Abstract
Background
The Global Viral Hepatitis Strategy aims to eliminate hepatitis as a public health threat by 2030. The hepatitis C virus (HCV) can be difficult to detect as infection can remain asymptomatic for decades. Individuals are often neither offered nor seek testing until symptoms develop. This highlights the importance of increasing awareness and knowledge among health care providers and the public to reach the viral hepatitis goals.
Objectives
To conduct a scoping review to characterize current awareness and knowledge among health care providers and the public regarding HCV infection, transmission, prevention and treatment and to identify knowledge gaps that public health action could address.
Methods
A literature search was conducted using Embase, Medline and Scopus to find studies published between January 2012 and July 2017. A search for grey literature was also undertaken. The following data were extracted: author, year of publication, study design, population, setting, country, method of data collection, and knowledge and awareness outcomes. Commentaries, letters to the editor and narrative reviews were excluded.
Results
Nineteen studies were included in this review. The definition of awareness and knowledge varied across studies; at times, these terms were used interchangeably. Health care providers identified injection drug use or blood transfusions as routes of HCV transmission more frequently than other routes of transmission such as tattooing with unsterile equipment and sexual transmission. Among the general public, misconceptions about HCV included believing that kissing and casual contact were routes of HCV transmission and that a vaccine to prevent HCV was available. Overall, there was a lack of data on other high-risk populations (e.g., Indigenous, incarcerated).
Conclusion
Continued public and professional education campaigns about HCV could help support HCV risk-based screening and testing. Future research could assess the awareness of other populations at increased risk and include consistent definitions of awareness and knowledge.
Keywords: awareness, knowledge, hepatitis C, scoping review, health care providers
Background
Hepatitis C virus (HCV) causes inflammation of the liver, which can become chronic. Chronic HCV infection can be asymptomatic for decades before symptoms appear. Globally, about 71 million people have chronic HCV infection (1). Chronic HCV infection is not easy to detect; even when symptoms are present, they are often nonspecific (e.g., fatigue) (2). Chronic HCV infection can lead to cirrhosis or liver cancer. Approximately half a million people die each year from HCV-related liver diseases (3).
In 2011, about 220,000-246,000 individuals were living with chronic HCV infection in Canada and approximately 44% were unaware of their infection (4). Over the past few years, there have been significant advances in HCV treatment, and infection is now curable. Previous treatment regimens consisted of peg-interferon and ribavirin, which involved longer treatment durations and more side effects. The new interferon-free direct acting antiviral (DAA) treatments have been found to be highly effective and have fewer side effects. Currently, most provincial and territorial formularies cover these new treatments and Canada has started to witness a decrease in hospitalizations associated with HCV infection and chronic liver disease (5).
In 2016, the 69th World Health Assembly adopted the Global Health Sector Strategy on Viral Hepatitis with the goal of eliminating both hepatitis B and C as a public health threat by 2030 (6). The goal is to have 90% of viral hepatitis B and C diagnosed and 80% of eligible people with chronic hepatitis B virus (HBV) and chronic HCV infection treated (6). Awareness and knowledge of hepatitis C is an important first step in the elimination strategy. The identification of HCV through screening and testing is essential for patients to make appropriate lifestyle changes and to begin treatment.
Limited awareness of and knowledge about HCV have been identified as the key barriers to health care providers offering hepatitis C testing and for patients seeking testing (7). This lack of awareness and knowledge leads to continued HCV transmission and missed prevention and treatment opportunities. In an effort to improve risk-based screening in Canada and to reduce the number of people who are unaware of their infection, it is important to understand current awareness and knowledge of HCV among health care providers and the public alike.
The objectives of this review are to summarize health care providers’ and the general public’s awareness and knowledge of the natural history of HCV and HCV transmission, prevention and treatment, and to identify knowledge gaps in both groups that public health action could address.
Methods
We worked with a research librarian to conduct a literature search in Embase, Medline and Scopus for published studies on awareness and knowledge of HCV among health care providers and the public. We also completed a search for grey literature (i.e., reports available on public domains) using Google. The following search terms were used: hepatitis C, HCV, awareness, and knowledge. Studies were included in the review if they were published between January 2012 and July 2017; published in English or French; conducted in Canada or similarly economically developed and well-resourced countries; and focused on the public or health care providers. We restricted the search years to the last five years to capture the most recent information. Commentaries, letters to editors and case studies were excluded. Outcomes of interest included HCV awareness and knowledge, which are defined in various ways based on the study.
After screening the titles and abstracts of potentially relevant articles, we reviewed the full texts of included studies. We developed data extraction forms and extracted data on the following: author, year of publication, study design, population, setting, country, method of data collection, and knowledge and awareness outcomes.
As a scoping review a qualitative analysis of the findings was completed and the results were summarized into themes but we did not conduct a detailed assessment of overall quality or risk of bias.
Results
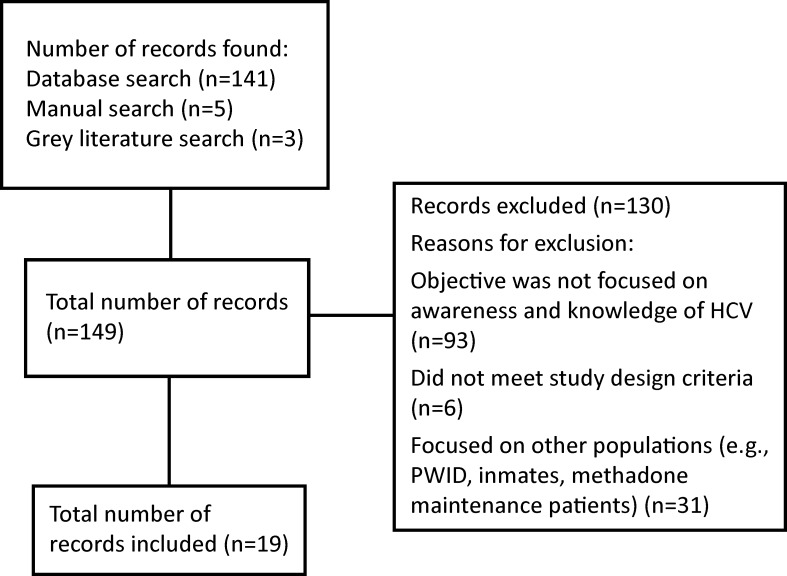
The literature search identified 141 potentially relevant articles on HCV awareness and knowledge of health care providers and the general public. A manual search of the reference lists identified five additional references. An additional three reports were identified through the grey literature search. After the title and abstract screening and the full text review, 19 studies were included in this review (Figure 1).
Figure 1. Flowchart of study selection process.
Abbreviations: HCV, hepatitis C virus; n, number; PWID, people who inject drugs
Awareness and knowledge were at times used interchangeably in the included studies. Awareness was defined as either awareness of one’s own HCV infection, diagnosis or seropositivity or awareness of the existence of HCV, the risk factors or availability of treatment. Knowledge could include the natural history and consequences of HCV, HCV risk factors and transmission routes, or vaccine and treatment availability. Consequently, the results are reported based on how the studies themselves defined awareness and knowledge.
Characteristics of included studies
The majority of the included studies were conducted in the United States (US; n=8), followed by Canada (n=5) and Australia (n=3). The remainder of the studies were from Germany, Italy, Japan and Netherlands. Most of the studies (n=13) targeted the general population and less than one-third (n=5) focused on health care providers; one study included both populations. Participants were recruited from a variety of settings including hospitals, outpatient clinics, primary care clinics, emergency departments and online panels. Data collection methods most often included questionnaires completed online, in-person or by phone. (For more details about the included studies, please refer to Appendix 1.)
Of the studies that focused on health care providers, job categories included physicians, nurses, residents, dental students and specialists (i.e., hepatologists and gastroenterologists). Of the studies that focused on non–health care providers, population groups included HCV-infected people with or without HIV coinfection, men who have sex with men (MSM), immigrants, the general public and adults born between 1945 and 1965 (Table 1).
Table 1. Summary of included studies.
| Characteristics | Number of studies (n)a |
|---|---|
| Country | |
| US | 8 |
| Canada | 5 |
| Australia | 3 |
| Netherlands | 2 |
| Germany | 1 |
| Italy | 1 |
| Japan | 1 |
| Other | 3 |
| Health care providers | |
| Physicians | 3 |
| Nurses | 3 |
| Specialists (e.g., hepatologist, gastroenterologist) | 2 |
| Medical students | 1 |
| Other | 1 |
| Non–health care providers | |
| People living with HCV with or without HIV coinfection | 4 |
| Men who have sex with men (MSM) | 3 |
| General public | 2 |
| People born between 1945–1965 | 2 |
| Immigrants | 1 |
| Other | 1 |
Abbreviations: HCV, hepatitis C virus; HIV, human immunodeficiency virus
a Some studies included more than one population or country
Awareness
There were six studies on awareness of hepatitis C (11,12,14,17,18,24). The types of awareness varied across these studies: awareness of risk factors, of treatment, of one’s own infection and of the existence of HCV. Four studies included findings on awareness of HCV by the general public (11,12,14,17), one on awareness of HCV by MSM (18) and one on awareness of treatment by Canadian health care providers (24).
Two studies found that the general public had some awareness (defined as the knowledge that something exists) of hepatitis C (11,17). Compared with the public (27%), Canadian-born baby boomers (33%) were more likely to be aware that injection drug users have an increased risk of HCV compared with the general public (27%) (14). However, results from the United States’ National Health and Nutrition Examination Survey (NHANES) indicated that fewer than half of Americans who had HCV infection were aware of their infection (12). Two studies found that the general public was not clear about the differences between hepatitis A, B and C (11,19).
Knowledge
All of the included studies assessed knowledge of HCV. Knowledge was measured using a series of yes/no/don’t know or true/false statements, or one’s perceived knowledge level. Knowledge was assessed in the following topics: natural history of HCV, transmission routes, the availability of a vaccine and the availability of treatment.
The natural history of HCV and its consequences
Three studies included information on health care providers’ knowledge of the natural history and consequences of HCV (16,25,26). In a convenience study of Canadian physicians, 35% reported “knowing a lot” about symptoms associated with HCV (16). In a small study of dental students from Bulgaria, 80% reported knowing that infection with hepatitis B virus or HCV may be asymptomatic (26). In addition, residents, physicians, nurse practitioners and physician assistants working in emergency departments in the US were reported to have high knowledge scores regarding the manifestations of HCV (percentage not reported) (25).
Eight studies included information on the public’s knowledge about the natural history of HCV (8,9,11,13,14,16,17,19). Two Canadian studies found that 83–90% of participants knew that people with HCV could be unaware of an existing infection (14,16). Similarly, over half (57%) of US baby boomers knew that HCV can lead to liver cancer and 61% believed that someone with HCV infection can present with no symptoms (8). One study reported that one-third of MSM knew that HCV infection could lead to liver cancer (31%) and liver failure (37%) (18). Conversely, in an international study with immigrants from Asia, it was reported that there was confusion about the different types of hepatitis infections and uncertainty about the natural history of the infection (19).
Knowledge of transmission
Two studies reported on health care providers’ knowledge of HCV transmission (22,26). The majority of health care providers in the studies identified the main routes of transmission as blood transfusions, exposure to blood during sexual activity and sharing needles while injecting drugs (22,26). A small percentage (12%) of nurses working in hemodialysis clinics in Italy believed, incorrectly, that HCV can be transmitted through kissing, and 19% did not know that getting a tattoo could be a means of HCV transmission (22).
Ten studies reported information on knowledge of HCV transmission among the general public (8,10-12,14-17,19,21). One Canadian study reported that the most frequently known HCV transmission routes were blood transfusions, unsafe/unprotected intercourse and injection drug use/sharing of needles (14). Few Canadians identified other routes of transmission such as sharing personal hygiene items (7%), getting tattoos and body piercings (4%), exposure to risk factors while travelling in foreign countries where HCV may be endemic (4%), and mother-to-child transmission through pregnancy (1%) (14). Furthermore, approximately 54–62% of the general population in Canada knew that HCV is transmitted mainly through blood-to-blood contact (16). In four studies, a small percentage of the general public indicated that HCV can be transmitted through kissing or casual contact (8,12,14,21).
Knowledge of treatment
Two recent studies, published after the new interferon-free DAA therapies became available, focused on knowledge of the curability of HCV (8,24).
Among health care providers, specialists (i.e., hepatologists, gastroenterologists, hepatology nurses) scored higher on knowledge statements about HCV treatment than general practitioners (GPs) (23,24). Of the 10 primary care physicians surveyed, seven were unsure or not aware of the new interferon-free DAAs and were not sure about the mechanisms of action (24).
In the US, 51% of baby boomers presenting to emergency departments correctly believed that HCV is curable and 77% had knowledge of new medications available to treat HCV (8). However, three studies detected a misconception among the general public about the availability of a vaccine to prevent HCV (11,15,21). About one half of the Canadians interviewed (50%) in one study believed there was a vaccine to prevent HCV (14). In two US studies, 42% of American baby boomers and 60% of African-American baby boomers believed there was a vaccine to prevent HCV (8,11).
A summary of the findings is shown in Table 2.
Table 2. Summary of findings on awareness and knowledge of hepatitis C virus among health care professionals and the general public.
| Outcomes | Key Findings |
|---|---|
| Awareness | Public: The general public was aware of HCV and main risk factors (14) MSM had high awareness of HCV treatment (18) |
| Knowledge | Health care providers: Specialists were more up-to-date on new HCV treatments than primary care physicians (24) Health care providers knew less about some routes of HCV transmission (e.g. unsafe tattooing practices or piercings) compared with the main routes (i.e., injection drug use) (22,26) |
| Public: The general public had misconceptions around risk factors for transmission of hepatitis C (e.g., casual contact, saliva, kissing) (11,12,14,16,19) There were also misconceptions about the availability of a vaccine (8,14,16) Overall, there was little knowledge about the interferon-free DAA hepatitis C treatment (8,9,13,14,16) |
Abbreviations: DAA, direct acting antivirals; HCV, hepatitis C virus; MSM, men who have sex with men
Discussion
To the best of our knowledge, this is the first scoping review that provides a snapshot of what health care providers and the general public know about HCV. Overall, health care providers know about the most common transmission routes and risk factors, whereas specialists are more up-to-date on treatments than primary care physicians (23,24). The general public is aware of HCV; however, some people do not know the difference between hepatitis A, B and C; there are misconceptions around routes of transmission; and some incorrectly believe that an HCV-preventable vaccine exists.
There are some limitations to consider when interpreting our findings. First, there was a lack of standard definitions for knowledge and awareness and the terms were often used interchangeably. Second, only a few studies captured awareness and knowledge of interferon-free DAA treatments. Finally, the findings were based on cross-sectional studies, which only capture data of a study population at a single point in time.
Future research could include assessment of high-risk populations (e.g., Indigenous peoples or incarcerated populations); incorporate clear and consistent definitions of awareness and knowledge; and assess factors that may be associated with differences in awareness and knowledge (e.g., rural versus urban settings, and socioeconomic status). Additional research on health care providers’ knowledge of HCV could also help tailor future knowledge translation and exchange products.
In conclusion, increasing health care providers’ and the general public’s awareness of and knowledge about HCV can facilitate the discussion about whether HCV testing should be considered. The findings and gaps identified in this review can help inform future interventions and public health campaigns to do with HCV and support the Global Health Sector Strategy on Viral Hepatitis.
Acknowledgements
We would like to thank Dr. Margaret Gale-Rowe and Dr. Jun Wu for their contributions to the conceptualization and revision of this manuscript, Audréanne Garand for her support in the data collection, extraction and initial analysis of the results, and the Health Canada librarian who helped conduct the literature search.
Appendix 1. Description of included studies (n=19)
| Author(s), year of publication / Country | Study design / Population / setting | Method of data collection | Outcome / Findings |
|---|---|---|---|
| General public(n=14) | |||
| Allison et al. (2016) (8) US |
Cross-sectional study Baby boomers (1945–1965) (n=915) Urban emergency department |
Structured interview within six weeks of HCV antibody test to assess knowledge | Knowledge
|
| CATIE (2015) (9) Canada |
Cross-sectional study People living with HCV (n=326) Medical clinics offering HCV infection care |
Self-administered questionnaire (paper and online) | Knowledge
|
| Chen et al. (2013) (10) US |
Cross-sectional study HCV infection and HIV/HCV coinfection (n=292) Outpatient clinic |
Cross-sectional survey and pre- and post-educational surveys | Knowledge
|
| Crutzen & Goritz (2012) (11) Germany and Netherlands |
Cross-sectional study General public in Germany (n=1989) and Netherlands (n=668) Online panel |
Two large-scale surveys administered to online panels | Awareness
|
| Denniston et al. (2012) (12) US |
Cross-sectional study General public who tested positive for HCV (n=32,847) NHANES 2001–2008 data |
Phone interview | Awareness
|
| Eguchi & Wada (2013) (13) Japan |
Cross-sectional study Japanese working population (n=3,129) Online |
Self-administered questionnaire (online) | Knowledge
|
| EKOS Research Associates Inc. (2012) (14) Canada |
Cross-sectional study General public (≥16 years old) (n=2,000) Survey panel |
Phone interview | Awareness and knowledge
|
| Hopwood et al. (2016) (15) Australia |
Cross-sectional study Gay and bisexual men living with HIV and/or HCV (n=474) Online study |
Self-administered questionnaire | Knowledge
|
| Ipsos (2012) (16) Canada |
Cross-sectional study General population (≥18 years) (n=1,000) (Setting unknown: information not available) |
Self-administered questionnaire (online) | Knowledge
|
| Lambers et al. (2013) (17) Netherlands |
Observational study HIV-positive and HIV-negative MSM (n=539) Various (recruitment campaigns, media, word of mouth) |
Self-administered questionnaire (paper) | Awareness
|
| Lea et al. (2016) (18) Australia |
Cross-sectional study MSM (n=405) Various (social media advertisements, community organization websites) |
Self-administered questionnaire (online) | Awareness
|
| Owiti et al. (2015) (19) Australia, Canada, Mexico, the Netherlands, US |
Systematic narrative review Predominantly Asian immigrants (n=51)a (Setting unknown: information not available) |
Information not available | Knowledge
|
| Pundhir et al. (2016) (20) US |
Cross-sectional study Patients (≥18 years) with HCV infection and with or without HIV coinfection (n=292) Primary care clinic |
Self-administered questionnaire (online and paper) | Knowledge
|
| Rashrash et al. (2016) (21) US |
Cross-sectional study African-American baby boomers (b. 1945–1965) (n=137) Hospital and wellness centre |
Cross-sectional survey using audio computer-assisted self-interviewing | Knowledge
|
| Health care providers (n=6) | |||
| Bianco et al. (2013) (22) Italy |
Cross-sectional study Nurses (n=326) Hemodialysis units |
Self-administered questionnaire | Knowledge
|
| Ipsos (2012) (16) Canada |
Cross-sectional study GPs/Family practitioners (n=300) (Setting unknown: information not available) |
Information not available | Knowledge
|
| McGowan et al. (2013) (23) Canada, Central/Eastern Europe, Latin America, Western Europe, Nordic countries, Asian/Pacific countries, Middle East/Africa, US |
Cross-sectional study Physicians providing HCV treatment (n=697) International market research database |
Phone interview or self-administered online questionnaire | Knowledge
|
| Naghdi et al. (2017) (24) Canada |
Cross-sectional study Primary care physicians, specialists, hepatology nurses and nurse practitioners (n=163) Convenience sample through provider organizations |
Self-administered questionnaire (online) | Knowledge
|
| Rotte et al. (2013) (25) US |
Observational study Residents, physicians, nurse practitioners, physician assistants (n=78) Emergency departments |
Self-administered questionnaire (online) | Knowledge
|
| Todorova et al. (2015) (26) Bulgaria |
Cross-sectional study Dental medicine students (n=96) Faculty of Dental Medicine, Medical University of Varna, Bulgaria |
Self-administered questionnaire | Knowledge
|
Abbreviations: CDC, Centers for Disease Control and Prevention; HAV, hepatitis A virus; HBV, hepatitis B virus; HCV, hepatitis C virus; HIV, human immunodeficiency virus; Gen, generation; GP, general practitioner; MSM, men who have sex with men; NHANES, National Health and Nutrition Examination Survey; n, number; RNA, ribonucleic acid; US, United States
a A number of studies were included in the systematic review
Conflict of interest: None.
Funding: This work was supported by the Public Health Agency of Canada.
References
- 1.World Health Organization. Hepatitis C: key facts. Geneva: World Health Organization; 2017. http://www.who.int/en/news-room/fact-sheets/detail/hepatitis-c
- 2.Westbrook RH, Dusheiko G. Natural history of hepatitis C. J Hepatol 2014. Nov;61(1 Suppl):S58–68. 10.1016/j.jhep.2014.07.012 [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization. Global hepatitis report, 2017. Geneva: World Health Organization; 2017. http://apps.who.int/iris/bitstream/handle/10665/255016/9789241565455-eng.pdf?sequence=1
- 4.Trubnikov M, Yan P, Archibald C. Estimated prevalence of hepatitis C virus infection in Canada, 2011. Can Commun Dis Rep 2014. Dec;40(19):429–36. https://www.ncbi.nlm.nih.gov/pubmed/29769874 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schanzer D, Pogany L, Aho J, Tomas K, Gale-Rowe M, Kwong J et al. Impact of availability of direct-acting antivirals for hepatitis C on Canadian hospitalization rates, 2012–2016. Can Commun Dis Rep 2018;44(7/8):150–6. https://www.canada.ca/en/public-health/services/reports-publications/canada-communicable-disease-report-ccdr/monthly-issue/2018-44/issue-7-8-july-5-2018/article-1-canadian-hospitalization-rates-hep-c.html [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Global Health Sector Strategy on Viral Hepatitis 2016–2021: towards ending viral hepatitis. Geneva: World Health Organization; 2016. http://apps.who.int/iris/bitstream/10665/246177/1/WHO-HIV-2016.06-eng.pdf?ua=1
- 7.McLeod A, Cullen BL, Hutchinson SJ, Roy KM, Dillon JF, Stewart EA et al. Limited impact of awareness-raising campaigns on hepatitis C testing practices among general practitioners. J Viral Hepat 2017. Nov;24(11):944–54. 10.1111/jvh.12724 [DOI] [PubMed] [Google Scholar]
- 8.Allison WE, Chiang W, Rubin A, Oshva L, Carmody E. Knowledge about hepatitis C virus infection and acceptability of testing in the 1945–1965 birth cohort (baby boomers) presenting to a large urban emergency department: a pilot study. J Emerg Med 2016. Jun;50(6):825–831.e2. 10.1016/j.jemermed.2016.02.001 [DOI] [PubMed] [Google Scholar]
- 9.CATIE. Room for improvement: knowledge exchange needs of people living with hepatitis C. Toronto: CATIE; 2015. http://www.catie.ca/sites/default/files/Hepatitis%20C%20needs%20assessment%20report_final.pdf
- 10.Chen EY, North CS, Fatunde O, Bernstein I, Salari S, Day B et al. Knowledge and attitudes about hepatitis C virus (HCV) infection and its treatment in HCV mono-infected and HCV/HIV co-infected adults. J Viral Hepat 2013. Oct;20(10):708–14. 10.1111/jvh.12095 [DOI] [PubMed] [Google Scholar]
- 11.Crutzen R, Göritz AS. Public awareness and practical knowledge regarding Hepatitis A, B, and C: a two-country survey. J Infect Public Health 2012. Apr;5(2):195–8. 10.1016/j.jiph.2011.12.001 [DOI] [PubMed] [Google Scholar]
- 12.Denniston MM, Klevens RM, McQuillan GM, Jiles RB. Awareness of infection, knowledge of hepatitis C, and medical follow-up among individuals testing positive for hepatitis C: National Health and Nutrition Examination Survey 2001-2008. Hepatology 2012. Jun;55(6):1652–61. 10.1002/hep.25556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eguchi H, Wada K. Knowledge of HBV and HCV and individuals’ attitudes toward HBV- and HCV-infected colleagues: a national cross-sectional study among a working population in Japan. PLoS One 2013. Sep;8(9):e76921. 10.1371/journal.pone.0076921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.EKOS Research Associates Inc. 2012 HIV/AIDS attitudinal tracking survey. Ottawa: EKOS; 2012 Oct. http://www.catie.ca/sites/default/files/2012-HIV-AIDS-attitudinal-tracking-survey-final-report.pdf
- 15.Hopwood M, Lea T, Aggleton P. Multiple strategies are required to address the information and support needs of gay and bisexual men with hepatitis C in Australia. J Public Health (Oxf) 2016. Mar;38(1):156–62. 10.1093/pubmed/fdv002 [DOI] [PubMed] [Google Scholar]
- 16.Ipsos Healthcare. Survey on hepatitis C knowledge and perception among Canadians and GP, September 2012. Paris: Ipsos; 2012. https://www.ipsos.com/sites/default/files/publication/2013–01/5977-report.pdf
- 17.Lambers FA, Prins M, Davidovich U, Stolte IG. High awareness of hepatitis C virus (HCV) but limited knowledge of HCV complications among HIV-positive and HIV-negative men who have sex with men. AIDS Care 2014. Apr;26(4):416–24. 10.1080/09540121.2013.832721 [DOI] [PubMed] [Google Scholar]
- 18.Lea T, Hopwood M, Aggleton P. Hepatitis C knowledge among gay and other homosexually active men in Australia. Drug Alcohol Rev 2016. Jul;35(4):477–83. 10.1111/dar.12333 [DOI] [PubMed] [Google Scholar]
- 19.Owiti JA, Greenhalgh T, Sweeney L, Foster GR, Bhui KS. Illness perceptions and explanatory models of viral hepatitis B & C among immigrants and refugees: a narrative systematic review. BMC Public Health 2015. Feb;15:151. 10.1186/s12889-015-1476-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pundhir P, North CS, Fatunde O, Jain MK. Health beliefs and co-morbidities associated with appointment-keeping behavior among HCV and HIV/HCV patients. J Community Health 2016. Feb;41(1):30–7. 10.1007/s10900-015-0059-4 [DOI] [PubMed] [Google Scholar]
- 21.Rashrash ME, Maneno MK, Wutoh AK, Ettienne EB, Daftary MN. An evaluation of hepatitis C knowledge and correlations with health belief model constructs among African American “baby boomers”. J Infect Public Health 2016. Jul-Aug;9(4):436–42. 10.1016/j.jiph.2015.11.005 [DOI] [PubMed] [Google Scholar]
- 22.Bianco A, Bova F, Nobile CG, Pileggi C, Pavia M; Collaborative Working Group. Healthcare workers and prevention of hepatitis C virus transmission: exploring knowledge, attitudes and evidence-based practices in hemodialysis units in Italy. BMC Infect Dis 2013. Feb;13(76):1-11. 10.1186/1471-2334-13-76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.McGowan CE, Monis A, Bacon BR, Mallolas J, Goncales FL, Goulis I et al. A global view of hepatitis C: physician knowledge, opinions, and perceived barriers to care. Hepatology 2013. Apr;57(4):1325–32. 10.1002/hep.26246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Naghdi R, Seto K, Klassen C, Emokpare D, Conway B, Kelley M et al. A hepatitis C educational needs assessment of Canadian healthcare providers. Can J Gastroenterol Hepatol 2017;2017:5324290. 10.1155/2017/5324290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rotte M, O’Donnell R. Knowledge, beliefs, and attitudes of emergency department health care providers towards hepatitis C and rapid hepatitis C testing. Ann Emerg Med 2013;62(4):S103 10.1016/j.annemergmed.2013.07.108 [DOI] [Google Scholar]
- 26.Todorova TT, Tsankova G, Tsankova D, Kostadinova T, Lodozova N. Knowledge and attitude towards hepatitis B and hepatitis C among dental medicine students. J of IMAB 2015;21(3):810–3. 10.5272/jimab.2015213.810 [DOI] [Google Scholar]