Watch a video presentation of this article
Watch the interview with the author
The careful selection of donor organs and recipients of liver transplantation (LT) is becoming increasingly important with the rising use of expanded criteria donors in an aging recipient population. Understanding the complex interplay of donor and recipient risk factors is essential to improving outcomes.
Deceased Donor Effects
Donor Risk Index
The donor risk index attempts to quantify the recipient risk of graft failure associated with donor characteristics at the time of the organ offer: a donor age greater 40 years, donation after cardiac death, split grafts, African American race, shorter height, cerebrovascular accident, and other causes of brain death (Table 1).1 However, without clear evidence of improving outcomes, its clinical utility has been questioned.2
Table 1.
Adjusted Donor Factors Significantly Associated With Liver Allograft Failure: Factors of the Donor Risk Index
| Donor Parameter | Relative Risk | 95% Confidence Interval | P Value |
|---|---|---|---|
| Age | |||
| <40 years | 1.00 | ||
| 40‐49 years | 1.17 | 1.08‐1.26 | 0.0002 |
| 50‐59 years | 1.32 | 1.21‐1.43 | <0.0001 |
| 60‐69 years | 1.53 | 1.39‐1.68 | <0.0001 |
| >70 years | 1.65 | 1.46‐1.87 | <0.0001 |
| African American race versus white race | 1.19 | 1.10‐1.29 | <0.0001 |
| Donor height (per 10‐cm decrease) | 1.07 | 1.04‐1.09 | <0.0001 |
| Cerebrovascular accident as cause of death | 1.16 | 1.08‐1.24 | <0.0001 |
| Donation after cardiac death | 1.51 | 1.19‐1.91 | 0.0006 |
| Partial/split graft | 1.52 | 1.27‐1.83 | <0.0001 |
This table has been adapted with permission from American Journal of Transplantation.1 Copyright 2006, American Society of Transplant Surgeons and American Society of Transplantation.
Donor Age
Multiple studies have illustrated the negative impact of older donors. Although there is no universally accepted age limit, one study found that the use of donors older than 70 years led to a markedly worse 5‐year patient survival rate of 47%.3 A donor age older than 40 years for recipients with hepatitis C virus (HCV) has been found to be a strong predictor of graft loss and death and is associated with the development of fibrosing cholestatic hepatitis.4, 5, 6
Hepatic Steatosis
Moderate (30%‐60%) and massive (>60%) macrovesicular steatosis has been associated with early graft dysfunction and primary nonfunction (Fig. 1). The impact of severe macrovesicular steatosis on graft survival may be greater than the impact of other donor factors, including the donor risk index. In contrast, donor microvesicular steatosis has been linked to poor early graft function when it is severe, but it does not seem to affect overall graft or patient survival.7
Figure 1.
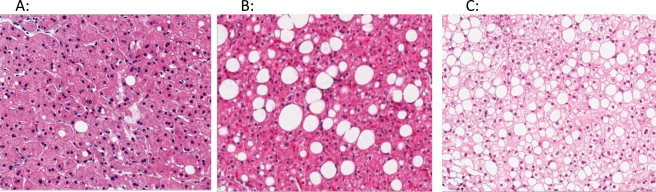
Examples of hepatic macrosteatosis (hematoxylin and eosin stains, ×10; photographs courtesy of A. Brad Farris, M.D.). (A) Mild steatosis, which is defined as <30% of hepatocytes affected (<5% in this example). (B) Moderate steatosis (30%‐60%), which has been associated in some studies with increased primary nonfunction and graft loss (∼33% in this example). (C) Severe steatosis, which is defined as >60% involvement (∼90% in this example). This is considered a contraindication to an organ's use as a donor graft.
Infections and High‐Risk Donors According to the Centers for Disease Control and Prevention
Although donors with systemic infections, a history of cardiopulmonary resuscitation, and inotropic medications are independent predictors of donor graft infection, there is no evidence of an effect on recipient survival.8 Although rare (0.96%),9 donor‐derived disease transmission (e.g., HCV and human immunodeficiency virus) is a recognized contributor to morbidity and mortality.10
Cold Ischemia Time
Cold preservation can affect graft and patient survival if it is more than 12 hours long, especially with other negative variables.11 A prolonged ischemic time has been associated with increased reperfusion injury, primary nonfunction, and the need for retransplantation.11, 12
Deceased Cardiac Donors
In an effort to expand the US donor pool, the use of donation after cardiac death organs has increased from <1% to more than 6% in the past decade. Reported outcomes vary dramatically between transplant centers because of variations in donor characteristics and surgical techniques. However, the use of donation after cardiac death organs has been associated with higher rates of primary nonfunction, nonanastomotic biliary strictures, resource utilization, renal dysfunction, and graft failure in comparison with donation after brain death organs.13, 14, 15
Sex/Race/Genetics
A multivariate analysis found that the transplantation of organs from female donors into male recipients led to lower 2‐year graft survival rates in comparison with other sex combinations.16 African American recipients of grafts from Caucasian donors and Hispanic recipients of grafts from African American donors were also found to have higher rates of graft loss and mortality than Caucasian‐matched pairs.17 The pairing of African American donors with Hispanic recipients has significantly decreased graft loss and mortality in comparison with Caucasian‐matched pairs. The effect of racial mismatch may be even more pronounced in HCV recipients, and perhaps this is related to interleukin‐28B genotypes.18, 19 Additionally, certain donor toll‐like receptor 4 gene polymorphisms have been associated with a higher rate of graft failure in all populations.20
Living Donors
One multicenter study found that living donor recipients had an increased risk of biliary leaks, re‐exploration, and vascular thrombosis.21 However, once centers had performed more than 20 procedures, the rate of nonbiliary complications was similar to the rate with deceased donation.
Recipient Effects
Models Predicting Post‐LT Outcomes
Although the Model for End‐Stage Liver Disease score is a sensitive predictor of death on the LT wait list, its use for predicting post‐LT outcomes is more limited. Other models, such as the Acute Physiology and Chronic Health Evaluation II score, the Charlson comorbidity index, and the Survival Outcomes Following Liver Transplantation score22 have been used but not fully implemented.
Etiology of Liver Disease
A recent analysis of United Network for Organ Sharing data for adult transplants from 1994 to 2009 revealed that in comparison with primary biliary cirrhosis, the 5‐year graft and patient survival rates were similar for primary sclerosing cholangitis, nonalcoholic steatohepatitis, and hepatitis B. When compared to chronic cholestatic liver disease. The graft and patient survival rates were worse for alcoholic cirrhosis and cryptogenic cirrhosis (hazard ratio = 1.3‐1.6) and worst for HCV, alcohol and HCV combined, and hepatocellular carcinoma (hazard ratio = 1.3‐2.3; Table 2).23 Although recipients with nonalcoholic steatohepatitis appear to experience more post‐LT cardiovascular events,24 graft and patient survival remain comparable to those with other etiologies.25 For recipients with HCV, independent predictors of progressive fibrosis and graft loss include female sex,26 a recipient age > 50 years (especially with older grafts),27 elevated pre‐LT HCV RNA titers (>1 × 106 vEq/mL)28, acute rejection, and HCV/human immunodeficiency virus coinfection.29
Table 2.
Recipient Factors: Cox Regression Analysis Models for Graft and Patient Survival
| Variable | Graft Survival | Patient Survival | ||
|---|---|---|---|---|
| Hazard Ratio | 95% Confidence Interval | Hazard Ratio | 95% Confidence Interval | |
| Etiology vs chronic cholestatic liver disease | ||||
| HCV | 1.61 | 1.52‐1.74 | 1.97 | 1.84‐2.11 |
| Alcoholic liver disease | 1.28 | 1.2‐1.69 | 1.64 | 1.52‐1.77 |
| Alcoholic liver disease + HCV | 1.6 | 1.46‐1.69 | 2.1 | 1.9‐2.23 |
| Nonalcoholic steatohepatitis | 1.19 | 1.04‐1.37 | 1.52 | 1.3‐1.77 |
| Chronic cholestatic | 1.27 | 1.18‐1.35 | 1.53 | 1.42‐1.66 |
| Hepatitis B virus | 1.07 | 0.96‐1.19 | 1.3 | 1.15‐1.47 |
| Hepatocellular carcinoma | 1.67 | 1.56‐1.78 | 2.15 | 1.99‐2.32 |
| Age increase (for every 10 years) | 1.09 | 1.07‐1.11 | 1.24 | 1.22‐1.27 |
| Female versus male | 0.99 | 0.96‐1.03 | 1.05 | 1.01‐1.09 |
| African American versus Caucasian | 1.28 | 1.21‐1.36 | 1.33 | 1.24‐1.42 |
| Ventilator support | 1.85 | 1.67‐2.05 | 1.63 | 1.44‐1.84 |
| Model for End‐Stage Liver Disease score increase (for every 3 points) | 1.03 | 1.03‐10.4 | 1.05 | 1.04‐1.06 |
This table has been adapted with permission from Transplantation.23 Copyright 2013, Transplantation Society.
Age
An increasing number of candidates older than 65 years are being referred for evaluation, and they are often denied because of other comorbid conditions. However, few studies (except in HCV‐positive recipients) have systematically examined the outcomes of carefully selected older recipients with minimal extrahepatic comorbidities.30
Comorbid Conditions
The incorporation of renal function into the Model for End‐Stage Liver Disease has in part increased the frequency of simultaneous liver‐kidney transplants from 2.5% in 1994 to 10.3% in 2009.23 Although simultaneous liver‐kidney transplantation is controversial, recipients have improved survival and less post‐LT renal failure in comparison with recipients of LT alone.31 Although exclusion criteria for cardiovascular disease also vary between transplant centers, post‐LT survival appears to be similar in patients with obstructive coronary artery disease and patients without obstructive coronary artery disease with current management strategies.32
Conclusions
Understanding donor and recipient risk factors for posttransplant outcomes is essential, even though the pairing of particular donor grafts with recipients is still an evolving science.
Potential conflict of interest: Nothing to report.
References
- 1. Feng S, Goodrich NP, Bragg‐Gresham JL, Dykstra DM, Punch JD, DebRoy MA, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant 2006; 6: 783‐790. [DOI] [PubMed] [Google Scholar]
- 2. Porrett PM, ter Horst M, Shaked A. Donor assessment scores: relevance and complete irrelevance. Liver Transpl 2012; 18(suppl 2): S25‐S30. [DOI] [PubMed] [Google Scholar]
- 3. Lai Q, Melandro F, Levi Sandri GB, Mennini G, Corradini SG, Merli M, et al. Use of elderly donors for liver transplantation: has the limit been reached? J Gastrointestin Liver Dis 2011; 20: 383‐387. [PubMed] [Google Scholar]
- 4. Satapathy SK, Sclair S, Fiel MI, Del Rio Martin J, Schiano T. Clinical characterization of patients developing histologically‐proven fibrosing cholestatic hepatitis C post‐liver transplantation. Hepatol Res 2011; 41: 328‐339. [DOI] [PubMed] [Google Scholar]
- 5. Verna EC, Abdelmessih R, Salomao MA, Lefkowitch J, Moreira RK, Brown RS Jr. Cholestatic hepatitis C following liver transplantation: an outcome‐based histological definition, clinical predictors, and prognosis. Liver Transpl 2013; 19: 78‐88. [DOI] [PubMed] [Google Scholar]
- 6. Lake JR, Shorr JS, Steffen BJ, Chu AH, Gordon RD, Wiesner RH. Differential effects of donor age in liver transplant recipients infected with hepatitis B, hepatitis C and without viral hepatitis. Am J Transplant 2005; 5: 549‐557. [DOI] [PubMed] [Google Scholar]
- 7. de Graaf EL, Kench J, Dilworth P, Shackel NA, Strasser SI, Joseph D, et al. Grade of deceased donor liver macrovesicular steatosis impacts graft and recipient outcomes more than the donor risk index. J Gastroenterol Hepatol 2012; 27: 540‐546. [DOI] [PubMed] [Google Scholar]
- 8. Wu TJ, Lee CF, Chou HS, Yu MC, Lee WC. Suspect the donor with potential infection in the adult deceased donor liver transplantation. Transplant Proc 2008; 40: 2486‐2488. [DOI] [PubMed] [Google Scholar]
- 9. Ison MG, Hager J, Blumberg E, Burdick J, Carney K, Cutler J, et al. Donor‐derived disease transmission events in the United States: data reviewed by the OPTN/UNOS Disease Transmission Advisory Committee. Am J Transplant 2009; 9: 1929‐1935. [DOI] [PubMed] [Google Scholar]
- 10. Ison MG, Llata E, Conover CS, Friedewald JJ, Gerber SI, Grigoryan A, et al.; for HIV‐HCV Transplantation Transmission Investigation Team . Transmission of human immunodeficiency virus and hepatitis C virus from an organ donor to four transplant recipients. Am J Transplant 2011; 11: 1218‐1225. [DOI] [PubMed] [Google Scholar]
- 11. Furukawa H, Todo S, Imventarza O, Casavilla A, Wu YM, Scotti‐Foglieni C, et al. Effect of cold ischemia time on the early outcome of human hepatic allografts preserved with UW solution. Transplantation 1991; 51: 1000‐1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Paugam‐Burtz C, Kavafyan J, Merckx P, Dahmani S, Sommacale D, Ramsay M, et al. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Liver Transpl 2009; 15: 522‐529. [DOI] [PubMed] [Google Scholar]
- 13. Skaro AI, Jay CL, Baker TB, Wang E, Pasricha S, Lyuksemburg V, et al. The impact of ischemic cholangiopathy in liver transplantation using donors after cardiac death: the untold story. Surgery 2009; 146: 543‐552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jay C, Ladner D, Wang E, Lyuksemburg V, Kang R, Chang Y, et al. A comprehensive risk assessment of mortality following donation after cardiac death liver transplant—an analysis of the national registry. J Hepatol 2011; 55: 808‐813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Leithead JA, Tariciotti L, Gunson B, Holt A, Isaac J, Mirza DF, et al. Donation after cardiac death liver transplant recipients have an increased frequency of acute kidney injury. Am J Transplant 2012; 12: 965‐975. [DOI] [PubMed] [Google Scholar]
- 16. Brooks BK, Levy MF, Jennings LW, Abbasoglu O, Vodapally M, Goldstein RM, et al. Influence of donor and recipient gender on the outcome of liver transplantation. Transplantation 1996; 62: 1784‐1787. [DOI] [PubMed] [Google Scholar]
- 17. Layden JE, Cotler SJ, Grim SA, Fischer MJ, Lucey MR, Clark NM. Impact of donor and recipient race on survival after hepatitis C‐related liver transplantation. Transplantation 2012; 93: 444‐449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Saxena V, Lai JC, O'Leary JG, Verna EC, Brown RS Jr, Stravitz RT, et al.; for Consortium to Study Health Outcomes in HCV Liver Transplant Recipients . Recipient‐donor race mismatch for African American liver transplant patients with chronic hepatitis C. Liver Transpl 2012; 18: 524‐531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Duarte‐Rojo A, Veldt BJ, Goldstein DD, Tillman HL, Watt KD, Heimbach JK, et al. The course of posttransplant hepatitis C infection: comparative impact of donor and recipient source of the favorable IL28B genotype and other variables. Transplantation 2012; 94: 197‐203. [DOI] [PubMed] [Google Scholar]
- 20. Oetting WS, Guan W, Schladt DP, Leduc RE, Jacobson PA, Matas AJ, et al. Donor polymorphisms of toll‐like receptor 4 associated with graft failure in liver transplant recipients. Liver Transpl 2012; 18: 1399‐1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Freise CE, Gillespie BW, Koffron AJ, Lok AS, Pruett TL, Emond JC, et al.; for A2ALL Study Group . Recipient morbidity after living and deceased donor liver transplantation: findings from the A2ALL Retrospective Cohort Study. Am J Transplant 2008; 8: 2569‐2579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rana A, Hardy MA, Halazun KJ, Woodland DC, Ratner LE, Samstein B, et al. Survival Outcomes Following Liver Transplantation (SOFT) score: a novel method to predict patient survival following liver transplantation. Am J Transplant 2008; 8: 2537‐2546. [DOI] [PubMed] [Google Scholar]
- 23. Singal AK, Guturu P, Hmoud B, Kuo YF, Salameh H, Wiesner RH. Evolving frequency and outcomes of liver transplantation based on etiology of liver disease. Transplantation 2013; 95: 755‐760. [DOI] [PubMed] [Google Scholar]
- 24. Vanwagner LB, Bhave M, Te HS, Feinglass J, Alvarez L, Rinella ME. Patients transplanted for nonalcoholic steatohepatitis are at increased risk for postoperative cardiovascular events. Hepatology 2012; 56: 1741‐1750. [DOI] [PubMed] [Google Scholar]
- 25. Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology 2011; 141: 1249‐1253. [DOI] [PubMed] [Google Scholar]
- 26. Lai JC, Verna EC, Brown RS Jr, O'Leary JG, Trotter JF, Forman LM, et al.; for Consortium to Study Health Outcomes in HCV Liver Transplant Recipients (CRUSH‐C) . Hepatitis C virus‐infected women have a higher risk of advanced fibrosis and graft loss after liver transplantation than men. Hepatology 2011; 54: 418‐424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Selzner M, Kashfi A, Selzner N, McCluskey S, Greig PD, Cattral MS, et al. Recipient age affects long‐term outcome and hepatitis C recurrence in old donor livers following transplantation. Liver Transpl 2009; 15: 1288‐1295. [DOI] [PubMed] [Google Scholar]
- 28. Charlton M, Seaberg E, Wiesner R, Everhart J, Zetterman R, Lake J, et al. Predictors of patient and graft survival following liver transplantation for hepatitis C. Hepatology 1998; 28: 823‐830. [DOI] [PubMed] [Google Scholar]
- 29. Terrault NA, Roland ME, Schiano T, Dove L, Wong MT, Poordad F, et al.; for Solid Organ Transplantation in HIV: Multi‐Site Study Investigators . Outcomes of liver transplant recipients with hepatitis C and human immunodeficiency virus coinfection. Liver Transpl 2012; 18: 716‐726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Abecassis M, Bridges ND, Clancy CJ, Dew MA, Eldadah B, Englesbe MJ, et al. Solid‐organ transplantation in older adults: current status and future research. Am J Transplant 2012; 12: 2608‐2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fong TL, Khemichian S, Shah T, Hutchinson IV, Cho YW. Combined liver‐kidney transplantation is preferable to liver transplant alone for cirrhotic patients with renal failure. Transplantation 2012; 94: 411‐416. [DOI] [PubMed] [Google Scholar]
- 32. Wray C, Scovotti JC, Tobis J, Niemann CU, Planinsic R, Walia A, et al. Liver transplantation outcome in patients with angiographically proven coronary artery disease: a multi‐institutional study. Am J Transplant 2013; 13: 184‐191. [DOI] [PubMed] [Google Scholar]


