Abstract
Background
Deficits in dynamic neuromuscular control of the knee may contribute to the higher incidence of the anterior cruciate ligament (ACL), specifically in female athletes. Little is known about the effects of preventive training programs on muscle onset time and activation during functional tasks.
Purpose
The purpose of this study was to evaluate the efficacy of perturbation-enhanced neuromuscular training on hamstring and quadriceps onset time and activation, and knee flexion angle in female athletes with quadriceps dominance (QD) deficit during a tuck-jump (TJ) task.
Study Design
Quasi-experimental study
Methods
Thirty-one collegiate female athletes with neuromuscular quadriceps dominance deficit randomly divided into experimental (n=16) and control (n=15) group. The experimental group performed a six-week perturbation training (18 sessions). Electromyograhic (EMG) assessment of quadriceps and hamstring activation and knee flexion angles during a TJ task were completed at baseline and after six weeks.
Results
A significant decrease in the preparatory(p=0.003) and reactive (p=0.013) quadriceps-hamstring (Q/H) co-activation ratio was found in the experimental group. Perturbation training markedly decreased latency in medial hamstring (MH) (p=0.001), vastus medialis (VM) (p=0.004) and lateral hamstring (LH) (p=0.031), while latency increased for rectus femoris (RF) (p=0.001) and vastus lateralis (VL) (p=0.023) during a TJ task. The experimental group had average increases of 41.1%, 40.8%, and 39.5% in initial knee flexion, peak knee flexion and knee flexion displacement angle during the TJ task, respectively.
Conclusion
Increased preparatory VM and MH activities and decreased Q/H co-activation ratio, decreased VM and MH latency represent preprogrammed motor strategies learned during the perturbation training. This observed neuromuscular adaptation during TJ task could potentially reduce the risk for non-contact ACL injury.
Level of evidence
2
Keywords: Anterior cruciate ligament, Electromyography, Female, Knee flexion angle, Movement System, Muscle activation
INTRODUCTION
Knee joint injuries are one of the most common injuries related to athletic activities, accounting for almost 10% to 25% of all injuries,1 and anterior cruciate ligament (ACL) comprises approximately 45% of them.2 ACL injury is associated with long recovery times and high socio-economic costs.2 Approximately 70% of ACL injury mechanisms are non-contact,2 and commonly occur during physical activities that require deceleration and acceleration, change of direction, landing, and pivoting maneuvers.2 Female athletes are two to eight times more likely than male athletes to sustain ACL injury.3 The reason for this difference could be due to the 2.7 ° to 5.8 ° greater quadriceps angle (Q angle), narrower A-shaped intercondylar notch, smaller ACL size, and increased medial posterior tibial slope.3
Analyses of videos recorded during non-contact anterior cruciate ligament (ACL) injury have repeatedly shown that awkward movements (i.e., decreased knee, hip, and trunk flexion which imply decreased sagittal-plane movement control) are potential risk factors for ACL injury.1-5
Electromyographical (EMG) studies have demonstrated that females may have sex-related differences in the muscle onset time during the athletic movement.6,7 Wojtys et al. reported that female athletes have a slower response of hamstring activation to anterior stress on the ACL (using anterior tibia translation tests) compared to male athletes in physical examination.7 Cowling and Steele8 reported sex differences in muscle activation strategies of the hamstrings musculature that contradicted the findings of Wojtys et al.7 Males activated their semi-membranosis muscle later than females in the pre-landing phase and reached peak activity sooner.8
Medina et al. stated that female non-athlete subjects recruited vastus medialis (VM) slower than their athletic peers (127.1 vs 408.1 ms), but not slower than the male athletes (127.1 vs 275.7 ms).4 No significant differences were seen among the groups for hamstring musculature activation.4 Medina et al. demonstrated that there were no differences between female and male athletes for time to initial contraction of any muscle groups in a drop landing task.4
Sex differences in neuromuscular control, including ligament dominance, quadriceps dominance (QD), leg dominance, and trunk dominance likely contribute to ACL injury especially in females.9 The inter-limb differences in muscle recruitment patterns, muscle strength, and muscle flexibility tend to be greater in females than in males.9 The second dominance called QD refers to the method of stabilizing the knee joint by primarily using the quadriceps muscles.9 Females preferentially use quadriceps muscles to stiffen and stabilize the knee joint, as compared to males.7,9 Thus, females may exhibit higher activation of quadriceps muscles relative to hamstrings muscles increasing the risk of ACL injury in the landing phase.9
During a jump-landing task, decreased knee flexion angle (0-30 °) is another of the important mechanism for non-contact ACL injuries in females.9 Diminished knee-flexion angles and QD during the preparatory phase of a jump is influenced by high Q/H co-activation ratio.2,10 Furthermore, it seems the high Q/H co-activation ratio was largely influenced by diminished hamstrings activity rather than excessive quadriceps activity during the preparatory phase of a jump task. Walsh et al. performed a correlational analysis of Q/H co-activation ratio during a jump-landing task.2 The result of Walsh's study indicated that Q/H co-activation ratio was significantly and negatively correlated with knee-flexion angle at initial contact (r=0.442).2 It is also reported that Q/H co-activation ratio was negatively correlated with hamstrings activity, but not quadriceps.2 These findings suggest that interventions designed to enhance preparatory hamstring activity may be effective in minimizing the Q/H co-activation ratio and placing the knee in a more flexed position at initial contact thereby preventing ACL loading and injury.11 Walsh et al. suggested that investigations on ACL injury-prevention programs should be conducted to examine strategies to modify preparatory phase, Q/H co-activation ratio, and decrease quadriceps activation after ground foot contact.2
In recent years, prevention of ACL injuries has become a key issue among researchers. Plyometric, balance training, agility training, and instructions for landing modifications with knee flexion more than 30 ° in jump-landing maneuver are common components of ACL injury prevention training programs.9,12 An increase in knee flexion has been reported as a result of conducting plyometric training,13 plyometric or balance training,14 and in response videotape feedback.15
It has been suggested that ACL injury prevention programs should target the development of motor programs characterized by coordinated muscle activation.9,16,17 Perturbation training is a specialized neuromuscular training program designed to aid in the development of dynamic knee stability among individuals with complete ACL rupture.11,17 Although the influence of perturbation training has been studied in varied populations, the effects of this types of training on female athletes with unbalanced hamstring and quadriceps muscle onset time and activation as well as limited knee flexion angles during landing has not been well understood. Letafatkar et al. recommended perturbation training to female athlete's coaches as a means to eliminate the QD deficit and improve athletic performance.9 Further research should be performed to focus on how to modify quadriceps and hamstrings muscle onset times, activation, and knee flexion angle.2,4,18
Therefore, the purpose of this study was to evaluate the efficacy of perturbation-enhanced neuromuscular training on hamstring and quadriceps onset time and activation, and knee flexion angle in female athletes with QD deficit during a tuck-jump (TJ) task. The first hypothesis was that the perturbation training group would experience significantly improvement in neuromuscular control and knee flexion angle. The second hypothesis was that the experimental group would experience more changes in neuromuscular control and knee flexion angle than those of the control group.
METHODS
Study Design
Pre - posttest control-group experimental design.
The independent variables were time (pre-test, post-test) and training intervention. The dependent variables were EMG measures including muscle onset time, average, and Q/H co-activation ratio, and knee flexion angle in initial contact, at peak knee flexion, and total knee flexion displacement. This study was approved by the Ethical Committee of the Tehran Medical University.
Participants
Based on the primary evaluation of 60 females, 31 collegiate female handball, basketball and soccer players with QD deficit, between 20 to 25 years of age, volunteered to participate in the study. The number of participants was based on the previous similar research.9 All subjects performed a TJ test to determine QD deficit. An experienced TJ tester assessed the test. A failed trial was defined as when the subjects 1) had an excessive landing contact noise, or 2) had peak knee flexion angle less than 30 ° during landing from TJ.9
All subjects signed the informed consent and completed the health history questionnaires. The questionnaires were reviewed for inclusion and exclusion criteria. Risk and benefits of the study participation were individually explained to the subjects. Exclusion criteria included any lower extremity reconstructive surgery in the prior two years, and any lower-extremity injury or unresolved musculoskeletal disorders that prohibited subjects from sports participation. All subjects participated in off-season training that involved performing three sessions per week, 90 to 120 minutes for every session.
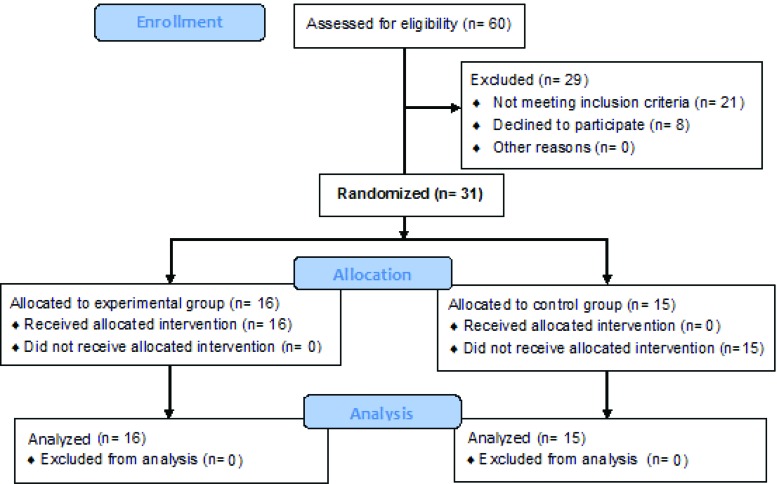
Random assignment was performed by participants selecting a sealed envelope to determine group allocation. Subjects were placed in either the experimental (n=16) group (mean height = 168.03 ± 7.42 cm, body mass = 58.22 ± 6.36 kg) or control (n=15) group (mean height = 167 ± 9.90 cm, body mass = 59.30 ± 7.81). Any subject who missed more than one training session was removed from the study. All control subjects were asked to refrain from any perturbation-type training. (Figure 1)
Figure 1.
Flow diagram of the study.
EMG Assessment
Data were collected by a surface EMG system (Megawin ME6000, Jali Medical, Waltham, MA). The EMG data were collected from five muscles: Rectus Femoris (RF), VM, Vastus Lateralis (VL), Medial Hamstring (MH), and Lateral Hamstring (LH) of the dominant leg.
The dominant leg was defined as the leg used to kick a ball for maximum distance. The skin over the bellies of these muscles was prepared for electrode placement by shaving and cleaning the area with 70% isopropyl alcohol.4 Dual surface electrodes (Skintact, Fannin Ltd, Dublin, Ireland) were placed over the prepared skin in the direction of the muscle fibers. A single reference electrode was positioned over the tibial tuberosity of the dominant limb.17,19 EMG electrodes were placed superficially on the midpoint of the muscle belly for the RF. The EMG sensors for the VM were placed 4 cm superior and 3 cm medial to the superior border of the patella and oriented 55 ° medially concerning vertical.2,18 The EMG sensors for VL were placed 10 cm superior and 7 cm lateral to the superior border of the patella and oriented at approximately 10 ° laterally concerning vertical. For MH the sensors were placed 36% of the distance between the ischial tuberosity and the medial side of the popliteus cavity, starting from the ischial tuberosity;2,18 and finally, the EMG sensors for the LH were placed over the measured midpoint (ischial tuberosity to fibular head) of the muscle belly.2,18 Sensor placements and the absence of cross-talk were confirmed by evaluating the activity of each muscle with manual muscle tests. Once EMG sensor placements were confirmed, the sensors and the leads were secured with pre-wrap and athletic tape to minimize movement artifact. EMG data were sampled at 1000 Hz.19
The maximum voluntarily contraction (MVC) values for each muscle were obtained by collecting one maximal five-second trial after a series of three warm-up trials performed at 50%, 75%, and 100% of maximal effort. The first and last seconds of the MVC trials were removed from the data to ensure only steady-state results during MVC test. The average activity during the middle three seconds of the MVC trial was determined for each muscle.
Data normalization was performed by dividing EMG raw signals into MVC data, and for standardization, the following equation was used, and the muscles activation was reported as the percentage of MVC.
For MVC of the VMO, VL, MH and LH, the subject was asked to sit on a chair with the hips and knees at 90 ° and straps around the legs and trunk. The subject kicked forward on the strap to extend the knee for the quadriceps MVC, and pulled back on the strap to flex the knee for the hamstring MVC.9
The Q/H co-activation ratios were assessed during the preparatory and reactive phases in a TJ task. The Q/H co-activation ratio was computed as the sum of the average EMG amplitude of the quadriceps (RF and VL) divided by the sum of the average EMG amplitude of the hamstrings (MH and LH) for each trial. The Q/H co-activation ratio was computed separately for each of the five TJ repetitions and then the average was taken.19 The preparatory phase encompassed 150 milliseconds before ground contact; the reactive phase consisted of initial ground contact to 350 milliseconds after ground contact.19
The time to initial contraction was based on three standard deviations above baseline, as previously described4 recorded during the quiet period before TJ The footswitch, made by the researchers and placed under the forefoot, simultaneously was used to determine initial ground contact and onset of muscle activity for each trial.9 Initial ground contact was the defined as the initial instant in time when the testing foot first came into contact with the ground.9
All EMG data (TJ task and MVC trials) were band-pass filtered (10 to 350 Hz) and notch filtered (60 Hz at 1-Hz width) using a Butterworth filter (4th order, zero-phase lag) in the Megawin software package used for the EMG processing. The data were rectified and smoothed by taking the root mean square average of the EMG signal and using a 50-millisecond sliding window function. The data were exported to technical computing software (MATLAB ver. 7.0) for further analysis.
TJ task assessment
The TJ is known as a reliable (ICC=0.88) measurement test to determine abnormal jump-landing mechanism.20 In the current study, the TJ was performed to measure the muscle onset time, muscle activation, and knee flexion angle assessment, before and after training. To perform the TJ, subjects started in a position with feet shoulder-width apart. Initially, they jumped from a slight downward crouched position, with extended arms behind the trunk. They then swung their arms forward as they simultaneously jumped straight up and pulled their knees up as high as possible. The subjects were instructed to get their thighs to parallel to the ground at the peak of the jump. The subjects were encouraged to immediately begin the next TJ to decrease downtime (or landing pause) between each jump. The subjects were also instructed to land softly, using a toe to midfoot rocker landing, and to land in the same footprint with each jump.21
Experimental Procedures
Subjects were first asked to perform a warm-up (bicycle ergometer for five to seven minutes, and dynamic stretching of both lower extremities for five minutes). Subjects were allowed a one-minute rest between test trials. Each subject then was allowed to practice three-reparation TJ preparation trials before data collection. In the next step, subjects performed the five-repetition TJ task, and the average scores of five repetitions were recorded. Subjects were allowed a one-minute rest between test trials.
During performing the TJ task on the foot switch, the EMG electrodes (as described above) and electrogoniometers (M110, Biometrics Ltd., Gwent, UK; ICC=0.64-0.9722) applied to the dominant leg. The lower segment of the electrogoniometer (known as the shank) was fixed and the knee movement was obtained by moving the upper segment (known as the thigh).22 Meanwhile, muscle activation and knee flexion angles were measured. Knee flexion angle at initial contact, peak knee flexion angle, and knee flexion displacement during the landing phase of the TJ task were calculated for each trial.20-24 Knee flexion displacement was calculated by subtracting the knee flexion angle at initial contact from the peak knee flexion angle.19
Perturbation- enhanced neuromuscular training
The subjects in experimental group performed eighteen sessions of perturbation-neuromuscular training over six weeks under the supervision of two investigators at the Physical Therapy Clinic according to the protocol described by Letafatkar et al.9 and Taylor.25
Every training session lasted approximately one hour and consisted of rocker board (Figures 2, 3) roller board (Figure 4) and roller board/BOSU ball (Figure 5) activities with stationary platform perturbation drills. (Figure 6) Progression of perturbation drills is shown in Table 1. The verbal instructions were provided to subjects for performing appropriate technique execution. The instructions included “keep your knees soft”, “keep your trunk still”, and “relax between perturbations”. Ultimately, each subject was free to respond to the perturbation given the constraints of the drill and verbal cuing. Intensity, sport specificity, and the difficulty of the drills were progressed systematically. (Figures 7, 8, 9) Sequencing of each training session consisted of different perturbation drills.9
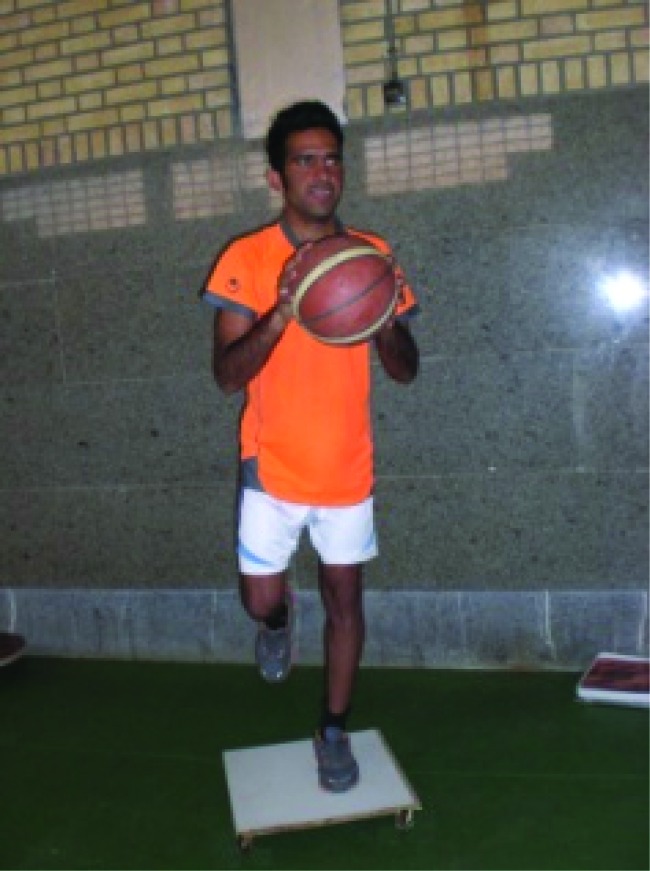
Figure 2.
Two leg rocker board.
Figure 3.
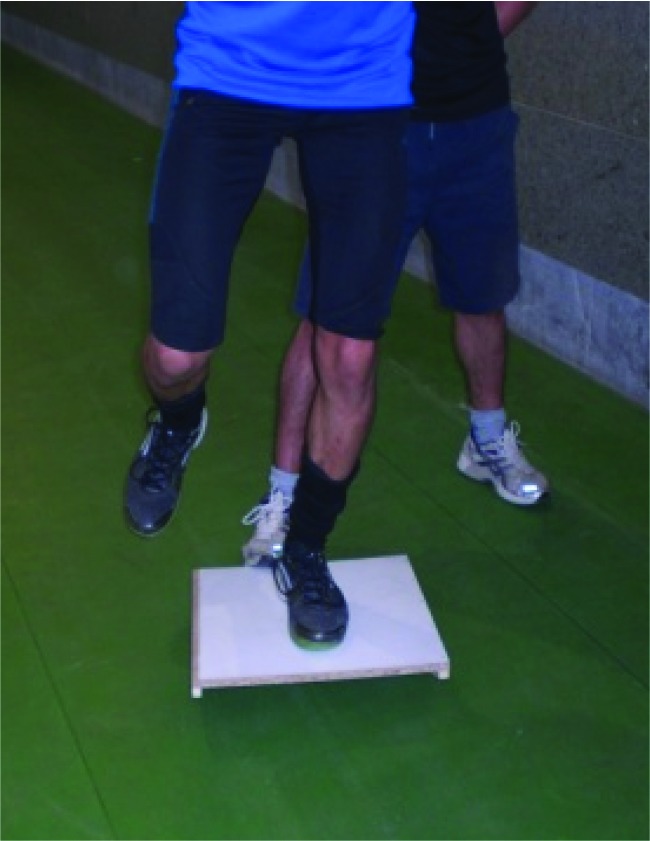
One leg rocker board.
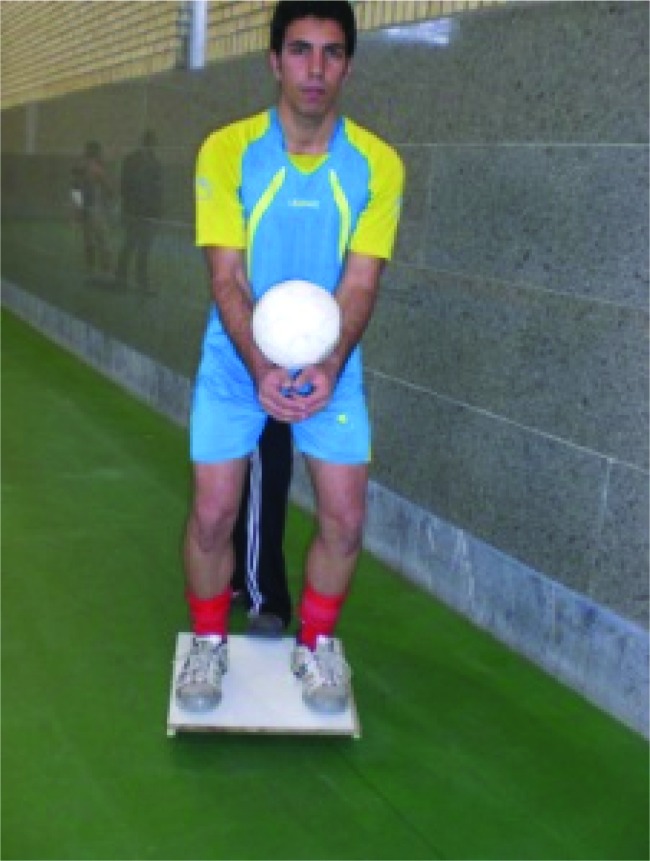
Figure 4.
Roller board/stable (weight scale) surface.
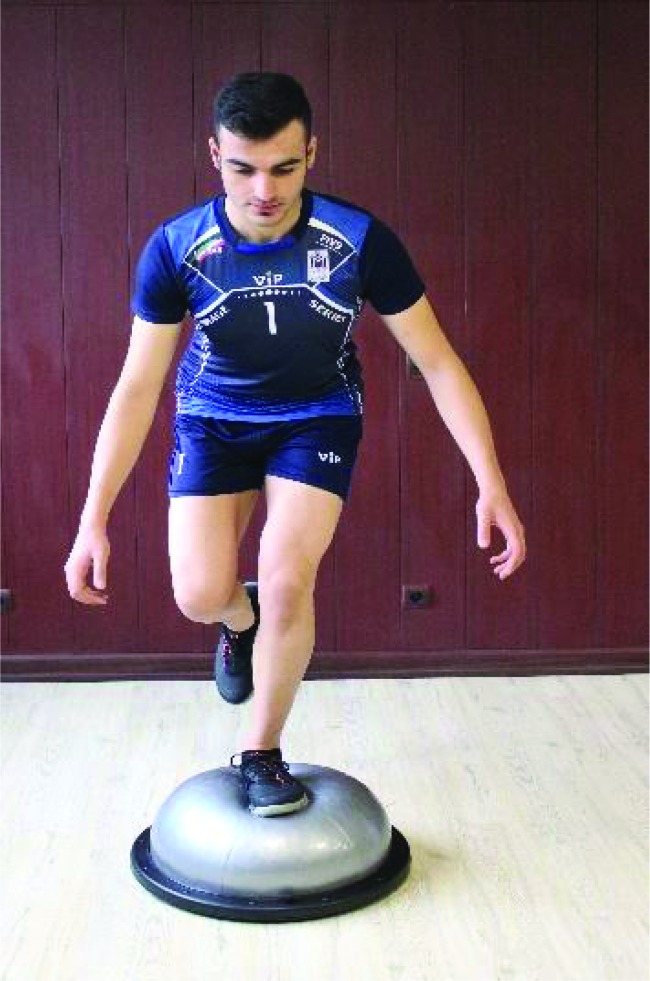
Figure 5.
Roller Board/BOSU ball.
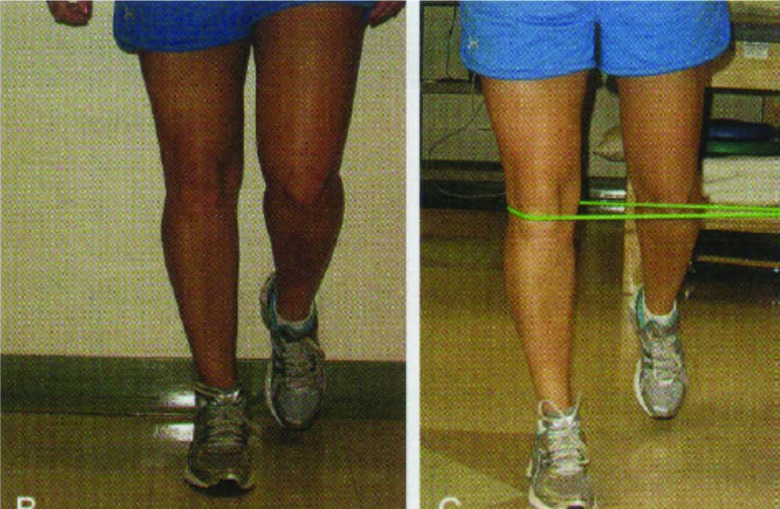
Figure 6.
Thera Band feedback/perturbation training.
Table 1.
Sample of perturbation training progression.
| Week | Exercises* |
|---|---|
| 1 | Two leg/ Rocker Board (A/P; M/L) (2 × 30-60 s) (Figure 2) One leg/ Rocker Board (A/P; M/L) (2 × 30-60) (Figure 3) Thera Band feedback training (A/P) (1 × 30-60) (Figure 4) |
| 2 | Two leg/ Rocker Board (A/P; M/L) (3 × 30-60) One leg/ Rocker Board (A/P; M/L) (3 × 30-60) Thera Band feedback training (A/P) (2 × 30-60) |
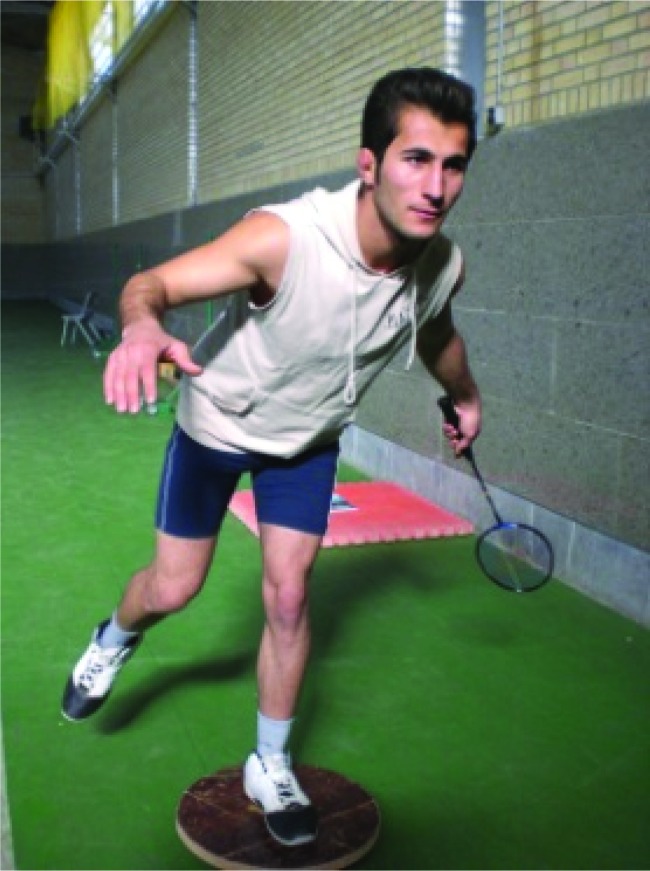
| 3 | Thera Band feedback training (A/P) (2 × 30-60) Roller Board/ Bosu ball (A/P; M/L; Diagonal) (2 × 30-60) (Figure 5) Simple sport specific technique on Rocker Board (2 × 30-60) (Figure 7) Moderate sport specific technique on Rocker Board (2 × 30-60) (Figure 8) |
| 4 | Thera Band feedback training (A/P) (2 × 30-60) Roller Board/ Bosu ball (A/P; M/L; Diagonal) (3 × 30-60) Simple sport specific technique on Rocker Board (3 × 30-60) Moderate sport specific technique on Rocker Board (2 × 30-60) |
| 5 | Simple sport specific technique on Rocker Board (3 × 30-60) Moderate sport specific technique on Rocker Board (3 × 30-60) Roller Board/ stable (weight scale) surface (2 × 30-60) (Figure 8) Advanced sport specific technique on Rocker Board (2 × 30-60) (Figure 9) |
| 6 | Simple sport specific technique on Rocker Board (3 × 30-60) Moderate sport specific technique on Rocker Board (3 × 30-60) Roller Board/ stable (weight scale) surface (3 × 30-60) (Figure 8) Advanced sport specific technique on Rocker Board (3 × 30-60) |
30 s between sets and 2 min between exercises.
A/P = anterior/posterior, M/ L = medial/lateral
Figure 7.
Simple sport specific technique on rocker board.
Figure 8.
Moderate demand sport specific technique on rocker board.
Figure 9.
Advanced sport specific technique on rocker board.
All subjects regularly participated in the scheduled off-season strength training, practices, and games and tournaments, but the experimental group also participated in a perturbation- enhanced neuromuscular training program three times a week over six weeks. The experimental group was given instructions and illustrations of each perturbation exercise before the first training session. Post-test were taken a day after the training program was completed.
Data Analysis
Descriptive data were calculated for all variables. A mixed-design repeated measure ANOVA (2 × 2) was used to test for interactions and main effects for time (pre- vs posttest) and group (perturbation training vs control) between the knee flexion angle and electromyography variables. Statistical analyses were conducted in SPSS (SPSS, Version 18.0, Chicago; IL). Statistical significance was established a priori at p < 0.05 to test the directional (one-sided) hypothesis that perturbation training would be more effective than control in improving knee flexion angle and electromyography in active participants.
The effect size (Cohen's d) was calculated to determine the standardized mean difference for each variable. Effect sizes were classified as small (d = 0.20), medium (d = 0.50), or large (d = 0.80).
RESULTS
The perturbation training and control groups had a participation rate of 100% during the study period. A significant interaction of group and time was observed following the study with selected knee flexion angle and electromyography measures which indicate that training outcomes were different between perturbation training and control groups.
The mean and standard deviation of the subjects’ demographic characteristics are presented in Table 2, and descriptive data of all variables are shown in Tables 3 and 4.
Table 2.
Demographic characteristics of participants, reported as mean +/- standard deviations.
| Experimental | Control | p-value | |
|---|---|---|---|
| Age (years) | 22.34 ± 2.4 | 21.56 ± 2.7 | 0.210 |
| Weight (kg) | 58.22 ± 6.36 | 59.30 ± 7.81 | 0.198 |
| Height (cm) | 168.03 ± 7.42 | 167 ± 9.90 | 0.109 |
| Exercise experience (years) | 5 ± 1.3 | 5.2 ± 0.7 | 0.280 |
Table 3.
Intra- and inter-group differences for muscle activation and Q:H co-activation variables.
| Variables | muscles | Phases | Group | Pre-test (Mean±SD) | Post-test (Mean±SD) | Intra-group differences | Inter-group differences |
|---|---|---|---|---|---|---|---|
| Muscle activation (mv) | RF | Preparatory | Experimental | 122.59 ± 25.10 | 89.18 ± 20.66 | 0.001* | p=0.003† ES: 0.628 |
| Control | 124.80 ± 24.26 | 123.84 ± 23.73 | 0.317 | ||||
| Reactive | Experimental | 130.59 ± 33.30 | 87.11 ± 23.18 | 0.001* | p=0.001† ES: 0.659 | ||
| Control | 135.03 ± 35.52 | 137.23 ± 36.99 | 0.434 | ||||
| VM | Preparatory | Experimental | 56.51 ± 11.65 | 78.88 ± 13.76 | 0.009* | p=0.011† ES: 0.621 | |
| Control | 51.73 ± 9.07 | 52.69 ± 9.25 | 0.315 | ||||
| Reactive | Experimental | 54.66 ± 16.52 | 88.77 ± 18.47 | 0.004* | p=0.003† ES: 0.619 | ||
| Control | 49.96 ± 14.56 | 47.03 ± 15.12 | 0.403 | ||||
| VL | Preparatory | Experimental | 115.48 ± 25.77 | 78.07 ± 13.68 | 0.014* | p=0.019† ES: 0.527 | |
| Control | 109.61 ± 26.19 | 108.92 ± 26.84 | 0.427 | ||||
| Reactive | Experimental | 108.81 ± 16.77 | 84.25 ± 14.12 | 0.023* | p=0.021† ES: 0.527 | ||
| Control | 104 ± 15.48 | 106.26 ± 17.87 | 0.368 | ||||
| MH | Preparatory | Experimental | 40.74 ± 9.78 | 76.62 ± 13.44 | 0.002* | p=0.007† ES: 0.675 | |
| Control | 36.69 ± 7.66 | 35.53 ± 8.11 | 0.248 | ||||
| Reactive | Experimental | 29.44 ± 8.42 | 83.25 ± 19.70 | 0.001* | p=0.001† ES: 0.689 | ||
| Control | 26.76 ± 9.67 | 27.34 ± 9.91 | 0.239 | ||||
| LH | Preparatory | Experimental | 75.03 ± 15.90 | 56.81 ± 13.96 | 0.028* | p=0.023† ES: 0.457 | |
| Control | 71.88 ± 9.96 | 72.07 ± 10.09 | 0.412 | ||||
| Reactive | Experimental | 96.14 ± 12 | 89.11 ± 16.11 | 0.032* | p=0.042† ES: 0.367 | ||
| Control | 94.38 ± 12.86 | 95.23 ± 12.80 | 0.334 | ||||
| Q:H co-activation | Preparatory | Experimental | 1.50 ± 0.29 | 1.18 ± 0.12 | 0.029* | p=0.003† ES: 0.689 | |
| Control | 1.51 ± 0.39 | 1.50 ± 0.34 | 0.373 | ||||
| Reactive | Experimental | 1.29 ± 0.12 | 1 ± 0.06 | 0.024* | p=0.013† ES: 0.669 | ||
| Control | 1.25 ± 0.11 | 1.24 ± 0.14 | 0.342 | ||||
* Intra-group difference; † Inter-group differences
Table 4.
Intra- and inter-group differences for onset of muscle activation variable.
| Variables | muscles | Group | Pre-test (Mean±SD) | Post-test (Mean±SD) | Intra-group differences | Inter-group differences |
|---|---|---|---|---|---|---|
| Onset of activation (ms) | RF | Experimental | 375.81 ± 37.13 | 240.29 ± 26.80 | 0.001* | p=0.001† ES: 0.718 |
| Control | 363.07 ± 30.10 | 370.76 ± 38.72 | 0.543 | |||
| VM | Experimental | 174.33 ± 18.81 | 204.48 ± 17.25 | 0.037* | p=0.004† ES: 0.657 | |
| Control | 181.38 ± 15.49 | 179.73 ± 15.42 | 0.311 | |||
| VL | Experimental | 274.22 ± 30.93 | 190.44 ± 19.51 | 0.026* | p=0.023† ES: 0.567 | |
| Control | 268.73 ± 24.24 | 270.26 ± 27.23 | 0.256 | |||
| MH | Experimental | 65.44 ± 9.91 | 157.59 ± 37.03 | 0.001* | p=0.001† ES: 0.711 | |
| Control | 68.34 ± 12.23 | 66.92 ± 12.53 | 0.436 | |||
| LH | Experimental | 89.55 ± 14.25 | 99.81 ± 17.80 | 0.038* | p=0.031† ES: 0.531 | |
| Control | 91.84 ± 11.16 | 90.38 ± 10.80 | 0.540 |
* Intra-group difference; † Inter-group differences.
ES = Effect size, RF = Rectus Femoris, VM = Vastus Medialis, VL = Vastus Lateralis, MH = Medial Hamstring, LH = Lateral Hamstring
Table 5.
Intra- and inter-group differences for kinematic variables during the Tuck Jump test.
| Variables | Group | Pre-test (Mean±SD) | Post-test (Mean±SD) | Intra-group differences | Inter-group differences | |
|---|---|---|---|---|---|---|
| Knee kinematic | Initial contact | Experimental | 28.29 ± 3.83 | 39.92 ± 2.41 | 0.027* | P=0.011† ES: 0.649 |
| Control | 27.15 ± 3.29 | 26.07 ± 3.14 | 0.673 | |||
| Peak | Experimental | 51.55 ± 2.79 | 72.59 ± 6.16 | 0.001* | P=0.001† ES: 0.832 | |
| Control | 52.73 ± 4.97 | 51.50 ± 6.71 | 0.458 | |||
| Displacement | Experimental | 24.40 ± 3.69 | 34.03 ± 5.39 | 0.037* | P=0.013† ES: 0.612 | |
| Control | 25.40 ± 4.18 | 24.26 ± 4.06 | 0.543 |
* Intra-group difference; † Inter-group differences
ES = Effect size
Demographic characteristics (age, p=0.210; weight, p=0.198; height, p=0.109; exercise experience, p=0.280) did not differ between the groups (p>0.05).
Muscle Activation and Onset of Muscle Activation
A significant interaction of group and time was also found following the perturbation training program on muscle activation and the onset of muscle activation measures. Relative to control, the perturbation training program showed greater improvement in muscle activation [RF (P preparatory=0.003, P reactive=0.001); VM (P preparatory=0.011, P reactive=0.003); VL (P preparatory=0.019, P reactive=0.021); MH(P preparatory=0.007, P reactive=0.001); and LH(P preparatory=0.023, P reactive=0.042)] and the onset of muscle activation [RF (P=0.001), VM(P=0.004), VL(P=0.023), MH (P=0.001) and LH (P=0.031)] from pretest to posttest.
Q/H co-activation ratio
A significant interaction of group and time was also found following the perturbation training program on Q/H co-activation measure. Relative to control, the perturbation program showed greater improvement in the Q/H co-activation ratio in preparatory phase from a mean (95% CI) pretest score of 1.50 ± 0.29 (1.28–1.63) to 1.18 ± 0.12 (1.03–1.43; p < .05) and reactive phase from a mean (95% CI) pretest score of 1.29 ± 0.12 (1.03–1.34) to 1 ± 0.06 (0.94–1.2; p < .05).
Kinematic data
A significant interaction of group and time was also found following the perturbation training program on knee flexion angle measures. Relative to control, the perturbation training program showed greater improvement in the initial contact knee flexion angle from a mean (95% CI) pretest score of 28.29 ± 3.83 (25–29.32) to 39.92 ± 2.41 (36.23–42.03; p < .05), peak knee flexion angle from a mean (95% CI) pretest score of 51.55 ± 2.79 (48–54.21) to 72.59 ± 6.16 (67.13–79; p < .05) and knee flexion displacement angle from a mean (95% CI) pretest score of 24.40 ± 3.69 (21–26.37) to 34.03 ± 5.39 (28.91–39; p < .05).
DISCUSSION
The purpose of this study was to determine the efficacy of a perturbation- enhanced neuromuscular training program on knee flexion angle as well as on hamstring and quadriceps muscle onset time and activation in athletes with QD deficit during the TJ task. It was hypothesized that a perturbation program would result in improvement of neuromuscular control as measured by EMG parameters and knee flexion angles during the TJ task in experimental group compared the control group.
Statistical analysis revealed that VM and MH pre-activation were significantly different between the experimental and control groups. A significant decrease in Q/H co-activation ratio may lead to improvement of dynamic stability to the sagittal plane at the knee and a significant increase in knee flexion in the decelerating phase of the TJ.
The findings of the current study may relate to ACL injury prevention. Perturbations can excite the afferent pathways that provide information to the muscle spindle. The more increased sensitivity of the muscle spindles, the higher state of readiness of muscles to respond to disruptive forces and consequently the more improvement in joint stability.11
Muscle onset time of hamstring and quadriceps
In the pretest, there were no statistical differences between the experimental and control groups in the muscle onset time of all five muscles. In both groups, RF and VL demonstrated somewhat earlier recruitment than hamstrings. This improper muscle onset time may be due to the demands of the subject's sport-specific task (football, handball, and basketball). Insufficient neuromuscular control in females could alter the recruitment of the knee muscles in landing tasks resulting in altered quadriceps and hamstrings activation strategies compared to males. Females may preferentially rely on higher activation of quadriceps muscles relative to hamstrings muscles in landing intensities in order to stabilize the knee. After training, females in the experimental group had an earlier onset of MH, LH and VM activity, indicating improved neuromuscular performance.
Notably, knee ligament injuries have been estimated to occur at 73 ms,11 with reflexive muscle responses occurring at 128 ms, after the offending stimulus. The latency of muscular responses in a knee ligament injury scenario suggests that muscular responses are too slow to prevent injury. Preparatory muscle activity may improve reactive muscle reactivity via the muscle spindle by identifying unexpected perturbations more quickly,26 and potentially reduce the risk of knee ligament injury.
In the current study, the latency of MH decreased after six weeks of perturbation training in the experimental group. Improvement in the activation of MH may decrease the incidence of the ACL injuries at high flexion angles. Decreased hamstring latency may decrease the time required to stabilize the tibia before an anterior translation force occurs. It also, before the loading phase that occurs during ground contact, may help dynamically protect the integrity of the knee joint and surrounding structures.27 In addition, the decrement of hamstring latency is of particular importance in landing, where the reduction in the response time can lead to a lack of appropriate postural adjustments and increase in the loads experienced at the knee joint.28
Consistent with Medina et al. after six weeks of perturbation training, a significant reduction in the muscle onset time of RF and VL was observed while the muscle onset time of VM, LH and MH were increased significantly.4 The training-induced change in muscle onset time of MH activity is a positive neuromuscular adaptation. Hamstring activation before ground contact (especially in female athletes) is a more desirable neuromuscular characteristic when attempting to reduce ACL injury risks.
Shultz et al. observed that after perturbation, a silent period occurs in the medial and lateral quadriceps.28 The silent period is likely to be either a function of reflexive inhibition in response to sudden unloading of the contracting quadriceps29 or a reciprocal inhibition in response to reflexive activation of the hamstring muscle group.30
Quadriceps earlier activation at knee flexion angles of less than 45 ° are antagonistic to the ACL, significantly increasing ACL strain.9 Conversely, the hamstrings are a dynamic ACL agonist. The combination of changes in quadriceps and hamstrings muscle onset time value among subjects after perturbation training resulted in a more balanced activation strategy that has the potential to reduce the possibility of ACL strain. Due to the medium to large effect sizes reported in this study, the increases and decreases in latency of quadriceps and hamstring are a direct effect of the perturbation training.
Muscle-Activation
The significant changes in EMG activity after six weeks of the perturbation- enhanced neuromuscular training included increased MH and VL muscle activation during the preparatory and reactive phases of landing. In the training sessions, subjects were instructed to keep a deep knee flexion angle and knees neutral (prevent from any sagittal and frontal-plane displacements by keep their knee in line with their toes) during landings and on the roller board/BOSU ball exercises. It is reported that peak activity of the hamstrings occurs between 50-70 degrees of knee flexion.22,23 therefore, the subjects learned the correct posture and landing technique which could increase hamstrings activity. Nagano et al. suggested that increased hamstrings activity after the jump and balance training resulted from the altered muscular control of the lower extremity. The increased activity of MH and VM EMG could indicate greater functional knee stability at ground contact which may decrease the incidence of knee injury because it provides fast compensation for encountering external loads.23
The current results indicated that a significant increase in preparatory and reactive Q/H co-activation ratio was achieved after training for the perturbation group, whereas the same measures in the control group were unchanged. Increased preparatory knee Q/H co-activation ratio may increase knee joint stiffness, decreasing adduction and abduction moments and enhancing dynamic restraint during functional activities.23 Dynamic restraint in the knee can also be achieved through reflexive or reactive neuromuscular control.2 These findings indicated only a trend toward increased reactive muscle activation. This was observed after ground contact, when the perturbation group appeared to have more symmetric Q/H co-activation. High Q/H co-activation ratio can increase strain on the ACL and predispose athletes to non-contact injuries.2,10 However, perturbation training may produce neuromuscular adaptations that encourage more symmetric quadriceps and hamstrings co-activation and balance joint loads for dynamic restraint.31 Calculations revealed that the intra-group effect size of perturbation training ranged from 0.06 to 0.61(small to moderate) (Table 4).
Knee flexion angle
The pretest initial knee flexion angle, peak knee flexion angle, and knee flexion displacement in the treatment group were 28.29 ± 3.83 °, 51.50 ± 5.79 ° and 24.40 ± 3.69 ° respectively. At posttest, the initial knee flexion, peak knee flexion, and knee flexion displacement significantly increased to 39.92 ± 2.41 °, 72.59 ± 6.16 ° and 34.03 ± 5.39 ° respectively in the perturbation training group, reaching a desirable level (50-70 degrees) of peak knee flexion.22 There were no significant differences from pretest to posttest in the control group. Myer stated that the quadriceps, through the anterior pull of the patellar tendon on the tibia, contributes to ACL loading when knee flexion is less than 30 º.2,10,20 Hamstrings contraction cannot reduce ACL strain with the knee slightly flexed because these muscles meet the tibia at a small angle.23 Increased flexion angle that is seen after perturbation training is described as the best accommodation in female athletes that can somewhat protect the ACL from injury risk.2
The results of the present study suggest that, during landing from a jump, one strategy for the prevention of ACL injury is to maintain high hamstring muscle activity, It seems exercises that increase the strength and activation of the hamstring muscle may be an effective method to prevent ACL injury.2,18 Hamstring activity was increased after training in both the preparatory and reactive phases both of which could lead to increased the knee stability. As previously mentioned, during the perturbation training subjects were instructed to have a deep knee flexion angle and keep their knees in line with their toes without any sagittal and frontal-plane displacements. It is found that increased knee flexion angles may lead to changes in the function of the quadriceps and the hamstrings.20-23 Previous authors have shown that subjects in the low flexion angle group during landing demonstrated decreased energy absorption at the knee and hip.32 Thus, increased knee flexion during landing could increase energy absorption in the knee.20,23
Limitations of the study
There were some limitations to this study. Firstly, only the short-term effects of the ACL injury prevention training were examined. Examining the long-term effects of the perturbation training program and its effects on ACL injury prevention in a larger sample size is recommended. The effects of the subjects’ menstrual cycle were not considered. Thus, the acquired changes after perturbation training in landing and TJ could be attributable something other than the training.
Considering the small to moderate effect sizes in the perturbation group, it would seem that this program could be used for the correction of QD deficit. However, the mechanism by which this occurs has not been determined and additional larger samples and other EMG factors (muscle activity) should be analyzed. Thirdly, there was likely cross-talk for the muscles used in this study, as is typical in surface EMG. The authors tried to minimize cross-talk by considering and carefully selecting the appropriate electrode size, inter-electrode distance, and the locations of electrode placement for EMG data recordings over each of the muscles. Fourthly, while the authors used a foot switch as the instrument to determine the initial ground contact during landing, this researcher created tool may have had some inherent error, which was a limitation of this study, therefore, using a more accurate and reliable tool such as a force plate is recommended. Finally, because of governmental rules pictures of female participants were not allowed, thus only male participants are shown in figures.
CONCLUSIONS
The results of the current study indicate that implementation of progressive perturbation training can increase VM and MH muscle pre-activation, decrease quadriceps to hamstring co-activation ratio, and decrease the latency for MH, LH, and VM in female athletes with QD deficit as determined via a TJ assessment. Significantly increased knee flexion angles during the TJ were also observed after the six-week perturbation training in female athletes with QD deficit. The resultant neuromuscular adaptations support the use of perturbation training to enhance dynamic functional stability at the knee joint during jumping activities.
REFERENCES
- 1.Krosshaug T Nakamae A Boden BP. Mechanisms of anterior cruciate ligament injury in basketball: video analysis of 39 cases. Am J Sports Med. 2007;35:359-67. [DOI] [PubMed] [Google Scholar]
- 2.Renstrom P Ljungqvist A Arendt E Beynnon B Fukubayashi T Garrett W Georgoulis T Hewett TE Johnson R Krosshaug T Mandelbaum B. Non-contact ACL injuries in female athletes. Br J Sports Med. 2008;42:394-412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sutton KM Bullock JM. Anterior cruciate ligament rupture: differences between males and females. J Am Acad Orthop Surg. 2013;21:41-50. [DOI] [PubMed] [Google Scholar]
- 4.Medina MJ McLeod CVT Howel KS, et al. Timing of neuromuscular activation of the quadriceps and hamstrings prior to landing in high school male athletes, female athletes, and female non-athletes. J Electromyo Kinesiol. 2008;18:591-97. [DOI] [PubMed] [Google Scholar]
- 5.Hewett TE Zazulak BT Myer GD, et al. A review of electromyographic activation levels, timing differences, and increased anterior cruciate ligament injury incidence in female athletes. Br J Sports Med. 2005;39:347-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Myer GD Ford KR Hewett TE. The effects of gender on quadriceps muscle activation strategies during a maneuver that mimics a high ACL injury risk position. J Electromyo Kinesiol. 2005;15:181-89. [DOI] [PubMed] [Google Scholar]
- 7.Wojtys EM Huston LJ. Neuromuscular performance in normal and anterior cruciate ligament-deficient lower extremities. Am J Sports Med. 1994;22:89-104. [DOI] [PubMed] [Google Scholar]
- 8.Cowling EJ Steele JR. Is lower limb muscle synchrony during landing affected by landing? J Electromyo Kinesiol. 2001;11:263-8. [DOI] [PubMed] [Google Scholar]
- 9.Letafatkar A Rajabi R Tekamejani EE, et al. Effects of perturbation training on knee flexion angle and quadriceps to hamstring co-contraction of female athletes with quadriceps dominance deficit: Pre-post intervention study. The Knee. 2015;22:230-36. [DOI] [PubMed] [Google Scholar]
- 10.Begalle LR DiStefano JL Blackburn T, et al. Quadriceps and Hamstrings Coactivation during Common Therapeutic Exercises. J Athl Train. 2012;47:396-405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hurd WJ Chmielewski TL Snyder-Mackler L. Perturbation- enhanced neuromuscular training alters muscle activity in female athletes. Knee Surg Sports Traumatol Arthrosc. 2006;14:60-9. [DOI] [PubMed] [Google Scholar]
- 12.Petersen W Braun C Bock W. A controlled prospective case control study of a prevention training program in female team handball players: The German experience. Ach Orthop Trauma Surg. 2005;125:614-21. [DOI] [PubMed] [Google Scholar]
- 13.Lephart SM Abt JP Ferris CM. Neuromuscular and biomechanical characteristic changes in high school athletes: a plyometric versus basic resistance program. Br J Sports Med. 2005;39:932-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Myer GD Ford KR McLean SG, et al. The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med. 2006;34:445-55. [DOI] [PubMed] [Google Scholar]
- 15.Onate JA Guskiewicz KM Marshall SW. Instruction of jump landing technique using videotape feedback. Am J Sports Med. 2005;33:831-842. [DOI] [PubMed] [Google Scholar]
- 16.Ball N Joanna S. Effect of muscle action, load and velocity variation on the bilateral neuromuscular response. J Exerc Physiol. 2011;14:1-2. [Google Scholar]
- 17.Fitzgerald GK Axe MJ Snyder-Mackler L. The efficacy of perturbation training in nonoperative anterior cruciate ligament rehabilitation programs for physical active individuals. Phys Ther. 2000;80:128-40. [PubMed] [Google Scholar]
- 18.Palmieri-Smith MR McLean GS Ashton-Miller AJ, et al. Association of Quadriceps and Hamstrings Cocontraction Patterns with Knee Joint Loading. J Athl Train. 2009;44:256-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Chmielewski TL Hurd WJ Rudolph KS, et al. Perturbation training improves knee kinematics and reduces muscle cocontraction after complete unilateral anterior cruciate ligament rupture. Phys Ther. 2005;85:740-9. [PubMed] [Google Scholar]
- 20.Myer GD Ford KR Khoury J, et al. Development and validation of a clinic-based prediction tool to identify female athletes at high risk for anterior cruciate ligament injury. Am J Sports Med. 2010;38:2025-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Myer GD Ford KR Hewett TE. Tuck jump assessment for reducing anterior cruciate ligament injury risk. Athl Ther Today. 2008;13:39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sato TD Hansson GÅ Coury HJ. Goniometer crosstalk compensation for knee joint applications. Sensors. 2010;10:9994-10005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nagano Y Ida H Akai M, et al. Effects of jump and balance training on knee kinematics and electromyography of female basketball athletes during a single limb drop landing: pre-post intervention study. Sports Med, Arthrosc Rehab Ther Technol. 2011;3:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Herrington L Myer GD Munro A. Intra and inter-tester reliability of the tuck jump assessment. Phys Ther Sport 2013;14:152-5. [DOI] [PubMed] [Google Scholar]
- 25.Taylor JB. Lower extremity perturbation training. Strength Cond J. 2011;33:76-83. [Google Scholar]
- 26.Beard DJ Dodd CA Trundle HR. Proprioception enhancement for anterior cruciate ligament deficiency: a prospective randomized trial of two physiotherapy regimes. J Bone Joint Surg. 1994;76:654-9. [PubMed] [Google Scholar]
- 27.DeMont RG Lephart SM. Effect of sex on preactivation of the gastrocnemius and hamstring muscles. Br J Sports Med. 2004;38:120-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Besier TF Lloyd DG Ackland TR. Muscle activation strategies at the knee during running and cutting maneuvers. Med Sci Sport Exerc. 2003;35:119-27. [DOI] [PubMed] [Google Scholar]
- 29.Shultz JS Perrin HD Adams JM, et al. Neuromuscular Response Characteristics in Men and Women after Knee Perturbation in a Single-Leg, Weight-Bearing Stance. J Athl Train. 2001;36:37-43. [PMC free article] [PubMed] [Google Scholar]
- 30.Hewett TE Ford KR Hoogenboom BJ. Understanding and preventing ACL injuries: current biomechanical and epidemiologic considerations. N Am J Sport Phys Ther. 2010;5:234. [PMC free article] [PubMed] [Google Scholar]
- 31.Chimera JN Swanik AK Swanik CB, et al. Effects of Plyometric Training on Muscle-Activation Strategies and Performance in Female Athletes. J Athl Train. 2004;39:24-31. [PMC free article] [PubMed] [Google Scholar]
- 32.Pollard CD Sigward SM Powers CM. Limited hip and knee flexion during landing is associated with increased frontal plane knee motion and moments. Clin Biomech. 2010;25:142-6. [DOI] [PMC free article] [PubMed] [Google Scholar]