Abstract
Background
Hamstring tightness is a common condition typically assessed via the active knee extension (AKE), passive straight leg raise (PSLR), V-sit and reach (VSR), and finger-floor-distance (FFD).
Purpose
The purpose of this study was to investigate the relationships between four common clinical tests of apparent hamstring tightness. A secondary purpose was to compare the differences in correlations between sub-groups based on positive test findings.
Study Design
Descriptive, correlational laboratory design.
Methods
Recreationally active individuals (N = 81; 23.7 ± 5.9 years) performed the AKE, PSLR, VSR, and FFD in a randomized order, and subsequent correlational analyses were conducted.
Results
Strong correlations were identified between the VSR and FFD (r = -.798, r2 = .637, p < .001); moderate correlations were demonstrated between the PSLR and FFD (r = -.565, r2 = .319, p < .001) and PSLR and VSR (r = .536, r2 = .287, p < .001). Low correlations were found between the PSLR and AKE (r = -.284, r2 = .081, p = 0.01), AKE and VSR (r = -.297, r2 = .088, p = .007), and AKE and FFD (r = .263, r2 = .069, p = .018). If one assessment was identified in a subject as dysfunctional, all relationships were affected, regardless of which assessment was dysfunctional.
Conclusions
The AKE, one of the most common measures for apparent hamstring tightness, has low correlations with the other assessments. Based on the findings of this study, it is possible that not all assessments of AHT are measuring the same phenomena, with each involving different factors of perceived hamstring length.
Level of Evidence
Level 2b.
Keywords: Active knee extension, gold standard, hamstring length, treatment-based classification
INTRODUCTION
The descriptors tightness and flexibility, though often used interchangeably, are related, but differing concepts. Muscular “tightness” is traditionally used as a descriptor of a muscle's physical length, with “tight” muscles having a mild to moderate decrease in length, or a decreased ability to elongate from a normal (neutral) position.1 Flexibility, in contrast, is a physiological concept in which joint excursion is represented by, although not synonymous with, range of motion (ROM) measures, and involves contributions from both joint and soft tissue structures (e.g., nerves, muscles).2
Hamstring tightness, often defined as a lack of ROM with a concomitant feeling of restriction in the posterior thigh, has been documented across all age groups as a potential cause of dysfunctional or restricted movement of the hip.3–11 Hamstring injury, a common occurrence,12–14 often results in lost playing time, decreased performance, and an increased risk of additional injury.15–20 Researchers have prospectively identified that decreased active or passive hip ROM is related to hamstring injury risk;21,22 therefore, clinicians should identify clinical exams that accurately assess apparent hamstring tightness. Apparent hamstring tightness is operationally defined as a multidimensional condition that may include musculoskeletal insufficiency or imbalance,23 neural tension,24 and lumbopelvic dysfunction.25 Several clinical examination tests have been proposed to assess this phenomenon. In research, the active knee extension (AKE)26,27 and the passive straight leg raise (PSLR)28 tests are often considered the gold standards. However, it is also common clinically for apparent hamstring tightness, as well as flexibility, to be assessed using the finger-to-floor distance (FFD) and v-sit and reach (VSR) tests in clinical practice. The AKE test was first described by Gajdosik and Lusin26 as an objective test for measuring hamstring length with the hip held in 90 ° of flexion as the knee is extended. A knee flexion angle of 20 ° or less is considered normal ROM on the AKE29 and knee flexion angles of greater than 20 ° have been used in several studies to identify patients with decreased hamstring extensibility.30–33 The AKE has been found to have high reliability for intra-rater agreement (ICC = .86-.99)26,34 and moderate inter-rater reliability (ICC = .76-.89).35 Variations in testing procedures have been reported in the literature, with some researchers stabilizing the hips using straps26,34 and utilizing a crossbar or box to maintain 90 ° of hip flexion,26,30,31,33,36,37 while other researchers do not.38
The PSLR is a test that allows for passive assessment of apparent hamstring flexibility. The PSLR is performed with the patient supine and the clinician passively raising the leg with the patient relaxed; care should be taken to avoid rotation of the pelvis or flexion of the uninvolved leg.28,39 Normal ROM for the PSLR has been reported as 80 ° of hip flexion.29 The PSLR has been reported to have high intra-rater (r = .91) and inter-rater (r = .93) reliability.40 Additionally, the PSLR has been reported to be moderately correlated with the AKE test (r = .72).34
The V-sit and-reach (VSR) test, a modified version of the classic sit-and-reach test often used when equipment is not available to perform the traditional test, is also used to assess lower extremity flexibility.41 During the VSR, the patient sits on the floor with the feet separated by 30 cm, forming a V-shaped leg position that is maintained as the patient reaches forward as far as possible.37,38 Intra-rater reliability of the VSR has been reported as high (r = 0.98; p<0.05).43 Inter-rater reliability has not been identified in the literature. The VSR has been identified to have a moderate correlation with the PSLR (r = .44-.65).41,44
The FFD is a test used to assess hamstring flexibility during active motion; it requires mobility at the pelvic girdle and lumbar spine, in addition to hamstring extensibility as the individual forward flexes towards the toes. There is conflicting research regarding the validity of determining lumbar motion from the FFD.45,46 The FFD is believed to be a good test for determining hamstring extensibility with intra- and inter-observer reliability ratings of .99.45,46
Although the AKE, PSLR, VSR, and FFD have been identified to have high reliability, the methods for performing the tests are not standardized. In research, these assessments often use cross bars, pulley systems, and straps; however, these methods are often not clinically feasible. Additionally, there is little evidence available in the literature to indicate whether these tests are assessing the same construct (i.e., tightness) or if they are assessing another construct related to flexibility or joint excursion of the hip. Also it is unclear how to interpret the results of the various tests if collected simultaneously in order to assess and categorize patient function. Therefore, the purpose of this study was to investigate the relationships between four common clinical tests of apparent hamstring tightness. A secondary purpose was to compare the differences in correlations between sub-groups based on positive test findings.
METHODS
Participants
For this multi-site study, physically active,47 non-injured participants [N = 58 (24 female, 20.5 ± 1.4 years; 34 males, 20.8 ± 1.7 years)] were recruited from university athletic training clinics as well as the graduate and undergraduate student bodies at two NCAA Division I (Towson, University, University of Idaho), one NCAA Division II (Azusa Pacific University), one NCAA Division III (Waynesburg College), and one NAIA school (Northwestern College).
All participants had complaints of hamstring tightness and an AKE of more than 20 °. The following exclusion criteria were applied: (1) lower extremity injury in the previous six weeks; (2) lumbar pathology including back injury in the previous six weeks, known lumbar spine pathology limiting ROM (discogenic), prior lumbar spine surgical procedures, known lumbosacral spine physical impairments limiting ROM and function; (3) lower extremity surgery within last six months; major ligamentous surgery within last one year; (4) vestibulocochlear disturbances/concussion (5) joint hypermobility syndrome (Beighton Score of four or higher); (6) connective tissue disorders (e.g., Marfans, Ehlos Danlos); or (7) lower extremity neurovascular pathology, including numbness, tingling, and loss of sensation. The study was approved by the Institutional Review Board (IRB) of each data collection site; each participant provided informed consent and the participants’ rights were protected.
Reliability Testing
Given the multi-site nature of the study, intra- and inter-rater reliability of the AKE, PSLR, FFD, and VSR were established prior to the start of the study (Table 1). A convenience sample of 24 participants (14 females, 30.2 ± 4.0 years; 10 males 33.5 ± 6.6 years) was recruited from the graduate population; these participants were not required to have complaints of hamstring tightness and were not included in the correlational analysis.
TABLE 1.
Reliability measures.
| Measurement | Intra-Rater ICC | Inter-Rater ICC (95% CI) | SEM | MDC |
|---|---|---|---|---|
| AKE | 0.80 - 0.89 R1: 0.89 (0.77, 0.95) R2: 0.86 (0.71, 0.94) R3: 0.8 (0.5, 0.92) R4: 0.87 (0.7, 0.94) R5: 0.88 (0.74, 0.95) |
0.94 (0.9, 0.97) | 3.28 ° | 9.08 ° |
| PSLR | 0.87 - 0.91 R1: 0.91 (0.78, 0.96) R2: 0.9 (0.79, 0.96) R3: 0.89 (0.69, 0.96) R4: 0.87 (0.71, 0.94) R5: 0.87 (0.73, 0.94) |
0.88 (0.77, 0.94) | 6.88 ° | 19.07 ° |
| FFD | 0.94 - 0.96 R1: 0.95 (0.89, 0.98) R2: 0.95 (0.9, 0.98) R3: 0.94 (0.86, 0.97) R4: 0.95 (0.88, 0.98) R5: 0.96 (0.91, 0.98) |
0.98 (0.96, 0.99) | 1.54 ° | 4.26 ° |
| VSR | 0.94 - 0.97 R1: 0.95 (0.88, 0.98) R2: 0.97 (0.92, 0.99) R3: 0.96 (0.91, 0.98) R4: 0.94 (0.87, 0.98) R5: 0.95 (0.89, 0.98) |
0.98 (0.97, 0.99) | 1.40 ° | 3.89 ° |
AKE = active knee extension test; FFD = finger-to-floor distance test; MDC = minimum detectable change; PSLR = passive straight leg raise test; SEM = standard error of mean; VSR = V-sit and reach test.
Assessment Procedures
All ROM measurements were collected by the primary investigators; The AKE and PSLR assessments utilized a digital inclinometer smartphone application (Clinometer, https://www.plaincode.com/products/clinometer/). While the Clinometer application has been identified as a valid measure for shoulder48 and ankle ROM,49 this is the first study to use the application for knee and hip measurements. Prior to each testing session, the Clinometer application was calibrated and the participant's leg was marked at the anterior tibia (7.62 cm below the tibial tuberosity) and on the anterior thigh (15.24 cm above the tibial tuberosity) to ensure accurate and consistent placement of the smartphone for use of the Clinometer app and a cloth tape measure was used for the FFD and VSR tests. For the AKE, PSLR, and FFD, the average of three measurements was reported; for the VSR, the third measure stood as the final score.42
Active Knee Extension (AKE) Measurement
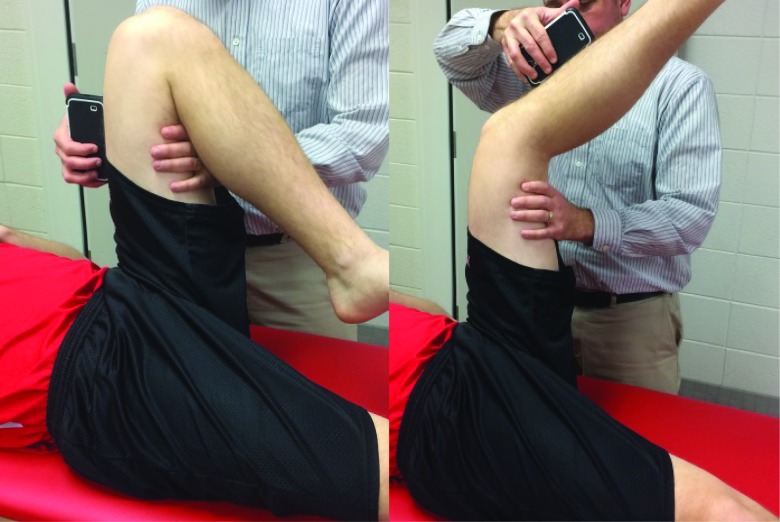
The AKE was measured with the participant in a supine position with one leg in a 90-90 position as an assistant stabilized the contralateral leg in extension. To maintain the 90-degree leg positioning, the clinician placed one hand on the hamstrings four inches superior to the knee while the other hand placed the smartphone inclinometer on the participant's quadriceps aligning the top of the phone with the marking on the participant's thigh. The participant was then instructed to actively extend the knee to the point of discomfort (i.e., an uncomfortable amount of tension),50 while maintaining 90 degrees of hip flexion (Figure 1). When the participant reached the point of discomfort the clinician relocated the smartphone inclinometer from the quadriceps to the mark at the mid-anterior tibia while maintaining 90 degrees of hip flexion with the other hand. Dysfunction on the AKE was defined a priori as more than 20 degrees.29–33
Figure 1.
The AKE was measured with the participant in a supine position with clinician monitoring 90-90 position using the Clinometer smart phone application. Smart phone was aligned at a mark 15.24 cm above tibial tuberosity to ensure 90-90 positioning while patient actively performed knee extension. The smartphone inclinometer was relocated to a mark 7.62 cm below the tibial tuberosity to obtain the measurement.
Passive Straight Leg Raise (PSLR) Measurement
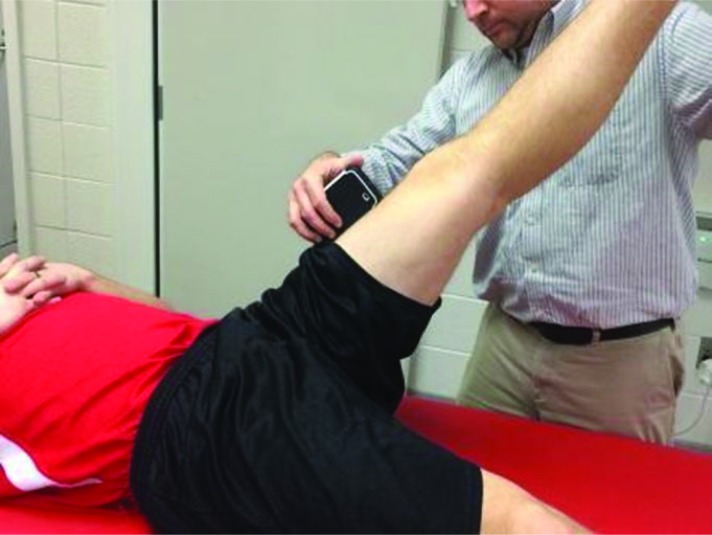
The PSLR was measured as the participant lay supine with the legs extended. While maintaining knee extension and monitoring pelvic rotation, the clinician slowly flexed the participant's hip until the point of discomfort was reached (Figure 2). An assistant stabilized the contralateral leg in an extended position during the procedure. The ROM measurement was recorded with the smartphone inclinometer placed at the mark on the thigh. Dysfunction on the PSLR was defined a priori as less than 80 degrees.29
Figure 2.
The PSLR was measured with the participant in a supine position with the legs extended. Clinician passively flexed hip while keeping knee extended and monitoring for pelvic rotation. The ROM measurement was recorded with the smartphone inclinometer placed a mark 15.24 cm above the tibial tuberosity.
V-Sit and Reach (VSR) Measurement
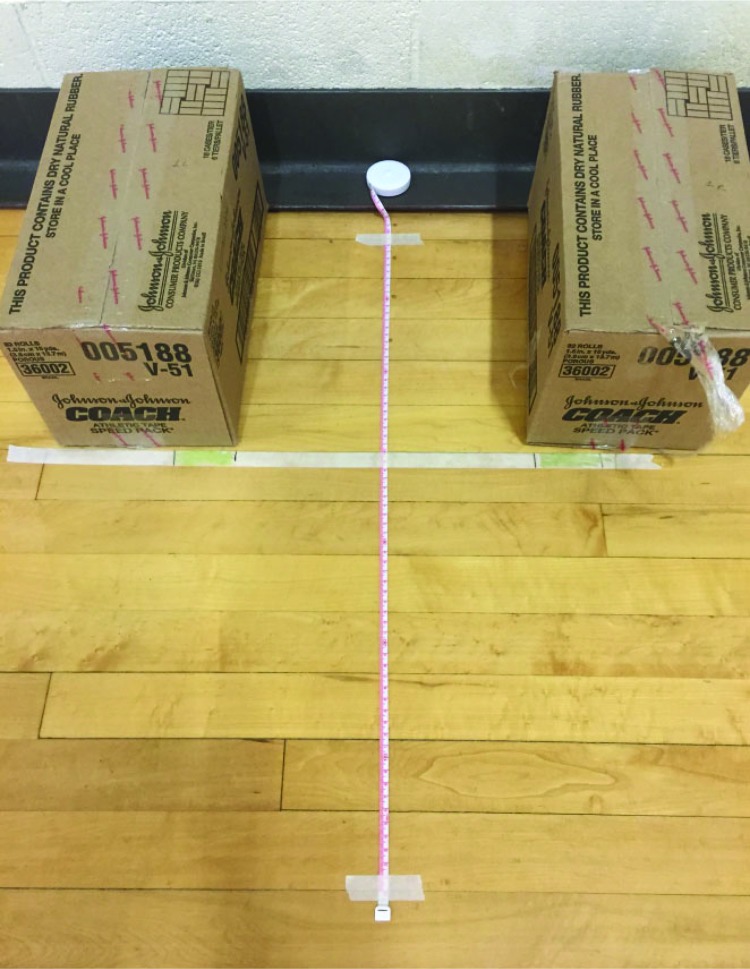
A cloth tape measure affixed to the floor was used to assess the participant's ROM. A piece of tape denoting the baseline “zero” point was placed at the 40 cm mark of the cloth tape measure. To denote the position of the participant's feet, on the baseline tape strip, two marks were placed 15 cm on either side of the tape measure (Figure 3).
Figure 3.
The VSR was performed with the participant in a seated position with the knees extended and feet 30 cm apart. The participant placed one hand over the top of the other hand, flexed at the waist, and reached towards the toes and the distance was recorded using a cloth tape measure.
The participant was instructed to sit on the floor with the legs extended, the feet spaced 30 cm apart, and the plantar surface of each foot touching a box to keep the ankle joints in a neutral position.42 The legs were stabilized in an extended position by the clinician and assistant. To perform the VSR, the participant placed one hand over the top of the other hand, flexed at the waist, and reached towards the toes to the point of discomfort. The motion was performed three times and the measurement was taken on the third attempt; the participant was required to hold the position while the measurement was obtained. The clinician measured from the edge of the baseline “zero” tape (located at the edge of the box) line to the tip of the middle finger. A measurement of “0” indicated the fingertip was in line with the edge of the baseline “zero” tape line. A negative number indicated that the fingers had not reached the edge of the line, while a positive number indicated the fingers were past the edge of the line. Measurements were rounded to the nearest half centimeter. Dysfunction on the VSR was defined a priori as an inability to reach to “zero” line on the tape.
Finger to Floor Distance (FFD) Measurement
The FFD test was performed with the participant standing feet together on a 20 cm box with toes positioned at the edge of the box. The participant flexed at the waist with hands on top of one another, reaching for the toes, and stopping at the point of discomfort. The clinician visually ensured the participant's knees did not flex while performing the movement. The clinician measured from the top edge of the box to the tip of the middle finger of the top hand in centimeters (Figure 4). A measurement of “0” indicated the fingertip was in line with the edge of the box. A positive number indicated that the fingers had not reached the edge of the box, while a negative number indicated the fingers were past the edge of the box. Measurements were rounded to the nearest half centimeter. Dysfunction on the FFD was defined a priori as an inability to reach the edge of the box.
Figure 4.
The FFD test was performed with the participant standing feet together on a 20 cm box with toes positioned at the edge of the box. The participant flexed at the waist with hands on top of one another, reaching for the toes. The clinician measured from the top edge of the box to the tip of the middle finger of the top hand in centimeters using a cloth tape measure.
Statistical Methods and Data Analysis
Statistical analysis was performed using SPSS statistical software (version 23; SPSS Inc., Chicago, IL). Intraclass Correlation Coefficients (ICC) (3,1), with absolute agreement were performed to establish intra- and inter-rater reliability for each measure (Table 1). The standard error of measurement (SEM) and minimal detectable change (MDC) values were also calculated for each dependent variable from the reliability testing data performed prior to this study (Table 1). Standard measurement error was derived using the interrater ICC and the following formula: SEM = SD × √((1)-ICC).51 Minimum detectable change for this study was subsequently calculated using the formula MDC = 1.96 × √2 × SEM (Table 1).51
Pearson's correlations were conducted to determine the relationship between the measurements for all participants (N = 81), as well as for each dysfunctional group (Table 2). For example, the “dysfunctional PSLR group” included all participants who demonstrated dysfunction on the PSLR test. Correlation values were established a priori at 0-0.25 = little, if any, 0.26-0.49 = low, 0.5-0.69 = moderate, 0.70.89 = high, and 0.9-1.0 = very high.52
TABLE 2.
Correlation analysis results between hamstring tightness measures for all participants and for participants with dysfunctional measures.
| AKE | PSLR | VSR | FFD | |
|---|---|---|---|---|
| PSLR | ||||
| All (N = 81) | r = -.284* r2 = .081 p = .01 |
|||
| Dysfunctional† (N = 73) | r = -.291* r2 = .085 p = .012 |
r = .464* r2 = .215 p < .001 |
r = -.520* r2 = .27 p < .001 |
|
| VSR | ||||
| All (N = 81) | r = -.297* r2 = .088 p = .007 |
r = .536* r2 = .287 p < .001 |
||
| Dysfunctional (N = 68) | r = -.266* r2 = .071 p = .028 |
r = .303* r2 = .092 p = .012 |
r = -.733* r2 = .537 p < .001 |
|
| FFD | ||||
| All (N = 81) | r = .263* r2 = .069 p = .018 |
r = -.565* r2 = .319 p < .001 |
r = -.798* r2 = .637 p < .001 |
|
| Dysfunctional (N = 51) | r = .101 r2 = .01 p = .481 |
r = -.297* r2 = .088 p = .034 |
r = -.572* r2 = .327 p < .001 |
AKE = active knee extension test; PSLR = passive straight leg raise test. VSR = V-sit and reach test. FFD = finger-to-floor distance test.
Indicates statistically significance correlation at p≤0.05.
Dysfunction for each group was identified based on the a priori cut points based on the best available literature, as described above. For example, the “dysfunctional PSLR group” included all participants who demonstrated dysfunction on the PSLR test. A priori definitions for dysfunction were as follows: AKE greater than 20 degrees; PSLR less than 80 degrees; VSR inability to reach “zero” line; and FFD inability to reach edge of box.
RESULTS
Reliability Measures
All measurements had high intra-rater and inter-rater reliability assessed with Intraclass Correlation Coefficients (ICC) (3,1), with absolute agreement (Table 1).53
Correlational Analysis for Dysfunctional AKE (N = 81)
Strong correlations were identified between the VSR (mean = -11.7 ± 9.6 cm) and FFD (mean = 6.1 ± 11 cm, r = -.798, r2 = .637, p<0.001). Moderate correlations were found for the PSLR (mean = 58.9 ° ± 15.1 °) and the FFD (r = -.565, r2 = .319, p<0.001) and the PSLR and the VSR (r = .536, r2 = .287, p<0.001). Low correlations were found between the PSLR and AKE (mean = 41.8 ° ± 8.9 °, r = -.284, r2 = .081, p = .01), the AKE and VSR (r = -.297, r2 = .088, p = .007), and the AKE and FFD (r = .263, r2 = .069, p = .018) (Table 2).
Correlational Analysis for Dysfunctional PSLR (N = 73)
Dysfunctional scores on the PSLR (N = 73, mean = 56.1 ° ± 13.2 °) have a strong correlation between the VSR (mean = -12.8 ± 8.8 cm) and FFD (mean = 7.2 ± 10.8 cm, r = -.785, r2 = .616, p<0.001). Moderate correlations were found between the PSLR and FFD (r = -.520, r2 = .27, p<0.001) and low correlations were identified for the PSLR and VSR (r = .464, r2 = .215, p<0.001), the PSLR and AKE (mean = 42.3 ° ± 8.6 °, r = -.291, r2 = .085, p = .012), the AKE and VSR (r = -.316, r2 = .01, p = .007), and the AKE and FFD (r = .244, r2 = .06, p = .038).
Correlational Analysis for Dysfunctional VSR (N = 68)
Dysfunction on the VSR (N = 68, mean = -14.7 ± 7.2 cm) also alters the correlations identified in this analysis. A strong correlation was identified between the VSR and FFD (mean = 8.5 ± 10 cm, r = -.733, r2 = .537, p<0.001). Weak correlations were found between the PSLR (mean = 55.8 ° ± 14.0 °) and FFD (r = -.437, r2 = .191, p<0.001), the PSLR and VSR (r = .303, r2 = .092, p = .012), the PSLR and AKE (mean = 42.6 ° ± 8.5 °, r = -.276, r2 = .076, p = .023), AKE and VSR (r = -.266, r2 = .071, p = .028), and the AKE and FFD (r = .194, r2 = .038, p = .113).
Correlational Analysis for Dysfunctional FFD (N = 51)
When the FFD was dysfunctional (N = 51, mean = 12.7 ± 8.0 cm), the correlation between the VSR (mean = -16.8 ± 6.8 cm) and FFD became moderate (r = -0.572, r2 = .327, p<0.001). Low correlations were identified between the PSLR (mean = 52.7 ° ± 12.7 °) and VSR (r = 0.292, r2 = .085, p = 0.038), the PSLR and FFD (r = -0.297, r2 = .088, p = 0.034), PSLR and AKE (mean = 43.7 ° ± 8.5 °, r = -0.190, r2 = .036, p = 0.183), AKE and VSR (r = -0.208, r2 = .043, p = 0.143), and AKE and FFD (r = 0.101, r2 = .01, p = 0.481).
DISCUSSION
Hamstring tightness is frequently assessed in various populations including pediatrics,4,5,8 active young adults,3,6,9–11 and the elderly.7 The use of the AKE, PSLR, VSR, and FFD to assess hamstring tightness is widespread; however, each of these tests may be measuring the dysfunction utilizing different constructs. If true, this may suggest that the measurements are not able to be used interchangeably when assessing and treating apparent hamstring tightness in clinical practice. The current study is the first that the researchers are aware of to examine the relationships between all four of these assessments.
The strong correlation between the VSR and FFD in this study remained relatively consistent, with r2 shared variance ranging from 34%-64% (Table 2), indicating a substantial portion of the variance in one test is associated with the other. A possible explanation is that both the VSR and FFD involve active trunk and hip flexion. Although the VSR utilizes a seated position (compared to the standing position of the FFD), both are closed kinetic chain assessments that require a patient to flex forward at the waist while also allowing for lumbar flexion. The similar movement pattern between the two tests may explain the shared variance, found between the VSR and FFD, while also explaining the low correlations with either of the “gold standard” AKE and PSLR tests. In weight bearing tests, such as the FFD, it is suggested that a dysfunctional motor control pattern of the postural muscles may present as apparent hamstring tightness.54
Despite being unilateral, non-weight bearing, open kinetic chain assessments that do not have overt trunk flexion components, the AKE and PSLR did not have a similarly strong relationships, with consistently low (∼8%) shared variance being found. The low correlation of r = .284 between the PSLR and AKE found in this study differs from the 0.53-0.72 range reported in previous studies,55,56 but is similar to the values reported by Gajdosik et al.57 A possible explanation may be the populations included in the different studies. The current study utilized a young adult population of at least recreationally active individuals as opposed to adolescents55 or young adults without activity requirements.56 While both the AKE26 and PSLR28 are purported to be the gold standards in the literature for measuring apparent hamstring length, the weak correlation and low shared variance demonstrated in the results of this study suggest that each test is may be measuring different underlying constructs of apparent hamstring tightness.
FACTORS INFLUENCING APPARENT HAMSTRING TIGHTNESS
Sensory Theory
Weppler and Magnusson58 proposed the sensory theory, suggesting that a patient's complaint of “tightness” may be a perception of decreased ROM rather than actual tissue shortening or lack of elongation. Treatments for apparent hamstring tightness (e.g. stretching) focused on increasing tissue extensibility may demonstrate increases in ROM due to an increase in stretch tolerance.
Quadriceps and Hamstrings Coactivation
The active versus passive nature of the AKE and PSLR, respectively, may be another explanation for the low correlation between the two tests; active ROM is typically less than the passive movement available during the same maneuver (e.g., straight leg raise). The AKE requires active contraction of the quadriceps musculature to perform knee extension while maintaining hip flexion, while the PSLR involves passive hip flexion with the knee extended. Quadriceps “weakness” or active insufficiency in combination with a tight hamstring may make the AKE more challenging for patients than PSLR, thus contributing to the low correlation between the two tests.
Lumbopelvic Control
Researchers have suggested that hamstring activation may occur as a stabilizing strategy in individuals with poor lumbopelvic/core control.54 As one function of the hamstrings is to create movement at the hip, the use of the musculature to stabilize the lumbopelvic region would potentially decrease the flexibility of the muscles. While the authors were unable to identify any articles in which hamstring activation was examined in relation to lumbopelvic stabilization, some researchers have discovered a reduction in hamstring stiffness after participants completed exercises designed to improve the stability of the lumbopelvic complex.59,60 In contrast to the AKE and PSLR, the FFD is a test that requires motion at the lumbopelvic complex as the participant forward flexes the trunk. The weak correlation between the AKE and the FFD may represent a discrepancy between laboratory and clinical assessment.
Clinical Application
Interventions used to treat apparent hamstring tightness have had varied results, with some researchers identifying that stretching alone is successful30,61 and others suggesting that lumbopelvic stability is key to treatment.25,62 Additionally, researchers have also suggested that treatment using neurodynamics, in addition or contrast to, stretching or rehabilitation is effective for treating apparent hamstring tightness.63–65 While the AKE is frequently referred to as the “gold standard” in assessing apparent hamstring tightness,26 clinicians will commonly perform other assessments such as a “toe touch” test to identify whether a patient has “tight” hamstrings. As the AKE was not correlated strongly with any of the other tests, the researchers emphasize the questionable use of the test as the stand-alone gold standard for clinical diagnosis of apparent hamstring tightness as it likely measures different constructs than the other assessments. As indicated by the low correlations amongst the majority of these assessments, apparent hamstring tightness is likely a multi-factorial problem and the AKE may not assess all of the associated factors. Thus, there is a potential need for an algorithm to guide decisions on which assessment(s) to utilize. For example, if the clinician utilizes a single assessment for apparent hamstring tightness, other underlying factors (e.g., neural tension, lumbopelvic dysfunction) may go ignored and result in poor patient outcomes. The researchers of the current study suggest that clinicians utilize multiple assessments when evaluating apparent hamstring tightness in order to determine what underlying constructs (e.g., neural tension, lumbopelvic dysfunction) may be involved for each individual patient.
Limitations
All data was collected using a multi-site research approach at five clinical sites to improve study external validity, however this methodology increases the potential for measurement error and reduced internal validity. Thus, intra- and inter-rater reliability was established to minimize variance between researchers
CONCLUSIONS
The results of the current study indicate low correlation and a lack of shared variance amongst the majority of the assessments utilized, suggesting that each assessment may be measuring a different underlying construct of apparent hamstring tightness, such as hamstring muscle length, neural tension, and/or lumbopelvic stability, amongst others. In light of the findings described in this paper, clinicians may wish to consider including a battery of tests in the clinical evaluation of apparent hamstring tightness in order to discover the source of dysfunction and to guide treatment choices based on identified underlying factors.
REFERENCES
- 1.Kendall HO Kendall FP Boynton DA. Posture and Pain. Robert E. Krieger Pub. Co. Inc; New York; 1952. [Google Scholar]
- 2.Holt LE Pelham TE Holt J. Flexibility: A concise guide: to conditioning, performance enhancement, injury prevention, and rehabilitation. Springer Science & Business Media; 2008. [Google Scholar]
- 3.Chandler TJ Kibler WB Uhl TL Wooten B Kiser A Stone E. Flexibility comparisons of junior elite tennis players to other athletes. Am J Sports Med. 1990;18(2):134–136. [DOI] [PubMed] [Google Scholar]
- 4.Gh ME Alilou A Ghafurinia S Fereydounnia S. Prevalence of faulty posture in children and youth from a rural region in Iran. Biomed Hum Kinet. 2012;4. [Google Scholar]
- 5.Józ´wiak M Pietrzak S Tobjasz F. The epidemiology and clinical manifestations of hamstring muscle and plantar foot flexor shortening. Dev Med Child Neurol. 1997;39(7):481-483. [DOI] [PubMed] [Google Scholar]
- 6.Mangine RE Noyes FR Mullen MP Barber SD. A physiological profile of the elite soccer athlete 1. J Orthop Sports Phys Ther. 1990;12(4):147–152. [DOI] [PubMed] [Google Scholar]
- 7.Mollinger LA Steffen TM. Knee flexion contractures in institutionalized elderly: prevalence, severity, stability, and related variables. Phys Ther. 1993;73(7):437-444. [DOI] [PubMed] [Google Scholar]
- 8.Reimers J Brodersen A Pedersen B. The incidence of hamstring shortness in Danish children 3-17 years old. J Pediatr Orthop B. 1993;2(2):173-175. [Google Scholar]
- 9.Weerasekara I. The prevalence of hamstring tightness among the male athletes of University of Peradeniya in 2010, Sri Lanka. Int J Phys Med Rehabil. 2013;01(01). [Google Scholar]
- 10.Worrell TW Perrin DH Gansneder BM Gieck JH. Comparison of isokinetic strength and flexibility measures between hamstring injured and noninjured athletes. J Orthop Sports Phys Ther. 1991;13(3):118–125. [DOI] [PubMed] [Google Scholar]
- 11.Youdas JW Krause DA Hollman JH Harmsen WS Laskowski E. The influence of gender and age on hamstring muscle length in healthy adults. J Orthop Sports Phys Ther. 2005;35(4):246–252. [DOI] [PubMed] [Google Scholar]
- 12.Ekstrand J Gillquist J. Soccer injuries and their mechanisms: a prospective study. Med Sci Sports Exerc. 1983;15(3):267-270. [DOI] [PubMed] [Google Scholar]
- 13.Henderson G Barnes CA Portas MD. Factors associated with increased propensity for hamstring injury in English Premier League soccer players. J Sci Med Sport. 2010;13(4):397-402. [DOI] [PubMed] [Google Scholar]
- 14.Orchard JW Seward H Orchard JJ. Results of 2 decades of injury surveillance and public release of data in the Australian Football League. Am J Sports Med. 2013;41(4):734-741. [DOI] [PubMed] [Google Scholar]
- 15.Arnason A. Risk factors for injuries in football. Am J Sports Med. 2004;32(90010):5S - 16. [DOI] [PubMed] [Google Scholar]
- 16.Brooks JHM. Epidemiology of injuries in English professional rugby union: part 2 training Injuries. Br J Sports Med. 2005;39(10):767-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ekstrand J Healy JC Walden M Lee JC English B Hagglund M. Hamstring muscle injuries in professional football: the correlation of MRI findings with return to play. Br J Sports Med. 2012;46(2):112-117. [DOI] [PubMed] [Google Scholar]
- 18.Feeley BT Kennelly S Barnes RP, et al. Epidemiology of National Football League training camp injuries from 1998 to 2007. Am J Sports Med. 2008;36(8):1597-1603. [DOI] [PubMed] [Google Scholar]
- 19.Liu H Garrett WE Moorman CT Yu B. Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J Sport Health Sci. 2012;1(2):92-101. [Google Scholar]
- 20.Verrall GM Kalairajah Y Slavotinek JP Spriggins AJ. Assessment of player performance following return to sport after hamstring muscle strain injury. J Sci Med Sport. 2006;9(1–2):87-90. [DOI] [PubMed] [Google Scholar]
- 21.Bradley PS Portas MD. The relationship between preseason range of motion and muscle strain injury in elite soccer players. J Strength Cond Res. 2007;21(4):1155–1159. [DOI] [PubMed] [Google Scholar]
- 22.Witvrouw E Danneels L Asselman P D’Have T Cambier D. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players a prospective study. Am J Sports Med. 2003;31(1):41–46. [DOI] [PubMed] [Google Scholar]
- 23.Fyfe JJ Opar DA Williams MD Shield AJ. The role of neuromuscular inhibition in hamstring strain injury recurrence. J Electromyogr Kinesiol. 2013;23(3):523-530. [DOI] [PubMed] [Google Scholar]
- 24.Turl SE George KP. Adverse neural tension: a factor in repetitive hamstring strain? J Orthop Sports Phys Ther. 1998;27(1):16-21. [DOI] [PubMed] [Google Scholar]
- 25.Hoskins W Pollard H. The effect of a sports chiropractic manual therapy intervention on the prevention of back pain, hamstring and lower limb injuries in semi-elite Australian Rules footballers: a randomized controlled trial. BMC Musculoskelet Disord. 2010;11(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 26.Gajdosik R Lusin G. Hamstring muscle tightness reliability of an active-knee-extension test. Phys Ther. 1983;63(7):1085-1088. [DOI] [PubMed] [Google Scholar]
- 27.Davis DS Quinn RO Whiteman CT Williams JD Young CR. Concurrent validity of four clinical tests used to measure hamstring flexibility. J Strength Cond Res. 2008;22(2):583–588. [DOI] [PubMed] [Google Scholar]
- 28.Bohannon RW. Cinematographic analysis of the passive straight-leg-raising test for hamstring muscle length. Phys Ther. 1982;62(9):1269–1274. [DOI] [PubMed] [Google Scholar]
- 29.Cook G. Movement: Functional Movement Systems: Screening, Assessment, and Corrective Strategies. Santa Cruz, CA: On Target Publications; 2010. [Google Scholar]
- 30.DePino GM Webright WG Arnold BL. Duration of maintained hamstring flexibility after cessation of an acute static stretching protocol. J Athl Train. 2000;35(1):56-59. [PMC free article] [PubMed] [Google Scholar]
- 31.Kang MH Jung DH An DH Yoo WG Oh JS. Acute effects of hamstring-stretching exercises on the kinematics of the lumbar spine and hip during stoop lifting. J Back Musculoskelet Rehabil. 2013;26(3):329-336. [DOI] [PubMed] [Google Scholar]
- 32.Mhatre BS Singh YL Tembhekar JY Mehta A. Which is the better method to improve “perceived hamstrings tightness” – Exercises targeting neural tissue mobility or exercises targeting hamstrings muscle extensibility? Int J Osteopath Med. 2013;16(3):153-162. [Google Scholar]
- 33.Spernoga SG Uhl TL Arnold BL Gansneder BM. Duration of maintained hamstring flexibility after a one-time, modified hold-relax stretching protocol. J Athl Train. 2001;36(1):44-48. [PMC free article] [PubMed] [Google Scholar]
- 34.Cameron DM Bohannon RW. Relationship between active knee extension and active straight leg raise test measurements. J Orthop Sports Phys Ther. 1993;17(5):257–260. [DOI] [PubMed] [Google Scholar]
- 35.Reurink G Goudswaard GJ Oomen HG, et al. Reliability of the active and passive knee extension test in acute hamstring injuries. Am J Sports Med. 2013;41(8):1757-1761. [DOI] [PubMed] [Google Scholar]
- 36.de Weijer VC Gorniak GC Shamus E. The effect of static stretch and warm-up exercise on hamstring length over the course of 24 hours. J Orthop Sports Phys Ther. 2003;33(12):727-733. [DOI] [PubMed] [Google Scholar]
- 37.Kuilart KE Woollam M Barling E Lucas N. The active knee extension test and Slump test in subjects with perceived hamstring tightness. Int J Osteopath Med. 2005;8(3):89-97. [Google Scholar]
- 38.Norris C Matthews M. Inter-tester reliability of a self-monitored active knee extension test. J Bodyw Mov Ther. 2005;9(4):256-259. [Google Scholar]
- 39.Kendall FP McCreary E Provance PG Rodgers MM Romani WA. Muscles: Testing and Function with Posture and Pain. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- 40.Gabbe BJ Bennell KL Wajswelner H Finch CF. Reliability of common lower extremity musculoskeletal screening tests. Phys Ther Sport. 2004;5(2):90-97. [Google Scholar]
- 41.Hui SS Yuen PY. Validity of the modified back-saver sit-and-reach test: a comparison with other protocols. Med Sci Sports Exerc. 2000;32(9):1655-1659. [DOI] [PubMed] [Google Scholar]
- 42.Miñarro PAL Andújar PS de B García PLR Toro EO. A comparison of the spine posture among several sit-and-reach test protocols. J Sci Med Sport. 2007;10(6):456-462. [DOI] [PubMed] [Google Scholar]
- 43.Cuberek R Machova I Lipenska M. Reliability of V sit-and-reach test used for flexibility self-assessment in females. Acta Gymnica. January 2013:35-39. [Google Scholar]
- 44.López-Miñarro PA de Baranda Andújar PS RodrÑGuez-GarcÑa PL. A comparison of the sit-and-reach test and the back-saver sit-and-reach test in university students. J Sports Sci Med. 2009;8(1):116. [PMC free article] [PubMed] [Google Scholar]
- 45.Kippers V Parker AW. Toe-touch test: a measure of its validity. Phys Ther. 1987;67(11):1680-1684. [DOI] [PubMed] [Google Scholar]
- 46.Perret C Poiraudeau S Fermanian J Colau MML Benhamou MAM Revel M. Validity, reliability, and responsiveness of the fingertip-to-floor test. Arch Phys Med Rehabil. 2001;82(11):1566–1570. [DOI] [PubMed] [Google Scholar]
- 47.Garber CE Blissmer B Deschenes MR, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 2011;43(7):1334-1359. [DOI] [PubMed] [Google Scholar]
- 48.Werner BC Holzgrefe RE Griffin JW, et al. Validation of an innovative method of shoulder range-of-motion measurement using a smartphone clinometer application. J Shoulder Elbow Surg. 2014;23(11):e275-e282. [DOI] [PubMed] [Google Scholar]
- 49.Cox RW Martinez RE Baker RT Larkins LW. Validity of a smartphone application for measuring ankle plantar flexion. J Sport Rehabil. 2017:1-11. [DOI] [PubMed] [Google Scholar]
- 50.Huang SY Di Santo M Wadden KP Cappa DF Alkanani T Behm DG. Short-duration massage at the hamstrings musculotendinous junction induces greater range of motion. J Strength Cond Res. 2010;24(7):1917-1924. [DOI] [PubMed] [Google Scholar]
- 51.Weir JP. Quantifying test-retest reliability using the intraclass correlation coefficient and the SEM. J Strength Cond Res. 2005;19(1):231–240. [DOI] [PubMed] [Google Scholar]
- 52.Hurley WL Denegar CR Hertel J. Research Methods: A Framework for Evidence-Based Clinical Practice. 1st ed. Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins Health; 2011. [Google Scholar]
- 53.Streiner DL Norman GR Cairney J. Health Measurement Scales: A Practical Guide to Their Development and Use. Oxford University Press; 2014. [Google Scholar]
- 54.Loutsch RA Baker RT May JM Nasypany AM. Reactive neuromuscular training results in immediate and long term improvements in measures of hamstring flexibility: a case report. Int J Sports Phys Ther. 2015;10(3):371. [PMC free article] [PubMed] [Google Scholar]
- 55.Hartman JG Looney M. Norm-referenced and criterion-referenced reliability and validity of the back-saver sit-and-reach. Meas Phys Educ Exerc Sci. 2003;7(2):71-87. [Google Scholar]
- 56.López-Miñarro P Sáinz de Baranda P Rodríguez-García P Yuste J. Comparison between sit-and-reach test and V sit-and-reach test in young adults. Gazz Med Ital. 2008;167:135-142. [Google Scholar]
- 57.Gajdosik RL Rieck MA Sullivan DK Wightman SE. Comparison of four clinical tests for assessing hamstring muscle length. J Orthop Sports Phys Ther. 1993;18(5):614-618. [DOI] [PubMed] [Google Scholar]
- 58.Weppler CH Magnusson SP. Increasing Muscle Extensibility: A Matter of Increasing Length or Modifying Sensation? Phys Ther. 2010;90(3):438-449. [DOI] [PubMed] [Google Scholar]
- 59.Kuszewski M Gnat R Saulicz E. Stability training of the lumbo-pelvo-hip complex influence stiffness of the hamstrings: a preliminary study. Scand J Med Sci Sports. 2009;19(2):260-266. [DOI] [PubMed] [Google Scholar]
- 60.Phrompaet S Paungmali A Pirunsan U Sitilertpisan P. Effects of pilates training on lumbo-pelvic stability and flexibility. Asian J Sports Med. 2011;2(1):16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Davis DS Ashby PE McCale KL Mcquain JA Wine JM. The effectiveness of three stretching techniques on hamstring flexibility using consistent stretching parameters. J Strength Cond Res. 2005;19(1):27–32. [DOI] [PubMed] [Google Scholar]
- 62.Sherry MA Best TM. A comparison of 2 rehabilitation programs in the treatment of acute hamstring strains. J Orthop Sports Phys Ther. 2004;34(3):116–125. [DOI] [PubMed] [Google Scholar]
- 63.Castellote-Caballero Y Valenza MC Puentedura EJ Fernández-de-las-Peñas C Alburquerque-Sendín F. Immediate effects of neurodynamic sliding versus muscle stretching on hamstring flexibility in subjects with short hamstring syndrome. J Sports Med. 2014;2014:1-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Castellote-Caballero Y Valenza MC Martín-Martín L Cabrera-Martos I Puentedura EJ Fernández-de-las-Peñas C. Effects of a neurodynamic sliding technique on hamstring flexibility in healthy male soccer players. A pilot study. Phys Ther Sport. 2013;14(3):156-162. [DOI] [PubMed] [Google Scholar]
- 65.Kornberg C Lew P. The effect of stretching neural structures on grade one hamstring injuries. J Orthop Sports Phys Ther. 1989;10(12):481-487. [DOI] [PubMed] [Google Scholar]