Summary
Cardiac surgery has been shown to be associated with increased risk of acute ischemic stroke. This report presents a case of a successful mechanical embolectomy procedure to treat a patient for an acute ischemic stroke, which was caused by the cardiac embolization of a ‘foreign body’ containing debris following a redo sternotomy procedure for mitral valve replacement and tricuspid valve annuloplasty.
Keywords: Acute ischemic stroke, mechanical embolectomy, mitral valve repair, embolic debris, redo sternotomy
Introduction
Mitral valve disease is the most common cardiac valve disorder, affecting more than four million people in the United States. The definitive treatment for patients with mitral valve disease is surgical valve repair or replacement with either mechanical or biological valves.1 Among patients with severe symptomatic mitral valve disease who are not candidates for surgical repair, mitral valve replacement is the recommended treatment.1 Furthermore, bioprosthetic valves are recommended in elderly patients with a relatively low likelihood of prosthetic structural valve degeneration, thereby reducing re-surgery rates in these patients. However, mechanical prosthetic valves lead to an increased risk of thromboembolic and hemorrhagic complications along with lifelong anticoagulation therapy.2
Despite the use of embolic protection devices, several studies have shown that embolic debris from cardiac procedures can result in an acute ischemic stroke3–5 and previous case reports have demonstrated a variety of causes of embolic debris following cardiac surgery leading to an acute ischemic stroke, for example, valve tissue,6 chordae tendineae7 and calcified and collagenous tissue.8
Herein we report a case of a patient who underwent a mitral valve repair and suffered a large vessel occlusion secondary to a foreign body embolism, which was successfully treated with mechanical thrombectomy.
Case report
A 79-year-old Caucasian male had a history of coronary artery disease and severe mitral insufficiency and underwent coronary artery bypass grafting and mitral valve repair with an annuloplasty in 2009. Additionally, he had been diagnosed with chronic atrial fibrillation, type 2 diabetes, hypertension, hyperlipidemia and obstructive sleep apnea. The patient was completely independent in his activities of daily living and had evidence of recurrent severe mitral regurgitation, moderate tricuspid regurgitation and papillary fibroelastomas on the aortic valve. He underwent a redo sternotomy procedure for mitral valve replacement with a 29 mm St. Jude Medical mechanical valve, tricuspid valve annuloplasty and debridement of fibroelastoma on the aortic valve.
On the second post-operative day, the patient was noted to have left hemiparesis and progressive weakness since the procedure. An acute stroke alert was activated with the clinician initially concerned about the possibility of an intraparenchymal haemorrhage given the presence of intravenous (IV) heparin. A STAT computed tomography (CT) scan of the head did not show any acute infarction or evidence of a haemorrhage. The patient was re-examined while he was in the CT scanner room and progressive deficits were noted. The case was discussed with the neuro intensive care unit at this time, and a decision was made to proceed with digital subtraction angiography (DSA) of the head and neck.
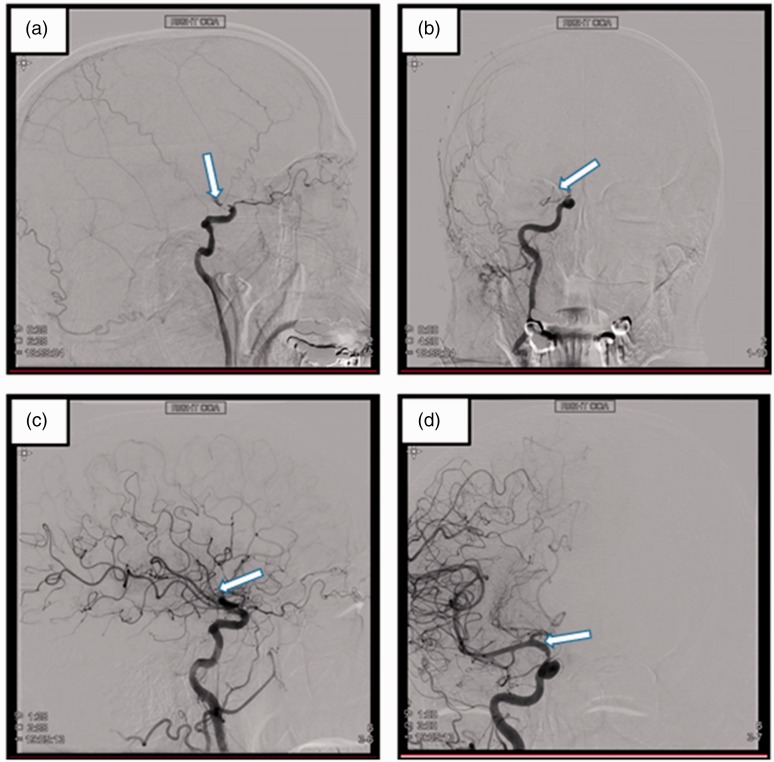
The DSA showed complete occlusion of the right internal carotid artery (ICA) distal cavernous and supraclinoid segments, with the presence of some collateral flow (Figure 1(a) and (b)). The pre-procedure National Institutes of Health (NIH) stroke scale was 16. The patient was not an IV tissue plasminogen activator candidate due to the unclear time of onset as well as recent history of major surgery. The patient underwent successful mechanical clot retrieval. A 6-French SOFIA aspiration catheter was used to make one pass in the right supraclinoid ICA to remove the embolus by mechanical embolectomy and complete revascularization (TICI 3) was achieved (Figure 1(c) and (d).
Figure 1.
Digital subtraction angiography (DSA) images pre- and post-mechanical thrombectomy. (a and b) DSA images show a filling defect in the right internal carotid artery (white arrows). (c and d) DSA images after retrieval of the embolic material from the right internal carotid artery show good subsequent flow (white arrows).
Following the procedure, the retrieved clot was collected for histological analysis and was immediately fixed in 10% phosphate-buffered formalin. The clot underwent standard tissue processing and was embedded in a paraffin block. Serial sections (3 µm) of the clot were cut using a microtome and mounted on glass slides. Representative slides from the clot were stained with hematoxylin and eosin.
A trained pathologist visually inspected the slides and noted the presence of non-human, ‘foreign body’ material contained within the clot (Figure 2). The histopathological assessment of the clot demonstrates there are cells intertwined with the ‘foreign body’ material, which we suspect could potentially be part of a sewing ring of the St. Jude Medical mechanical valve prosthesis (Figure 2(d)). The material did not bear any histological resemblance to previously reported causes of embolic debris following cardiac surgery such as valve tissue,6 chordae tendineae,7 and calcified and collagenous tissue.
Figure 2.
Gross photo and histological images of embolic debris material. (a) Gross photograph of the removed clot following the mechanical thrombectomy procedure, 1.6× magnification. (b, c and d) Histological images of the hematoxylin and eosin-stained clot sample containing the non-human ‘foreign-body’ material (black arrows) at 1.6×, 20× and 40× respectively. The presence of the ‘foreign body’ material (black arrow) along with the common acute ischemic stroke clot components of red blood cells (red arrow), white blood cells (purple arrow) and fibrin (pink arrow) is clearly visible in the 40x image (d).
Outcome and follow up
Following the procedure, the patient's strength began to improve as did his neglect. The post-procedure NIH Stroke Scale was 11.
Discussion
Acute ischemic stroke is a common complication of cardiac surgery that occurs more often during the surgical procedure. However, up to 38% of strokes occur within 2 days of surgery.9 Previous reports have demonstrated a variety of causes of embolic debris following cardiac surgery and histopathological analysis of embolic debris, captured in embolic protection devices used during cardiac procedures, demonstrated that a ‘foreign body’ was collected in 10% of trans-catheter aortic valve replacement cases. However, the origin of these foreign bodies remains somewhat unclear.10
We believe this is one of the first confirmed cases of large vessel occlusion following cardiac surgery caused by ‘foreign body’ material. The histopathological assessment of this clot demonstrates that the common components of acute ischemic stroke clots such as red blood cells, white blood cells and fibrin are intertwined with the ‘foreign body’ material. The authors suspect the ‘foreign body’ material could potentially be a part of the sewing ring of the St. Jude Medical mechanical valve prosthesis (Figure 2(d)). Therefore, it is the authors’ considered opinion that in the ‘foreign body’ material likely embolized during the procedure and over the subsequent 2 days, cells began to adhere to the material resulting in the formation of an occlusive thromboembolus. This aligns with the patient’s symptoms as he demonstrated progressive weakening over the 2 days post-surgery. One can expect that foreign-body material will not respond to IV thrombolysis, precluding its use and indicating mechanical thrombectomy alone as the optimum treatment approach for post-surgery cases in which embolization of foreign-body material is the suspected aetiology. Therefore, patients that are post-cardiac surgery should be observed closely for signs and symptoms of stroke.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Institutes of Health (R01 NS105853), Science Foundation Ireland (13/RC/2073) and our industrial partners Cerenovus.
References
- 1.Nishimura RA, Vahanian A, Eleid MF, et al. Mitral valve disease: Current management and future challenges. Lancet 2016; 387(10025): 1324–1334. [DOI] [PubMed] [Google Scholar]
- 2.Bucerius J, Gummert JF, Borger MA, et al. Stroke after cardiac surgery: A risk factor analysis of 16,184 consecutive adult patients. Annals Thoracic Surg 2003; 75: 472–478. [DOI] [PubMed] [Google Scholar]
- 3.Haider AS, Garg P, Watson IT, et al. Mechanical thrombectomy for acute ischemic stroke after cardiac surgery. Cureus 2017; 9: e1150–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Madeira M, Martins C, Koukoulis G, et al. Mechanical thrombectomy for stroke after cardiac surgery. J Cardiac Surg 2016; 31: 517–520. [DOI] [PubMed] [Google Scholar]
- 5.Anyanwu AC, Filsoufi F, Salzberg SP, et al. Epidemiology of stroke after cardiac surgery in the current era. J Thoracic Cardiovascular Surg 2007; 134: 1121–1127. [DOI] [PubMed] [Google Scholar]
- 6.Anuwatworn A, Raizada A, Kelly S, et al. Stroke with valve tissue embolization during transcatheter aortic valve replacement treated with endovascular intervention. JACC: Cardiovascular Interventions 2015; 8: 1261. [DOI] [PubMed] [Google Scholar]
- 7.Thomas MC, Delgado Almandoz JE, et al. A case of right middle cerebral artery ‘tendonectomy’ following mitral valve replacement surgery. J Neurointerventional Surg 2017; 9: e35. [DOI] [PubMed] [Google Scholar]
- 8.Fassa A-A, Mazighi M, Himbert D, et al. Successful endovascular stroke rescue with retrieval of an embolized calcium fragment after transcatheter aortic valve replacement. Circulation: Cardiovascular Interventions 2014; 7: 125–126. [DOI] [PubMed] [Google Scholar]
- 9.Svensson LG, Tuzcu M, Kapadia S, et al. A comprehensive review of the PARTNER trial. J Thorac Cardiovasc Surg 2013; 145: S11–S6. [DOI] [PubMed]
- 10.Van Mieghem N, Schipper M, Ladich E, et al. Histopathology of embolic debris captured during transcatheter aortic valve replacement. Circulation. 2013; 127: 2194. [DOI] [PubMed] [Google Scholar]