Abstract
Background:
Psychiatry inpatients frequently have co-occurring substance use and mental health disorders, which are related to poor post-discharge outcomes. Telephone monitoring is effective in specialty substance use disorder treatment settings in increasing continuing care and 12-step program utilization and improving substance use outcomes. This study examined the effectiveness of telephone monitoring among psychiatry inpatients with co-occurring substance use and mental health disorders.
Methods:
This randomized controlled trial (n=406) compared usual care to usual care plus telephone monitoring (one in-person session during the inpatient stay, followed by weekly telephone contact for three months post-discharge). Follow-ups were conducted at end-of-intervention (3 months post-baseline) and 9 and 15 months post-baseline (73% followed). Primary outcomes were number of days, out of the past 30, of drinking alcohol, using drugs, and experiencing psychological problems. Secondary outcomes were outpatient substance use treatment, and 12-step group, utilization.
Results:
Longitudinal modeling found that patients in both conditions improved over time on each primary outcome. Improvement was comparable between conditions on alcohol and drug use and psychological problems. Receipt of outpatient treatment decreased over the follow-up period and was not related to condition. Likelihood of attending 12-step group meetings did not change over follow-ups, and was not related to condition.
Conclusions:
Among these patients, improvement over time was evident regardless of condition assignment. Patients maintained attendance at 12-step groups from pre- to post-discharge. Short-term telephone monitoring in addition to usual care for patients with co-occurring substance use and mental health disorders may not be sufficiently intensive to achieve additional improvements on outcomes.
Keywords: Substance use, mental health, co-occurring, telephone monitoring, 12-step groups
1. Introduction
Substance use and mental health disorders frequently co-occur. Population-based surveys indicate that over 8.4 million adults in the US have co-occurring substance use and mental health disorders (SAMHSA, 2014). Specifically, over 30% of people with mental illness, and over 50% of people with severe mental illness, will experience a substance use disorder in their lifetime (SAMHSA, 2014). Co-occurring disorders are associated with greater symptom severity and poorer functioning than either disorder alone (Merikangas & Kalaydjian, 2007).
The impact of co-occurring substance use and mental health disorders is particularly striking in clinical settings. Among all inpatient stays in the US by patients with a primary substance use or mental health disorder diagnosis, stays involving co-occurring conditions were more common (45% of all stays) than those involving a substance use or mental health disorder diagnosis alone (15% and 39% of stays, respectively) (Heslin et al., 2015). Substance use disorders co-occurring with mental health disorders are associated with an increased likelihood of negative outcomes, including poor management of the psychiatric condition and greater likelihood of additional use of health services (Fleury et al., 2015).
The period immediately following a psychiatry inpatient stay is of high risk for adverse patient outcomes, including suicide (Valenstein et al., 2009; Olfsen et al., 2016). However, among psychiatry inpatients with co-occurring substance use and mental health disorders, greater engagement in post-discharge substance use disorder outpatient care was associated with a lower likelihood of rehospitalization (Ilgen et al., 2008). These findings highlight the importance of developing and testing novel interventions to improve use of outpatient substance use disorder treatment and 12-step groups, and outcomes, among patients with co-occurring substance use and mental health disorders following an inpatient psychiatry treatment episode.
1.1. Telephone monitoring
Telephone monitoring was developed to provide ongoing support and improve participation in continuing substance use disorder care and outcomes among substance use disorder patients who had achieved initial stabilization during a substance use disorder treatment episode (Stout et al., 1999). Telephone monitoring is utilized to maintain a relationship with the patient using the key elements of continued low-intensity contact via supportive and non-judgmental interactions, monitoring of substance use and other major life problems, reinforcing the use of continuing substance use disorder care, and facilitating entry into more active treatment as necessary. Research demonstrates that telephone monitoring improves substance use outcomes among substance use disorder patients. In a randomized trial of patients with alcohol use disorders, at one-year post-intervention, the frequency of heavy drinking was twice as high among controls (24%) than among telephone-monitored patients (12%) who received telephone calls on a tapering schedule. Telephone-monitored patients had 73% fewer emergency room visits and 58% fewer substance-related hospitalizations during the year (Hilton et al., 2001).
Subsequently, McKay and colleagues (2004, 2005) randomized patients who had completed outpatient intensive treatment for alcohol or cocaine use disorders to one of three conditions: telephone monitoring (one face-to-face session followed by weekly calls for three months), in-person relapse prevention, and in-person 12-step group counseling. At one-year and two-year follow-ups, the telephone condition was generally as or more effective in terms of improved outcomes as the two face-to-face conditions (McKay et al., 2004; 2005). Patients in the telephone monitoring condition also sustained higher levels of 12-step group participation, and more 12-step participation predicted a higher likelihood of abstinence across four-month and two-year follow-ups (Mensinger et al., 2007). An analysis of a telephone monitoring intervention for adults with cocaine dependence found it to be a cost-effective and potentially cost saving strategy for reducing substance use (McCollister et al., 2016). In contrast to robust findings of the McKay studies, a randomized controlled trial that assigned intensive substance use disorder outpatients to six months of telephone monitoring or usual care found that telephone-monitored patients achieved better substance use and psychiatric outcomes at 3-month, but not at 12-month, follow-up (McKellar et al. 2012).
In summary, research in specialty substance use disorder treatment shows that telephone monitoring is effective for increasing substance use continuing care utilization (i.e., outpatient substance use disorder treatment and 12-step group attendance after discharge from the current treatment setting) and improving substance use outcomes. The present study built on these prior results and contributed important new clinical knowledge by determining whether telephone monitoring is similarly effective when adapted for veteran psychiatry inpatients with co-occurring substance use and mental health disorders. Importantly, patients in the prior studies were already engaged in the substance use disorder treatment system. The telephone monitoring intervention was delivered following an episode of intensive treatment and most participants had already reduced or eliminated their substance use. In contrast, psychiatry inpatients may not be aware of or convinced that they have, and need help with, a substance use disorder. Patients with both substance use and mental health disorders often view their psychiatric problem as primary, deny their substance use problems, and perceive substance-focused care as minimizing problems of living with psychiatric disabilities, and as inhibiting freedom to discuss and obtain new information about psychiatric illnesses (Priester et al., 2016).
The present study used a randomized design in which patients newly admitted to psychiatry inpatient treatment with co-occurring substance use and mental health disorders were assigned to usual care or usual care plus telephone monitoring. Patients were followed at 3 months (end-of-intervention for telephone-monitored patients), 9 months, and 15 months post-baseline to determine whether telephone monitoring was associated with better outcomes compared to no monitoring. To enhance the findings’ clinical usefulness, primary outcomes assessed the number of days in the past 30 days the patient had used alcohol and drugs and had psychological difficulties. To examine the effectiveness of telephone monitoring at facilitating use of continuing care, we also examined the secondary outcomes of outpatient substance use disorder treatment utilization and 12-step group attendance.
2. Material and methods
2.1. Sample and procedures
Patients entering inpatient psychiatry treatment at one of two health care facilities within the same health care system were included on the basis of having been consecutively screened by the case manager as (a) being dually diagnosed, i.e., having substance use and mental health disorders documented in the medical record, (b) having sufficient cognitive functioning to understand study procedures, i.e., able to answer the Orientation and Registration questions from the Mini-Mental State Examination (Tombaugh & McIntyre, 1992), and (c) self-reported having access to a cell or land line telephone when not hospitalized. After receiving a study introduction, participants signed an informed consent form and completed the baseline interview. Study procedures were approved by Stanford University’s Institutional Review Board (IRB) for Human Subjects, and the Veterans Affairs Ann Arbor Health Care System IRB.
According to medical records, participants were admitted to inpatient care for solely substance use reasons (14%, e.g., heroin overdose), solely psychiatric reasons (40%, e.g., suicide attempt), or both substance use and psychiatric reasons (46%, e.g., suicidal ideation in context of recent heavy crack cocaine use). The modal length of stay was seven days (interquartile range=five to 13 days). A total of 29 participants left inpatient treatment against medical advice. Participants’ psychiatric diagnoses were mainly depression (78.1%), anxiety disorder (63.4%), PTSD (41.3%), schizophrenia or schizoaffective disorder (29.1%), and bipolar disorder (16.9%); 67% had alcohol use disorders and 53% had drug use disorders. (Percentages of psychiatric and substance use disorders add to more than 100% because some participants had more than one of each type of disorder.)
After the baseline interview, participants were randomly assigned by the project manager to condition (usual care or usual care plus telephone monitoring) using permuted blocking whereby ID numbers to be given sequentially to patients were randomly preselected within different sized blocks to be assigned to each condition. Regarding follow-ups, the research assistant, blinded to patients’ condition assignment, collected self-report data from patients by telephone at three months post-baseline, which was upon completion of the intervention for the group in the telephone monitoring condition. Self-report data were also collected six months and one year after the three-month follow-up (nine and 15 months post-baseline). We used an intent-to-treat design and so followed all participants irrespective of participation in the intervention. Follow-ups were conducted by telephone because not all patients resided in close geographical proximity to the inpatient facility.
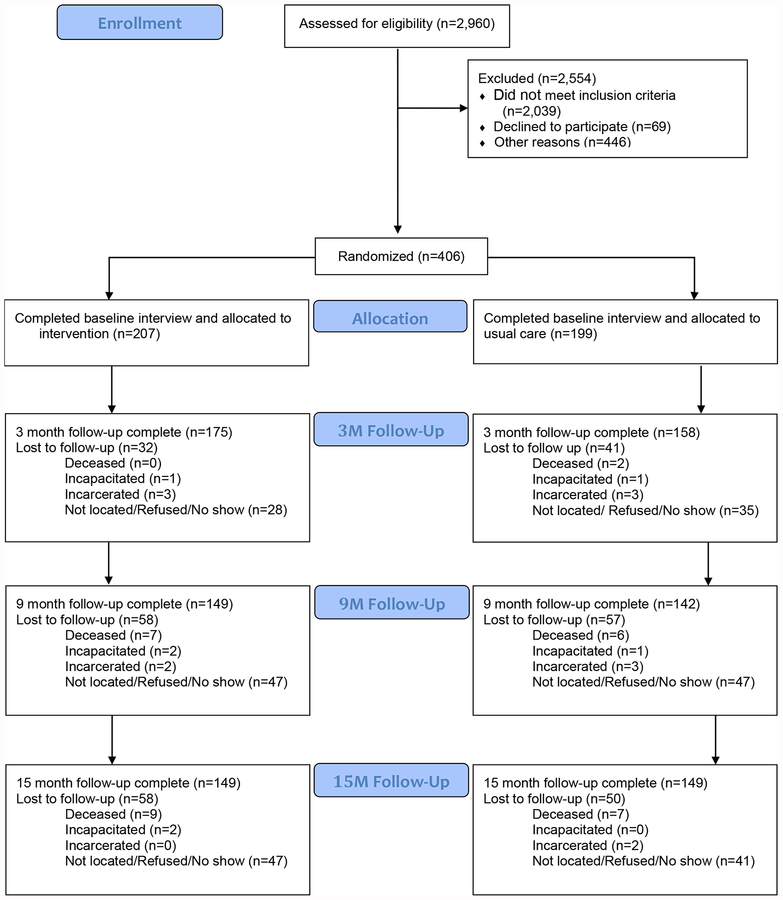
Figure 1 summarizes the flow of patients through the trial. Of the 2,960 patients who were assessed for eligibility, 406 were randomly assigned. The sample size was determined by conducting a power analysis on primary and secondary outcomes; specifically, power was based on the expected observation of at least a medium effect size (.50) between the two conditions in substance use outcomes, outpatient treatment entry, and 12-step group participation. A sample size of 392 (196 in each condition) was calculated as allowing an 80% likelihood of detecting a medium effect size at the 5% level of significance (two-tailed test). The trial was stopped when follow-up procedures for all enrolled participants were completed (2/28/16). Excluded were 2,554 patients because of refusal (n=69), ineligibility (n=2,039), or other reason (e.g., were discharged before the baseline was complete; n=446). In all, 199 patients were randomly assigned to usual care; of these, 158 (79.4%) were followed at three months, 142 (71.4%) at nine months, and 149 (74.9%) at 15 months. In addition, 207 patients were randomly assigned to the usual care plus telephone monitoring condition; 175 (84.5%) were followed at three months, 149 (72.0%) at nine months, and 149 (72.0%) at 15 months. The usual care and usual care plus telephone monitoring patients lost to follow-up were deceased, incarcerated, incapacitated, or unable to be located, located but refused, or located and agreed to, but did not complete, an interview (Figure 1).
Figure 1:
Flow of patients through the trial.
Baseline comparisons on demographic characteristics of patients followed or not followed at 3, 9, and 15 months post-baseline found that followed participants were older than those lost to follow-up (3 months: M=45.6 (SD=12.4) vs. M=41.9 (SD=14.4), t=2.22, p=.027; 9 months: 46.0 (12.3) vs. 42.1 (13.7), t=2.84, p=.005; 9 months: 46.1 (12.4) vs. 41.4 (13.6), t=3.33, p=.001). Otherwise, there were no differences on gender, race, education, or marital, employment, or housing status. Baseline comparisons on substance use and psychiatric diagnoses of patients followed or not followed at 3, 9, and 15 months post-baseline did not identify any differences.
2.2. Conditions
2.2.1. Usual care.
Inpatient psychiatry treatment used a biopsychosocial approach involving stabilizing patients. Participants received a multidisciplinary assessment within 72 hours of admission. Interventions included comprehensive assessment, psychopharmacology, individual and group psychotherapy, and behavioral interventions. Each patient met daily with the treatment team to evaluate progress, address problems, and review the treatment plan.
2.2.2. Usual care plus telephone monitoring.
Telephone monitoring was delivered by trained Telephone Monitors, who were licensed, master’s-level clinical social workers. Participants assigned to this condition received one 30 to 50-minute in-person session during hospitalization followed by monitoring over the telephone, which was planned for one phone call per week for three months, with each phone call planned to last approximately 15 minutes. The in-person session followed procedures for Session 1 in McKay and colleagues’ (2010a) manual for implementing telephone monitoring with individuals transitioning from more to less intensive substance use disorder treatment; it integrated motivational interviewing principles to address the participant’s awareness of having a substance use disorder (Miller & Rollnick, 1992) and provided specific orientation to the telephone monitoring protocol. Discussions between Telephone Monitors and participants were designed to raise possible discrepancies between using substances and meeting goals. This session also introduced the idea of a change plan, and began to address post-discharge engagement in substance use disorder treatment and 12-step groups, as well as keeping mental health and medical appointments. Patients were oriented to the protocol by going over how calls would work, and a time was set for the first telephone monitoring session.
During each telephone session, which also followed procedures in McKay and colleagues’ (2010a) manual, patients answered a Risk Assessment Worksheet (McKellar et al., 2012) covering behaviors since the previous call, i.e., substance use, psychiatric symptoms, compliance with substance use and mental health treatment (including medications), and participation in 12-step groups. Telephone Monitors positively reinforced any steps toward recovery, and reacted in a non-judgmental fashion to setbacks such as relapsing to substance use. Patients were expected to answer calls at predetermined times. When a patient failed to answer a call, the Telephone Monitor made at least two more attempts to contact the patient for the scheduled contact, and when successful, reasons for the missed call were discussed. The Telephone Monitor continued to attempt to contact the patient weekly for 12 weeks, irrespective of how many calls were completed or missed.
Of 207 patients randomized to usual care plus telephone monitoring, 180 (87%) completed at least one phone call with the Telephone Monitor. The mean number of phone calls completed was 7.6 (SD=3.2), and the range was 0–12 (14% [n=26] completed all 12). The percent of intervention participants who completed the weekly phone call drifted downward over the follow-up period, i.e., 73% Week 1, 62% Week 6, 44% Week 12. After in-person training sessions with clinical experts in motivational interviewing with the study’s patient population, a start-up practice phase was conducted during which Telephone Monitors were certified after delivering the intervention to enrolled patients who were considered training cases and not included in analyses. Telephone Monitors received regular supervision from a doctoral-level, licensed clinician that included review of session content and feedback on adherence to the manual, using a protocol checklist (McKellar et al., 2012).
2.3. Outcome measures
Primary outcomes were items on the Addiction Severity Index (McLellan et al., 2006) with regard to the past 30 days: number of days used alcohol; number of days used drugs (summed across 10 drugs including non-medical use of prescription drugs and capped at 30), and number of days troubled or bothered by psychological or emotional problems. Secondary outcomes were receipt of any outpatient alcohol and/or drug treatment in the past 30 days (no or yes), and attendance of any 12-step groups (no or yes) in the past year (at baseline) or since the previous assessment (at follow-ups).
2.4. Data Analysis
Longitudinal, hierarchical mixed modeling was conducted to assess the within-person random effects and the between-person fixed effects of interest in the examination of study outcomes. There were distributions of time to follow-up around each target of 3, 9, and 15 months; thus, elapsed time in months was a random, within-persons effect, and the baseline outcome measure served as a person-specific random intercept. The random effects were blocked on facility. Preliminary data exploration suggested that the model form might not be linear, and that the baseline outcome was an important contributor to outcome change over time. To address these issues, the baseline measure of the outcome was included in each longitudinal model, which included data from the follow-up time points only. Past 30-day alcohol use, drug use, and psychological problems were treated as counts and modeled via a Poisson distribution with log link function. Outpatient addiction treatment utilization was examined as a binary indicator variable with values of (1) any treatment was obtained vs. (0) no treatment was obtained. Twelve-step meeting attendance was evaluated in terms of (1) any meetings attended vs. (0) no meetings attended. Categorical outcomes were modeled via the Binary or Multinomial distribution, as appropriate, with log link function. Analyses were carried out with the GLIMMIX procedure in SAS 13.2.
3. Results
3.1. Baseline
Baseline characteristics of patients randomly assigned to the usual care or usual care plus telephone monitoring condition are shown in Table 1.
Table 1.
Baseline characteristics of usual care (n=199) and telephone monitoring (n=207) patients.
| Demographics | Usual care | Telephone monitoring |
|---|---|---|
| Male (percent, n) | 92.0 (183) | 90.9 (188) |
| White (percent, n) | 64.1 (127) | 62.0 (128) |
| Age (M, SD) | 45.2 (12.6) | 45.1 (12.6) |
| Married (percent, n) | 20.1 (40) | 12.5 (26) |
| Years of education (M, SD) | 13.4 (2.2) | 13.5 (1.9) |
| Employed (percent, n) | 43.9 (87) | 48.8 (101) |
| Homeless (percent, n) | 14.6 (29) | 12.1 (25) |
| Number of days in past 30 days: | ||
| Drank alcohol (M, SD) | 8.8 (9.6) | 9.1 (9.3) |
| Used drugs (M, SD) | 9.4 (11.6) | 10.3 (11.6) |
| Psychological problems (M, SD) | 21.5 (9.9) | 23.2 (9.6) |
| Use of continuing care: | ||
| Any outpatient substance use disorder treatment (percent, n) | 12.8 (25) | 15.3 (31) |
| Any 12-step group meetings (percent, n) | 47.9 (95) | 56.9 (118) |
Note: M=Mean, SD=Standard Deviation
3.2. Longitudinal analyses
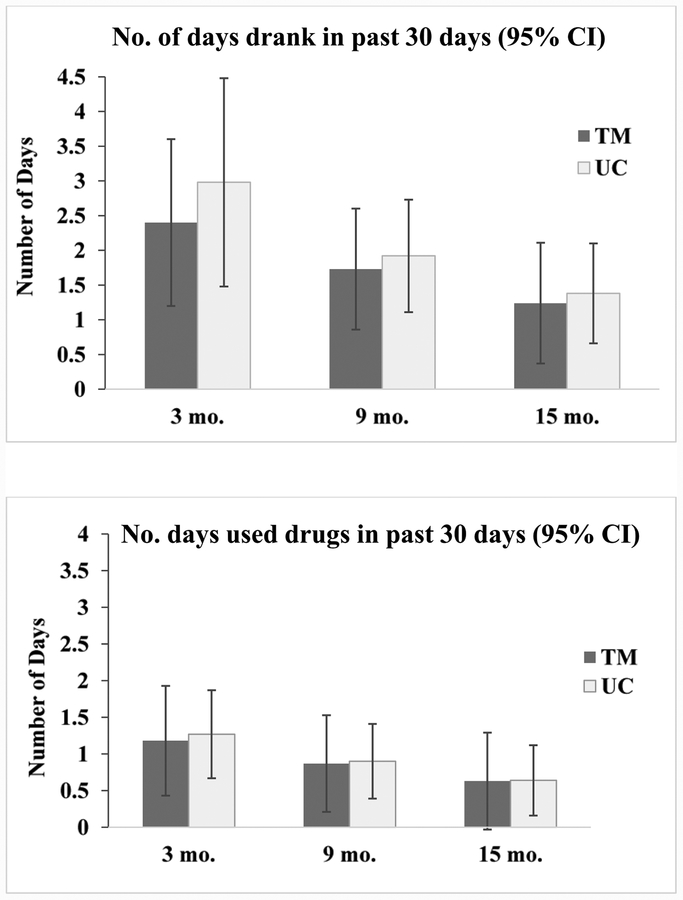
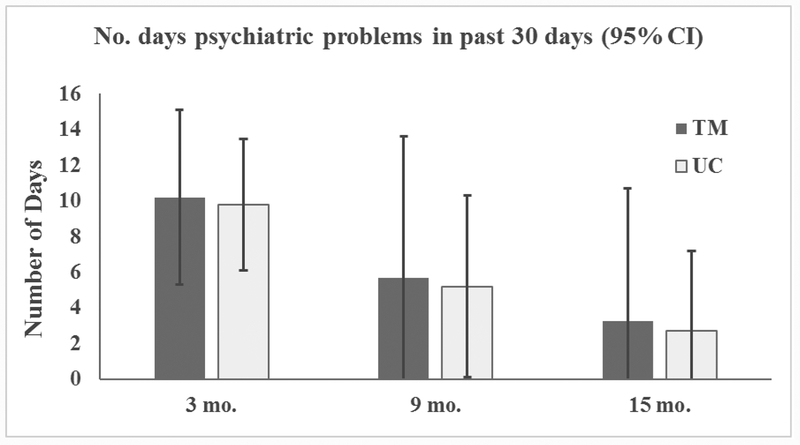
Table 2 presents results for longitudinal modeling of the outcomes of past 30-day alcohol use, drug use, and being bothered by psychological problems; Figure 2 presents model-based estimates of the means and confidence intervals by condition at each follow-up. More baseline alcohol use in the past 30 days significantly predicted greater alcohol use over the follow-up (βlog(se) = 0.073 (0.014); p<0.01, Table 2). Mean number of days of alcohol use in the past 30 decreased significantly over the follow-up interval (βlog(se) = −0.056 (0.018); p<0.01). However, there was not a significant difference between conditions in days of alcohol use during the follow-up interval (βlog(se) = −0.217 (0.174); ns). In addition, the interaction between time and treatment condition on alcohol use was not significant (βlog(se) = 0.001 (0.024); ns). Similarly, greater baseline drug use in the past 30 days predicted more drug use in the 30 days prior to each follow-up (βlog(se) = 0.078 (0.013); p<0.01) and number of drug use days in the past 30 days decreased with time (βlog(se) = −0.062 (0.024); p<0.01), with no significant difference between conditions (βlog(se) = −0.174 (0.317); ns) or significant interaction of time by condition (βlog(se) = 0.009 (0.033); ns). Past 30-day psychological problems at baseline were associated with past 30-day psychological problems over the follow-up (βlog(se) = 0.021 (0.005); p<0.01), and decreased over time (βlog(se) = −0.118 (0.053); p<0.01), with no significant difference by condition (βlog(se) = 0.0003 (0.096); ns) or interaction of time by condition (βlog(se) = 0.023 (0.040); ns).
Table 2.
Longitudinal modeling of primary outcomes.
| Number of days in past 30 days | |||
|---|---|---|---|
| Used alcohol B (se) | Used drugs B (se) | Psychological problems B (se) | |
| Intercept | 0.383 (0.127)a | −0.672 (0.269)a | 2.14 (0.130)a |
| Baseline value | 0.073 (0.014)a | 0.078 (0.013)a | 0.021 (0.005)a |
| Time (mos.) | −0.056 (0.018)a | −0.062 (0.024)a | −0.118 (0.053)b |
| Condition | |||
| Monitoring | −0.217 (0.174) | −0.174 (0.317) | 0.0003 (0.096) |
| Usual care | (referent) | (referent) | (referent) |
| Time*Condition | |||
| Monitoring | 0.001 (0.024) | 0.009 (0.033) | 0.023 (0.040) |
| Usual care | (referent) | (referent) | (referent) |
| Fit statistics | Gen. X2/df = 1.85 | Gen. X2/df = 1.64 | Gen. X2/df = 1.83 |
| Type III p-values | |||
| Baseline | <0.01 | <0.01 | <0.01 |
| Time | <0.01 | <0.01 | <0.01 |
| Condition | 0.21 | 0.58 | 0.99 |
| Time*Condition | 0.97 | 0.77 | 0.75 |
p<.01;
p<.05
Note: Outcomes were assessed at 3-, 9-, and 15-month follow-ups.
Figure 2.
Model-based estimates (95% confidence interval) at each follow-up for primary outcomes.
Note: For the TM group, at 3, 9, and 15 months, respectively, number of days drank in past 30 days: Ms (SDs)=3.3 (5.6), 3.8 (6.6) and 3.9 (6.6); number of days used drugs in past 30 days: Ms (SDs)=3.9 (7.2), 5.7 (9.5), and 5.6 (9.3); and number of days of psychiatric problems in past 30 days: Ms (SDs)=15.3 (12.0), 14.2 (11.7), and 14.0 (13.8). For the UC group, at 3, 9, and 15 months, respectively, number of days drank in past 30 days: Ms (SDs)=3.8 (6.0), 5.0 (7.4) and 5.3 (7.7); number of days used drugs in past 30 days: Ms (SDs)=4.8 (7.9), 5.0 (8.9), and 5.5 (9.2); and number of days of psychiatric problems in past 30 days: Ms (SDs) = 13.9 (11.7), 14.9 (12.3), and 12.6 (13.0).
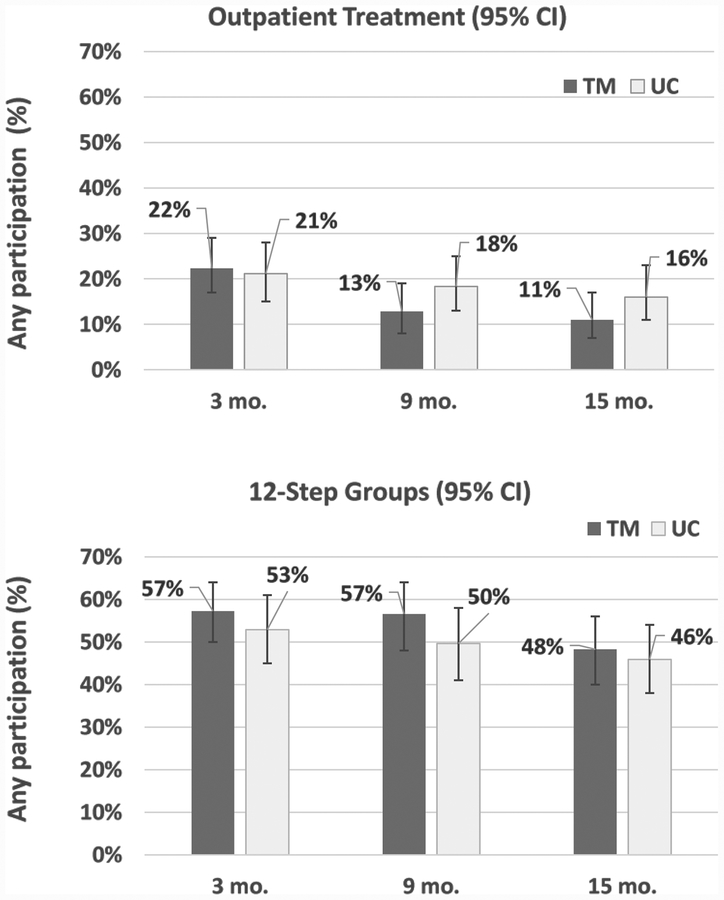
Table 3 presents longitudinal findings for any outpatient addiction treatment and any 12-step meeting attendance; results are presented graphically in Figure 3. Patients who had received outpatient treatment prior to baseline were more likely to receive such treatment during follow-up (βlog(se) = 0.677 (0.331); p<0.05). The odds of receiving treatment decreased significantly over the follow-up (βlog(se) = −0.043 (0.029); p<0.01. There was not a significant effect for condition on odds of receiving treatment (βlog(se) = 0.347 (0.399); ns), or a significant interaction of time by condition (βlog(se) = −0.072 (0.043), ns). For odds of 12-step attendance, baseline attendance was significantly related to follow-up attendance (βlog(se) = 2.183 (0.243); p<0.01), but time was not related to attendance over the follow-up (βlog(se) = −0.046 (0.030); ns). Treatment condition was not significantly related to odds of 12-step attendance (βlog(se) = 0.312 (0.395); ns), nor was there a significant interaction between time and treatment condition (βlog(se) =−0.022 (0.041); ns).
Table 3.
Longitudinal modeling of secondary outcomes.
| Outpatient treatment B (se) | 12-step group attendance B (se) | |
|---|---|---|
| Intercept | −1.339 (0.289) | −0.681 (0.295) |
| Baseline value | 0.677 (0.331)b | 2.183 (0.243)a |
| Time (mos.) | −0.043 (0.029)a | −0.046 (0.030) |
| Condition | ||
| Monitoring | 0.347 (0.399) | 0.312 (0.395) |
| Usual care | (referent) | (referent) |
| Time*Condition | ||
| Monitoring | −0.072 (0.043) | −0.022 (0.041) |
| Usual care | (referent) | (referent) |
| Fit statistics | Gen. X2/df = 0.68 | Gen. X2/df = 0.61 |
| Type III p-values | ||
| Baseline | <0.05 | <0.01 |
| Time | <0.01 | 0.12 |
| Condition | 0.39 | 0.43 |
| Time*Condition | 0.09 | 0.59 |
p<.01;
p<.05
Figure 3.
Prevalence (95% confidence interval) at each follow-up for secondary outcomes.
4. Discussion
In this randomized controlled trial of psychiatry inpatients with co-occurring substance use and mental health disorders, a low-intensity telephone monitoring intervention based on motivational interviewing was not associated with reductions in substance use or psychological symptoms, or increases in utilization of continuing care, relative to the usual care condition. The telephone monitoring intervention was intended to facilitate use of continuing care, which was specified as substance use treatment and 12-step groups after discharge. Participants in both the usual care and usual care plus telephone monitoring conditions reduced their substance use and psychiatric distress over the study period of 15 months. These participants also showed decreases over time in the likelihood of receiving outpatient treatment, but maintained relatively consistent levels of participation in 12-step groups over the follow-up period.
One possible reason for the intervention’s lack of effectiveness is that these patients were already receiving sufficient levels of mental health or substance-related continuing care such that telephone monitoring had little incremental value. Indeed, among telephone-monitored patients, 60%, 64%, and 54% received continuing mental health outpatient care at the 3-, 9-, and 15-month follow-ups, respectively; among usual care patients, corresponding percentages were 65%, 63%, and 59%. In this regard, Rosen et al. (2013) examined whether adding a telephone care management protocol to usual continuing care improved patients’ outcomes in the year after discharge from residential mental health treatment; over one-half of study participants had co-occurring mental health and substance use disorders. They found no differences in substance use, psychiatric symptoms, time to first outpatient visit or rehospitalization, or number of outpatient visits between patients who received telephone care management and usual care at four months or one year postdischarge. The lack of differences was attributed to the high utilization of mental health care services post-discharge by study participants.
Subsequently, Rosen et al. (2017) examined whether adding telephone care management (twice-per-month phone calls for three months) to usual outpatient mental health care improved treatment attendance and clinical outcomes of mental health patients; few patients (6% of usual care, and 16% of telephone monitored) had co-occurring substance use disorders. Telephone monitoring patients completed more mental health visits during the intervention period than usual care patients. However, telephone monitoring and usual care patients did not differ on treatment visits at the last (one-year) follow-up, or on substance use or psychiatric symptoms at any follow-up. Rosen et al. (2017) concluded that, even when telephone monitoring increases treatment attendance, treatment outcomes depend upon treatment effectiveness. More broadly, it is possible that, as health care systems prioritize linkage to post-inpatient services, the incremental benefit of brief interventions such as telephone continuing care is diminished.
In our study, few patients in either condition received outpatient substance use disorder treatment in the 30 days prior to the baseline assessment or any follow-up; the greatest likelihood of treatment occurred at the 3-month follow-up when 22% and 21% of the telephone monitored and usual care patients, respectively, were receiving outpatient substance use disorder treatment. Our findings are consistent with general population surveys reporting that, among people with co-occurring disorders, more accessed specialty mental health than specialty substance use care (Han et al., 2017; Ubanoski et al., 2017). Regarding reasons that relatively low proportions of patients received specialty substance use care, other studies found that inpatient psychiatry staff members often report negative attitudes toward patients with co-occurring disorders, have a lack of training in how to address substance use, difficulty in accessing supervisors with such training, and that poor communication and coordination exist between inpatient psychiatry and outpatient substance use treatment settings (Danda, 2012; Howard & Holmshaw, 2010).
However, we found that about one-half of patients had attended 12-step group meetings prior to baseline and each follow-up. Again, the greatest likelihood of 12-step group attendance occurred at the 3-month follow-up when 57% of telephone monitored patients, and 53% of usual care patients, attended. For many individuals with co-occurring disorders, peers in 12-step groups in the community are the prevailing resource for support beyond any ongoing treatment (Donovan & Floyd, 2008; Matusow et al., 2013; Timko & Sempel, 2004). Twelve-step group involvement, whether substance-focused (e.g., Alcoholics Anonymous) or dual-focused (e.g., Double Trouble in Recovery), is beneficial in reducing both substance use and mental health symptom severity among individuals with co-occurring disorders (Bogenschutz et al., 2014; Rosenblum et al., 2014; Timko et al., 2013). Possibly, the benefits of 12-step attendance were further enhanced when, as was the case in the present sample, the majority of participants were receiving other mental health services. Our finding that participants without prior 12-step group or outpatient treatment participation were less likely to engage with these settings suggests that this subset of patients may benefit from brief linkage approaches to initiate 12-step group participation (Cucciare & Timko, 2015; Timko et al., 2011).
In both our and Rosen et al.’s (2013, 2017) studies, the lack of advantage for the telephone monitoring condition on outcomes occurred despite having successfully delivered the intervention. In our study, 87% of patients assigned to telephone monitoring completed at least one phone call with the telephone monitor, and a mean of eight phone calls were completed. In Rosen et al.’s (2013) study, telephone monitors completed at least one call for 86% of participants in the intervention condition, and patients contacted by phone completed an average of four of six planned calls. These telephone call “doses” are comparable to those in other trials of telephone interventions with mental health patients (Cook et al., 2008; Seal et al., 2012). However, studies focused on patients with substance use disorders (Hilton et al., 2001; McKay et al., 2004, 2005, 2010b) conducted telephone monitoring over a much longer period than used in our or others’ (Seal et al., 2012; Rosen et al., 2013, 2017) research. For example, McKay et al.’s (2010b) telephone monitoring consisted of tapering telephone contacts for 18 months. The benefits of monitoring appeared to be stronger between months 10–15 of follow-up, with deterioration of effects over the final three months. Together, studies suggest that longer periods of monitoring may be necessary and any benefits of telephone monitoring may not be sustained beyond the period of the active monitoring intervention.
In additional analyses of their data, McKay et al.’s (2011) examination of several moderators found in part that telephone monitoring was more effective than usual care among women but not among men, although the benefits of telephone monitoring were not sustained at a 24-month follow-up for either women or men; in addition, women in usual care had particularly poor outcomes. In another analysis of data from cocaine-dependent patients examining 10 potential moderators, McKay et al. (2014) found no significant main or moderator effects for gender on outcomes, but the size of effects favoring telephone monitoring over usual care were somewhat larger among women than men. Thus, the present study’s sample being mainly men may have contributed to the lack of effects of the telephone monitoring intervention. In addition, McKay and colleagues’ studies suggest future directions for analyses of this study’s data to examine potential subgroups for whom the telephone monitoring intervention may have been effective, such as patients with more motivation to reduce substance use. Findings from these analyses may indicate selected subsets of patients to whom health systems should target telephone monitoring interventions.
We found that patients in both conditions improved on alcohol and drug use and psychiatric symptoms over the 15-month follow-up period. Other studies of patients with co-occurring substance use and mental health disorders have similarly found that these patients improve on severity of both disorders following receipt of treatment, even when treatment targets one disorder but does not specifically target the other disorder (Hunter et al., 2012; Watkins et al., 2011). For example, psychiatric medications are effective for the treatment of substance use as well as mental health disorders when these disorders co-occur (Agabio et al., 2018; Kelly et al., 2012; Murthy & Chand, 2012). However, experts recommend that treatment services for individuals with substance use and mental health disorders should be well-coordinated in terms of addressing the co-occurring disorders, take a multidisciplinary, team approach, and provide for long-term follow-up (Horsfall et al., 2009).
More specifically, our clinical experience delivering telephone monitoring to these patients resonates with the research literature on improving treatments for individuals with both substance use and psychiatric disorders. We concur with the robust support found for Motivational Interviewing for establishing a therapeutic alliance between providers and patients with co-occurring disorders (Kelly et al., 2012). Indeed, studies of patients with co-occurring disorders identified trust between patients and providers as the basis for treatment engagement and recovery (Brekke et al., 2018; Newman et al., 2015). In addition, in light of participants’ experience with 12-step groups, we concur with the potential use of peers to help this patient population. Having a peer on the treatment team of patients with co-occurring disorders was associated with better fidelity to treatment plans, more engagement in care (e.g., outpatient care after hospital discharge), and better outcomes (e.g., reduced substance use and mental health symptoms) (Harrison et al., 2017; O’Connell et al., 2017). Further, to enhance use of outpatient treatments after hospital discharge, new integrated treatments should continue to be developed and tested, such as cognitive behavioral therapies for co-occurring substance use and anxiety disorders (McHugh, 2015; McHugh et al., 2017), and combined behavioral and pharmacotherapies for alcohol use disorders and depression (Samakhvalov et al., 2017).
4.1. Limitations
Despite this study’s strengths (e.g., high retention rates among this difficult-to-follow patient population), there were also limitations. Patients were mainly male and all were initially treated in one health care system, the Veterans Health Administration (VHA). Compared to non-veterans, veterans are more likely to have health insurance, but report poorer health generally, greater numbers of chronic conditions, and more frequent serious psychological distress and work limitations (Kramarow & Pastor, 2012). Therefore, study participants may not represent patients with co-occurring disorders who are treated in the community. However, VHA is the largest health care system and provider of mental health and substance use treatment services in the US, and systematic reviews show that health care provided in VHA is similar to that in non-VHA health care systems (Trivedi et al., 2011). More specifically, community rates of outpatient treatment after inpatient psychiatry discharge are quite similar to those reported in this study (Smith et al., 2016). Another limitation was the lack of more complete data to corroborate participants’ self-reports of substance use. Although substance use reports were assessed by trained staff using validated instruments and procedures to aid recall and minimize bias, and studies support the veracity of individuals’ self-reports of substance use (Napper et al., 2010; SAMSHA, 2010), future studies should consider methods requiring biological testing or collateral reports.
4.2. Conclusions
The patients with co-occurring mental health and substance use disorders in our study were psychiatrically hospitalized during an acute crisis, such as a period of symptom exacerbation or an overdose episode or posing harm to self (a suicide attempt) or others (homicidal ideation). Our findings suggest that these patients improve over time after they are discharged from inpatient care, and that a telephone monitoring intervention during the post-discharge period was not associated with more use of continuing care or improvement on substance use or mental health outcomes than usual care. However, we also observed that many of these patients may maintain a stable social network in the form of peers participating in 12-step groups, which are free of charge and widely available. Gaining a better understanding of how more patients may more fully utilize this resource may be helpful to their well-being. In addition, it is important to continue to develop and test novel methods to improve post-discharge outcomes among those receiving intensive services for co-occurring substance-related and mental health problems.
Acknowledgments
This research was supported by an Investigator Initiated Research project (IAC 09–055 to Dr. Timko and Dr. Ilgen as Multiple Principal Investigators), Senior Research Career Scientist Award (RCS 00–001 to Dr. Timko), and Research Career Scientist Award (RCS 14–232 to Dr. Harris) by the Department of Veterans Affairs (VA) Health Services Research and Development (HSR&D) Service (Clinical Trials.gov; NCT00135420). The views expressed are the authors’ and do not necessarily reflect those of the VA. No conflicts of interest are reported by any of the authors listed on this manuscript.
References
- Agabio R, Trogu E, Pani PP, 2018. Antidepressants for the treatment of people with co-occurring depression and alcohol dependence. Cochrane Database of Systematic Reviews, 4, CD008581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogenschutz MP, Rice SL, Tonigan JS, Vogel HS, Nowinski J, Hume D, Arenella PB, 2014. 12-step facilitation for the dually diagnosed: A randomized clinical trial. Journal of Substance Abuse Treatment, 46(4), 403–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brekke E, Lien L, Biong S, 2018. Experiences of professional helping relations by persons with co-occurring mental health and substance use disorders. International Journal of Mental Health and Addiction, 16(1), 53–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality, 2014. 2013 National Survey on Drug Use and Health: Mental Health Detailed Tables. Substance Abuse and Mental Health Services Administration, Rockville, MD. [Google Scholar]
- Cook PF, Emiliozzi S, Waters C, El Hajj D, 2008. Effects of telephone counseling on anti- psychotic adherence and emergency department utilization. American Journal of Managed Care, 14, 841–846. [PubMed] [Google Scholar]
- Cucciare MA, Timko C, 2015. Bridging the gap between medical settings and specialty addiction treatment. Addiction, 110(9), 1417–1419. [DOI] [PubMed] [Google Scholar]
- Danda MC, 2012. Attitudes of health care professionals towards addictions clients accessing mental health services. Journal of Ethics in Mental Health, 7, 1–5. [Google Scholar]
- Donovan DM, Floyd AS, 2008. Facilitating involvement in twelve-step programs. Recent Developments in Alcoholism, 18, 303–320. [DOI] [PubMed] [Google Scholar]
- Fleury MJ, Grenier G, Bamvita JM, Caron J, 2015. Profiles associated respectively with substance dependence only, mental disorders only and co-occurring disorders. Psychiatric Quarterly, 86(3), 355–371. [DOI] [PubMed] [Google Scholar]
- Han B, Compton WM, Blanco C, Colpe LJ, 2017. Prevalence, treatment, and unmet treatment needs of US adults with mental health and substance use disorders. Health Affairs, 36(10), 1739–1747. [DOI] [PubMed] [Google Scholar]
- Harrison J, Cousins L, Spybrook J, Curtis A, 2017. Peers and co-occurring research-supported interventions. Journal of Evidence-Informed Social Work, 14(3), 201–215. [DOI] [PubMed] [Google Scholar]
- Heslin KC, Elixhauser A, Steiner CA, 2015. Hospitalizations involving mental and substance use disorders among adults, 2012 HCUP Statistical Brief #191. Agency for Healthcare Research and Quality, Rockville, MD. [PubMed] [Google Scholar]
- Hilton ME, Maisto SA, Conigliaro J, McNiel M, Kraemer K, Kelley ME, Conigliaro R, Samet JH, Larson MJ, Savetsky J, Winter M, Sullivan LM, Saitz R, Weisner C, Mertens J, Parthasarathy S, Moore C, Hunkeler E, Hu TW, Selby J, Stout RL, Zywiak W, Rubin A, Zwick W, Shepard D, 2001. Improving alcoholism treatment across the spectrum of services. Alcoholism, Clinical and Experimental Research, 25(1), 128–135. [PubMed] [Google Scholar]
- Horsfall J, Cleary M, Hunt GE, Walter G, 2009. Psychosocial treatments for people with co-occurring severe mental illnesses and substance use disorders (dual diagnosis): A review of empirical evidence. Harvard Review of Psychiatry, 17(1), 24–34. [DOI] [PubMed] [Google Scholar]
- Howard V, Homshaw J, 2010. Inpatient staff perceptions in providing care to individuals with co-occurring mental health problems and illicit substance use. Journal of Psychiatric and Mental Health Nursing, 17(10), 862–72. [DOI] [PubMed] [Google Scholar]
- Hunter SB, Watkins KE, Hepner KA, Paddock SM, Ewing BA, Osilla KC, Perry S, 2012. Treating depression and substance use: A randomized controlled trial. Journal of Substance Abuse Treatment, 43(2), 137–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ilgen MA, Hu KU, Moos RH, McKellar J, 2008. Continuing care after inpatient psychiatric treatment for patients with psychiatric and substance use disorders. Psychiatric Services, 59(9), 982–988. [DOI] [PubMed] [Google Scholar]
- Kelly TM, Daley DC, Douaihy AB, 2012. Treatment of substance abusing patients with comorbid psychiatric disorders. Addictive Behaviors, 37(1):11–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kramarow EA, Pastor PN, 2012. The health of male veterans and nonveterans aged 25–64. National Center for Health Statistics, Centers for Disease Control and Prevention, Hyattsville, MD. [Google Scholar]
- Matusow H, Dickman SL, Rich JD, Fong C, Dumont DM, Hardin C, Marlowe D, Rosenblum A, 2013. Medication assisted treatment in US drug courts: Results from a nationwide survey of availability, barriers and attitudes. Journal of Substance Abuse Treatment, 44(5), 473–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCollister K, Yang X, McKay JR, 2016. Cost-effectiveness analysis of a continuing care intervention for cocaine-dependent adults. Drug & Alcohol Dependence, 158, 38–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, 2015. Treatment of co-occurring anxiety disorders and substance use disorders. Harvard Review of Psychiatry, 23(2), 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHugh RK, Votaw VR, Barlow DH, Fitzmaurice GM, Greenfield SF, Weiss RD, 2017. Development of an integrated cognitive behavioral therapy for anxiety and opioid use disorder. Contemporary Clinical Trials, 60, 105–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM, 2005. The effectiveness of telephone-based continuing care for alcohol and cocaine dependence: 24-month outcomes. Archives of General Psychiatry, 62(2), 199–207. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinati HM, 2004. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12-month outcomes. Journal of Consulting and Clinical Psychology, 72(6), 967–979. [DOI] [PubMed] [Google Scholar]
- McKay JR, Van Horn DH, Lynch KG, Ivey M, Cary MD, Drapkin M, Coviello D, 2014. Who benefits from extended continuing care for cocaine dependence? Addictive Behaviors, 39(3), 660–668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn DH, Morrison R, 2010a. Telephone Continuing Care Therapy for Adults. Hazelden, Minnesota. [Google Scholar]
- McKay JR, Van Horn DH, Oslin DW, Lynch KG, Ivey M, Ward K, Drapkin ML, Becher JR, Coviello DM, 2010b. A randomized trial of extended telephone-based continuing care for alcohol dependence: Within-treatment substance use outcomes. Journal of Consulting and Clinical Psychology, 78(6), 912–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Van Horn D, Oslin DW, Ivey M, Drapkin ML, Covielle DM, Yu Q, Lynch KG, 2011. Extended telephone-based continuing care for alcohol dependence: 24-month outcomes and subgroup analyses. Addiction, 106(10), 1760–1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKellar J, Wagner T, Harris A, Oehlert M, Buckley S, Moos R, 2012. One-year outcomes of telephone case monitoring for patients with substance use disorder. Addictive Behaviors, 37(10), 1069–1074. [DOI] [PubMed] [Google Scholar]
- McLellan TA, Cacciola JC, Alterman AI, Rikoon SH, Carise C, 2006. The Addiction Severity Index at 25: Origins, contributions, and translations. The American Journal on Addictions, 15 (2), 113–124. [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Lynch KG, TenHave TR, McKay JR, 2007. Mediators of telephone-based continuing care for alcohol and cocaine dependence. Journal of Consulting and Clinical Psychology, 75(5), 775–784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas KR, Kalaydjian A, 2007. Magnitude and impact of comorbidity of mental disorders from epidemiologic surveys. Current Opinion in Psychiatry, 20(4), 353–358. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S, 1991. Motivational Interviewing: Preparing People to Change Addictive Behavior. Guilford Press, New York. [Google Scholar]
- Murthy P, Chand P, 2012. Treatment of dual diagnosis disorders. Current Opinion in Psychiatry, 25(3), 194–200. [DOI] [PubMed] [Google Scholar]
- Napper LE, Fisher DG, Johnson ME, Wood MM, 2010. The reliability and validity of drug users’ self reports of amphetamine use among primarily heroin and cocaine users. Addictive Behaviors, 35(4), 350–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman D, O’Reilly P, Lee SH, Kennedy D, 2015. Mental health service users’ experiences of mental health care: An integrative literature review. J of Psychiatric and Mental Health Nursing, 22(3), 171–82. [DOI] [PubMed] [Google Scholar]
- O’Connell MJ, Flanagan EH, Delphin-Rittmon ME, Davidson L, 2017. Enhancing outcomes for persons with co-occurring disorders through skills training and peer recovery support. J of Mental Health, 10, 1–6. [DOI] [PubMed] [Google Scholar]
- Olfson M, Wall M, Wang S, Crystal S, Liu SM, Gerhard T, Blanco C, 2016. Short-term suicide risk after psychiatric hospital discharge. JAMA Psychiatry, 73(11), 1119–1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Priester MA, Browne T, Iachini A, Clone S, DeHart D, Seay KD, 2016. Treatment access barriers and disparities among individuals with co-occurring mental health and substance use disorders: an integrative literature review. Journal of Substance Abuse Treatment, 61, 47–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen CS, Azevedo KJ, Tiet QQ, Greene CJ, Wood AE, Calhoun P, Bowe T, Capehart BP, Crawford EF, Greenbaum MA, Harris AH, Hertzberg M, Lindley SE, Smith BN, Schnurr PP, 2017. An RCT of effects of telephone care management on treatment adherence and clinical outcomes among veterans with PTSD. Psychiatric Services, 68(2), 151–158. [DOI] [PubMed] [Google Scholar]
- Rosen CS, Tiet QQ, Harris AH, Julian TF, McKay JR, Moore WM.. Schnurr PP, 2013. Telephone monitoring and support after discharge from residential PTSD treatment: A randomized controlled trial. Psychiatric Services, 64(1), 13–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum A, Matusow H, Fong C, Vogel H, Uttaro T, Moore TL, Magura S, 2014. Drug and Alcohol Dependence, 135, 78–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samokhvalov AV, Awan S, George TP, Irving J, Le Foll B, Perrotta S, Probst C, Voore P, Rehm J, 2017. Integrated care pathway for co-occurring major depressive and alcohol use disorders. The American Journal on Addictions, 26(6), 602–609. [DOI] [PubMed] [Google Scholar]
- Seal KH, Abadjian L, McCamish N, Shi Y, Tarasovsky G, Weingardt K, 2012. A randomized controlled trial of telephone motivational interviewing to enhance mental health treatment engagement in Iraq and Afghanistan veterans. General Hospital Psychiatry 34, 450–459. [DOI] [PubMed] [Google Scholar]
- Smith TE, Abraham M, Bolotnikova NV, Donahue SA, Essock SM, Ofson M, Shao WS, Wall MM, Radigan M, 2016. Psychiatric inpatient discharge planning practices and attendance at aftercare appointments. Psychiatric Services, 68(1), 92–95. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, 2010. Reliability of Key Measures in the National Survey on Drug Use and Health, Office of Applied Studies, Rockville, MD. [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Adminisration, 2014. 2013 National Survey on Drug Use and Health, Center for Behavioral Health Statistics and Quality, Rockville, MD. [Google Scholar]
- Stout RL, Rubin A, Zwick W, Zywiak W, Bellino L, 1999. Optimizing the cost-effectiveness of alcohol treatment: A rationale for extended case monitoring. Addictive Behaviors, 24(1), 17–35. [DOI] [PubMed] [Google Scholar]
- Timko C, Cronkite RC, McKellar J, Zemore S, Moos RH, 2013. Dually diagnosed patients’ benefits of mutual-help groups and the role of social anxiety. Journal of Substance Abuse Treatment, 44(2), 216–223. [DOI] [PubMed] [Google Scholar]
- Timko C, Sempel JM, 2004. Intensity of acute services, self-help attendance and one-year outcomes among dual diagnosis patients. Journal of Studies on Alcohol, 65(2), 274–282. [DOI] [PubMed] [Google Scholar]
- Timko C, Sutkowi A, Cronkite RC, Makin-Byrd K, Moos RH, 2011. Intensive referral to 12-step dual-focused mutual-help groups. Drug and Alcohol Dependence, 118(2–3), 194–201. [DOI] [PubMed] [Google Scholar]
- Tombaugh TN, McIntyre NJ, 1992. The mini‐mental state examination: a comprehensive review. Journal of the American Geriatrics Society, 40(9), 922–935. [DOI] [PubMed] [Google Scholar]
- Trivedi AN, Matula S, Miake-Lye I, Glassman PA, Shekelle P, Asch S, 2011. Systematic review: comparison of the quality of medical care in Veterans Affairs and non-Veterans Affairs settings. Medical Care, 76–88. [DOI] [PubMed] [Google Scholar]
- Ubanoski K, Inglis D, Veldhuizen S, 2017. Service use and unmet needs for substance use and mental disorders in Canada. Canadian Journal of Psychiatry, 62(8), 551–559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valenstein M, Kim HM, Ganoczy D, McCarthy JF, Zivin K, Austin KL, Hoggatt K, Eisenberg D, Piette JD, Blow FD, Olfson M, 2009. Higher-risk periods for suicide among VA patients receiving depression treatment: prioritizing suicide prevention efforts. Journal of Affective Disorders, 112(1), 50–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watkins KE, Hunter SB, Hepner KA, Paddock SM, de la Cruz E, Zhou AJ, Gilmore J, 2011. An effectiveness trial of group cognitive behavioral therapy for patients with persistent depressive symptoms in substance abuse treatment. Archives of General Psychiatry, 68(6), 577–584. [DOI] [PMC free article] [PubMed] [Google Scholar]