Abstract
Background:
Paediatric airway assessment remains the most challenging task before the anaesthesiologists. Recent advancement in ultrasonography techniques should now allow for accurate and descriptive evaluation of paediatric airway. To compare calculated external diameters of the endotracheal tube from physical indices of traditional formulas and predetermined by ultrasound.
Materials and Methods:
100 subjects of either sex between 12-60 months of age, undergoing various elective surgeries under general anaesthesia requiring endotracheal intubation were enrolled in the study. The transverse diameter was measured at the level of cricoids cartilage by ultrasonography. The tracheal tube was considered best fit if air leak was satisfactory at 15-20 cm H2O of airway pressure. The obtained values were compared with the values of endotracheal tube size calculated by various age, height, weight based formulas and diameter of right and left little finger. The correlation of size of Endotracheal tube by different modalities was done and Pearson's correlation coefficient was obtained.
Results:
According to Pearson's correlation there was a moderate correlation of best fit Endotracheal tube with endotracheal tube size by age based formula (r = 0.743), body length based formula (r = 0.683), right little finger based formula (r = 0.587), left little finger based formula (r = 0.587) and multivariate formula (r = 0.741). There was a strong correlation with ultrasonography (r = 0.943).
Conclusion:
Ultrasonography is a reliable method of estimation of subglottic diameter and for prediction of endotracheal tube size in children.
Keywords: Endotracheal intubation, paediatric, subglottic diameter, ultrasonography, traditional formulas
Introduction
Knowledge of the influence of the age of the child on laryngeal dimensions is essential for all practitioners who are dealing with paediatric airway. In the neonatal period the trachea is funnel shaped with upper end wider than the lower; and as the age advances it becomes cylindrical.[1] The developing airway anatomy is the main determinant for recommendation for the use of uncuffed endotracheal tubes in patients younger than 8 years.[2]
Selection of the correct endotracheal tube size is a crucial step in paediatric patients because a large sized tube may cause complications like post extubation stridor and subglottic stenosis.[3] Whereas smaller tube there will be increased gas flow resistance, aspiration risk, poor ventilation, inaccurate monitoring of end tidal gases and reintubation may also be required with a different size of tracheal tube.[4]
Different physical indices formulas used for prediction of endotracheal tube size are age based formula (Age + 16)/4,[5] body length based formula [2 + length (in cms)/30],[6] multivariate Formula (2.44 + age in year × 0.1 + height in cm × 0.02 + weigh in kg × 0.016.),[7] diameter of fifth right and left finger[8] which is measured as anterior to posterior diameter of the distal digit with the caliper to the nearest 0.1 mm. All these formulas are poor predictor of actual tracheal diameter and repeated laryngoscopies are often needed to identify the appropriate endotracheal tube size.
Readily available ultrasound devices and increasing familiarity of anaesthesiologists has made a way for consideration of this modality in the assessement of paediatric airway.[9,10]
This study was formulated in order to compare the efficacy of ultrasound with traditional formulas for estimation of correct size of endotracheal tube in paediatric age in order to minimize the repeated attempts on intubation.
Materials and Methods
After approval from Institute's Ethical and Research committee, and written and informed consent from parents/guardians, 100 pediatric subjects aged between 12-60 months of age, were included in the study. The inclusion criteria was American society of anesthesiologist (ASA) grade I, II subjects undergoing various elective surgeries under general anaesthesia and requiring endotracheal intubation.
The patients having upper respireatory tract infection, tracheal and laryngeal pathology, belonging to American society of anaesthesiologist grade III and IV, patients in whom supraglottic airway device was inserted or patient required post operative mechanical ventilation, all such children were excluded. If previous anaesthesia record revealed that the child had required an exceptionally large or small size tube the child was excluded.
Technology of ultrasonography and study methodology
The patients were kept nil per oral from 6 hrs prior to surgery for solid food and clear fluids and plain water was allowed till 2 hrs prior to surgery.
They were premedicated 2 hrs before surgery with oral midazolam 0.5-0.75mg/kg and under the influence of premedication ultrasounography was done. The subglottic diameter was assessed with high resolution B mode ultrasonography with a small footprint linear probe having frequencies 7 to 15 MHz and length 40 mm. It was positioned on the midline with their head extended and neck flexed which is known as sniffing position. Predetermined standard scanning plane was used to prevent any examination bias and artifacts.
Ultrasonography was performed by the same experienced radiologist. He began with the true vocal cords localisation which is seen as paired hyperechoic linear structures which moves on respiration and swallowing. Then probe was moved caudally to visualize the cricoid arch in order to avoid any confusion between the cricoid cartilage and the tracheal ring. The measure of tracheal diameter was taken as the transverse air column diameter measurement done at the cephalic half of the cricoid cartilage which is narrower than the caudal part [Figure 1]. The larynx situated below the hyoid bone, and the ring shaped trachea which is located inferior to the cricoid cartilage, were easily visualised by ultrasound in vertical or transverse section. The radiologist had no further involvement in the study.
Figure 1.
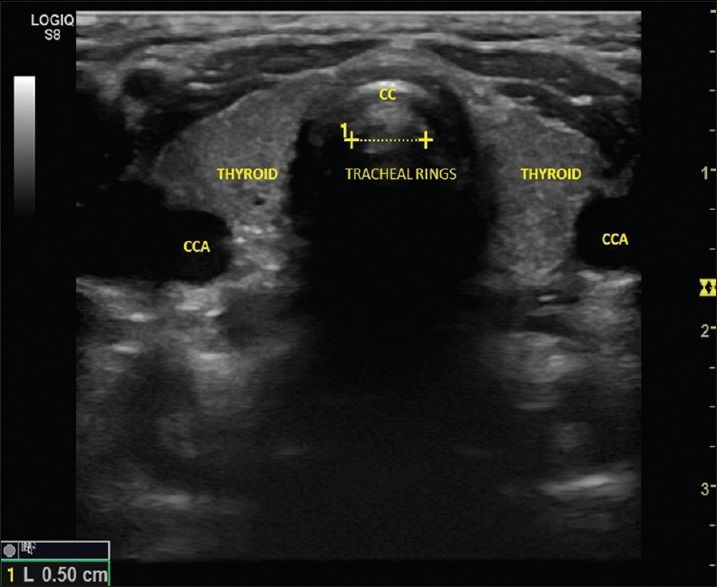
Ultrasonography showing measurement of tracheal diameter. CCA: Common carotid artery, CC: Cricoid cartilage
After performing ultrasonography patient was shifted to operation theatre. Operating theatre temperature was kept constant around 24°C and surface warming was done using Smiths warmer (serial number 20060201). Electrocardiography, non invasive blood pressure (systolic blood pressure, diastolic blood pressure and mean arterial pressure), capnography, temperature, pulse oximeter were monitored using Drager Infinity Vista® monitor (Model MS14750E5394). Clinical monitoring was done by assessing the colour of the patient and precordial stethoscope.
General anesthesia was induced by inhalation of 50% oxygen and 50% nitrous oxide and incremental concentration of sevoflurane starting from 1% and gradually increasing to 5-6% that is 1% every 6-8 breaths via Jackson Rees circuit. Intravenous access was secured with 22 G cannula and 0.33% Dextrose in normal saline/Ringer Lactate was started. Intravenous Inj Fentanyl 2 μg/kg and iv Inj Atracurium 0.5mg/kg was administered and patient was ventilated for three minutes with O2 (50%)+ N2O (50%) and sevoflurane. After achieving adequate relaxation, tracheal intubation was done by the same anaesthesiologist who had an experience of at least 100 paediatric intubations. He was also kept unaware of the diameter assessed by the radiologist. All the intubations were done with uncuffed endotracheal tube (Portex Tracheal Tube Smiths Medical India Pvt. Ltd.) with Murphy's eye.
The correct position of the tracheal tube will be confirmed by capnography and by auscultation for bilateral breath sounds. The tracheal tube size was chosen and selected as ‘best fit’ by the attending anesthesiologist if air leakage was satisfactory at a 15-20 cm H2O airway pressure. For the purpose of air leak measurement, the head and body positions were standardized; the patient was supine with the head roughly in a neutral position to limit any impact on the leak test. The endotracheal tube was changed to a 0.5 mm larger tube when air leak was excessive or if a leak occurred at an inflated pressure <10 cm H20. Alternatively, when there was resistance to the passage of the endotracheal tube into the trachea or when air leak was not detected, the tube was exchanged with 0.5 mm smaller tube.
After intubation all the patients were ventilated to normocapnia using Drager Fabius GS (ARXK-0102) and Jackson Rees circuit according to the patient weight. The end-tidal concentration of sevoflurane was adjusted to 1-1.5 minimum alveolar concentration (MAC) in oxygen and nitrous oxide. Sevoflurane was delivered using Datum Vaporiser (serial number 03060107C). Standardized ventilatory sendotracheal tubeings were applied: volume-controlled ventilation, peak inspiratory pressure of 10-15 cm H2O to give tidal volume of 7-10ml/kg, breathing frequency according to patient's age and PEtCO2 (end tidal CO2), fresh gas flow of 3 L/min.
At the end of the procedure and removal of tracheal tube all patients were transferred to the recovery room for postoperative follow-up to assess post-extubation respiratory complications (croup, cough, sore throat, dyspnea, dysphonia or stridor).
For all patients, the size predicted by the above mentioned formulae was calculated preoperatively and recorded in a sheet that was not informed to the intubating anaesthesiologist and the radiologist. Because the calculated values might not be clinically applicable (0.5 multiples), we calculated the difference between the used and estimated sizes and considered the estimate to match the size actually used when the difference was between-0.5 and +0.5.
A comparative analysis was done between calculated external diameters of the endotracheal tube from physical indices formulas and size by comparison to little finger, predetermined by ultrasound and clinically used endotracheal tube for intubation during general anesthesia was obtained.
Statistical analysis
It was an observational-cross sectional study. In the available literature estimation of appropriate size of endotracheal tube by preoperative assessment of subglottic region by ultrasonography in children was found to be 40% to 60% accurate.[11] Therefore, assuming (p)=50% as the accuracy of estimated size of endotracheal tube with 10% margin of error, the minimum required sample size at 5% level of significance is 92 patients. To be conservative we enrolled 100 patients in the study who fulfilled the inclusion criteria. Sample size was calculated using:

Where p is the observed accuracy
q = 1-p
d is the margin of error
Zα/2 is the ordinate of standard normal distribution at α% level of significance
Interpretation and analysis of obtained results was carried out using software Microsoft office Excel 2010 and Statistical package for social science (SPSS) International business machines (IBM) version 22, IBM SPSS Statistics base (SPSS South Asia Pvt., Ltd., Bengaluru, India).
Qualitative data was expressed using range, frequencies and percentages whereas mean and standard deviation expressed quantitative data. The distribution of the predicted endotracheal tube size by different modalities was compared with best fit endotracheal tube using the Chi-square test. Comparison of efficacy of different modalities for prediction of endotracheal tube size was done by using Pearsons correlation coefficient. The distribution of size of endotracheal tube was compared between different age groups using the Chi-square test. The comparison of mean size of endotracheal tube, endotracheal tube size by age based formula, endotracheal tube size by body length, endotracheal tube size by comparison to right little finger, endotracheal tube size by comparison to left little finger, endotracheal tube size by ultrasonography and endotracheal tube size by multivariate formula was done using the Friedman's test and Wilcoxon sign-rank test was used.
Results
Comparable pattern was seen in the demographic and physical characteristics of all 100 patients [Table 1].
Table 1.
Demographic and physical profile of the subjects and type of surgery performed
| Frequency (n=100) | |
|---|---|
| Age, mean±SD (months) | 26.88±16.21 |
| Male: female | 66:34 |
| Weight, mean±SD (kg) | 11.28±3.34 |
| Height, mean±SD (cm) | 79.94±15.74 |
| ASA Grade I: II | 98:2 |
| Type of surgery | |
| Plastic | 40 |
| Paediatrics | 25 |
| Orthopaedics | 10 |
| ENT | 5 |
| Ophthalmics | 10 |
| Urology | 10 |
ASA: American society of Anesthesiologist; ENT: Ear, nose and throat; SD: Standard deviation
Comparison between the Best fit and predicted size of Endotracheal tube by various modalities was done by using chi square test [Table 2]. The predicted tube size was equal to best fit and best determined by ultrasonography (100%) followed by comparison to left little finger (98%) and right little finger (97%) and Age based formula (95%) followed by Multivariate formula (83%) and Body Length (81%) formula.
Table 2.
Comparison between the best fit and predicted size of endotracheal tube by various modalities
| Frequency (%) | Pearson correlation with best fit tube | |||
|---|---|---|---|---|
| “Best fit’”< size predicted | “Best fit”=size predicted | “Best fit” >size predicted | ||
| Predicted size by age based formula | 4 (4.0) | 95 (95.0) | 1 (1.0) | 0.743 |
| Predicted size by body length based formula | 14 (14.0) | 81 (81.0) | 5 (5.0) | 0.683 |
| Predicted size by comparison to right little finger | 1 (1.0) | 97 (97.0) | 2 (2.0) | 0.587 |
| Predicted size by comparison to left little finger | 1 (1.0) | 98 (98.0) | 1 (1.0) | 0.587 |
| Predicted size by ultrasonography | 0 (0.0) | 100 (100.0) | 0 (0.0) | 0.973 |
| Predicted size by multivariate formula | 4 (4.0) | 83 (83.0) | 13 (13.0) | 0.741 |
On correlation using Pearson's correlation coefficient [Table 2]. It was observed that there was a moderate correlation of best fit Endotracheal tube with endotracheal tube size by age based formula (r = 0.743), body length based formula (r = 0.683), right little finger based formula (r = 0.587), left little finger based formula (r = 0.587) and multivariate formula (r = 0.741). A strong correlation was seen with ultrasonography (r = 0.943).
57 (57%) subjects were successfully intubated in first attempt. While 40 (40%) subjects required a second attempt owing to significant leak in 20 (20%), technical difficulty in 15 (15%) and tube too big in 5 (5%) subjects. Three (3%) subjects required a third attempt at intubation due to improper technique [Table 3].
Table 3.
Number of attempts for intubation
| Age group | Number of attempts for intubation | Total | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| 12-24 months | 39 (59.1) | 26 (39.4) | 1 (1.5) | 66 (100.0) |
| 25-36 months | 5 (31.3) | 10 (62.5) | 1 (6.3) | 16 (100.0) |
| 37-48 months | 3 (50.0) | 3 (50.0) | 0 (0.0) | 6 (100.0) |
| 49-60 months | 10 (83.3) | 1 (8.3) | 1 (8.3) | 12 (100.0) |
| Total | 57 | 40 | 3 | |
The mean and standard deviation of best fit endotracheal tube was 4.55 ± 0.45. The mean and standard deviation for endotracheal tube size predicted by age based formula, body length based formula, comparison by right little finger, comparison by left little finger, ultrasound and multivariate formula is 4.56 ± 0.34, 4.65 ± 0.52, 4.58 ± 0.39, 4.56 ± 0.40, 4.67 ± 0.46 and 4.42 ± 0.47 respectively [Table 4].
Table 4.
Comparison of endotracheal tube size estimated by different modalities with the best fit endotracheal tube
| Number of cases | Best fit ETT | Endotracheal tube size by age based formula | Endotracheal tube size by body length based formula | Endotracheal tube size by comparison to right little finger based formula | Endotracheal tube size by comparison to left little finger based formula | Endotracheal tube size by ultrasound | Endotracheal tube size by multivariate formula | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD | ||
| 1 | 3.5 | 4.25 | 0.00 | 4.03 | 0.00 | 4.50 | 0.00 | 4.50 | 0.00 | 3.50 | . | 3.84 | 0.00 |
| 25 | 4.0 | 4.33 | 0.12 | 4.29 | 0.28 | 4.36 | 0.23 | 4.34 | 0.24 | 4.16 | 0.12 | 4.10 | 0.20 |
| 45 | 4.5 | 4.43 | 0.23 | 4.52 | 0.38 | 4.46 | 0.28 | 4.43 | 0.31 | 4.59 | 0.09 | 4.27 | 0.29 |
| 21 | 5.0 | 4.88 | 0.26 | 5.11 | 0.48 | 4.93 | 0.43 | 4.90 | 0.41 | 5.16 | 0.11 | 4.85 | 0.41 |
| 8 | 5.5 | 5.16 | 0.23 | 5.41 | 0.32 | 5.06 | 0.32 | 5.06 | 0.18 | 5.60 | 0.07 | 5.22 | 0.28 |
| Total | 4.55±0.45 | 4.56 | 0.34 | 4.65 | 0.52 | 4.58 | 0.39 | 4.56 | 0.40 | 4.67 | 0.46 | 4.42 | 0.47 |
Ultrasonography was the most sensitive (100%) method of prediction followed by comparison to Left (98%) and Right (97%) little finger and age based formula (95%), the Multivariate formula had even lesser sensitivity (83%). Whereas Body length based formula was least sensitive with sensitivity of 78% [Table 5].
Table 5.
Comparison of sensitivity of different modalities for prediction of endotracheal tube size
| Sensitivity, frequency (%) | |
|---|---|
| Predicted size by age based formula | 95 (95.0) |
| Predicted size by body length based formula | 78 (78.0) |
| Predicted size by right little finger based formula | 97 (97.0) |
| Predicted size by left little finger based formula | 98 (98.0) |
| Predicted size by ultrasonography based formula | 100 (100.0) |
| Predicted size by multivariate formula | 83 (83.0) |
Discussion
Ultrasonography has recently found a place in anaesthesiology and is a newer modality for the anaesthesiologists. It is a operator dependent technique, relatively easy to learn and with a total of approximately 15 procedures the operator can reproduce reliable results.[4]
Other noninvasive methods such as chest X-ray, computed tomography, magnetic resonance imaging were not considered as they are relatively expensive and assessment of laryngeal dimensions maybe overestimated as shape of the subglottic area is frequently uncylindrical also it may require to sedate the child for immobility whereas in case of ultrasonography there is no such need.[4]
Preoperative planning, premedication, anaesthesia technique or postoperative care during the time frame of the study was kept constant. In all the subjects the transverse airway column was measured as previous studies have reported that ultrasound can accurately measure airway diameter in the transverse, which is not possible in the anteroposterior direction. As the anteroposterior diameter of the trachea is larger than its transverse diameter, and leads to underestimation of the actual tracheal diameter and the selection of a smaller endotracheal tube.[10]
In terms of location, in previous studies, the probe was positioned at the cricoid cartilage level, either at the lower end of the cricoid ring or at mid pont. The lower edge of hypoechoic cricoids cartilage was taken as reference point for measurement of subglottic diameter. This measure represents a reliable and consistent value that can be comparable among the patients.[10]
We believe that we avoided both underestimation and overestimation in our study by monitoring leak pressure thresholds and peak airway pressures. Further, in this study, we standardised brand of endotracheal tube, as the wall thickness of the endotracheal tube may affect the tube size ID for a given OD and hence may also affect the peak airway pressure.
All radiological measurement were performed by the same experienced radiologist in the study to rule out any bias in the accuracy of measurement with ultrasonography also our department till then did not have an ultrasound. The time required for ultrasonographic estimation was less than two minutes in all patients. Portex endotracheal tubes were used in all the cases to prevent bias as the outer diameter of endotracheal tube varies with different manufacturers.[10]
We preffered to use uncuffed endotracheal tube as selected outer diameters have a tendency to be smaller in cuffed than in uncuffed endotracheal tube. We preferred to measure the subglottic diameter as this was the narrowest part of the trachea thus preventing trauma due to insertion of a large size endotracheal tube.
In this novel feasibility study we observed that direct ultrasonography measurements of the subglottic diameter to identify uncuffed endotracheal tube size with 100% success rate. Whereas the success rate with age based formula, body length based formula and multivariate formula was 95%, 78% and 83% respectively. Interestingly the rough estimation done by right and left little finger was much accurate in prediction of endotracheal tube size with 97% and 98% success rate. The disparity between height based formula and multivariate formula and the clinically optimal endotracheal tube size was substantial, Whereas ultrasonography was highly predictive. height based formula generally predicted undersized endotracheal tube than the clinically optimal endotracheal tube. The multivariate formula also predicted undersized tubes. We performed USG in children pre-anaesthetically in sedated state as we did not have an ultrasound machine in the operating room. USG in crying and uncooperative children could lead to false subglottic tracheal diameter values. a sedated child would be more cooperative and yield accurate results.
The use of ultrasonography to predict appropriate uncuffed endotracheal tube size in children has been previously studied. The results of these studies are comparable to our study as shown in Table 6.
Table 6.
Comparison of the results of our study with other studies
| Author | Population | Initial tube size selection | Type of tube | Condition | Allowed leak pressure | Measurement level |
|---|---|---|---|---|---|---|
| Shibasaki et al.[11] | n=192 1 month-6 years | Age and height based formulas versus ultrasonography | Cuffed and uncuffed | Apnoea with no continuous positive airway pressure | 10-20 cm H20 for uncuffed ETT 20-30 cm H2O for cuffed ETT | At lower edge of the cricoids cartilage |
| Bae et al.[3] | n=141<8 years | Age based formulas versus ultrasonography | Uncuffed | 10 cm H2O continuous positive airway pressure | 15-30 cm H2O | At the mid cricoids cartilage level |
| Schramm et al.[12] | n=50<5 years | Age based formulas versus ultrasonography | Uncuffed | Apnoea with continuous positive airway pressure | 15.3-25.5 cm H2O | At the narrowest portion of the subglottic airway (MTDSA) |
| Kim et al.[13] | n=215 1-72 months | Age based recommendation versus ultrasonography | Cuffed | Apnoea | No air leak test | At the mid cricoids cartilage level |
| Gupta et al.[4] | n=112 3-18 years | Physical indices versus ultrasonography | Cuffed and Uncuffed | Awake | 20-30 cm H2O | Cephalic half of the cricoid cartilage |
| Our study | n=100 12-60 months | Traditional formulas versus ultrasonography | Uncuffed | Preoperative, sedated | 20-30 cm H2O | Subglottic region, airway transverse diameter |
ETT: Endotracheal tube; MTDSA: Minimal transverse diameter of the subglottic airway
Limitations of the present study are the selection of endotracheal tube as best fit by observing the air leak test is subjective and may not be very accurate. Also this was a descriptive study performed in a single hospital sendotracheal tubeing, a larger multicentric prospective study would be able to validate the results. The limitations of ultrasonography should also be considered as it measures the transverse diameter of the trachea at one level which is subject to variations. We did not include the subjects below one year of age because transverse diameter is difficult to measure in these cases. due to anatomical variations. And there are few formulas which are exclusive for the subjects above one year of age so the subjects below one year of age could not be included.
Conclusion
Ultrasonography proved to be a reliable predictor for the assessment of the subglottic diameter of the airway in children to estimate the appropriate endotracheal tube size for intubation and can prevent the repeated attempts on intubation.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Wailoo MP, Emery JL. Normal growth and development of the trachea. Thorax. 1982;37:584–7. doi: 10.1136/thx.37.8.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Taylor C, Subaiya L, Corsino D. Pediatric cuffed endotracheal tubes: An evolution of care. Ochsner J. 2011;11:52–6. [PMC free article] [PubMed] [Google Scholar]
- 3.Bae JY, Byon HJ, Han SS, Kim HS, Kim JT. Usefulness of ultrasound for selecting a correctly sized uncuffed tracheal tube for paediatric patients. Anaesthesia. 2011;66:994–8. doi: 10.1111/j.1365-2044.2011.06900.x. [DOI] [PubMed] [Google Scholar]
- 4.Gupta K, Gupta PK, Rastogi B, Krishan A, Jain M, Garg G, et al. Assessment of the subglottic region by ultrasonography for estimation of appropriate size endotracheal tube: A clinical prospective study. Anesth Essays Res. 2012;6:157–60. doi: 10.4103/0259-1162.108298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Davis D, Barbee L, Ririe D. Pediatric endotracheal tube selection: A comparison of age-based and height-based criteria. AANA J. 1998;66:299–303. [PubMed] [Google Scholar]
- 6.Shih MH, Chung CY, Su BC, Hung CT, Wong SY, Wong TK, et al. Accuracy of a new body length-based formula for predicting tracheal tube size in Chinese children. Chang Gung Med J. 2008;31:276–80. [PubMed] [Google Scholar]
- 7.Turkistani A, Abdullah KM, Delvi B, Al-Mazroua KA. The ‘best fit’ endotracheal tube in children – Comparison of four formulae. Middle East J Anaesthesiol. 2009;20:383–7. [PubMed] [Google Scholar]
- 8.King BR, Baker MD, Braitman LE, Seidl-Friedman J, Schreiner MS. Endotracheal tube selection in children: A comparison of four methods. Ann Emerg Med. 1993;22:530–4. doi: 10.1016/s0196-0644(05)81937-7. [DOI] [PubMed] [Google Scholar]
- 9.Lakhal K, Delplace X, Cottier JP, Tranquart F, Sauvagnac X, Mercier C, et al. The feasibility of ultrasound to assess subglottic diameter. Anesth Analg. 2007;104:611–4. doi: 10.1213/01.ane.0000260136.53694.fe. [DOI] [PubMed] [Google Scholar]
- 10.Altun D, Sungur MO, Ali A, Bingül ES, Seyhan TÖ, Çamcı E, et al. Ultrasonographic measurement of subglottic diameter for paediatric cuffed endotracheal tube size selection: Feasibility report. Turk J Anaesthesiol Reanim. 2016;44:301–5. doi: 10.5152/TJAR.2016.60420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shibasaki M, Nakajima Y, Ishii S, Shimizu F, Shime N, Sessler DI, et al. Prediction of pediatric endotracheal tube size by ultrasonography. Anesthesiology. 2010;113:819–24. doi: 10.1097/ALN.0b013e3181ef6757. [DOI] [PubMed] [Google Scholar]
- 12.Schramm C, Knop J, Jensen K, Plaschke K. Role of ultrasound compared to age-related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth. 2012;22:781–6. doi: 10.1111/j.1460-9592.2012.03889.x. [DOI] [PubMed] [Google Scholar]
- 13.Kim EJ, Kim SY, Kim WO, Kim H, Kil HK. Ultrasound measurement of subglottic diameter and an empirical formula for proper endotracheal tube fitting in children. Acta Anaesthesiol Scand. 2013;57:1124–30. doi: 10.1111/aas.12167. [DOI] [PubMed] [Google Scholar]


