Abstract
Every 10 years, the Diabetic Pregnancy Study Group, a study group of the EASD, conducts an audit meeting to review the achievements of the preceding decade and to set the directions for research and clinical practice improvements for the next decade. The most recent meeting focused on the following areas: improving pregnancy outcomes for women with pregestational type 1 diabetes and type 2 diabetes; the influence of obesity and gestational diabetes on pregnancy outcomes; the determinants and assessment of fetal growth and development; and public health issues, including consideration of transgenerational consequences and economic burden. The audit meeting also considered the likely impact of ‘omics’ on research within the field and the potential of these technologies to enable precision-medicine approaches to management. Through sharing of the findings and ideas of audit meeting participants, the DPSG hopes to promote networking, research and advances in clinical care, to improve outcomes for all women and their offspring affected by diabetes and obesity in pregnancy.
Keywords: Fetus, Gestational diabetes mellitus, Obesity, Placenta, Pregnancy, Review, Type 1 diabetes, Type 2 diabetes
Introduction
The Diabetic Pregnancy Study Group (DPSG) (www.dpsghome.org) of the EASD aims to further research and promote education to improve the management of pregnant women with diabetes and their offspring. Every 10 years, DPSG conducts an audit meeting to review the achievements of the previous decade and to set the directions for research and clinical practice improvements for the next decade. This review is a summary report of the October 2016 audit meeting sessions held in Dublin, Ireland. The challenges surrounding diabetes in pregnancy, facing researchers and clinicians over the coming decade, are summarised in the Text box.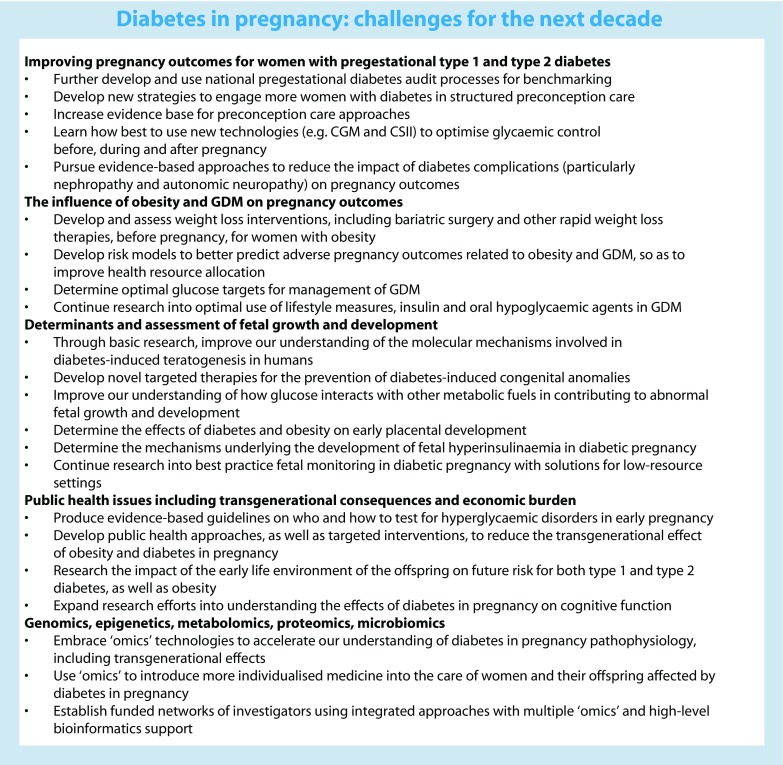
Improving pregnancy outcomes for women with pregestational type 1 and type 2 diabetes
Women with pregestational type 1 and type 2 diabetes mellitus continue to have poorer pregnancy outcomes than the background population, including a three- to fourfold higher rate of perinatal mortality [1, 2]. However, lower stillbirth rates have recently been reported in centres involved in the UK National Pregnancy in Diabetes (NPID) 2015 audit compared with those reported in the Confidential Enquiry into Maternal and Child Health audit from 2002–2003, suggesting that improvement is possible and highlighting the value of national audit programmes [3]. Importantly, social disadvantage was still strongly related to poorer diabetic pregnancy outcomes in the NPID audit [3]. The challenges ahead include increasing the percentage of women with diabetes who prepare for pregnancy, translating new glycaemic control technologies to the circumstances of pregnancy and reducing the impact of diabetes complications on maternal and fetal outcomes.
Preconception care
The available evidence strongly suggests that structured preconception care for women with pregestational diabetes reduces the risk of major congenital anomalies and perinatal mortality in women with type 1 and type 2 diabetes and is cost-effective [4, 5]. This care encompasses optimisation of glycaemic control, assessment and management of diabetes complications, cessation of potentially harmful drugs and commencement of folic acid, delivered by an experienced multidisciplinary team. Local and national campaigns have not achieved sufficient rates of pregnancy preparation in women with pregestational diabetes [6]. It remains unclear how best to improve these results. Healthcare teams need to promote awareness of preparation for a successful pregnancy to all adolescent girls and women of child-bearing age who have diabetes. Confidential and expert counselling on sexual and reproductive health, including advice on use of contraception and avoidance of unplanned pregnancies and unsafe sexual practices, is essential.
Due to the lack of high-level RCT evidence in this area [7], studies trialling different preconception care approaches in women with pregestational diabetes are being encouraged and a core outcome set has been developed for this purpose [8].
Optimising glycaemic control
The well-known harmful consequences of maternal hyperglycaemia must be balanced against the significant risk of hypoglycaemia, despite lack of data on the effects of maternal hypoglycaemia on neonatal outcomes [9]. The importance of optimal control in the first and second trimesters for prevention of pre-eclampsia, preterm birth and large for gestational age (LGA) neonates is becoming clearer [3, 10]. The American Diabetes Association and the UK National Institute for Health and Care Excellence targets for glycaemic control for women with type 1 diabetes during early pregnancy (HbA1c <48 mmol/mol [<6.5%]), individualised for safety, seem to be reasonable [11, 12]. Based on the recent NPID audit results, HbA1c levels of <42 mmol/mol (<6.0%) in later pregnancy should be safely achievable without serious hypoglycaemia in some women with type 1 diabetes and many women with type 2 diabetes [3].
Engagement of women in their own glycaemic control through diabetes education, with promotion of sensible lifestyle, frequent self-monitoring of blood glucose and a supported active approach to insulin adjustment is clearly important. While the use of insulin analogues (e.g. lispro, aspart, glargine and detemir) can be associated with reduced hypoglycaemia and glucose excursions, the safety and efficacy of newer insulin analogues and concentrated insulin preparations need to be clarified. Improved pregnancy outcomes from the use of continuous subcutaneous insulin infusion (CSII) have not yet been shown, such that its use should be on a case-by-case basis [13].
A recent RCT comparing continuous glucose monitoring (CGM) with capillary blood glucose monitoring only in women with type 1 diabetes (CONCEPTT) showed that CGM during pregnancy can increase the percentage of time that blood glucose is in the target range and reduce neonatal complications [14]. CGM compared with capillary blood glucose monitoring resulted in an approximately 50% reduction in LGA, neonatal intensive care admissions >24 h and neonatal hypoglycaemia [14].
Combining CGM and CSII systems, with or without closed-loop, may enable more effective insulin pump use in pregnancy, with studies in selected populations showing promise [15, 16].
Diabetes complications
Retinopathy, nephropathy and neuropathy frequently affect pregnancies of women with pregestational diabetes. Less common, but potentially life-threatening, is ischaemic heart disease. Guidelines recommend screening for diabetes complications before conception, during gestation and after delivery, as they can manifest or progress at these times [12, 13]. Diabetic nephropathy is associated with higher rates of congenital anomalies and pre-eclampsia [17, 18]. We would encourage study of pre-eclampsia prevention in diabetic women, with and without nephropathy, through the exploration of early biological and clinical markers and the use of low-dose aspirin [19]. The impact of lower blood pressure targets on pregnancy outcomes, including pre-eclampsia rates [17], and the effect of intravitreal dexamethasone implants on diabetic retinopathy during pregnancy [20] are topics that warrant further research. Improved management approaches to women with autonomic neuropathy causing gastroparesis and/or postural hypotension are required.
The influence of obesity and gestational diabetes mellitus on pregnancy outcomes
Obesity and gestational diabetes mellitus
Obesity in women of reproductive age is increasing worldwide and its negative impact on various pregnancy outcomes, including the risk of gestational diabetes mellitus (GDM), is now realised [21]. The 2009 Institute of Medicine guidelines on gestational weight gain (GWG) recommend that women with BMI ≥30 kg/m2 gain 5–9 kg during pregnancy. While there is evidence to support not exceeding these GWG recommendations, whether to recommend a GWG of <5 kg remains debatable due to an increased risk of small for gestational age (SGA) neonates [22, 23]. For women with BMI ≥35 kg/m2, however, a gestational weight change in the range of −4.9 to +4.9 kg has been reported to reduce the incidence of LGA births without an increase in SGA births [23].
As for bariatric surgery, retrospective studies show that it improves fertility, reduces the incidence of GDM, pre-eclampsia and LGA births, but increases rates of SGA births and possibly maternal venous thromboembolism and perinatal mortality [24–26]. Well-conducted prospective studies of bariatric surgery pre-pregnancy are required. In addition, research into the alternatives to bariatric surgery for rapid weight loss before and between pregnancies, such as very low energy diets, pharmacological therapy (e.g. liraglutide) and endoluminal devices is warranted.
Prevention of GDM
To date, interventions to prevent GDM in at-risk women have generally not been successful. Despite the known adverse effects of excessive GWG in obese women [27], multiple RCTs of lifestyle interventions during pregnancy have largely failed to prevent GDM, even though some reduction in GWG can be achieved [28, 29]. Whether such interventions need to commence earlier [30], have a greater effect on limiting GWG or work only in certain phenotypes or genotypes [31] is unknown. Despite hope from small studies, use of vitamin D, fish oil, metformin and inositol for GDM prevention have not been confirmed in larger RCTs [32–34]. We await results of larger probiotics studies, such as the Study of Probiotics in the Prevention of Gestational Diabetes (SPRING) trial [35]. Failure of strategies to prevent GDM could be a consequence of established dysfunction of glucose regulation, particularly of islet beta cells, well in advance of the affected pregnancy. Focus on GDM prevention is now turning to lifestyle interventions before and between pregnancies [36].
Predicting risk in GDM and treatment approaches including glucose targets
Due to the high prevalence of GDM, there is increasing interest in risk stratification to more effectively allocate limited healthcare resources. Risk engines are being developed (e.g. Brisbane risk model, unpublished, H. D. McIntyre, Mater Health Services and The University of Queensland, South Brisbane, QLD, Australia), recognising the fact that blood glucose needs to be considered in the context of other factors, such as maternal age and BMI. Another tool for risk stratification is fetal biometry, with tight vs less-tight glycaemic control being advocated for fetuses with greater or normal abdominal circumferences, respectively [37].
Ongoing controversies in GDM include whether early diagnosis is useful, glucose targets for management and the role for oral hypoglycaemic agents. Of note, glucose levels in healthy pregnant women are lower than recommended target levels in GDM guidelines [38], and both fasting and postprandial glucose levels in GDM adversely affect outcomes [39]. However, too-aggressive glucose lowering in certain women could result in an SGA birth, with the potential for detrimental long-term effects in the offspring. Of the oral glucose-lowering agents metformin shows most promise but its use in pregnancy is debatable due to its easy placental transfer [40].
Determinants and assessment of fetal growth and development
The most serious adverse outcomes of diabetic pregnancy continue to be congenital anomalies, stillbirth and excessive fetal growth. Our understanding of the causative mechanisms, however, remain limited. Improved accuracy of fetal growth assessment is essential to guide obstetric management.
Congenital anomalies
Poor glycaemic control at the time of conception and during the first trimester is clearly linked to higher rates of congenital anomalies. Multiple non-glycaemic factors (e.g. cytokines and other nutrients) interacting with glucose and the fetal genotype are also likely to influence teratogenesis. Within rodent models, oxidative, hexosamine and endoplasmic reticulum stresses, as well as disturbed autophagy and apoptosis processes, have all been implicated [41, 42]. Greater focus on determining human diabetes-induced teratogenic pathways is required; this might involve the use of human embryonic stem cells [43]. The long-term goal is development of novel targeted therapies to prevent diabetes-induced congenital anomalies.
Maternal, placental and fetal determinants of fetal growth
While maternal blood glucose control and adiposity clearly contribute to excess fetal adiposity, fetal factors, including fetal sex, genes and the presence or absence of hyperinsulinaemia, are also important determinants of fetal growth [44–47]. Once established, fetal hyperinsulinaemia can potentially contribute to an exaggerated fetal glucose steal [44]. This hypothesis might explain the occurrence of macrosomia in pregnancies with (near) normal maternal glucose values in late pregnancy [44].
There is still much to be discovered about how maternal lipids and their placental handling contribute to neonatal adipose tissue development. Complex regulatory mechanisms involving peroxisome proliferator-activated receptors are involved [48, 49]. Neonatal adiposity correlates with maternal BMI and plasma triacylglycerol, although it negatively correlates with cord serum triacylglycerol, suggesting increased fetal tissue lipid uptake [46, 47]. Indeed, hyperinsulinism increases lipoprotein lipase activity, a putative mechanism leading to the increased incorporation of lipids into fetal adipocytes [45]. Deficiency in polyunsaturated fatty acids occurs in parallel with increased lipoperoxidation in maternal diabetes [50].
Early pregnancy and diabetic fetopathy
Maternal first-trimester HbA1c is a good predictor of fetal macrosomia [51]. In addition, dietary glycaemic index and glycaemic load in early, but not late, pregnancy has been linked with offspring childhood adiposity [52]. There is also evidence indicating that fetal hyperinsulinaemia develops in early pregnancy [44]. Thus, the effects of diabetes on early placental and fetal islet development [53–55], key determinants of fetal growth and development, need further investigation. Lifestyle and diabetes management intervention RCTs focused on conception and the first-trimester time-points are warranted.
Assessment of fetal growth
Correct assessment of fetal growth prior to delivery is crucial for determining optimal management of delivery. A recent study suggests that fractional thigh volume is the best predictor of neonatal percentage body fat and birthweight z scores in suspected macrosomic fetuses [56]. MRI, while being more specific, is not more sensitive than two-dimensional ultrasound in detecting macrosomia [57] and its cost and availability are prohibitive. Assessments may be improved by the use of customised fetal growth charts, although they require further optimisation and need to be more inclusive of diverse populations [58]. Identification of novel biomarkers indicative of excessive fetal growth would be an advance. RCTs to determine optimal timing and frequency of ultrasound assessments in women with GDM are required, so that limited resources can be best allocated. Surveillance strategies also need to be developed for use in low-resource settings.
Public health issues including consideration of transgenerational consequences and economic burden
Increasing prevalence of obesity and diabetes is placing a major burden on maternity health services in developed and developing countries. Diabetes in pregnancy is associated with increased long-term cardiometabolic risk for both women and offspring. Optimal management of GDM, obesity and pregestational diabetes in pregnancy has the potential to lessen the transgenerational and population-level impact of metabolic disease.
Diagnosis of GDM
The WHO adopted the International Association of Diabetes in Pregnancy Study Groups (IADPSG) 2010 criteria for the diagnosis of GDM in 2013 [59, 60]. Many countries have adopted these diagnostic criteria, with some regional accommodations, but approaches to diagnosing GDM still vary widely. Performance of an OGTT during pregnancy after a screening glucose challenge test has not been validated against the IADPSG diagnostic approach. Diagnostic criteria for GDM have not been validated for early pregnancy, although early screening for ‘overt diabetes’ (IADPSG) or ‘diabetes in pregnancy’ (WHO) in at-risk women is recommended [61]. Further research to determine the value of testing for and treating early GDM (<24 weeks gestation), as well as optimal early diagnostic criteria, is required.
Public health issues and GDM
GDM is an independent and robust risk factor for the progression of women and their offspring to cardiometabolic diseases [62]. Early identification of women and offspring at highest risk after delivery and development of evidence-based prevention programmes are required. Lifestyle change and metformin treatment, initiated on average 12 years following a GDM pregnancy, and followed for 10 years post intervention, have been demonstrated to be highly effective in reducing progression to type 2 diabetes [63]. There is insufficient data to show whether treating maternal GDM has any effect on the long-term metabolic health of offspring. This may be due to suboptimal maternal therapy and/or insufficient follow-up time, or to stronger influence of the post-delivery family lifestyle. Post-pregnancy intervention programmes for the offspring need to be developed.
Type 1 diabetes and transgenerational issues
Type 1 diabetes occurs in genetically susceptible individuals and evidence of islet cell autoimmunity appears long before diagnosis [64]. Having a mother with type 1 diabetes is associated with a lower risk of future diabetes compared with the genetic/shared-environmental risk of having a father or sibling with type 1 diabetes [65]. The implications that the diabetic intrauterine endocrine–metabolic–immunological milieu might have on the conditioning of the developing endocrine pancreas is intriguing and is yet to be explored.
Diabetes in pregnancy and cognitive disorders
Diabetes in pregnancy may have an impact on cognitive function and may increase the risk of autism spectrum disorders or attention deficit hyperactivity disorder in offspring [66]. However, lower cognitive test scores in offspring of women with GDM may be explained by co-existing risk factors rather than by maternal hyperglycaemia [66]. Of note, delayed cortical evoked responses in the neonatal period and at age 3 years were found in infants of mothers with type 1 diabetes [67]. More studies into the impact of maternal diabetes on neurocognitive development of offspring are required.
Genomics, epigenetics, metabolomics, proteomics and microbiomics
The rapid emergence of the powerful ‘omics’ technologies, supported by bioinformatics, provides new insights into disease mechanisms, more accurate diagnosis and new precision therapies. The value of genomics for accurate diagnosis of neonatal diabetes and maturity-onset diabetes of the young is established [68]. New paradigms are evolving for precision-medicine approaches to type 2 diabetes, which will also be highly relevant to GDM and type 2 diabetes in pregnancy [68]. However, to date, genetic risk scores, derived from known diabetes-associated gene polymorphisms, have not meaningfully contributed to GDM prediction. Epigenetic changes have been proposed to be involved in the effects of in utero exposure to maternal hyperglycaemia on long-term metabolic health issues of the offspring [69]. An example of success using whole-transcriptome analysis comes from a study that showed marked upregulation of tryptophan hydroxylase-1 in islets of pregnant mice [70]. Serotonin is now an established mediator of the islet beta cell adaptive response to lactogenic hormones in pregnancy [70]. Proteomics is also being used to better understand islet beta cell responses to pregnancy [71]. Metabolomics profiles of fasting plasma in women with GDM at 6 weeks post-partum identified 21 amino acids and fatty acids that were able to distinguish those who would progress to type 2 diabetes [72]. While the maternal and offspring microbiome differ between GDM and normoglycaemic pregnancies, reproducible intervention trials with probiotics are still needed to translate these findings to clinical practice. Limitations need to be considered in ‘omics’ study design, as large cohorts are usually required for adequate power and ‘causation’ (as opposed to ‘association’) is often difficult to prove. Networking of investigators using integrated approaches with multiple ‘omics’ technologies and high-level bioinformatics support is recommended for future studies within our field.
Conclusion
The work of the last decade has best defined the challenges ahead for research and clinical care in diabetes in pregnancy. Research and clinical focus on the preconception period and first trimester is essential to improve pregnancy outcomes for women with pregestational diabetes. New technologies for improving glycaemic control (CGM and CSII) in diabetic pregnancy show promise but it is still unclear how best to use them. The need to consider GDM within the context of other maternal characteristics, such as maternal ethnicity and BMI, has been realised. A reappraisal of whether GDM is a condition of late pregnancy only is required. The long-term maternal and offspring effects of any interventions for use in pregnancy are difficult to study, but need to be explored. Last, scientific endeavour within this field is central to achieving better outcomes for women with diabetes in pregnancy. This requires the development of networked programmes enabling the most effective use of powerful new research technologies and high-quality clinical trials for the translation of new discoveries into best practice.
Acknowledgements
The authors wish to acknowledge the chair of the local organising committee (F. P. Dunne, School of Medicine, National University of Ireland, Ireland), the input of the external auditors (L. A. Barbour, Division of Endocrinology, Metabolism, and Diabetes, University of Colorado, USA; I. Cetin, Department of Obstetrics and Gynaecology, University of Milan, Italy; D. B. Dunger, Department of Paediatrics, University of Cambridge, UK and D. Schlembach, Department of Obstetrics and Gynecology, University of Jena, Germany) and the contributions of all attendees of the 2016 DPSG audit meeting to this work (listed in the Appendix). We would also like to thank G. Desoye (Department of Obstetrics and Gynecology, Medical University of Graz, Austria), M. del Pilar Ramos Álvarez (Facultad de Farmacia, Universidad San Pablo-CEU, Spain) and D. Moller Jensen (Department of Endocrinology, Odense University Hospital, Denmark) for their guidance in preparing this manuscript.
Contribution statement
All attendees of the 2016 audit meeting (listed in the Appendix) contributed to the preparation of this article. US-G., AN and CJN drafted the initial version of the article. All attendees critically revised it for accurate content and gave approval to the final submitted version.
Abbreviations
- CGM
Continuous glucose monitoring
- CSII
Continuous subcutaneous insulin infusion
- DPSG
Diabetic Pregnancy Study Group
- GDM
Gestational diabetes mellitus
- GWG
Gestational weight gain
- IADPSG
International Association of Diabetes in Pregnancy Study Groups
- LGA
Large for gestational age
- NPID
National Pregnancy in Diabetes
- SGA
Small for gestational age
Appendix
Attendees at DPSG audit meeting, Dublin, 2016
Writing group: Ute Schaefer-Graf1, Angela Napoli2 and Christopher J. Nolan3.
Contributing attendees: Eleni Anastasiou4, Katrien Benhalima5, Patrick Catalano6, Ana Chico7, Cheril Clarson8, Rosa Corcoy7, Donald R. Coustan9, Maria G. Dalfra10, Tine D. Clausen11, Peter Damm12, Philippe Deruelle13, Harold de Valk14, Gernot Desoye15, Roland Devlieger16, Josip Djelmis17, Anne Dornhorst18, Nicoletta Dozio19, Fidelma P Dunne20, Aoife M. Egan20, Ulf J. Eriksson21, Helena Fadl22, Denice S. Feig23, Sander Galjaard24, Emilio Herrera25, David Hill8, Alicia Jawerbaum26, Dorte M. Jensen27, Alexandra Kautzky-Willer28, Louise Kelstrup12, Annunziata Lapolla10, Jeannet Lauenborg29, Jacques Lepercq30, Robert S Lindsay31, Mary R. Loeken32, William L. Lowe33, Michael J. Maresh34, Elisabeth R. Mathiesen12, David R. McCance35, H. David McIntyre36, Giorgio Mello37, Sara J. Meltzer38, Boyd E. Metzger39, Helen R. Murphy40, Jenny E. Myers41, Yasue Omori42, Per Ovesen43, Martina Persson44, Maria del Pilar Ramos-Alvarez25, Kristina M. Renault12, Lene Ringholm45, Janet A. Rowan46, Luisa Ruas47, David A. Sacks48, Charles Savona-Ventura49, Eleanor Scott50, David Simmons51, Takashi Sugiyama52, Adam Tabak53, Mette Tanvig54, Rosemary C. Temple55, Anne Vambergue56, Mireille N.M. van Poppel57, Marta Viana25, Christina Vinter54, Ewa Wender-Ozegowska58, Parri Wentzel21, Agnieszka Zawiejska58 and Christos Zoupas59.
1Berlin Center for Diabetes in Pregnancy, Department of Obstetrics and Gynecology, St Joseph’s Hospital, Berlin, Germany
2Department of Clinical and Molecular Medicine, Sant’Andrea Hospital Faculty of Medicine and Psychology, Sapienza University, Rome, Italy
3Department of Endocrinology at The Canberra Hospital and the Australian National University Medical School, Canberra, ACT, Australia
4Diabetes Center, Alexandra General Hospital, Athens, Greece
5Department of Endocrinology, UZ Gasthuisberg, KU Leuven, Leuven, Belgium
6Centre for Reproductive Health, Department of Obstetrics and Gynecology, MetroHealth Medical Center, Cleveland, OH, USA
7Department of Endocrinology and Nutrition, Hospital de la Santa Creu I Sant Pau, Barcelona; CIBER-BBN, Zaragoza, Spain
8Lawson Health Research Institute, London, ON, Canada
9Division of Maternal-Fetal Medicine, Women & Infants Hospital of Rhode Island and Warren Alpert Medical School of Brown University, Providence, RI, USA
10Department of Medical and Surgical Sciences, University of Padua, Padova, Italy
11Department of Obstetrics and Gynaecology, Hilleroed Hospital, Hilleroed, Denmark
12Center for Pregnant Women with Diabetes, Department of Obstetrics, Copenhagen, Denmark
13Department of Obstetrics and Gynaecology, CHU Lille, Lille, France
14Department of Internal Medicine, University Medical Center Utrecht, Utrecht, the Netherlands
15Department of Obstetrics and Gynecology, Medical University of Graz, Graz, Austria
16Department of Obstetrics and Gynaecology, KULeuven, University of Leuven, Leuven, Belgium
17Department of Obstetrics and Gynecology, School of Medicine, Zagreb, Croatia
18Department of Endocrinology, Hammersmith Hospital, London, UK
19Department of Diabetes, Diabetes Research Institute, Ospedale San Raffaele and San Raffaele, Vita-Salute University, Milan, Italy
20School of Medicine, National University of Ireland, Galway, Ireland
21Department of Medical Cell Biology, Biomedical Center, Uppsala University, Uppsala, Sweden
22Department of Obstetrics and Gynecology, School of Health and Medical Sciences, Orebro University, Orebro, Sweden
23Department of Medicine, University of Toronto, Toronto, ON, Canada
24Department of Obstetrics and Gynaecology, Erasmus Medical Center (EMC) Rotterdam, Rotterdam, the Netherlands
25Facultad de Farmacia, Universidad, San Pablo-CEU, Madrid, Spain
26Laboratory of Reproduction and Metabolism, CEFYBO-CONICET, School of Medicine, University of Buenos Aires, Buenos Aires, Argentina
27Department of Endocrinology, Odense University Hospital, Faculty of Health Science, University of Southern Denmark, Odense, Denmark
28Internal Medicine III, Endocrinology & Metabolism, Gender Medicine Unit, Medical University of Vienna, Vienna, Austria
29Department of Obstetrics and Gynecology, Copenhagen University Hospital, Herlev, Denmark
30Maternite Port-Royal, Paris, France
31Institute of Cardiovascular and Medical Sciences, British Heart Foundation Glasgow Cardiovascular Research Centre, University of Glasgow, University of Glasgow, Scotland, UK
32Section on Islet Cell and Regenerative Biology, Joslin Diabetes Center, Harvard Medical Center, Boston, MA, USA
33Northwestern University Feinburg School of Medicine, Northwestern University, Chicago, IL, USA
34Manchester University Hospitals, Manchester, UK
35Metabolic Unit, Royal Victoria Hospital, Belfast, N. Ireland, UK
36Department of Endocrinology and Obstetric Medicine, Mater Health Services and The University of Queensland, South Brisbane, QLD, Australia
37Perinatology and Human Reproduction, University of Florence, Florence, Italy
38McGill University Health Centre, McGill University, Montreal, QC, Canada
39Center of Endocrinology, Northwestern University, Chicago, IL, USA
40Department of Medicine, University of East Anglia, Norwich, UK
41Maternal & Fetal Health Research Centre, St Mary’s Hospital for Women and Children, Manchester, UK
42Diabetes Center, Ebina General Hospital, Kanagawa, Japan
43Department of Obstetrics and Gynaecology, Aarhus University Hospital, Aarhus, Denmark
44Department of Medicine, Clinical Epidemiology, Karolinska University Hospital, Solna, Sweden
45Steno Diabetes Center Copenhagen, Gentofte, Denmark
46National Women’s Hospital, Auckland City Hospital, Auckland, New Zealand
47Endocrinology, Diabetes and Metabolism, Hospitais da Universidade de Coimbra, Coimbra, Portugal
48Division of Maternal-Fetal Medicine, Department of Obstetrics and Gynecology, University of Southern California, Keck School of Medicine, Los Angeles, CA, USA
49Department of Obstetrics and Gynaecology, University of Malta Medical School, Mater Dei Hospital, Malta
50Leeds Institute of Cardiovascular and Metabolic Medicine, University of Leeds, Leeds, UK
51School of Medicine, University of Western Sydney, Campbelltown, NSW, Australia
52Department of Obstetrics and Gynecology, Ehime University Graduate School of Medicine, Ehime, Japan
53Diabetes Unit, Faculty of Medicine, Semmelweis University, Budapest, Hungary
54Department of Gynecology and Obstetrics, Odense University Hospital, Faculty of Health Science, University of Southern Denmark, Odense, Denmark
55Department of Diabetes and Endocrinology, Norfolk and Norwich University Hospital NHS Trust, Norwich, UK
56Department of Endocrinology and Diabetology, University of Lille, Lille, France
57Institute of Sport Science, University of Graz, Graz, Austria
58Division of Reproduction, Department of Obstetrics, Gynecology and Gynecological Oncology, Poznan University of Medical Sciences, Poznan, Poland
59Athens Diabetes Center, Hygeia General Hospital, Athens, Greece
Funding
Funding was not available for the writing of this manuscript.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Footnotes
The Diabetic Pregnancy Study Group 2016 audit meeting attendees (including the writing group) are listed in the Appendix.
References
- 1.Colstrup M, Mathiesen ER, Damm P, Jensen DM, Ringholm L. Pregnancy in women with type 1 diabetes: have the goals of St. Vincent declaration been met concerning foetal and neonatal complications? J Matern Fetal Neonatal Med. 2013;26:1682–1686. doi: 10.3109/14767058.2013.794214. [DOI] [PubMed] [Google Scholar]
- 2.Macintosh MC, Fleming KM, Bailey JA, et al. Perinatal mortality and congenital anomalies in babies of women with type 1 or type 2 diabetes in England, Wales, and Northern Ireland: population based study. BMJ. 2006;333:177. doi: 10.1136/bmj.38856.692986.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murphy HR, Bell R, Cartwright C, et al. Improved pregnancy outcomes in women with type 1 and type 2 diabetes but substantial clinic-to-clinic variations: a prospective nationwide study. Diabetologia. 2017;60:1668–1677. doi: 10.1007/s00125-017-4314-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wahabi HA, Alzeidan RA, Esmaeil SA. Pre-pregnancy care for women with pre-gestational diabetes mellitus: a systematic review and meta-analysis. BMC Public Health. 2012;12:792. doi: 10.1186/1471-2458-12-792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheffler RM, Feuchtbaum LB, Phibbs CS. Prevention: the cost-effectiveness of the California Diabetes and Pregnancy Program. Am J Public Health. 1992;82:168–175. doi: 10.2105/AJPH.82.2.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.NHS Digital (2016) National Diabetes in Pregnancy Audit. Available from http://content.digital.nhs.uk/npid. Accessed 16 Oct 2017
- 7.Tieu J, Middleton P, Crowther CA, Shepherd E (2017) Preconception care for diabetic women for improving maternal and infant health. Cochrane Database Syst Rev, Issue 8, Art. no.: CD007776 [DOI] [PMC free article] [PubMed]
- 8.Egan AM, Galjaard S, Maresh MJA, et al. A core outcome set for studies evaluating the effectiveness of prepregnancy care for women with pregestational diabetes. Diabetologia. 2017;60:1190–1196. doi: 10.1007/s00125-017-4277-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maresh MJ, Holmes VA, Patterson CC, et al. Glycemic targets in the second and third trimester of pregnancy for women with type 1 diabetes. Diabetes Care. 2015;38:34–42. doi: 10.2337/dc14-1755. [DOI] [PubMed] [Google Scholar]
- 10.Secher AL, Ringholm L, Andersen HU, Damm P, Mathiesen ER. The effect of real-time continuous glucose monitoring in pregnant women with diabetes: a randomized controlled trial. Diabetes Care. 2013;36:1877–1883. doi: 10.2337/dc12-2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Diabetes Association Management of diabetes in pregnancy. Diabetes Care. 2017;40:S114–S119. doi: 10.2337/dc17-S016. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence (NICE) (2015). Diabetes in pregnancy: management from preconception to the postnatal period. Available from nice.org.uk/guidance/ng3. Accessed 16 Oct 2017 [PubMed]
- 13.Farrar D, Tuffnell DJ, West J, West HM (2016) Continuous subcutaneous insulin infusion versus multiple daily injections of insulin for pregnant women with diabetes. Cochrane Database Syst Rev, Issue 6, Art. no.: CD005542 [DOI] [PMC free article] [PubMed]
- 14.Feig DS, Donovan LE, Corcoy R, et al. Continuous glucose monitoring in pregnant women with type 1 diabetes (CONCEPTT): a multicentre international randomised controlled trial. Lancet. 2017;390:2347–2359. doi: 10.1016/S0140-6736(17)32400-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stewart ZA, Wilinska ME, Hartnell S, et al. Closed-loop insulin delivery during pregnancy in women with type 1 diabetes. N Engl J Med. 2016;375:644–654. doi: 10.1056/NEJMoa1602494. [DOI] [PubMed] [Google Scholar]
- 16.Fresa R, Visalli N, Di Blasi V, et al. Experiences of continuous subcutaneous insulin infusion in pregnant women with type 1 diabetes during delivery from four Italian centers: a retrospective observational study. Diabetes Technol Ther. 2013;15:328–334. doi: 10.1089/dia.2012.0260. [DOI] [PubMed] [Google Scholar]
- 17.Ringholm L, Mathiesen ER, Kelstrup L, Damm P. Managing type 1 diabetes mellitus in pregnancy—from planning to breastfeeding. Nat Rev Endocrinol. 2012;8:659–667. doi: 10.1038/nrendo.2012.154. [DOI] [PubMed] [Google Scholar]
- 18.Bell R, Glinianaia SV, Tennant PW, Bilous RW, Rankin J. Peri-conception hyperglycaemia and nephropathy are associated with risk of congenital anomaly in women with pre-existing diabetes: a population-based cohort study. Diabetologia. 2012;55:936–947. doi: 10.1007/s00125-012-2455-y. [DOI] [PubMed] [Google Scholar]
- 19.Zeisler H, Llurba E, Chantraine F, et al. Predictive value of the sFlt-1:PlGF ratio in women with suspected preeclampsia. N Engl J Med. 2016;374:13–22. doi: 10.1056/NEJMoa1414838. [DOI] [PubMed] [Google Scholar]
- 20.Concillado M, Lund-Andersen H, Mathiesen ER, Larsen M. Dexamethasone intravitreal implant for diabetic macular edema during pregnancy. Am J Ophthalmol. 2016;165:7–15. doi: 10.1016/j.ajo.2016.02.004. [DOI] [PubMed] [Google Scholar]
- 21.Poston L, Caleyachetty R, Cnattingius S, et al. Preconceptional and maternal obesity: epidemiology and health consequences. Lancet Diabetes Endocrinol. 2016;4:1025–1036. doi: 10.1016/S2213-8587(16)30217-0. [DOI] [PubMed] [Google Scholar]
- 22.Catalano PM, Mele L, Landon MB, et al. Inadequate weight gain in overweight and obese pregnant women: what is the effect on fetal growth? Am J Obstet Gynecol. 2014;211:137 e131-137. doi: 10.1016/j.ajog.2014.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hinkle SN, Sharma AJ, Dietz PM. Gestational weight gain in obese mothers and associations with fetal growth. Am J Clin Nutr. 2010;92:644–651. doi: 10.3945/ajcn.2010.29726. [DOI] [PubMed] [Google Scholar]
- 24.Abenhaim HA, Alrowaily N, Czuzoj-Shulman N, Spence AR, Klam SL. Pregnancy outcomes in women with bariatric surgery as compared with morbidly obese women. J Matern Fetal Neonatal Med. 2016;29:3596–3601. doi: 10.3109/14767058.2016.1143927. [DOI] [PubMed] [Google Scholar]
- 25.Johansson K, Cnattingius S, Naslund I, et al. Outcomes of pregnancy after bariatric surgery. N Engl J Med. 2015;372:814–824. doi: 10.1056/NEJMoa1405789. [DOI] [PubMed] [Google Scholar]
- 26.Dalfrà MG, Busetto L, Chilelli NC, Lapolla A. Pregnancy and foetal outcome after bariatric surgery: a review of recent studies. J Matern Fetal Neonatal Med. 2012;25:1537–1543. doi: 10.3109/14767058.2012.663829. [DOI] [PubMed] [Google Scholar]
- 27.Egan AM, Dennedy MC, Al-Ramli W, Heerey A, Avalos G, Dunne F. ATLANTIC-DIP: excessive gestational weight gain and pregnancy outcomes in women with gestational or pregestational diabetes mellitus. J Clin Endocrinol Metab. 2014;99:212–219. doi: 10.1210/jc.2013-2684. [DOI] [PubMed] [Google Scholar]
- 28.Simmons D, Devlieger R, van Assche A, et al. Effect of physical activity and/or healthy eating on GDM risk: the DALI lifestyle study. J Clin Endocrinol Metab. 2017;102:903–913. doi: 10.1210/jc.2016-3455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Oostdam N, van Poppel MN, Wouters MG, van Mechelen W. Interventions for preventing gestational diabetes mellitus: a systematic review and meta-analysis. J Women’s Health. 2011;20:1551–1563. doi: 10.1089/jwh.2010.2703. [DOI] [PubMed] [Google Scholar]
- 30.Song C, Li J, Leng J, Ma RC, Yang X. Lifestyle intervention can reduce the risk of gestational diabetes: a meta-analysis of randomized controlled trials. Obes Rev. 2016;17:960–969. doi: 10.1111/obr.12442. [DOI] [PubMed] [Google Scholar]
- 31.Grotenfelt NE, Wasenius NS, Rono K, et al. Interaction between rs10830963 polymorphism in MTNR1B and lifestyle intervention on occurrence of gestational diabetes. Diabetologia. 2016;59:1655–1658. doi: 10.1007/s00125-016-3989-1. [DOI] [PubMed] [Google Scholar]
- 32.Syngelaki A, Nicolaides KH, Balani J, et al. Metformin versus placebo in obese pregnant women without diabetes mellitus. N Engl J Med. 2016;374:434–443. doi: 10.1056/NEJMoa1509819. [DOI] [PubMed] [Google Scholar]
- 33.Farren M, Daly N, McKeating A, Kinsley B, Turner MJ, Daly S. The prevention of gestational diabetes mellitus with antenatal oral inositol supplementation: a randomized controlled trial. Diabetes Care. 2017;40:759–763. doi: 10.2337/dc16-2449. [DOI] [PubMed] [Google Scholar]
- 34.Agha-Jaffar R, Oliver N, Johnston D, Robinson S. Gestational diabetes mellitus: does an effective prevention strategy exist? Nat Rev Endocrinol. 2016;12:533–546. doi: 10.1038/nrendo.2016.88. [DOI] [PubMed] [Google Scholar]
- 35.Nitert MD, Barrett HL, Foxcroft K, et al. SPRING: an RCT study of probiotics in the prevention of gestational diabetes mellitus in overweight and obese women. BMC Pregnancy Childbirth. 2013;13:50. doi: 10.1186/1471-2393-13-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma RC, Schmidt MI, Tam WH, McIntyre HD, Catalano PM. Clinical management of pregnancy in the obese mother: before conception, during pregnancy, and post partum. Lancet Diabetes Endocrinol. 2016;4:1037–1049. doi: 10.1016/S2213-8587(16)30278-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kjos SL, Schaefer-Graf UM. Modified therapy for gestational diabetes using high-risk and low-risk fetal abdominal circumference growth to select strict versus relaxed maternal glycemic targets. Diabetes Care. 2007;30(Suppl 2):S200–S205. doi: 10.2337/dc07-s216. [DOI] [PubMed] [Google Scholar]
- 38.Hernandez TL, Friedman JE, Van Pelt RE, Barbour LA. Patterns of glycemia in normal pregnancy: should the current therapeutic targets be challenged? Diabetes Care. 2011;34:1660–1668. doi: 10.2337/dc11-0241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rowan JA, Gao W, Hague WM, McIntyre HD. Glycemia and its relationship to outcomes in the metformin in gestational diabetes trial. Diabetes Care. 2010;33:9–16. doi: 10.2337/dc09-1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lindsay RS, Loeken MR. Metformin use in pregnancy: promises and uncertainties. Diabetologia. 2017;60:1612–1619. doi: 10.1007/s00125-017-4351-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Eriksson UJ. Congenital anomalies in diabetic pregnancy. Semin Fetal Neonatal Med. 2009;14:85–93. doi: 10.1016/j.siny.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 42.Zabihi S, Loeken MR. Understanding diabetic teratogenesis: where are we now and where are we going? Birth Defects Res A Clin Mol Teratol. 2010;88:779–790. doi: 10.1002/bdra.20704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kang HY, Hong EJ, Kang HS, Ahn C, Jeung EB. Assessment of neurotoxicity of pharmacological compounds during early neural development of human embryonic stem cells. J Physiol Pharmacol. 2017;68:231–241. [PubMed] [Google Scholar]
- 44.Desoye G, Nolan CJ. The fetal glucose steal: an underappreciated phenomenon in diabetic pregnancy. Diabetologia. 2016;59:1089–1094. doi: 10.1007/s00125-016-3931-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herrera E, Desoye G. Maternal and fetal lipid metabolism under normal and gestational diabetic conditions. Horm Mol Biol Clin Invest. 2016;26:109–127. doi: 10.1515/hmbci-2015-0025. [DOI] [PubMed] [Google Scholar]
- 46.Schaefer-Graf UM, Meitzner K, Ortega-Senovilla H, et al. Differences in the implications of maternal lipids on fetal metabolism and growth between gestational diabetes mellitus and control pregnancies. Diabet Med. 2011;28:1053–1059. doi: 10.1111/j.1464-5491.2011.03346.x. [DOI] [PubMed] [Google Scholar]
- 47.O’Tierney-Ginn P, Presley L, Minium J, Hauguel deMouzon S, Catalano PM. Sex-specific effects of maternal anthropometrics on body composition at birth. Am J Obstet Gynecol. 2014;211(292):e291–e299. doi: 10.1016/j.ajog.2014.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Poulos SP, Dodson MV, Culver MF, Hausman GJ. The increasingly complex regulation of adipocyte differentiation. Exp Biol Med. 2016;241:449–456. doi: 10.1177/1535370215619041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Jawerbaum A, Capobianco E. Review: effects of PPAR activation in the placenta and the fetus: implications in maternal diabetes. Placenta. 2011;32(Suppl 2):S212–S217. doi: 10.1016/j.placenta.2010.12.002. [DOI] [PubMed] [Google Scholar]
- 50.Lappas M, Hiden U, Desoye G, Froehlich J, Mouzon SH, Jawerbaum A. The role of oxidative stress in the pathophysiology of gestational diabetes mellitus. Antioxid Redox Signal. 2011;15:3061–3100. doi: 10.1089/ars.2010.3765. [DOI] [PubMed] [Google Scholar]
- 51.Hughes RC, Moore MP, Gullam JE, Mohamed K, Rowan J. An early pregnancy HbA1c ≥ 5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care. 2014;37:2953–2959. doi: 10.2337/dc14-1312. [DOI] [PubMed] [Google Scholar]
- 52.Okubo H, Crozier SR, Harvey NC, et al. Maternal dietary glycemic index and glycemic load in early pregnancy are associated with offspring adiposity in childhood: the Southampton Women’s Survey. Am J Clin Nutr. 2014;100:676–683. doi: 10.3945/ajcn.114.084905. [DOI] [PubMed] [Google Scholar]
- 53.Frohlich JD, Huppertz B, Abuja PM, Konig J, Desoye G. Oxygen modulates the response of first-trimester trophoblasts to hyperglycemia. Am J Pathol. 2012;180:153–164. doi: 10.1016/j.ajpath.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 54.Effendi M, Demers S, Giguere Y, et al. Association between first-trimester placental volume and birth weight. Placenta. 2014;35:99–102. doi: 10.1016/j.placenta.2013.11.015. [DOI] [PubMed] [Google Scholar]
- 55.Bonner-Weir S, Aguayo-Mazzucato C, Weir GC. Dynamic development of the pancreas from birth to adulthood. Ups J Med Sci. 2016;121:155–158. doi: 10.3109/03009734.2016.1154906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gibson KS, Stetzer B, Catalano PM, Myers SA. Comparison of 2- and 3-dimensional sonography for estimation of birth weight and neonatal adiposity in the setting of suspected fetal macrosomia. J Ultrasound Med. 2016;35:1123–1129. doi: 10.7863/ultra.15.06106. [DOI] [PubMed] [Google Scholar]
- 57.Malin GL, Bugg GJ, Takwoingi Y, Thornton JG, Jones NW. Antenatal magnetic resonance imaging versus ultrasound for predicting neonatal macrosomia: a systematic review and meta-analysis. BJOG. 2016;123:77–88. doi: 10.1111/1471-0528.13517. [DOI] [PubMed] [Google Scholar]
- 58.Gonzalez Gonzalez NL, Plasencia W, Gonzalez Davila E, et al. The effect of customized growth charts on the identification of large for gestational age newborns. Eur J Obstet Gynecol Reprod Biol. 2013;26:62–65. doi: 10.3109/14767058.2012.726298. [DOI] [PubMed] [Google Scholar]
- 59.Agarwal MM, Boulvain M, Coetzee E, et al. Diagnostic criteria and classification of hyperglycaemia first detected in pregnancy: a World Health Organization Guideline. Diabetes Res Clin Pract. 2014;103:341–363. doi: 10.1016/j.diabres.2013.10.012. [DOI] [PubMed] [Google Scholar]
- 60.International Association of Diabetes in Pregnancy Groups Consensus Panel International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33:676–682. doi: 10.2337/dc09-1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McIntyre HD, Sacks DA, Barbour LA, et al. Issues with the diagnosis and classification of hyperglycemia in early pregnancy. Diabetes Care. 2016;39:53–54. doi: 10.2337/dc15-1887. [DOI] [PubMed] [Google Scholar]
- 62.Damm P, Houshmand-Oeregaard A, Kelstrup L, Lauenborg J, Mathiesen ER, Clausen TD. Gestational diabetes mellitus and long-term consequences for mother and offspring: a view from Denmark. Diabetologia. 2016;59:1396–1399. doi: 10.1007/s00125-016-3985-5. [DOI] [PubMed] [Google Scholar]
- 63.Aroda VR, Christophi CA, Edelstein SL, et al. The effect of lifestyle intervention and metformin on preventing or delaying diabetes among women with and without gestational diabetes: the Diabetes Prevention Program outcomes study 10-year follow-up. J Clin Endocrinol Metab. 2015;100:1646–1653. doi: 10.1210/jc.2014-3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Insel RA, Dunne JL, Atkinson MA, et al. Staging presymptomatic type 1 diabetes: a scientific statement of JDRF, the Endocrine Society, and the American Diabetes Association. Diabetes Care. 2015;38:1964–1974. doi: 10.2337/dc15-1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Harjutsalo V, Reunanen A, Tuomilehto J. Differential transmission of type 1 diabetes from diabetic fathers and mothers to their offspring. Diabetes. 2006;55:1517–1524. doi: 10.2337/db05-1296. [DOI] [PubMed] [Google Scholar]
- 66.Camprubi Robles M, Campoy C, Garcia Fernandez L, Lopez-Pedrosa JM, Rueda R, Martin MJ. Maternal diabetes and cognitive performance in the offspring: a systematic review and meta-analysis. PLoS One. 2015;10:e0142583. doi: 10.1371/journal.pone.0142583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Brinciotti M, Matricardi M, Colatrella A, Torcia F, Fallucca F, Napoli A. Visual evoked potentials in infants of diabetic mothers: relations to clinical and metabolic status during pregnancy and delivery. Clin Neurophysiol. 2009;120:563–568. doi: 10.1016/j.clinph.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 68.Hattersley AT, Patel KA. Precision diabetes: learning from monogenic diabetes. Diabetologia. 2017;60:769–777. doi: 10.1007/s00125-017-4226-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Houshmand-Oeregaard A, Hansen NS, Hjort L, et al. Differential adipokine DNA methylation and gene expression in subcutaneous adipose tissue from adult offspring of women with diabetes in pregnancy. Clin Epigenetics. 2017;9:37. doi: 10.1186/s13148-017-0338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kim H, Toyofuku Y, Lynn FC, et al. Serotonin regulates pancreatic beta cell mass during pregnancy. Nat Med. 2010;16:804–808. doi: 10.1038/nm.2173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Horn S, Kirkegaard JS, Hoelper S, et al. Research resource: a dual proteomic approach identifies regulated islet proteins during β-cell mass expansion in vivo. Mol Endocrinol. 2016;30:133–143. doi: 10.1210/me.2015-1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Allalou A, Nalla A, Prentice KJ, et al. A predictive metabolic signature for the transition from gestational diabetes mellitus to type 2 diabetes. Diabetes. 2016;65:2529–2539. doi: 10.2337/db15-1720. [DOI] [PMC free article] [PubMed] [Google Scholar]


