Abstract
Background/Objectives:
Potentially inappropriate opioid prescribing (PIP) may contribute to risk for fatal opioid overdose among older adults (age 50+). Our objective was to examine the effect of age on the likelihood of PIP exposure, as well as the effect of PIP exposure on adverse outcomes.
Design:
Retrospective cohort study
Setting:
Data from multiple state agencies in Massachusetts, 2011–2015
Participants:
Over 3 million adult Massachusetts residents (3,078,163) who received at least one prescription opioid during the study period; approximately half (1,589,365) were older adults (age 50+).
Measurements:
We measured exposure to five types of PIP: high-dose opioids, co-prescription with benzodiazepines, multiple opioid prescribers, multiple opioid pharmacies, and continuous opioid therapy without a pain diagnosis. We examined three adverse outcomes: non-fatal opioid overdose, fatal opioid overdose, and all-cause mortality.
Results:
The rate of any PIP exposure increased with age, ranging from 2% among individuals age 18–29 to 14% among those age 50 and older. Older adults also had elevated rates of exposure to two or more different types of PIP, including 5% of adults age 50–69 and 4% of adults age 70 or older, in comparison to 2.5% of age 40–49 and lower percentages in younger age groups. Among covariates assessed, increasing age was the greatest positive predictor of PIP exposure. In analyses stratified by age, exposure to both any PIP and specific types of PIP were associated with non-fatal overdose, fatal overdose, and all-cause mortality among both younger and older adults.
Conclusion:
Older adults are more likely to be exposed to PIP, which elevates their risk for adverse events. Strategies to reduce exposure to PIP, and to improve outcomes among those already exposed, will be instrumental to addressing the opioid crisis as it manifests among older adults.
Keywords: potentially inappropriate opioid prescribing, aged, opioid overdose, mortality
INTRODUCTION
Opioid use and opioid-related harms may be different among older adults (age 50+) than among younger adults.1 Prescription opioids account for more than twice as many deaths as illicit opioids among older adults.2 Potentially inappropriate prescribing (PIP) involves either suboptimal prescribing or high-risk medication use. Research has shown an association between PIP and fatal opioid overdose,3–12 and at least one study has shown higher rates of PIP in older adults than in younger adults.13 Older adults may be particularly vulnerable to toxicity from PIP, given increased pharmacokinetic vulnerability inherent to the aging process.14
To date, few studies have characterized patterns of PIP among older adults, and few among these have examined its consequences. This study uses the population of an entire state (Massachusetts) over a 5-year period to address this gap in the literature by examining age as a predictor of PIP exposure and the degree to which age may modify the effect of PIP on adverse events. The results of this study can inform practice- and policy-level interventions to reduce PIP exposure and also reduce harms for patients already exposed to PIP.
METHODS
Database and Patient Sample
We used databases administered by the Massachusetts Department of Public Health (MDPH) under the authority of Chapter 55 legislation.15 Chapter 55 of the Acts of 2015 mandated that MDPH analyze data from several state agencies, and allowed for linkage of datasets to analyze trends in opioid-related overdose.15 The dataset, covering more than 98% of the state’s population, included Massachusetts’ prescription monitoring program (PMP), all-payer claims database (APCD), mortality records (including autopsy and postmortem toxicology), demographic and area-level socioeconomic status data, and ambulance/emergency medical services (EMS) records.
Our study population included all patients age ≥ 18 years who filled at least one opioid prescription from 2011 to 2015 (n = 3,078,163); we excluded patients with regionally or distantly disseminated cancer (Supplementary Appendix S1). Prescription opioid analgesics included codeine, fentanyl, hydrocodone, hydromorphone, meperidine, methadone (used as an analgesic), morphine, oxycodone, and oxymorphone (Supplementary Appendix S2). Burprenorphine and methadone used for treatment of opioid use disorder were not considered when assessing prescription opioid exposure;12 however, individuals who received them were not excluded if they also received prescription opioid analgesics. The study was exempted from review by the Institutional Review Boards of MDPH and RAND Corporation.
Measures
Potentially Inappropriate Opioid Prescribing Subtypes
Similar to other studies,3–11 we identified patients exposed to one or more types of PIP including:
High-dose opioids, defined by the daily dose equivalent for each patient in each month in milligram morphine equivalents (MME) (Supplementary Appendix S2). We considered a patient to have received high-dose opioids if their prescriptions averaged MME ≥ 100 mg/day in three or more separate months.
Overlapping opioid and benzodiazepine prescriptions, defined as opioid and benzodiazepine prescriptions that overlapped by at least one day in three or more separate months.
Multiple opioid prescribers, defined as four or more opioid prescribers in any three-month period.
Multiple opioid pharmacies, defined as opioids from four or more pharmacies in any three-month period.
Lack of a documented pain diagnosis, defined as receiving opioids for three consecutive months without a pain diagnosis code on a medical service claim (Supplementary Appendix S3).
Patient Outcomes
Outcomes included 1) non-fatal opioid overdose; 2) fatal opioid overdose; and 3) all-cause mortality. Non-fatal overdose was identified in EMS data using an MDPH algorithm and in-hospital or emergency department encounter data using ICD-9 codes (Supplementary Appendix S4). For non-fatal overdose, we considered only the first occurrence. Fatal overdose and all-cause mortality were identified using state mortality data (Supplementary Appendix S5).
Covariates
Sex was defined as male or female. Race and ethnicity were not used as covariates because data were missing in nearly half the cases. Two comorbid conditions likely relevant to the development of opioid-related adverse events, major depression and alcohol use disorder, were identified using claims data (Supplementary Appendix S6). We characterized community-level socioeconomic status (SES) by the percentage of households below the federal poverty level in the patient’s ZIP code of residence.16
Statistical Analyses
We used logistic regression to estimate the age-specific odds of receiving any PIP, controlling for covariates, among the population of patients who received any prescription opioids. We then stratified the sample into older adults (age 50+) and younger adults (age 18–49). For each stratum and patient outcome (i.e., nonfatal overdose, fatal overdose, and all-cause mortality), we conducted a separate logistic regression to examine the influence of each PIP subtype on the outcome, controlling for the other subtypes of PIP and patient-level covariates other than age. Finally, we examined the influence of the number of PIP subtypes to which the patient had been exposed (0, 1, 2, or 3+) on each outcome, controlling for patient-level covariates. For all analyses regarding non-fatal overdoses, exposure to PIP was only included if it had occurred before the overdose event. All analyses were performed using SAS Studio, Version 3.5 (SAS Corporation, Cary, NC).
RESULTS
Patient Characteristics and Outcomes
Between 2011 and 2015, over 3 million adult Massachusetts residents (3,078,163, or 57% of the state’s adult population) received at least one opioid prescription. Approximately half of those opioid recipients (52%) were age 50 or older. Older opioid recipients were more likely than younger recipients to live in the lowest-poverty ZIP codes (56% vs. 47%, p < 0.001) and somewhat more likely to have major depression (19% vs. 16%, p < 0.001) (Supplementary Appendix S7). The rate of all-cause mortality was much higher in the older group (8% vs. 0.6% over the five years of the study, p < 0.001), whereas younger patients had considerably higher rates of both fatal opioid overdose (0.2% vs. 0.06%, p < 0.001) and non-fatal opioid overdose (1.0% vs. 0.5%, p < 0.001).
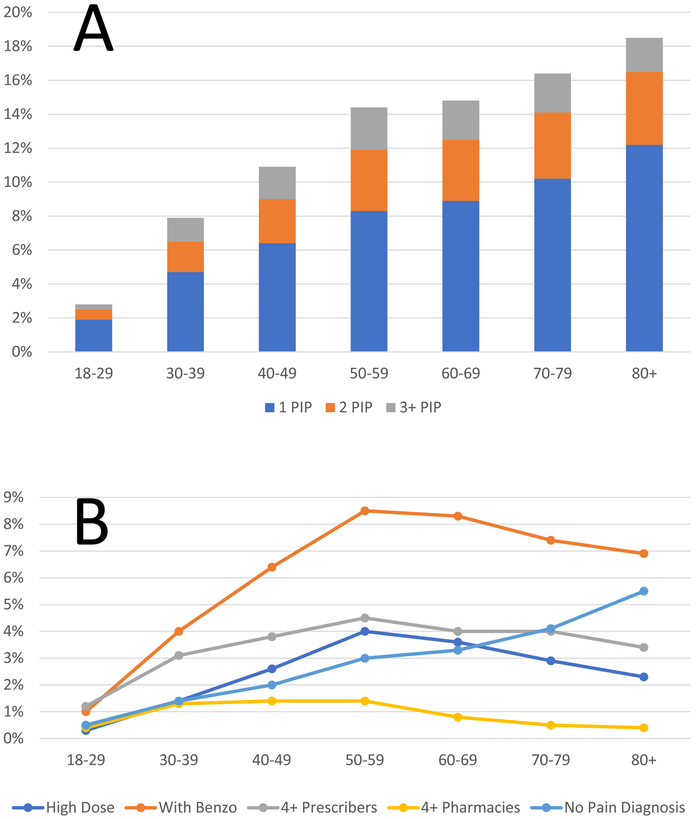
Age Distribution of Potentially Inappropriate Prescribing of Opioids
The percentage of prescription opioid recipients experiencing any PIP increased with age, but plateaued above age 50 (Figure 1a). The proportion of patients experiencing two or more PIP subtypes during the study period also varied with age, peaking for age 50–59. Prevalence of each PIP subtype had a distinctive age distribution (Figure 1b), with most PIP subtypes peaking during age 50–59. Receipt of high-dose opioids, co-prescription of benzodiazepine, having multiple prescribers, and having multiple pharmacies all peaked during age 50–59. High-dose opioids declined somewhat with older age (from 4.0% among age 50–59 to 2.3% among age 80+). For benzodiazepine co-prescribing, the decline with older age was less pronounced (from 8.5% among age 50–59 to 6.9% among age 80+). In contrast to the other PIP subtypes, receiving continuous opioid prescriptions without a pain diagnosis increased monotonically with age, reaching a high of 5.5% among age 80+.
Figure 1a:
Age-specific percentages of adult prescription opioid recipients experiencing one, two, or three or more types of potentially inappropriate opioid prescribing, of five examined.
b: Age-specific percentages of adult prescription opioid recipients experiencing specific subtypes of potentially inappropriate opioid prescribing in Massachusetts, from 2011–2015.
Patient-Level Predictors of Receiving Potentially Inappropriate Opioid Prescribing
Among individuals prescribed any opioid during the study period, the adjusted odds of receiving PIP increased with age (Table 1), plateauing above age 50–59, and rising as high as 6.37 for age 80+, when compared to age 18–29. Females (OR 1.12), individuals with depression (OR 2.73), and individuals with alcohol use disorder (OR 1.88) were also significantly more likely to receive PIP.
Table 1:
Patient-level predictors of receiving any PIP (as compared to no PIP) among Massachusetts adults who received prescribed opioids at least once between 2011 and 2015 (n = 3,078,163).
| Variable | Proportion of Patients in Category* | Adjusted Odds Ratio for receiving PIP (95% CI) |
p-value |
|---|---|---|---|
| Age | |||
| 18-29 | 17% | REF | REF |
| 30-39 | 16% | 3.02 (2.95-3.08) |
< 0.001 |
| 40-49 | 16% | 4.45 (4.37-4.55) |
< 0.001 |
| 50-59 | 19% | 6.08 (5.96-6.34) |
< 0.001 |
| 60-69 | 16% | 6.22 (6.10-6.34) |
< 0.001 |
| 70-79 | 9% | 6.37 (6.24-6.50) |
< 0.001 |
| 80+ | 9% | 6.37 (6.24-6.51) |
< 0.001 |
| Sex | |||
| Male | 45% | REF | REF |
| Female | 55% | 1.12 (1.11-1.13) |
< 0.001 |
| ZIP Code Level Percentage of Households Below Federal Poverty Line | |||
| 0-9.99% | 52% | REF | REF |
| 10-19.99% | 29% | 1.13 (1.12-1.14) |
< 0.001 |
| 20-29.99% | 14% | 1.17 (1.15-1.18) |
< 0.001 |
| 30%+ | 5% | 1.09 (1.07-1.11) |
0.28 |
| Comorbid Conditions/History | |||
| Major Depression | 18% | 2.73 (2.71-2.75) |
< 0.001 |
| Alcohol Use Disorder | 5% | 1.88 (1.85-1.91) |
< 0.001 |
Proportion of all patients who received any prescription opioids. May not sum to 100% due to rounding.
Association Between Potentially Inappropriate Prescribing and Outcomes
PIP was associated with all-cause mortality, fatal opioid overdose, and non-fatal overdose across the study population (Table 2). Most PIP subtypes were associated with greater increases in the odds of all-cause mortality among younger adults than older adults. For example, co-prescribing with benzodiazepines was associated with greater odds of all-cause mortality among younger adults (ages 18–49, OR 2.84, 95% CI 2.66–3.03) than older adults (age 50+, OR 1.47, 95% CI 1.44–1.50).
Table 2:
Association of PIP and all-cause mortality, fatal opioid overdose, and non-fatal opioid overdose in Massachusetts, from 2011-2015, by age.
| All-Cause Mortality AOR (95% CI) |
Fatal Opioid Overdose* AOR (95% CI) |
Non-Fatal Opioid Overdose† AOR (95% CI) |
||||
|---|---|---|---|---|---|---|
| Age 18-49 | Age 50+ | Age 18-49 | Age 50+ | Age 18-49 | Age 50+ | |
| Number of PIP‡ | ||||||
| No PIP | REF | REF | REF | REF | REF | REF |
| One PIP | 4.61 (4.34-4.90) |
2.11 (2.07-2.15) |
4.80 (4.29-5.37) |
5.93 (4.79-6.76) |
1.81 (1.72-1.92) |
2.25 (2.12-2.39) |
| Two PIP | 8.87 (8.27-9.51) |
4.13 (4.02-4.24) |
8.10 (7.09-9.27) |
10.68 (8.86-12.88) |
2.39 (2.22-2.58) |
4.06 (3.78-4.36) |
| Three or More PIP | 14.95 (13.89-16.09) |
7.69 (7.42-7.97) |
13.80 (12.04-15.80) |
18.61 (15.35-22.57) |
3.10 (2.84-3.38) |
5.36 (4.93-5.83) |
| Specific PIP Subtypes§ | ||||||
| High Dose (>100 MME 3+ months) | 3.59 (3.34-3.87) |
2.70 (2.63-2.78) |
1.96 (1.70-2.25) |
2.53 (2.12-3.03) |
1.58 (1.45-1.72) |
2.77 (2.58-2.97) |
| Co-prescription with Benzodiazepine (overlap 3+ months) | 2.84 (2.66-3.03) |
1.47 (1.44-1.50) |
4.54 (4.03-5.10) |
4.52 (3.83-5.34) |
1.51 (1.42-1.60) |
1.97 (1.86-2.10) |
| Multiple (4+) prescribers | 2.05 (1.91-2.20) |
1.68 (1.64-1.73) |
1.46 (1.28-1.68) |
1.29 (1.07-1.57) |
1.37 (1.28-1.47) |
1.23 (1.14-1.33) |
| Multiple (4+) pharmacies | 0.87 (0.79-0.96) |
1.39 (1.32-1.47) |
1.60 (1.36-1.88) |
1.59 (1.25-2.02) |
1.47 (1.34-1.62) |
1.30 (1.16-1.44) |
| No documented pain diagnosis | 3.79 (3.50-4.10) |
2.78 (2.71-2.84) |
2.72 (2.30-3.22) |
2.64 (2.15-3.24) |
1.50 (1.32-1.71) |
1.15 (1.02-1.30) |
AOR: Adjusted Odds Ratio; CI: Confidence Interval; MME: Milligram morphine equivalents.
Every fatal overdose, by definition, is also an all-cause mortality.
For non-fatal overdose, patients are only considered to have been exposed to PIP if the exposure occurred before the outcome.
None, one, two, or three or more out of the five types of PIP mentioned above. Controlling for sex, ZIP code level poverty, depression, and alcohol use disorder.
Controlling for sex, ZIP code level poverty, depression, alcohol use disorder, and the other four PIP variables.
PIP was generally associated with similar odds of non-fatal and fatal opioid overdose among older and younger adults, relative to prescription opioids alone. For example, benzodiazepine co-prescription was associated with fatal overdose with odds ratios of 4.54 among younger adults (95% CI 4.03–5.10) and 4.53 among older adults (95% CI 3.83–5.34).
The effect of multiple PIP subtype exposures on all-cause mortality was stronger among younger adults: younger adults exposed to three or more PIP subtypes had 14.95 times the odds (95% CI 13.89–16.09) of all-cause mortality relative to same-age adults with non-PIP opioid prescribing, whereas exposure to three or more PIP subtypes was associated with 7.69 times the odds (95% CI 7.42–7.97) of all-cause mortality among older adults. In contrast, more exposure to PIP increased the odds for fatal and non-fatal opioid overdose more markedly among older adults. Specifically, older adults exposed to three or more PIP subtypes had 18.61 times the odds (95% CI 15.35–22.57) of fatal opioid overdose, relative to same-age adults with non-PIP opioid prescribing.
DISCUSSION
Prescription opioids are a key driver of opioid-related death, especially among older adults.2 Studies have demonstrated that PIP is associated with higher odds of non-fatal opioid overdose, fatal opioid overdose, and all-cause mortality.3–11 In our study, age was by far the strongest predictor of receiving PIP. We also found that PIP was strongly associated with higher odds for adverse events, both among older and younger adults.
These results support the idea that policy solutions to the opioid crisis need to address the effect of PIP on opioid-related adverse events in older adults.1 Such solutions will require at least two distinct goals. The first goal is to reduce the incidence of new exposures to PIP by changing prescribing habits through prescriber and patient education, regulations, decision support, and other complementary efforts. The second is to implement effective, evidence-based treatment strategies to reduce risk of overdose among older adults exposed to PIP. Both PIP patients and their prescribers should be offered increased monitoring and clinical support, overdose education and naloxone rescue kits, alternative pain treatments, and low-barrier access to treatment for opioid use disorder, if warranted.
Our findings suggest that PIP exposure may have somewhat different, if overlapping, effects among older adults and younger adults. This, in turn, may be driven by the fact that PIP may have different origins and different meanings in the two groups. PIP is generally considered to represent a mix of inappropriate use (by the patient) and inappropriate and possibly dangerous prescribing (by the provider). Among younger adults, the opioid misuse aspect of PIP may be more predominant. In contrast, among older adults, PIP may have more to do with excessively high doses and/or co-prescribing with benzodiazepines, which may confer risk not through misuse but through use as directed. This points to a need to tailor approaches to reducing new PIP incidence among different patient populations, particularly those of different ages.
Finding ways to improve outcomes for patients already exposed to PIP—the second goal above—may be as important as reducing PIP incidence, though it may be receiving less attention. Our findings suggest that PIP is a problem of considerable magnitude and significance among older adults. We found that in Massachusetts, 215,210 older adults were exposed to PIP at least once during the study period. Extrapolating to the entire United States, this implies that at least 11 million older adults were exposed to PIP during this period. Management of older adults already exposed to PIP will be critical to improving their outcomes, but to our knowledge there have been no studies of how best to conduct such management. For example, should older adults on high-dose opioids be tapered to below 100 MME—or to below 80, or below 60—and over what period of time? Does tapering reduce risk to individuals who have previously been exposed to PIP, or does it paradoxically increase risk? Answers to these and similar questions would inform a presently evidence-free zone.
We acknowledge the study’s limitations. First, like any observational study, ours is subject to residual confounding. This refers to differences between patients who received opioids with PIP and patients who received opioids without PIP that may contribute to differences in outcomes. While we controlled for some differences in our models, other factors were not measured in this study. Second, population-based results from Massachusetts may not fully generalize to other states. Third, the list of opioids in this study did not include tramadol, which has opioid-like properties and can sometimes cause an opioid use disorder. Finally, opioid overdose deaths may be undercounted, and this may be especially true for older patients due to increasing plausibility of death from natural causes.
In summary, we found that older age was the strongest predictor of receiving PIP among people who were prescribed opioids. We also found that PIP was associated with risk for adverse outcomes among both older and younger adults. Policy strategies are urgently needed to reduce PIP exposure among older adults and to reduce risk among those already exposed.
Supplementary Material
Definition of advanced-stage cancer
Table of milligram morphine equivalents (MME) by medication.
Definition of pain conditions
Definition of non-fatal opioid overdose
Definition of fatal opioid overdose
Definitions of depression and alcohol use disorder
Comparison of characteristics and clinical outcomes between older and younger Massachusetts adults who received prescribed opioids at least once between 2011 and 2015 (n = 3,078,163).
Acknowledgments
Funding: This research was funded by the GE Foundation (PI: Stopka). Dr. Stein was supported in part by P50DA046351–01. Dr. Larochelle was supported by NIDA (K23 DA042168), the National Center for Advancing Translational Sciences, National Institutes of Health, through BU-CTSI Grant Number 1UL1TR001430, and a Boston University School of Medicine Department of Medicine Career Investment Award. The funders had no role in the study design, methods, collection of data, analysis, manuscript writing, or decision to submit the manuscript for publication.
Footnotes
Previous Presentations: None
Conflicts of Interest: The authors report no conflicts of interest.
Disclaimer: The opinions expressed in this manuscript are those of the authors and do not represent the official views or policies of the Massachusetts Department of Public Health or the Commonwealth of Massachusetts.
References
- 1.McBain R, Rose AJ, Larochelle MR. The US Opioid Epidemic: One Disease, Diverging Tales. Preventive Medicine 2018;112:176–178. [DOI] [PubMed] [Google Scholar]
- 2.Unick GJ, Ciccarone D. US regional and demographic differences in prescription opioid and heroin-related overdose hospitalizations. Int J Drug Policy 2017;46:112–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bohnert AS, Valenstein M, Bair MJ, et al. Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA 2011;305:1315–21. [DOI] [PubMed] [Google Scholar]
- 4.Cochran G, Gordon AJ, Lo-Ciganic WH, et al. An Examination of Claims-based Predictors of Overdose from a Large Medicaid Program. Med Care 2017;55:291–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dunn KM, Saunders KW, Rutter CM, et al. Opioid prescriptions for chronic pain and overdose: a cohort study. Ann Intern Med 2010;152:85–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Garg RK, Fulton-Kehoe D, Franklin GM. Patterns of Opioid Use and Risk of Opioid Overdose Death Among Medicaid Patients. Med Care 2017;55:661–8. [DOI] [PubMed] [Google Scholar]
- 7.Gomes T, Mamdani MM, Dhalla IA, Paterson JM, Juurlink DN. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med 2011;171:686–91. [DOI] [PubMed] [Google Scholar]
- 8.Gwira Baumblatt JA, Wiedeman C, Dunn JR, Schaffner W, Paulozzi LJ, Jones TF. High-risk use by patients prescribed opioids for pain and its role in overdose deaths. JAMA Intern Med 2014;174:796–801. [DOI] [PubMed] [Google Scholar]
- 9.Park TW, Saitz R, Ganoczy D, Ilgen MA, Bohnert AS. Benzodiazepine prescribing patterns and deaths from drug overdose among US veterans receiving opioid analgesics: case-cohort study. BMJ 2015;350:h2698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yang Z, Wilsey B, Bohm M, et al. Defining risk of prescription opioid overdose: pharmacy shopping and overlapping prescriptions among long-term opioid users in medicaid. J Pain 2015;16:445–53. [DOI] [PubMed] [Google Scholar]
- 11.Zedler B, Xie L, Wang L, et al. Risk factors for serious prescription opioid-related toxicity or overdose among Veterans Health Administration patients. Pain Med 2014;15:1911–29. [DOI] [PubMed] [Google Scholar]
- 12.Rose AJ, Bernson D, Chui KKH, et al. Potentially inappropriate opioid prescribing, overdose, and mortality in Massachusetts, 2011–2015. J Gen Intern Med 2018;33:1512–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heins SE, Sorbero MJ, Jones CM, Dick AW, Stein BD. High-Risk Prescribing to Medicaid Enrollees Receiving Opioid Analgesics: Individual- and County-Level Factors. Subst Use Misuse 2018;53:1591–1601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mangoni AA, Jackson SH. Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 2004;57:6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Commonwealth of Massachusetts: Chapter 55 Report. https://www.mass.gov/files/documents/2017/08/31/legislative-report-chapter-55-aug-2017.pdf. Accessed September 13, 2018.
- 16.United States Census Bureau. American FactFinder. Available at: http://factfinder.census.gov. Accessed: May 5, 2017.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Definition of advanced-stage cancer
Table of milligram morphine equivalents (MME) by medication.
Definition of pain conditions
Definition of non-fatal opioid overdose
Definition of fatal opioid overdose
Definitions of depression and alcohol use disorder
Comparison of characteristics and clinical outcomes between older and younger Massachusetts adults who received prescribed opioids at least once between 2011 and 2015 (n = 3,078,163).