Abstract
Over the last 2 decades, there have been a number of changes in clinical practice that individually could affect the outcome of allogeneic hematopoietic cell transplantation (HCT), but until recently the collective impact of these changes was unknown. Accordingly, several groups asked the question of whether the outcome of allogeneic HCT has improved, and if so, why. Four large studies including a total of more than 10,000 patients have been performed and have reached very similar conclusions. Compared to transplants performed in the 1990s, the hazard ratio for nonrelapse mortality for transplants performed in the 2000s was roughly 0.5. This remarkable improvement was seen when the analyses were restricted to myeloablative transplants, to recipients of marrow rather than peripheral blood, or to transplants from matched siblings, and persisted after analyses were adjusted for patient risk. Likely explanations for this improvement include the avoidance of the most toxic preparative regimens, use of agents that spare hepatic and renal function, and improved methods for control of infections.
Keywords: allogeneic HCT, hematopoietic cell transplantation (HCT), marrow, matched sibling, myeloablative, nonrelapse mortality, peripheral blood, transplant-related mortality
Introduction
Our perceptions of the toxicity and efficacy of various therapies are often based on studies that are decades old. In the case of allogeneic hematopoietic cell transplantation, the majority of the comparative trials included in the evidence-based reviews to reach conclusions about indications for transplantation were performed in the 1990s [1–3]. There have been a number of changes in clinical practice that could each potentially affect the outcome of transplantation, but until recently, the collective impact of these advances was unknown. Accordingly, several groups have asked the question of whether the outcome of allogeneic hematopoietic cell transplantation (HCT) has improved, and if so, why.
Recent comparative studies
Seattle
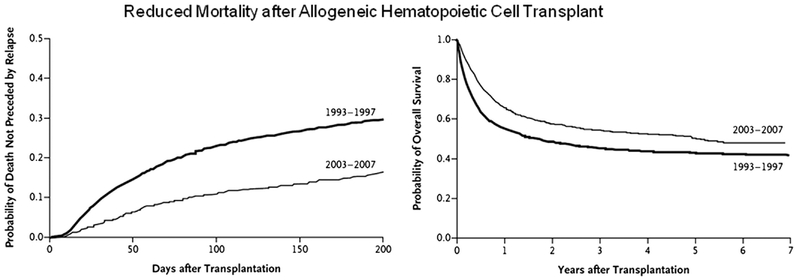
In 2010, the Seattle group published a study in which they compared the outcome of allogeneic HCT among 1418 patients transplanted between 1993 and 1997 with that of 1148 patients transplanted a decade later, from 2003–2207 [4]. As shown in Figure 1, the nonrelapse mortality (NRM) during the first 200 days post transplant was almost halved (from 30% to 16%) in the more recent cohort, and overall survival improved from 37% to 53%. These results were also analyzed after adjusting for possible differences in severity of illness at the time of transplant using the Pretransplant Assessment of Mortality (PAM) score [5]. Because the more recent cohort was, in general, older and had more advanced disease, the improvements over time were more striking than in the unadjusted data. As shown in Table 1, the hazard ratio for 200 day NRM was 0.40 (P<0.001) in the more recent cohort, and the hazard for overall mortality was 0.59 P<0.001).
Figure 1.
The figure on the left shows the probability of death not preceded by relapse, and the figure on the right shows overall survival for patients receiving allogeneic HCT in Seattle from 1993–1997 (n=1418) and 2003–2007 (n=1148) [4]. From New England Journal of Medicine, Gooley TA, Chien JW, Pergam SA, et al, Reduced mortality after allogeneic hematopoietic-cell transplantation. Volume 363, Page 2098, Copyright © 2010 Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
Table 1.
Outcome of Allogeneic Transplantation in Two Eras.
| Event | 1993–7 (N=1418) | 2003–7 (N=1148) | Adjusted HR |
|---|---|---|---|
| D200 NRM | 30% | 16% | 0.40 (P<0.001) |
| Overall NRM | 41% | 26% | 0.48 (P<0.001) |
| Relapse | 27% | 26% | 0.79 (P=0.008) |
| Overall mortality | 63% | 47% | 0.59 (P<0.001) |
In an effort to gain further insight into the possible reasons for these overall improvements, the frequencies of various life-threatening toxicities over time were examined. As shown in Table 2, the incidence of severe hepatic, renal, and pulmonary disease all were markedly diminished over the more recent era. Similarly, the frequencies of viral, bacterial and mold infections have all markedly diminished, as has the frequency of several acute graft-versus-host disease (GVHD).
Table 2.
Outcome of Allogeneic Transplantation in Two Eras.
| Event | 1993–7 (N=1418) | 2003–7 (N=1148) | Adjusted HR |
|---|---|---|---|
| Bilirubin > 10 | 20% | 6% | 0.24 (P<0.001) |
| Creatinine ↑ x 3 | 18% | 10% | 0.51 (P<0.001) |
| Respiratory failure | 15% | 11% | 0.69 (P=0.007) |
| CMV disease | 8% | 5% | 0.53 (P=0.02) |
| Gram negative bacteremia | 15% | 11% | 0.57 (P<0.001) |
| Mold infection | 9% | 7% | 0.55 (P<0.001) |
| Grade III/IV aGVHD | 30% | 14% | 0.33 (P<0.001) |
When specific subpopulations of patients were examined, the same general trend towards improvement over time was seen. Specifically, the magnitude of improved nonrelapse mortality and survival was seen in each disease category (acute myeloid leukemia [AML], acute lymphocytic leukemia, and myelodysplasia), and in those with low and high PAM scores. There was no difference in the magnitude of improvement over time in those receiving transplants from matched related donors and in those receiving mismatched or unrelated transplants. Finally, our results were similar when the analyses were limited to patients who received myeloablative conditioning therapy.
Stockholm
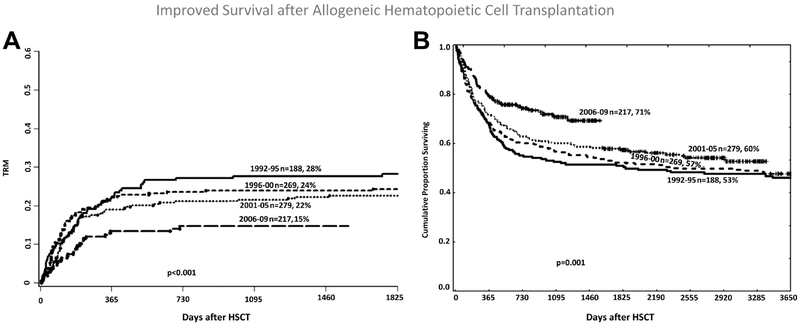
Several other groups have conducted studies similar in form to the one from Seattle. The group from the Karolinska Institute in Stockholm analyzed the outcome of allogeneic HCT in 953 patients transplanted from 1992 through 2009 [6]. They divided the group into four different time periods: 1992 to 1995, 1996 to 2000, 2001 to 2005, and 2006 to 2009. Similar to the Seattle study, nonrelapse mortality significantly diminished and overall survival improved in the more recent cohorts (see Figure 2). These improvements were seen both in the raw data and after correcting for apparent differences in the patient cohorts. In multivariate analysis, the hazard ratio for overall mortality in the last period was 0.59 (P<0.001) compared to earlier periods, and the risk of nonrelapse mortality was 0.63 (P= 0.02).
Figure 2.
Shown are the cumulative probabilities of nonrelapse mortality (on the left) and overall survival (on the right) for patients transplanted in Stockholm over 4 different time periods [6]. Reprinted from Biology of Blood and Marrow Transplantation, Vol 17/Issue 11, Remberger M, Ackefors M, Berglund S, et al, Improved survival after allogeneic hematopoietic stem cell transplantation in recent years. A single-center study, Pages 1688–1697, Copyright 2011, with permission from Elsevier.
Eastern Europe
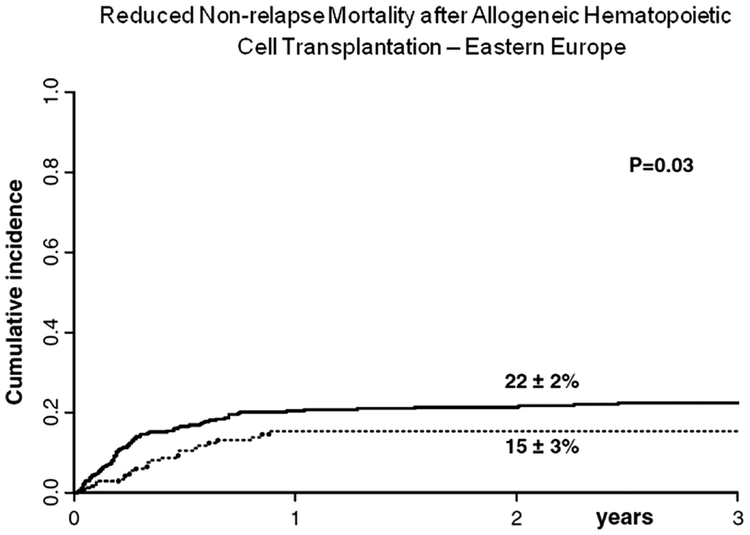
In a registry study, the European Group for Blood and Marrow Transplantation examined the outcome of allogeneic HCT for acute leukemia in Eastern European countries [7]. Among 640 patients transplanted in first remission, the 2-year leukemia-free survival, nonrelapse mortality, and relapse incidence were 58%, 19%, and 23%, respectively. The cumulative incidence of nonrelapse mortality decreased from 22% among the 377 patients treated prior to 2003 to 15% for those transplanted from 2003–2006 (P=0.02) (see Figure 3). In multivariate analysis, the risk of nonrelapse mortality was 0.58 in the more recently transplanted cohort.
Figure 3.
The curves show the cumulative incidence of nonrelapse mortality in patients receiving allogeneic transplantation between 1990 and 2002 (solid line) and 2003–2006 (dotted line) [7]. With kind permission from Springer Science and Business Media.
Center for International Blood and Marrow Transplant Research (CIBMTR)
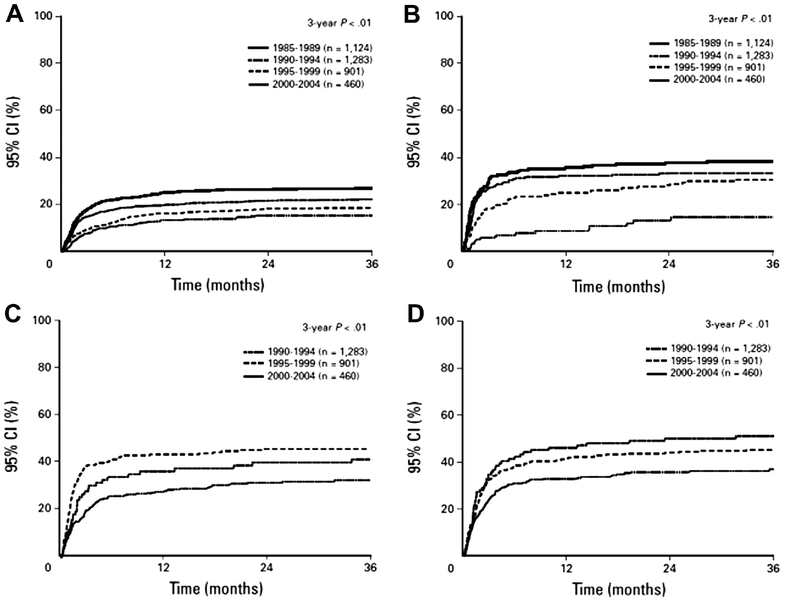
The CIBMTR recently published an analysis of 5972 patients younger than age 50 years who received myeloablative conditioning and allogeneic HCT for AML in first or second complete remission [8]. Similar to the Stockholm report, they compared outcomes in four cohorts, those transplanted from 1985–1989 (n=1124), 1990–1994 (n=1283), 1995–1999 (n=901), and 2000–2004 (n=400). Among HLA-matched sibling donor HCT recipients, the hazard for death from a complication of transplant was 0.5 and 0.3 for the 2000–2004 cohort compared to the 1985–1989 cohort for patients transplanted in CR1 and CR2, respectively (P<0.001). Among unrelated donor recipients, the hazards were 0.73 and 0.58 for the 2000–2004 cohort compared to the 1990–1994 cohort in the CR1 and CR2 groups respectively (see Figure 4). These reductions in transplant-related deaths led to reductions in all-cause mortality in the more recent transplant populations.
Figure 4.
Transplanted-related mortality by 5 year periods for 4 subgroups is shown: (A) Recipients of HLA-matched related donor transplants in first CR, (B) Recipients of HLA-matched related transplants in second CR, (C) Recipients of unrelated donor transplants in first CR, and (D) Recipients of unrelated donor transplants in second CR [8]. Reprinted with permission. © 2011 American Society of Clinical Oncology. All rights reserved.
After adjusting for changes in patient and disease characteristics over time, a multivariate analysis confirmed the significant reduction in transplant-related mortality among matched siblings transplanted in first or second remission (0.5 and 0.25 respectively, P<0.001 for both). For recipients of unrelated donor transplants, the hazard ratios for CR1 and CR2 patients in the most recent cohorts were 0.73 and 0.58 (P=0.09 and <0.001).
The reductions in transplant-related mortality were similar when the analysis was restricted to patients under age 20 years or age 20 years and older, to those who received bone marrow as the source of stem cells, or to those who received cyclosporine and methotrexate as GVHD prophylaxis.
Aggregate results
Table 3 lists the changes in nonrelapse mortality risk found in each of these four large studies. The overall hazard ratios of death from a transplant complication range from 0.48 to 0.59 in the most recent cohorts compared to those transplants performed approximately a decade earlier.
Table 3.
Changes in Non-relapse Mortality Risk.
| Study | Comparison | Hazard Ratio |
|---|---|---|
| Seattle | 1993–7 vs 2003–7 | 0.48 |
| Stockholm | 1992–5 vs 2006–9 | 0.59 |
| Eastern Europe | 1990–2 vs 2003–6 | 0.59 |
| CIBMTR | 1985–9 vs 2000–4 | 0.50 |
Possible but at best minor explanations for the recent reduction in mortality
The decrease in nonrelapse mortality associated with allogeneic HCT seen over the last 2 decades is inarguable, but the reasons for it are less clear. A number of explanations come to mind that at first seem plausible but on closer examination are at best minor contributors. These include the increased use of reduced intensity transplant preparative regimens, advances in HLA typing, improved patient selection for allogeneic HCT, and increased use of mobilized peripheral blood as the source of stem cells for transplantation.
While the development of nonablative and reduced intensity transplant preparative regimens have been a major advance allowing for the application of a curative therapy for older patients and those with significant comorbidities, they are not the explanation for the reduction in transplant-related mortality seen over the last 2 decades in the studies referenced above. In the Seattle study, the reduction in nonrelapse mortality was equally impressive when the analysis was restricted to recipients of ablative preparative regimens. While the isolated impact of reduced intensity regimens was not stated in the Stockhom study, only a minority of patients were treated using them. Similarly, only 10% of the patients in the Eastern European study were treated with reduced intensity conditioning, and most convincingly, the entire CIBMTR study was limited to patients who received myeloablative conditioning regimens.
Prior to 1998, HLA-typing for donor selection largely relied on serologic methods incapable of identifying all HLA subtypes (low resolution typing). More recent studies using automated direct sequencing of HLA-A, HLA-B, HLA-C, HLA-DRB1, and HLA-DQ and HLA-DP (high resolution typing) demonstrate that approximately 30% of serologically matched unrelated donors are mismatched for one or more alleles. Thus, it could be argued that some of the recent improvement in transplant outcome might be due to improved donor selection. However, the magnitude of improvement in nonrelapse mortality seen in the more recent era was just as striking in recipients of matched sibling transplants, where molecular typing offers no advantage over serologic typing. In the Seattle study, the hazard ratio for nonrelapse mortality by day 200 in the most recent cohort compared to that of a decade ago was 0.45 for recipients of matched sibling HCT and 0.35 for recipients of unrelated transplants. In the CIBMTR study, the hazard of nonrelapse mortality in the more recent groups transplanted in CR1 were 0.5 with matched siblings and 0.73 for recipients of unrelated transplants.
Patient selection could play a role in the improved outcomes seen more recently. Each of the four studies cited above did make efforts to account for patient selection. The Seattle study presented outcomes both unadjusted and after making adjustments for severity of illness at the time of transplant using the PAM score. The other three studies all presented both univariate and multivariate analyses. The general observations of all four studies were that our more recent transplant populations are older and have more advanced disease. Thus, the degree of improvement in transplant-related mortality seen in recent results is even greater once adjustments are made for patient selection.
In 2001/2002, the results of the first prospective randomized trials comparing bone marrow and mobilized peripheral blood as a source of stem cells for allogeneic HCT from matched related donors were published [9,10]. These studies suggested a survival advantage with the use of mobilized peripheral blood, a finding that has affected standard practice and possibly could account for some of the recent improvements in nonrelapse mortality. Arguing against this possibility are that in the Eastern European and CIBMTR studies, which looked explicitly at this question, the reduction in transplant-related mortality was equally striking in the bone marrow and peripheral blood groups. Further, a recent randomized trial failed to find a survival difference between bone marrow and peripheral blood in the setting of unrelated donor transplantation [11].
Some likely reasons for reduced mortality with allogeneic HCT
As noted above, the increased use of reduced-intensity conditioning is not a direct explanation for the recent reduced mortality seen with allogeneic HCT, since similar improvements were seen when studies were restricted to myeloablative transplants. However, it is likely that the relative success of reduced-intensity conditioning has influenced the development and choice of myeloablative conditioning. In Seattle, for example, in the cohort transplanted from 1993–1997, 70% were treated with high-dose myeloablative regimens, defined as regimens that included cyclophosphamide (Cy) and more than 12 Gy total body irradiation (TBI) or Cy with nontargeted busulfan (Bu). A decade later, only 10% of our patients received such regimens; the large majority were instead treated with Cy and 12 Gy TBI or targeted Bu plus Cy. Unfortunately, insufficient details were available from the other studies to reach conclusions about the impact of preparative regimen choice, but it seems at least possible, if not highly likely, that avoidance of the most intensive preparative regimens combined with individualized dosing of Bu has contributed to the improved safety of allogeneic HCT.
Severe liver dysfunction is now much less common following allogeneic HCT, and grade IV hepatic GVHD has all but disappeared. Based on observations that ursodiol improves the results of liver function tests in patients with GVHD, reduces the frequency of jaundice, and improves survival after transplantation, ursodiol prophylaxis has been broadly adopted and likely makes at least a small contribution to recent improvements in transplant outcome[12].
Likely, the greatest contribution to improved outcomes in recent years is improvements in the control of infections, particularly fungal disease. Fluconazole prophylaxis prevents fungal infections and improves overall survival [13]. And the availability of mold-active azoles and echinocandins means that invasive Aspergillus infections, previously almost universally fatal, can now sometimes be cured. Thus, the hazard ratios for Candida and mold infections in the most recent era compared to a decade earlier are 0.15 and 0.55 in the Seattle study. A further benefit in the availability of these agents is the avoidance of amphotericin products, thereby sparing renal function. The risk of CMV disease has also decreased in the more recent era, with a hazard ratio of 0.53 compared to a decade earlier in the Seattle experience. Since ganciclovir was available over both time periods, the likely explanation for this drop is the development of more sensitive diagnostic testing for CMV viremia, allowing for more effective preemptive therapy. The drop in the risk for gram-negative bacteremia in more recent times may be due to a switch in bacterial prophylaxis from cephalosporins to quinolones, at least in our experience.
Conclusions
Based on the four large studies described above, the evidence is overwhelming that the risk of transplant-related mortality following allogeneic HCT has reduced dramatically over the last 2 decades, dropping approximately in half. Avoidance of the most toxic preparative regimens, use of agents that spare hepatic and renal function, and the development of improved methods to control infections are some of the steps that have contributed to this advance. Other less obvious advances probably also contribute but are more difficult to isolate. All of us who have been involved in the field of allogeneic HCT should celebrate, at least a little, over these findings. These results also imply that prior studies comparing the outcome of transplantation to other modalities may need to be revisited. Finally, while there has been considerable progress made in reducing transplant-related mortality, advances in reducing the risk of relapse after transplant have been much less apparent, and this problem now deserves most of our attention.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement:
Consulting fees: SuperGen (Astex Pharmaceuticals); Celator; Igenica.
References
- [1].Oliansky DM, Appelbaum F, Cassileth PA, et al. The role of cytotoxic therapy with hematopoietic stem cell transplantation in the therapy of acute myelogenous leukemia in adults: an evidence-based review. Biol Blood Marrow Transplant 2008;14:137–180. [DOI] [PubMed] [Google Scholar]
- [2].Yanada M, Matsuo K, Emi N, Naoe T. Efficacy of allogeneic hematopoietic stem cell transplantation depends on cytogenetic risk for acute myeloid leukemia in first disease remission: a metaanalysis. Cancer 2005;103(8):1652–1658. [DOI] [PubMed] [Google Scholar]
- [3].Koreth J, Schlenk R, Kopecky KJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: a systematic review and meta-analysis of prospective clinical trials. JAMA 2009;301(22):2349–2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Gooley TA, Chien JW, Pergam SA, et al. Reduced mortality after allogeneic hematopoietic-cell transplantation. N Engl J Med 2010;363(22):2091–2101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Parimon T, Au DH, Martin PJ, Chien JW. A risk score for mortality after allogeneic hematopoietic cell transplantation. Ann Intern Med 2006;144(6):407–414. [DOI] [PubMed] [Google Scholar]
- [6].Remberger M, Ackefors M, Berglund S, et al. Improved survival after allogeneic hematopoietic stem cell transplantation in recent years. A single-center study. Biol Blood Marrow Transplant 2011;17(11):1688–1697. [DOI] [PubMed] [Google Scholar]
- [7].Giebel S, Labopin M, Holowiecki J, et al. Outcome of HLA-matched related allogeneic hematopoietic stem cell transplantation for patients with acute leukemia in first complete remission treated in Eastern European centers. Better results in recent years. Ann Hematol 2009;88(10):1005–1013. [DOI] [PubMed] [Google Scholar]
- [8].Horan JT, Logan BR, Agovi-Johnson MA, et al. Reducing the risk for transplantation-related mortality after allogeneic hematopoietic cell transplantation: how much progress has been made? J Clin Oncol 2011;29(7):805–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Bensinger WI, Martin PJ, Storer B, et al. Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers. N Engl J Med 2001;344(3):175–181. [DOI] [PubMed] [Google Scholar]
- [10].Couban S, Simpson DR, Barnett MJ, et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood 2002;100(5):1525–1531. [DOI] [PubMed] [Google Scholar]
- [11].Anasetti C, Logan BR, Lee SJ, et al. Increased incidence of chronic graft-versus-host disease (GVHD) and no survival advantage with filgrastim-mobilized peripheral blood stem cells (PBSC) compared to bone marrow (BM) transplants from unrelated donors: results of Blood and Marrow Transplant Clinical Trials Network (BMT CTN) protocol 0201, a phase III, prospective, randomized trial [abstract]. Blood. 2011;118(21):#1 [Google Scholar]
- [12].Ruutu T, Eriksson B, Remes K, et al. Ursodeoxycholic acid for the prevention of hepatic complications in allogeneic stem cell transplantation. Blood 2002;100(6):1977–1983. [DOI] [PubMed] [Google Scholar]
- [13].Marr KA, Seidel K, Slavin M, et al. Prolonged fluconazole prophylaxis is associated with persistent protection against candidiasis-related death in allogeneic marrow transplant recipients: long-term follow-up of a randomized, placebo-controlled trial. Blood 2000;96(6):2055–2061. [PubMed] [Google Scholar]