Watch a video presentation of this article
Noncirrhotic portal hypertension comprises diseases of the liver manifesting with portal hypertension due to intrahepatic or prehepatic lesions in the absence of cirrhosis. Noncirrhotic portal fibrosis (NCPF) or idiopathic portal hypertension (IPH) is a common cause of noncirrhotic intrahepatic portal hypertension and has been reported worldwide. Other terms for this condition used throughout the world include obliterative venopathy, hepatoportal sclerosis, and idiopathic noncirrhotic portal hypertension (NCPH).1 The various denominations for noncirrhotic intrahepatic portal hypertension are outlined in Table 1. NCPF/IPH is characterized by the involvement of small and medium portal vein (PV) branches and periportal fibrosis.1 Extrahepatic portal vein obstruction (EHPVO) is an extrahepatic cause of NCPH and has been defined as “a vascular disorder of liver, characterized by obstruction of the extrahepatic PV with or without involvement of intrahepatic PV radicles or splenic or superior mesenteric veins.”2 Other causes of noncirrhotic intrahepatic portal hypertension are listed in Table 2.
Table 1.
Denominations for Noncirrhotic Intrahepatic Portal Hypertension
| Noncirrhotic portal fibrosis (NCPF) |
| Idiopathic portal hypertension (IPH) |
| Idiopathic noncirrhotic portal hypertension (INCPH) |
| Obliterative venopathy |
| Hepatoportal sclerosis |
Table 2.
Causes of Noncirrhotic Intrahepatic Portal Hypertension
| Noncirrhotic portal fibrosis, idiopathic portal hypertension, idiopathic noncirrhotic portal hypertension |
| Schistosomiasis |
| Primary or secondary biliary cirrhosis (precirrhosis) |
| Congenital hepatic fibrosis |
| Veno‐occlusive disease |
| Nodular regenerative hyperplasia |
| Partial nodular transformation |
| Peliosis hepatis |
Etiology and Pathogenesis
Systemic and intra‐abdominal infections, toxin and medication exposure, immunological phenomena, and prothrombotic state are the broad etiological factors with a potential role in the disease (Table 3).3 The pathogenesis is not well understood, particularly for noncirrhotic intrahepatic portal hypertension. Sarin and Kumar3 presented a unifying common hypothesis for both NCPF/IPH and EHPVO wherein a major thrombotic event in the main PV at a young age results in EHPVO, whereas repeated microthrombotic events in smaller and medium‐sized (<300 μm) branches lead to NCPF. Schouten et al.4 explained idiopathic noncirrhotic portal hypertension (INCPH) by presenting a dual theory of intrahepatic venous obstruction (obliterative venopathy) and increased splenic blood flow (due to high levels of endothelial nitric oxide synthase and inducible nitric oxide synthase). Sato and Nakanuma5 described a third concept of endothelial mesenchymal transition for IPH in which the vascular endothelial cells of portal venules acquire myofibroblastic features.5
Table 3.
Etiological Factors for NCPH
| Etiological Factor | Agents/Causes | Mechanisms |
|---|---|---|
| Systemic and intra‐abdominal infections | Bacteria, protozoa, schistomsomiasis | Infections lead to portal pyemia leading to thrombosis, sclerosis, and obstruction |
| Toxins and medications | Arsenic, vinyl chloride, vitamin A, copper sulphate, methotrexate, 6‐mercaptopurine, azathioprine, didanosine, irradiation | Fibrogenic process |
| Immunological | SLE, scleroderma, celiac disease, hypo‐gammaglobulinemia, HLA DR3 | Immunological factors causing perivenular inflammation, cell recruitment, and fibrosis |
| Prothrombotic state | Myeloproliferative disorders, MTHFR deficiency, protein C and S deficiency, ACLA, prothrombin gene mutation | Thrombogenic process |
Abbreviations: ACLA, anticardiolipin antibody; HLA, human leukocyte antigen; MTHFR, methylenetetrahydrofolate reductase.
Presentation and Diagnosis
NCPF usually presents in young males between the third and fourth decade of life, whereas IPH (in Japan) and INCPH (in the West) presents in the fifth decade of life with a female preponderance.6 The major presenting symptoms in Japanese patients with IPH are splenomegaly (88%), hepatomegaly (44%), gastrointestinal bleeding (35%), and ascites (12%). Patients with NCPF commonly present with splenomegaly (74%‐97%), variceal bleed (65%‐72%), anemia (90%), and ascites (10%‐25%). INCPH in the West usually manifests with less common splenomegaly (26%‐36%), variceal bleed (32%‐55%), and more common ascites (34%) than NCPF and IPH. Variceal bleed is usually well tolerated. Ascites and hepatic encephalopathy are usually precipitated by bleed or shunt surgery. Jaundice and signs of chronic liver disease are rare. Anemia and thrombocytopenia are more common in NCPF than IPH. Coagulation and platelet function abnormalities are seen despite a procoagulant cause. A pilot study in NCPH (NCPF/EHPVO) showed that a latent hypercoagulable state may be evident on thromboelastographic evaluation.7 Hypersplenism is seen in 27%‐87% of patients. Liver function tests are invariably normal. Endoscopy may reveal esophageal varices in 80%‐90% of patients with NCPF/IPH and in 33%‐43% of patients with INCPH. Esophageal varices are larger than those seen in patients with cirrhosis. Gastric and anorectal varices are more common, whereas portal hypertensive gastropathy is less common than cirrhosis.6 Imaging in NCPF reveals a normal, enlarged, or shrunken liver and large spleen with dilated and patent splenoportal axis, thickened PV (>3 mm), Gandy–Gamna bodies in the enlarged spleen. A withered tree appearance due to sudden narrowing of intrahepatic branches may also be seen. Spontaneous shunts are seen in 15.9% of patients and decrease the risk of variceal bleeding.8 Wedged hepatic venous pressure is usually normal, whereas intrasplenic and PV pressures are elevated.6 Nuclear imaging technetium‐99m sulphur colloid scanning has been shown to differentiate NCPF from cirrhosis by demonstrating patchy uptake of colloids in cirrhosis and a significant colloid shift to bone marrow.9 ARFI elastography shows that liver stiffness in IPH is lower than cirrhosis and similar to chronic hepatitis whereas splenic stiffness is highest in IPH and lowest in chronic hepatitis.10 The major histological features in NCPH are shown in Fig. 1. Noncirrhotic intrahepatic portal hypertension needs to be differentiated from EHPVO and cirrhosis; the differences are outlined in Table 4.
Figure 1.
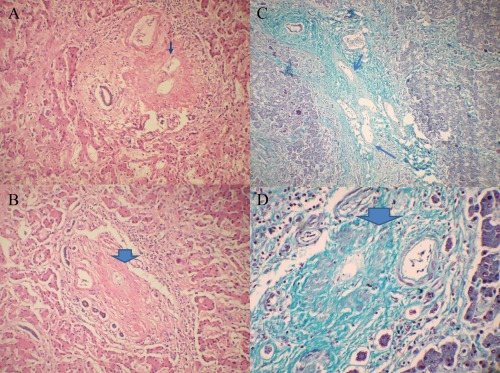
Histology in noncirrhotic intrahepatic portal hypertension. A combination of photomicrographs depicting the obliterative changes in the portal veins is shown. (A) Thick portal vein with fibrous obliteration of lumen (hematoxylin and eosin stain). (B) Near complete fibrous occlusion of portal venous radicle (hematoxylin and eosin stain). (C) Multiple dilated portal venous radicles in a portal tract (Masson's trichrome stain). (D) Markedly occluded thick walled portal venous radicle (Masson's trichrome stain).
Table 4.
Differences Between Noncirrhotic Intrahepatic Portal Hypertension, EHPVO, and Cirrhosis
| NCPF/IPH/INCPH | EHPVO | Cirrhosis | |
|---|---|---|---|
| Mean age (years) | 30 (NCPF), 50 (IPH/INCPH) | 10 | 40 |
| Upper GI bleed | Well tolerated | Well tolerated | Not well tolerated |
| Ascites and HE | Transient and precipitated by bleed | Transient and precipitated by bleed | Common |
| Jaundice | Uncommon | Uncommon | Common |
| Liver | Normal, rarely irregular | Normal or small | Small nodular |
| Splenomegaly | Massive | Moderate to massive | Mild |
| Liver function tests | Normal | Normal | Deranged |
| Imaging | Normal SP axis, withered tree appearance | Portal cavernomatous transformation | Irregular shrunken liver, dilated portal and splenic vein |
| Hemodynamics | |||
| Intrasplenic pressure | High | High | High |
| PV pressure | High | Normal to raised | High |
| WHVP | Normal to raised | Normal | High |
| Long‐term survival | Good | Good | Worse |
Abbreviations: GI, gastrointestinal; HE, hepatic encephalopathy; SP, spleno‐portal; WHVP, wedged hepatic vein pressure.
Natural History
NCPF has a long‐term survival of 100% with endoscopic eradication of varices and 80% with shunt surgery. However, up to one‐third of patients may have progressive liver dysfunction, leading to decompensation and need for liver transplantation. Ascites and hepatic encephalopathy have been reported to occur in 26% and 7% of patients, respectively, with IPH on long‐term follow up. The 1‐year probability of developing portal vein thrombosis (PVT) is 9%, and 53% of patients show recanalization with anticoagulation. HIV and variceal bleeding at diagnosis are independent predictors of PVT in IPH.11 A study of explant liver from India showed that 9 (2.4%) out of 84 (22.6%) patients with cryptogenic cirrhosis had evidence of NCPF on pathological examination, emphasizing the natural course of decompensation in NCPF.12 NCPF accounts for 5% of end‐stage liver disease patients who undergo liver transplantation.13 The probability of transplantation‐free survival is 82% at 10 years in IPH, and the 1‐year probability of first variceal bleed (in large varices) despite primary prophylaxis is 9%. Ascites at presentation and severe associated disorders are markers of poor survival.11 Liver transplantation has been done in severe cases of portal hypertension, advanced disease, and hepatopulmonary syndrome, but sufficient data are lacking.
Management
Treatment with endoscopic sclerotherapy and endoscopic variceal ligation are both effective in the eradication of varices. Endoscopic variceal ligation is faster in eradicating varices with less bleeding rates but with increased recurrence rates. The role of drug therapy alone or in combination in noncirrhotic intrahepatic portal hypertension is lacking. There are insufficient data at present to recommend the use of beta blockers for primary or secondary prophylaxis. However, Sarin et al.14 showed that for secondary prophylaxis, endoscopic variceal ligation was no more effective than beta blockers. Gastric varices as a cause of bleed are usually managed with cyanoacrylate glue injection, in contrast to esophageal varices, for which band ligation is the recommendation. Portosystemic shunting is indicated in cases of uncontrolled or recurrent portal hypertensive bleed and failed endotherapy. Transjugular intrahepatic portosystemic shunt or shunt surgery can be considered for failed endotherapy, ectopic variceal bleed, symptomatic hypersplenism, noncompliance with endoscopic therapy, severe growth retardation, and poor chance of follow‐up.15 Shunts may be selective or nonselective. Shunt surgery is effective in NCPF with reduction in splenic pulp pressure and splenic size after a successful patent shunt surgery.16 Symptomatic hypersplenism is treated with shunt surgery with or without splenectomy. A recent retrospective analysis of surgery in hypersplenism over 10 years showed effective normalization of hypersplenism with splenectomy with or without shunt surgery. Shunt surgery, like proximal splenorenal shunt, also takes care of underlying portal hypertension.17
Anticoagulation is controversial and is currently not recommended for patients with NCPF/IPH and EHPVO; however, in noncirrhotic intrahepatic portal hypertension, it may be recommended for patients who develop PVT.
Abbreviations
- EHPVO
extrahepatic portal vein obstruction
- INCPH
idiopathic noncirrhotic portal hypertension
- IPH
idiopathic portal hypertension
- NCPF
noncirrhotic portal fibrosis
- NCPH
noncirrhotic portal hypertension
- PV
portal vein
- PVT
portal vein thrombosis.
Potential conflict of interest: Nothing to report.
References
- 1. Sarin SK, Kumar A, Chawla YK, Baijal SS, Dhiman RK, Jafri W, et al. Noncirrhotic portal fibrosis/idiopathic portal hypertension: APASL recommendations for diagnosis and treatment. Hepatol Int 2007;1:398‐413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sarin SK, Sollano JD, Chawla YK, Amarapurkar D, Hamid S, Hashizume M, et al. Members of the APASL working party on portal hypertension. Consensus on extra‐hepatic portal vein obstruction. Liver Int 2006;26:512‐519. [DOI] [PubMed] [Google Scholar]
- 3. Sarin SK, Kumar A. Noncirrhotic portal hypertension. Clin Liver Dis 2006;10:627‐651. [DOI] [PubMed] [Google Scholar]
- 4. Schouten JNL, Garcia‐Pagan JC, Valla DC, Janssen HL. Idiopathic noncirrhotic portal hypertension. Hepatology 2011;54:1071‐1081. [DOI] [PubMed] [Google Scholar]
- 5. Sato Y, Nakanuma Y. Role of endothelial‐mesenchymal transition in idiopathic portal hypertension. Histol Histopathol 2013;28:145‐154. [DOI] [PubMed] [Google Scholar]
- 6. Khanna R, Sarin SK. Non‐cirrhotic portal hypertension—diagnosis and management. J Hepatol 2014;60:421‐441. [DOI] [PubMed] [Google Scholar]
- 7. Kapoor S, Pal S, Sahni P, Chattopadhyay TK. Thromboelastographic evaluation of coagulation in patients with extrahepatic portal vein thrombosis and non‐cirrhotic portal fibrosis: a pilot study. J Gastroenterol Hepatol 2009;24:992‐997. [DOI] [PubMed] [Google Scholar]
- 8. Dhiman RK, Chawla Y, Vasishta RK, Kakkar N, Dilawari JB, Trehan MS, et al. Non‐cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol 2002;17:6‐16. [DOI] [PubMed] [Google Scholar]
- 9. Chakraborty D, Sunil HV, Mittal BR, Bhattacharya A, Singh B, Chawla Y. Role of Tc99m sulfur colloid scintigraphy in differentiating non‐cirrhotic portal fibrosis from cirrhosis liverRole of Tc99m sulfur colloid scintigraphy in differentiating non cirrhotic portal fibrosis from cirrhosis liver. Indian J Nucl Med 2010;25:139‐142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Furuichi Y, Moriyasu F, Taira J, Sugimoto K, Sano T, Ichimura S, et al. Noninvasive diagnostic method for idiopathic portal hypertension based on measurements of liver and spleen stiffness by ARFI elastography. J Gastroenterol 2013;48:1061‐1068. [DOI] [PubMed] [Google Scholar]
- 11. Siramolpiwat S, Seijo S, Miquel R, Berzigotti A, Garcia‐Criado A, Darnell A, et al. Idiopathic portal hypertension: natural history and long‐term outcome. Hepatology 2013. doi: 10.1002/hep.26904. [DOI] [PubMed] [Google Scholar]
- 12. Nayak NC, Jain D, Vasdev N, Gulwani H, Saigal S, Soin A. Etiologic types of end‐stage chronic liver disease in adults: analysis of prevalence and their temporal changes from a study on native liver explants. Eur J Gastroenterol Hepatol 2012;24:1199‐1208. [DOI] [PubMed] [Google Scholar]
- 13. Saigal S, Nayak NC, Jain D, Kumaran V, Mohanka R, Saraf N, et al. Non‐cirrhotic portal fibrosis related end stage liver disease in adults: evaluation from a study on living donor liver transplant recipients. Hepatol Int 2011;5:882‐889. [DOI] [PubMed] [Google Scholar]
- 14. Sarin SK, Gupta N, Jha SK, Agrawal A, Mishra SR, Sharma BC, et al. Equal efficacy of endoscopic variceal ligation and propranolol in preventing variceal bleeding in patients with noncirrhotic portal hypertension. Gastroenterology 2010;139:1238‐1245. [DOI] [PubMed] [Google Scholar]
- 15. Chawla Y, Duseja A, Dhiman RK. Review article: the modern management of portal vein thrombosis. Aliment Pharmacol Ther 2009;30:881‐894. [DOI] [PubMed] [Google Scholar]
- 16. Sharma BC, Singh RP Chawla YK, Narasimhan KL, Rao KL, Mitra SK. Effect of shunt surgery on spleen size, portal pressure and esophageal varices in non cirrhotic portal fibrosis. J Gastroenterol Hepatol 1997;12:582‐584. [DOI] [PubMed] [Google Scholar]
- 17. Rajalingam R, Javed A, Sharma D, Sakhuja P, Singh S, Nag HH, et al. Management of hypersplenism in non cirrhotic portal hypertension: a surgical series. Hepatobiliary Pancreat Dis Int 2012;11:165‐171. [DOI] [PubMed] [Google Scholar]


