty following infected total hip arthroplasty. J Bone Joint Surg Am. 1980;62:889–896. doi: 10.2106/00004623-198062060-00003. [DOI] [PubMed] [Google Scholar]
- 22.Charlton WP, Hozack WJ, Teloken MA, Rao R, Bissett GA. Complications associated with reimplantation after girdlestone arthroplasty. Clin Orthop Relat Res. 2003:119–126. doi: 10.1097/00003086-200302000-00019. [DOI] [PubMed] [Google Scholar]
- 23.Huang TW, Huang KC, Lee PC, Tai CL, Hsieh PH. Encouraging outcomes of staged, uncemented arthroplasty with short-term antibiotic therapy for treatment of recalcitrant septic arthritis of the native hip. J Trauma. 2010;68:965–969. doi: 10.1097/TA.0b013e3181af6e70. [DOI] [PubMed] [Google Scholar]
- 24.Hsieh PH, Chang YH, Chen SH, Shih CH. Staged arthroplasty as salvage procedure for deep hip infection following intertrochanteric fracture. Int Orthop. 2006;30:228–232. doi: 10.1007/s00264-005-0059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Romanò CL, Romanò D, Logoluso N, Meani E. Long-stem versus short-stem preformed antibiotic-loaded cement spacers for two-stage revision of infected total hip arthroplasty. Hip Int. 2010;20:26–33. doi: 10.1177/112070001002000104. [DOI] [PubMed] [Google Scholar]
- 26.Regis D, Sandri A, Rizzo A, Bartolozzi P. A preformed temporary antibiotic-loaded cement spacer for the treatment of destructive septic hip arthritis: A case report. Int J Infect Dis. 2010;14:e259–e261. doi: 10.1016/j.ijid.2009.04.019. [DOI] [PubMed] [Google Scholar]
- 27.Ganzoury IE, Eid AS. Two-stage arthroplasty using functional temporary prosthesis to treat infected arthroplasty and septic arthritis of the hip. J Orthop. 2015;12(Suppl 1):S86–S93. doi: 10.1016/j.jor.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fink B, Grossmann A, Fuerst M, Schäfer P, Frommelt L. Two-stage cementless revision of infected hip endoprostheses. Clin Orthop Relat Res. 2009;467:1848–1858. doi: 10.1007/s11999-008-0611-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Masri BA, Panagiotopoulos KP, Greidanus NV, Garbuz DS, Duncan CP. Cementless two-stage exchange arthroplasty for infection after total hip arthroplasty. J Arthroplasty. 2007;22:72–78. doi: 10.1016/j.arth.2006.02.156. [DOI] [PubMed] [Google Scholar]
- 30.Fehring TK, Odum S, Calton TF, Mason JB. Articulating versus static spacers in revision total knee arthroplasty for sepsis. The ranawat award. Clin Orthop Relat Res. 2000:9–16. doi: 10.1097/00003086-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Sanchez-Sotelo J, Berry DJ, Hanssen AD, Cabanela ME. Midterm to long-term followup of staged reimplantation for infected hip arthroplasty. Clin Orthop Relat Res. 2009;467:219–224. doi: 10.1007/s11999-008-0480-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rutz E, Spoerri M. Septic arthritis of the paediatric hip-A review of current diagnostic approaches and therapeutic concepts. Acta Orthop Belg. 2013;79:123–134. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.