Abstract
A substantial body of literature indicates that shift workers have a significantly higher risk of workplace accidents and injuries, compared to workers in regular daytime schedules. This can be attributed to work during nights which require workers to stay awake during normal sleeping hours and sleep during natural waking hours, leading to circadian desynchronization, sleep disruption and cognitive impairment. A fatigue-risk trajectory model developed by Dawson and McCulloch has been used to describe the series of events which may precede fatigue-related incidents. This includes insufficient sleep opportunities, impaired sleep, fatigue-behavioral symptoms, and fatigue-related errors. The purpose of this paper is to provide examples of control measures along each level of the fatigue-risk trajectory, which include: (i) work scheduling strategies to include breaks for adequate sleep opportunities; (ii) training and educational programs to help workers make best use of recovery times for quality sleep; (iii) fatigue-detection devices to alert workers and safety managers of fatigue-related behaviors and errors. A brief introduction to Fatigue-Risk Management systems is also included as a long-term sustainable strategy to maintain shift worker health and safety. The key statements in this paper represent a consensus among the Working Time Society regarding a multi-level approach to managing occupational sleep-related fatigue.
Keywords: Shift work, Safety interventions, Fatigue-risk trajectory, Nonstandard shifts
Consensus Statements.
-
1)
Sleep-related fatigue associated with shiftwork is a complex hazard stemming from a variety of work and nonwork related sources. Successful management of occupational sleep-related fatigue requires a multi-layered, multi-level approach that addresses each level of the fatigue-incident risk trajectory:
provision of adequate opportunities for sleep
obtaining adequate, quality sleep
detection of fatigue-related behaviors and symptoms among workers
management of fatigued behavior
identification of fatigue as a cause of adverse events
-
2)
Developing an ‘optimal’ work schedule to provide adequate opportunities for sleep requires consideration of many factors such as hours of work, rest breaks between and within-shifts, shift sequences, work demands, workforce demographics and culture. As such, scheduling is unique to each industry, occupation and workplace. However, some general guidelines include:
the risk for a fatigue-related incident increases with the duration of time at work, night shifts, successive shifts and sequences of shift structure.
short, frequent breaks (up to 30 min) may be more protective than fewer, long breaks. However, inclusion of rest breaks should not extend the workday beyond a point where recovery may be impinged.
most adults require at least 7 h of sleep per night for optimal health and performance. Because time away from work is often devoted to a range of activities (e.g. social recovery, household/childcare duties), shift workers need at least 11 h between shifts in order to obtain 7 h sleep.
At least 2 night sleep periods with a day off in between blocks of shifts are required to offset accumulated work-related fatigue. However, more time may needed when workers experience extended working hours and/or severe circadian disruption.
-
3)
In addition to providing employees with an adequate opportunity to rest and recover, it is also important to ensure that they understand how best to ensure adequate sleep between shifts. An essential aspect of helping workers obtain adequate, quality sleep is competence-based training and education (T/E) programs. This requires a significant effort to understand the workforce so that programs can be tailored for specific needs and ensure adoption of better sleep behaviors. Programs should be available throughout the course of a workers’ career to reinforce key messages and to provide new information and strategies to improve sleep. While current studies suggest that successful sleep hygiene programs to improve sleep should be personalized, combined with face-to-face cognitive behavioral techniques and situated in a broader Fatigue Risk Management framework, more studies are needed to support these findings and explore what factors (e.g. culture) may have the greatest impact on success.
-
4)
Strategies and technologies used to mitigate/detect fatigue should be implemented judiciously but should not be relied on as a primary risk mitigation system. Considerations should be made with respect to scientific criteria (validity, reliability, generalizability,
-
5)
While relatively new as a regulatory approach, Fatigue Risk Management is generally considered to be an effective long-term solution for fatigue mitigation in the workplace because it requires constant monitoring, feedback and adaption to changing organizational needs. As part of a Safety Management System, it includes strategies in fatigue management policies and procedures, risk management, safety assurance, and safety promotion. Long term efforts to successful sustainable fatigue management include ingraining a safety culture as a core value in the workplace, committed involvement and input from all levels (i.e. senior leaders, management, workers, safety professionals), regular monitoring and evaluation for effectiveness and are flexible to meet continually changing needs of the company and workforce.
Consensus statements review expert panel: Anna ARLINGHAUS1(Chair), Torbjörn ÅKERSTEDT2, Göran KECKLUND2
1Ximes GmbH, Austria
2Stockholm University, Sweden
Full consensus among panel members on all statements.
Introduction
There has been strong evidence linking shiftwork with increased risk of occupational injuries and accidents1,2,3,4,5,6,7,8). Human beings, by nature, follow a regular wake/sleep cycle that coincides with daily light/dark cycles as dictated by the sun. Normal biological functioning, such as circadian rhythms follows these cycles, resulting in activity during brightness (daytime) and rest and recuperation in the absence of light (night). Shiftwork, defined as work outside of the hours of 0700–1800 h9), often requires workers to remain awake during the dark and to sleep during the day. This disrupts normal circadian rhythms and, in the short term, can lead to sleep disruption/reduction and increased risk for safety critical events such as work-related injuries. Studies have shown that after only one night shift, workers can exhibit significant sleep impairment and short-term memory deficits10,11,12). Long term exposure to shiftwork and extended working hours can have lasting effects on cognition and worker safety. Experimental studies have demonstrated that restricting sleep to <6 h per day for up to 2 wk in a laboratory setting resulted in the same cognitive function deficits as would be achieved with 48 h of total sleep loss13). Most recently, a prospective cohort study reported a dose–response relationship between shiftwork and cognition, with increasing cognitive losses among those with longer shiftwork tenure14). This same study also found that it may take several years to return to regular cognitive functioning after leaving nonstandard schedules14). Sleep disruption and cognitive impairment have been attributed to the almost two-fold increased risk for work-related injuries among shift workers compared to daytime only workers1, 2). As such, addressing mechanisms to mitigate fatigue-related incidents among shift workers is critical in both short- and long-term worker health and safety.
This manuscript is part of a series of consensus papers developed by the Working Time Society, under the auspices of the International Commission on Occupational Health15). The goal of this series is to provide guidance for a broad, international audience of researchers, industry members, workers, labor representatives, policy makers, and other interested stakeholders on managing fatigue associated with nonstandard working hours and ensuring worker health and safety. Collectively, the papers provide overviews of the current state of research, identify health and safety risks, make recommendations for effective interventions, and suggest future research directions. Each paper presents a number of consensus statements, developed through the procedures outlined elsewhere in this issue15), and describes the background information on which the consensus statements are based.
Scope of consensus review
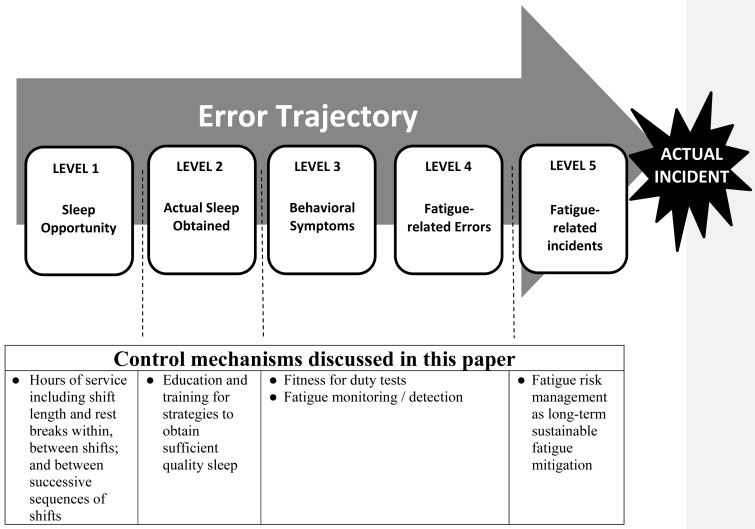
It has been suggested that work-place fatigue cannot easily be eliminated, but rather limited or managed; and that successful controls use a multi-factorial approach which focus on systematically identifying and mitigating risk factors for fatigue16). This multi-factorial approach has been described in a fatigue-risk trajectory model by Dawson and McCulloch, derived from Reason’s model of accident causation17), which describes a sequence of events preceding a fatigue-related incident (FRI) (Fig. 1)18). At the most basic level (Level 1) an individual may not have the opportunity to obtain sufficient sleep, possibly due to work scheduling. Individuals may lack the opportunity to obtain sufficient sleep or not utilize recovery periods to obtain sufficient quality sleep (Level 2), thus exhibiting fatigue-related behaviors and symptoms (Level 3). This increases the risk of fatigue-related errors (Level 4), and ultimately, leads to a FRI (Level 5). As such, fatigue can be mitigated through a series of controls to reduce the risk for fatigue-related errors.
Fig. 1.
Fatigue-risk trajectory (adapted from Dawson and McCulloch18)) describing the sequence of events which often lead to fatigue-related incident (Level 1–5), and examples of control mechanisms for each level of the trajectory.
The purpose of this paper is to describe a multi-level approach to managing occupational sleep-related fatigue. This paper is not meant to be an exhaustive review of all safety controls. Rather, we describe and suggest how to evaluate examples of workplace control measures which can be applied at each level of the fatigue-risk trajectory model to mitigate workplace FRI. In addition, we will also introduce the concept of fatigue-risk management as part of a safety management systems implementation for a long-term sustainable approach to mitigating fatigue-related workplace incidents.
For further description of other strategies, please refer to Satterfield et al.1919), Lerman et al.20) and other consensus papers in this edition of Industrial Health.
Controls for Level 1 (Opportunities for Sleep and Recovery): Working Time Arrangements
Traditional approaches to fatigue management have focused on working time arrangements (WTA), which provides guidelines or regulations regarding a combination of hours of work, successive shifts and recovery periods within and between shifts. However, these approaches rarely take into account social and individual aspects that drive recovery. At the most basic level, WTA have involved creating limits on working hours and mandating minimum duration of recovery periods to provide opportunities for rest and recovery from the physical and mental strain of working (Level 1, Fig. 1). For some industries (e.g. transportation) WTA may be strictly enforced via regulations21, 22), whereas for other industries, WTA may arise as a product of labor negotiations with little enforcement23, 24). Or in worse-case scenarios, such as for contractors or small businesses, there may be no limits on working hours or prescribed periods for rest. In the very extreme, in some cultures such as in Japan, there has been an ingrained mentality to work with very little rest, such that the term “death by overwork” (i.e. Karoshi) has been coined25).
Shift length and successive shifts
Four consistent trends in FRI have been reported after accounting for confounding factors such as number of staff, supervision levels and job tasks26, 27). In terms of shift length, it has been reported that the risk of a FRI generally increases exponentially with time on shift. Prior studies have reported that relative to an 8 h shift, the likelihood of a FRI increased by 13% for 10-h shifts, and 27% for 12-h shifts. The likelihood of FRIs also increased over successive shifts, with greater risk among successive night shifts, compared to successive day shifts. Shift structure also has been demonstrated to have a significant influence on fatigue-related incidents. Folkard and Lombardi28), found that the risk for a fatigue-related injury during 8-h shifts over 6 consecutive days was only marginally higher than the “standard” 8-h shifts over 5 d. However, the authors also found that if working hours were extended but the number of consecutive days decreased (e.g. 12 h over 4 d), the risk for a workplace accident increased by 25%, with a more pronounced effect among night shifts28).
Rest breaks
While time on shift increases the likelihood of an FRI2, 28,29,30,31,32), rest breaks need to also be considered as a crucial element in designing an effective work schedule to mitigate fatigue. Several dimensions have been considered with regard to recovery periods: within-shift breaks, recovery between shifts, and reset breaks between sequences of shifts.
Within-shift breaks (duration, frequency and timing)
A recent study demonstrated a clear dose-response relationship between total accumulated time of rest-breaks and decreased risk for work-related ladder falls33), suggesting that more time for breaks may reduce the risk for fatigue-related incidents either by reducing the exposure to work-related hazards and/or allowing more recovery time. However, frequent within-shift breaks could come as a tradeoff, with less time spent working. In addition, increasing within-shift breaks may extend shift length, with cascading effects such as increasing time on task and less time for sleep, which ultimately increases the risk for FRI. As such, a strategic balance between rest and work should also be considered for productivity and safety. Discussions between employers and workers may determine an optimal solution.
While duration of breaks is one aspect of recovery, frequency and timing should also be considered. Arlinghaus et al. reported that frequent, short rest breaks may have a stronger protective effect for work-related ladder falls than a single, long break33). This finding has also been demonstrated among other occupational settings, where workers reported feeling less tired with frequent, shorter breaks compared to longer breaks, spaced apart at longer intervals34,35,36). Similarly, Tucker et al.37) also found that the beneficial effects of rest breaks may be relatively short-lived in at least some work environments. A review of trends in working hours and accidents also supports this conclusion28). Folkard and Lombardi found that rest breaks at 2-h intervals are more effective to reduce risk for accidents and errors compared to 4- and 6-h intervals28). In a study modeling rest breaks among truck drivers, Chen and Xie found that more rest breaks can reduce crash-risk among truck drivers. Results of this study showed that taking one, two and three rest breaks can reduce drivers’ crash odds by 68%, 83%, and 85%, respectively, compared to drivers who did not take any rest breaks38). To determine the optimal duration for rest breaks for truck drivers, Chen and Xie, in a separate study, found that while increasing total rest-break duration can consistently reduce fatigue-related crash risk, 30 min breaks may be a sufficient length of time39). This same study also demonstrated that taking rest breaks too soon after the beginning of a shift would be less effective in protecting against motor vehicle crash risk39). An additional concern would be commuting duration and mode (e.g. driver vs. passenger), as it may have a significant effect on fatigue during the work shift. As such, timing of within-shift breaks is also a critical factor in occupational safety.
Between-shift breaks
Most developed countries have some form of regulation concerning working time arrangements, either as legislation or collective agreements. These regulations not only focus on hours of work, but also the interceding rest periods with the underlying assumption that time away from work will help offset occupational physical and psychological strains40). However, while there is agreement among most developed countries regarding this general assumption, there is no consensus on a standard minimum duration for recovery. For example, in the European Union, workers are entitled to at least 11 h of rest per 24-h period, with at least one day off each week41). In comparison, in the US, there are no federal laws governing minimum hours of rest between shifts for most workers, with the exception of some transportation sectors (e.g. commercial drivers, aviation crew, train operators). Across countries among different industry sectors and even workplaces, there is much variation in recovery periods from work (see Gärtner et al., for more detail, in this current issue of Industrial Health).
At a very basic level, a consensus among sleep experts has recommended that adults between the ages of 18−60 yr should sleep 7 or more hours per night on a regular basis to promote optimal health42). However, this expert-based consensus recommended that for those who are recovering from sleep debt, such as shift workers, 9 or more hours per night may be required at maintaining health and reducing the risk for impaired performance, increased errors and injuries/accidents. Prior recommendations suggest at least 11 h of recovery between shifts, with further considerations for additional recovery time43). Workers require time outside of their jobs for daily activities such as eating, socializing, child care, household duties and commuting. Work conditions also play an important role in determining optimal recovery after shifts43). These factors include the nature of work, job tasks, shift length and number of successive sequence of shifts (discussed in further detail in the following section). Lastly, while recommendations can be tailored to suit specific workplace requirements, individual worker variability also can affect the extent which between-shift recovery periods are effective at mitigating fatigue and fatigue-related incidents. (See Ritonja et al., in this edition of IH for more information about individual differences in shiftwork tolerance).
Reset breaks between sequences of successive shifts
There is general agreement that shortened or disturbed sleep impairs cognition and performance, leading to an increased risk for fatigue-related incidents. This is illustrated most effectively in laboratory experiments which demonstrate that performance under the short-term effects of sleep deprivation is similar to performance while at the legal limit of alcohol consumption for driving (either 0.05% or 0.08% blood alcohol consumption)44,45,46,47,48). However, for those whose jobs involve shiftwork, chronic sleep deprivation can have lasting effects. It has been reported that fatigue-related incidents increase with successive shifts, with a greater effect among night shifts26), and greater cognitive decline and accelerated brain aging occurs among those with longer shiftwork tenure13, 49). It is also important to note that sleep during the daytime is not as recuperative as sleep during nighttime because natural human circadian rhythms promote wakefulness during daylight hours5). Day sleeps after night shifts are generally shorter and reduced quality compared to normal night sleep43, 50). Thus for shiftwork involving overnight shifts, additional time for recovery between successive sequences of shifts may be necessary, compared to those in daytime only schedules. Providing adequate reset breaks between sequences of successive shifts would be critical to maintaining worker health and safety over the long term.
A study of recovery among shift working nurses which examined sleep, mood and social satisfaction on rest days following day and night shifts found that these self-reported measures were worse on the first rest day as compared to the subsequent work days40). The authors suggested that recovery took longer than anticipated and did not occur on the first rest day, but rather at the end of the second rest day. As such, the authors recommended at least 2 d of consecutive rest would enhance the benefit of the rest period. Significant differences in recovery were also observed by shift type. Alertness scores, ascertained from reaction-time and memory tasks, were worse on rest days following night shifts compared to days. The authors conclude that night shift workers were less alert on rest days, compared to daytime workers, because of frequent circadian shifting and misalignment experienced during night work, followed by a readjustment to a diurnal routine on days off. As such, recommendations from this study include allowing for a longer recovery period following night shifts; and that the day following a night shift should not be included as part of recovery time. Similar recommendations were made by the International Labor Organization51).
Similar findings were reported from a study that pooled data from several studies across different industries Åkerstedt et al52). This study found that self-reported sleepiness was most pronounced during the first recovery day, and not during the last working day. While the authors observed different recovery times associated with different working time arrangements (e.g. shift length, job type, shift sequences), they reported their data supported prior findings that one day of recovery is not sufficient, but two days, in most cases, was enough. However, for periods where workers may experience severe circadian disruption, longer periods of rest may be necessary. For example, Kecklund et al. recommended at least 3 d of recovery following 7 consecutive night shifts53). As such, while rest breaks are crucial in mitigating the effects of fatigue, the nature of work (e.g. physical demands, mental stimulation, job strain, job tasks) plays an important role in the accumulation of fatigue. Therefore, in modeling work schedules it is critical to assess and incorporate all aspects of the work itself, in addition to breaks and working hours. What remains unclear is if more recovery time is needed with longer shiftwork tenure?
For a broad overview of basic work scheduling descriptions and recommendations, see reviews such as Knauth43). A more recent review on limited wake shiftwork schedules has been reported by Short54).
Recommendations for working time arrangements
Optimal work scheduling is often unique to individual industries, workplaces or work forces. As such, there is no ‘perfect’ schedule. The best schedules must inevitably balance the competing operational, financial and social obligations (including safety) of all the key stakeholders, i.e. the organization, clients/customers, employees and their community. This may require a participatory design approach among all key stakeholders (e.g. senior executives, management, workers, regulators, and community representatives).
A schedule should at a minimum provide employees with an adequate opportunity to sleep and return fit-for-work as well as discharging appropriate family and social roles and responsibilities.
A system of work is a shared responsibility. Schedule design needs to ensure an adequate opportunity to rest and recover. In doing this, organizations should consider the duration, type and sequences of shifts. Workers should ensure that time away from work is used responsibly.
A Rest breaks pay a critical role in recovery from, and mitigation of, fatigue
Consider frequency, timing and duration; within and between shifts
There are trade-offs: more time for recovery will mitigate fatigue, but at a cost to time spent working and perhaps to some short-term measures of productivity
Short, frequent breaks (up to 30 min) may be more protective than fewer, long breaks
In general, at least 2 consecutive days of recovery between sequences of shifts can offset accumulated work-related fatigue. However, the nature of work needs to also be considered. Work that is extremely physically or mentally demanding or results in severe sleep loss or circadian disruption may require more time for recovery between shifts.
It has been suggested that adults should obtain at least 7 h of rest for optimal health. However, for those with chronic circadian disruption and sleep debt, such as night shift workers, it has been suggested that at least 11 h is needed for recovery, with further considerations for other additional time for social and household activities.
Various features of a work schedule (e.g. hours of work, rest periods, sequences of shifts) need to be considered in combination with one another rather than as independent factors, as is the case with most duty time regulations. Models that that take account of the various features simultaneously may help with this (e.g. the UK’s Health and Safety executive “Fatigue Risk Index”)55).
Controls for Level 2 (Actual Sleep Obtained): Training and Education
Most workers obtain sleep outside of the workplace, usually in their private homes. Ensuring adequate sleep could therefore be considered primarily an employee responsibility. However, in recent decades employers and regulators have introduced guidance materials focused on lifestyle training to promote an understanding of strategies to maximize recovery value of sleep opportunities. Sleep hygiene training and education (T/E) programs can be considered as an example of a control measure to obtain quality sleep. These types of programs address aspects of lifestyle and behavior in addition to environmental factors (e.g. light, noise) and include topics such as: guidelines for minimum hours of sleep needed to maintain optimal health, information about the role of circadian rhythms in regulating sleep and sleepiness and strategies for mitigating sleep disruption attributed to non-standard schedules (e.g. sleep phase shifting, personal aids, environmental factors). T/E programs can be delivered in a variety of different modes with different levels of participant involvement and competency checking. The most common methods include informational brochures or pamphlets, informal small group discussions and formal in-class training. In addition, with the greater acceptance of mobile phones and electronic tablets among the general population, there has also been an increase in online and computer-based training programs. Examples of North American T/E online resources freely available for public use include industry-specific (e.g. nurses, emergency responders, commercial pilots in Alaska) NIOSH-developed programs (https://www.cdc.gov/niosh/topics/workschedules/education.html), the Sleep and Health Education Program from Harvard Medical School (http://healthysleep.med.harvard.edu/portal/), and the Federal Railroad Administration’s Railroaders Guide to Health Sleep (https://www.railroadersleep.org/).
Evidence of effectiveness of training/education programs at improving sleep among shiftworkers
While there are many T/E resources available to address good sleep hygiene, there is limited evidence of the effectiveness of these products at improving sleep among the working population outside of a laboratory setting. Among the limited number of studies, a few common findings emerge. Firstly, one-time, short lectures are not sufficient to enact long term behavioral change to increase sleep duration and improve sleep quality among a chronically sleep-deprived working population, particularly where a culture of poor sleep is readily accepted. This was demonstrated in a study of the Sleep, Alertness, and Fatigue Education in Residency (SAFER) program, a 60 to 90 min mandatory lecture for all first year medical interns at the inpatient general medicine service at the University of Chicago hospital. Topics such as the neurobiology of sleep-wake activity, adverse effects of sleep loss and countermeasures to mitigate fatigue of medical residence were presented56). Although interns were provided recommended guidelines from the American Academy of Sleep Medicine for sleep pre- and post- work shift rotation, actigraphy data showed that interns continued to consistently obtain less than adequate sleep. Longer T/E programs may be more effective in helping workers retain information and adopt subtle changes in their routines over time to successfully improve sleep. Chen et al. reported on the efficacy of a 5-wk T/E sleep hygiene program provided to working women with sleep disorders, and therefore a more immediate concern to address57). Significant improvements in sleep hygiene education and self-reported sleep quality were associated with strategies to develop good sleep environment/habits, reduce emotional stress and improve diet and exercise habits. However, exercise and alternative therapies were not effective, which the authors attribute to the study’s short follow-up period, suggesting that these strategies may be effective if workers were given more time to incorporate them into their daily routines.
A second common finding suggests that education alone is not sufficient to change sleep behaviors and improve sleep. A suite of random control trials among Japanese white-collar workers hint that combining knowledge with some forms of personalized cognitive behavior therapy may be the most effective. Suzuki et al. examined the effectiveness of a 2-wk, internet-based self-help program which provided information about sleep, sleep problems, health behaviors that affect sleep quality and strategies to improve sleep quality58). Participants concentrated on changing 3 behaviors over a 3 wk period, during which they documented their actions with a sleep e-diary. While they received daily and weekly feedback, encouragement generated by the website and participated in a self-reward program, results did not show a significant improvement in self-reported sleep quality. Although internet-based T/E programs allow for easier and broader distribution of sleep hygiene material, further studies suggest that some forms of face-to-face, personalized contact may have better success in changing sleep behaviors in certain workforce populations59, 60). In a study by Kakinuma et al.61), systems engineers volunteered to attend a 1 h sleep hygiene T/E session, delivered in a classroom setting by an occupational health physician who emailed participants 2 wk later to inquire about the participant’s progress at improving sleep hygiene behaviors and to provide encouragement. After a 3 wk follow up period, statistically significant reductions in afternoon sleepiness were associated with the intervention, but self-reported sleep quality was not. In a study with a higher degree of personal interaction and longer follow up period, subjective sleep quality significantly improved among a group of white collar workers who attended a one hour classroom T/E session led by an occupational physician and received an additional 30 min cognitive behavioral training session specifically adapted to each individual to modify their sleep behaviors59). Instructors were also available to answer participants’ questions via email at any time during the 3 month study follow up. Results demonstrated that individual behavioral training significantly improved sleep quality compared to receiving just T/E alone. Similar results were reported among a group of white collar workers with insomnia60) who participated in a 30-min T/E session combined with a 2 h individualized session on sleep behavior, adapted to suit their specific needs. Study findings indicated significant improvements in sleep duration and quality among those who received the combined approach, compared to those who received just the educational portion. Further information about behavioral change strategies have been discussed by DeJoy62) and Cooper63).
A further common finding among studies suggests that inclusion of T/E programs with other fatigue risk management strategies may provide successful results in improving sleep among shift workers. A study of law enforcement officers who took part in an educational sleep hygiene workshop found an improvement in officers’ knowledge of good sleep practices one month post-intervention, though subjective sleep satisfaction did not improve. While their status as volunteers suggest an interest in improving their sleep habits, subjects reported difficulties adopting new sleep behaviors and indicated problems could be attributed to their difficult work schedules, which were not changed64). A study of the Alertness Management Program, which included a 3.5 h self-paced digital education module combined with a new scheduling rota, reported that participants significantly expanded their knowledge of good sleep hygiene, improved their performance measures and increased duration of subjective and objectively measured sleep in a 24 h period by more than one hour during work days and days off65). Improvements in sleep quality and duration was reported 12 wk post-intervention in a study of the Fatigue Countermeasures Program for Nurses (FCMPN)66). This program included a 60 min educational component providing information about sleep, circadian rhythms, adverse effects of poor sleep and strategies for mitigating fatigue, such as strategic caffeine use and napping. Additional institutional strategies such as provision of adequate staffing and full utilization of within-shift breaks were included. These findings support recommendations from prior literature suggesting that education is less effective when applied as the sole countermeasure to improve sleep habits67) and that T/E programs are most effective when they are part of a comprehensive fatigue management program68).
Recommendations for training and educational programs in sleep hygiene
Findings from sleep hygiene T/E programs among the workforce population suggest that frequent industry-specific T/E programs offered throughout the course of a workers’ career, combined with individualized behavioral strategies with professional medical support, and situated in a broader Fatigue Risk Management System may be the most beneficial in helping workers obtain optimal, recovery sleep. Additional components, such as a competency-based approach, cultural norming and feedback loops that reinforce the training still need to be better understood.
Differences in T/E effectiveness reported in current literature may be also be attributed to differences in a variety of factors such as follow up time, cultural acceptances, organizational needs, etc. As such, future studies are needed to understand the importance of which factors may be critical for success.
More longitudinal studies are needed to examine the long-term effects of T/E programs.
A series of recommendations and preliminary principles for development of effective T/E programs for shiftworkers has been presented by Tepas69):
It is important to distinguish the difference between providing “information” and “education”. “Information” can be defined as the presentation of knowledge and facts, whereas “education” requires development of instruction along with relevant materials to ensure that information can be learned and used. As such, design of an effective program requires considerable thought regarding the intended audience and thus will shape the information provided, mode of delivery, frequency and duration of session and additional tools such as cognitive behavioral programs.
Effective T/E programs should be relevant to the specific workforce. Developing programs to change sleep behaviors requires a significant amount of effort and time and may also require participation of family members as they also have an influence on shiftworkers’ sleep habits. Taking the time to understand the specific workforce will allow for the tailoring of T/E programs (e.g. delivery modes, language) and increase chances for success.
The optimal number and duration of sessions is a delicate balance between providing a sufficient number to convey all pertinent information, but not too many such that the key messages can be retained.
Recommendations and interventions should be practical and socially acceptable, otherwise they will not be adopted for use.
The effectiveness of T/E programs should be monitored frequently and evaluated by workers to ensure that information remains relevant and assessable.
Future directions include additional and more deliberate evaluations of T/E sleep hygiene programs which are shared across organization and industries to identify best practices.
Controls for Level 3 & 4 (Behavioral Symptoms and Fatigue-related Errors): Fatigue Monitoring/Detection Technology
There are several mechanisms that have been explored to monitor and detect fatigue-related behaviors and errors. This includes subjective measures such as self-reported behavioral scales and symptom checklists18), and objective measures such as those assessed with technology or through biomarkers. To meet the increasing interest in emerging technologies, this paper will concentrate on objective measures. For more information regarding subjective measures, please see references such as Neuberger70) and Aaronson et al.71).
Advancements and implementation of fatigue monitoring or detection devices have generally been concentrated among the transportation and mining industries. In-vehicle monitoring systems have mostly been used among commercial drivers, although in recent years have been more readily available in luxury automobiles on the public market. It has been estimated that the number of motor vehicle crashes would be reduced by 10–20% by monitoring and predicting driver behavior72). As such, the introduction of these technologies in non-commercial transportation could have a significant effect for driver and public safety. However, despite the advances made in fatigue monitoring and detection technologies (e.g. less intrusive, less cumbersome) they are still most common in transportation, but could be suitable for other activities outside of driving.
Generally, devices to monitor or detect fatigue can be categorized as those which predict future fatigue as a measure of fitness for duty, or those which monitor current state of drowsiness. Monitoring devices can be further classified as those which monitor driver physiology versus those which assess driver behavior. This section will provide a general review of available technologies. For more detailed information regarding specific devices, please refer to Dawson et al.16) and Kerick et al73).
Fitness for duty tests
The assessment of fitness for work is defined as the determination of whether an individual is fit to perform his or her tasks without the risk to self or others74). In terms of fatigue-related incidents, fitness for duty is often assessed at the beginning of the shift and predicts whether a worker will be at a high risk for a fatigue related incident during their subsequent working hours. These predictions are based on prior behavior such as work and sleep duration, or can also include performance on neurobehavioral tasks such as psychomotor vigilance or hand-eye coordination (See Dawson et al.16) for detailed information about specific technologies). Assessing fitness for duty and predicting the risk of fatigue related incidents can allow for the planning and implementation of optimally timed interventions or countermeasures (e.g. change in job tasks, scheduled rest breaks).
While fitness for duty assessments can be a relatively easy add-on to existing Fatigue Risk Management Systems, there are several caveats that should be considered. One of these key issues is determining what level of risk is acceptable, and who has the authority to make that decision (e.g. employer vs industry standard)75). In addition, predictive models may account for work and sleep hours, but may not include other considerations such as job tasks (e.g. physically or mentally demanding) or non-occupational external influences (e.g. family responsibilities, underlying chronic health issues such as sleep apnea). Consequently, their ability to properly predict risk for fatigue related incidents may be limited due to lack of relevant information, inability to tailor to individual state, or poor data due to reporting bias. As such, predictions may not be accurate and should be used with caution as a stand-alone product.
Monitoring/detection devices
The largest gains in monitoring/detection devices have been made in the transportation sector to assess driver drowsiness. One of the most common physiological features used to determine fatigue is eye-related movement, such as eyelid closure and blink rate76, 77). Perhaps one of the most widely recognized validated eye-related marker of fatigue is PERCLOS, defined as the percent of eyelid closure. Risk for high fatigue is defined as more than 80% eyelid closure, accompanied by slow eyelid closure78). While many devices have been built upon the PERCLOS platform, there are limitations to this measure including inaccurate readings at low light levels, and inability to determine micro-sleeps (sleep-related lapses of attention lasting a few seconds79)) which may not be accompanied by eyelid closure. Other options to detect signs of driver drowsiness include facial-recognition systems which examine not only eye-related movements, but also consider other facial aspects. For example, yawning could be detected from the rate and changes in mouth contours80). Estimation of head pose and motion detection can provide information about head nodding, considered to be another sign of driver drowsiness81, 82). Other facial characteristics used to assess drowsy driving include wrinkles on brows, mouth and nasolabial fold83). While facial recognition (including artificial intelligence/machine learning) systems provide an objective measure of driver characteristics which may indicate fatigue, there are several limitations that should be considered. Often times, these monitoring devices are built into workstations, thus being effective for only stationary workers. In addition, some sensors may be sensitive to interference from other equipment or low light conditions. Privacy issues are also of concern, as some monitoring devices use video capturing to assess workers. There is much more research and validation that still needs to occur to address these issues.
Internal physiological measures such as heart rate variability, Electro-Dermal Activity and steering-wheel grip pressure are considered as methods of indirectly estimating the driver’s fatigue level84). Brain wave activity measured with electroencephalogram (EEG) and electro-oculogram (EOG), and more recently with near-infrared spectroscopy (NIRS), are considered to be gold standard measures of fatigue85, 86). It has been suggested that these physiological signals can sense the onset of fatigue earlier than external signals, which may make them more effective at preventing fatigue-related events87). However, while many of these physiological sensors are effective under controlled laboratory conditions, signals may be too sensitive to collect in real world driving conditions thus creating artifacts and erroneous readings. Continuous physiological monitoring may be effective for workers who are mobile but require the use of body sensors which can be cumbersome and intrusive for practical purposes and can result in long latency in detection and significant error rates. However, recent advances have included wireless technologies and non-intrusive sensory devices that can be placed in the steering wheel or driver’s seat88,89,90). User acceptance, understanding, and ability to properly use such systems is still a significant challenge.
More recently, embedded performance measures have been used to determine impaired performance. These types of measures are more commonly used in the transportation sector and involve continuous monitoring and recording of driving behavior by in-vehicle equipment. Types of driver performance or behavior measures include steering wheel movement, laneway departures, distance to vehicles ahead and hard accelerations/braking91,92,93,94,95). Among these measures, steering wheel movement and laneway departures are the most commonly used leading indicators of elevated fatigue and likelihood of inadvertent sleep onset. Steering wheel movement is measured through an angle sensor mounted on the steering column. As a driver becomes drowsy, the number of micro-corrections (defined as movements between 0.5° and 5°) diminishes, compared to an alert state. While this technology is currently being adopted in some car companies, it is effective only in limited situations due to their reliability in specific environments96). Laneway deviations have been reported to be correlated with the Karolinska Sleepiness Scale97), however, external factors (e.g. road conditions, lighting) not related to driver drowsiness may influence results. In general, driving behavior indicators are unique to each vehicle type and vary among drivers based on driving habits, skills and experience.
To overcome limitations in specific monitoring devices, hybrid systems have emerged fusing together different technologies. Recent studies have shown that a mixture of PERCLOS, EEG and EOG were more reliable in correlating with driver drowsiness than the individual measures98). Advances in real-time monitoring have also recently emerged, providing visual and audible alarms for the driver and off-site safety managers to alert when the driver is at a “high level” of fatigue. While effective at encouraging quick changes in behavior during work to remain alert, in some instances, some drivers may begin to over rely on the device, or further push themselves, ultimately increasing the risk for a fatigue-related crash further down the road.
Recommendations for fatigue monitoring/detection technologies
Choosing an effective fatigue monitor/detection device is unique to each workplace. However, several considerations should be made such as feasibility, acceptance from workers and existing policy, practice or legal issues78, 99, 100).
Validity − does the system measure the fatigue or fatigue-related decrements it purports to measure?
Reliability − does the system exhibit consistency in its measurement over time?
Generalizability − how well does the system recognize the same fatigue-related event across diverse environments?
Sensitivity − does the system correctly identify true fatigue-related events?
Specificity − conversely, does the system correctly reject false events that are not fatigue-related?
Adaptability − does the system adapt to individual differences in susceptibility to fatigue, or to changes in operator behavior over time?
Compatibility − is the system compatible with other required systems such as in-vehicle telematics?
Predictability − is there a time lag between the recognition of fatigue and the likelihood of an accident?
Hybrid solutions which predict and monitor/detect increased risk for fatigue-related events may overcome limitations of individual monitoring systems and provide a broader range of protection from fatigue related incidents.
Effective systems also should provide compelling and effective feedback to the user so that appropriate actions can be made within a useful timeframe.
Ensuring privacy with information gathered from fatigue monitoring device is critical. Given that these devices are measuring individual behaviors and include personal identification, assurances need to be made that the data will be kept secured, only serve for the purposes it was intended for and be viewed only by those in interest of worker safety and health. How the company uses the information will ultimately affect acceptance (e.g. to promote safety or be used for disciplinary actions).
A critical limiting factor to overall utility is human response and acceptance to the technology provided. For example, there may be the danger of over-reliance on technologies, leading to an inflated trust in the system. This is especially problematic in novel situations where the system may not recognize cues. False alarms can also be detrimental to effectiveness by fostering a lack of trust in the system, with potential for increased distraction and the possibility of abandoning the system altogether. The nature of information and delivery of alerting signals (e.g. visual, auditory, tactile), will also play an important role in how workers may interact with the system. Compliance is also a critical concern. If the system is too complicated to use or is not accepted (e.g. cultural acceptance, trust), it will not serve its intended purpose.
Further discussions on the benefits and challenges of technological approaches are discussed elsewhere16, 73, 99, 100).
An Introduction to Fatigue Risk Management as a Long-term Sustainable Effort to Mitigate Workplace Fatigue
While there are many possible individual solutions that can address fatigue and fatigue-related behaviors, some precautions should be observed. To date, there are no studies that demonstrate a long-term benefit of monitoring/detection devices or intervention strategies for workers who are subject to chronic sleep impairment and fatigue, as is common with most nonstandard shift workers. For those who are chronically fatigued, one acute event could have serious consequences. As such, it is critical to have a mechanism to continually monitor and address fatigue and FRI. Inclusion of Fatigue Risk Management Systems (FRMS) into existing Safety Management Systems (SMS) has been emerging as a potentially effective solution to providing a sustainable fatigue management that will mitigate fatigue-related incidents over the long term. Actual efficacy of these programs still need to be evaluated and published.
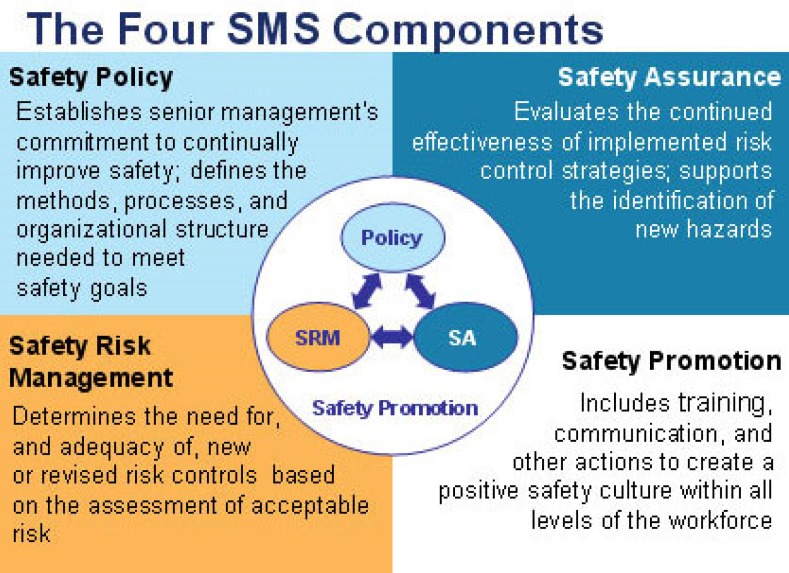
Fatigue Risk Management Systems have been defined as “scientifically based, data-driven addition or alternative to prescriptive hours of work limitations which manages employee fatigue in a flexible manner appropriate to the level of risk exposure and the nature of the operation”20). While a number of Fatigue Risk Management System guidelines have been developed for a range of industries20, 101,102,103,104,105,106,107,108,109,110,111), a set of commonalities have emerged based on the core components of SMSs (i.e. safety management policies and procedures, risk management, safety assurance and safety promotion) (Fig. 2)112, 113). The following section will be a broad description of these core components and their application into FRMS.
Fig. 2.
Four components of a Safety Management System from the Federal Aviation Administration113).
More detailed information about FRMS is provided by Honn et al. in this special edition of Industrial Health and other reviews such as Lerman et al.20) and Gander et al107).
Policies and procedures
Policies and procedures are the foundation of any SMS and represents the basis for the organization’s safety culture by reflecting the organization’s mission, vision and values for safety. In terms of a FRMS, an inventory of policies and procedures regarding fatigue management should be identified and where gaps or improvements are needed. It also involves identifying organizational roles and responsibilities with commitment of senior management and opportunities for meaningful engagement from employees. In addition, the policy should identify the authority under which it is issued and identifies roles and responsibilities of those tasked to implement the plan20, 112).
Risk management
Safety risk management is the process of hazard identification and evaluation, management to control hazards at an acceptable risk, and evaluation of results112). In terms of fatigue risk management, it is important for each working environment to determine what would be an acceptable level of fatigue impairment, and manage the risk for fatigue-related incidents. This entails the planning and control of the working environment in order to minimize, as far as is reasonably practicable, the adverse effects of fatigue on workforce alertness and performance in a manner appropriate to the level of risk exposure and the nature of the operation. For example, a fatigue-related incident at a clerical position is likely to have less severe consequences compared to air-traffic control. As such, a greater level of fatigue may be more tolerable in clerical positions compared to air-traffic controllers.
Safety assurance
Safety assurance is the process of auditing, monitoring, investigating and reporting any fatigue-related incidents to provide information about the organization’s performance and safety management effectiveness112). It requires identification of indicators for monitoring (e.g. near-miss or accident reports, improvement in knowledge following training sessions) and assessment of changes or improvements to safety over time. This allows for continuous improvement and adjustments to meet the changing needs of the organization and workforce.
Safety promotion
Safety promotion refers to the broad concept of the organization’s safety culture and philosophies. Safety communication and training are key subcomponents that can have a critical impact on the effectiveness. Communication needs to be prevalent company-wide, starting from senior leadership down to front line workers. Discussions are necessary to help identify risks, create solutions to mitigate risks and provide a feedback system where fatigue management systems can be updated with the changing needs of the organization. Training ensures that all workers and managers understand roles and responsibilities related to fatigue management, ultimately reducing exposure to risks for fatigue-related incidents. More importantly, a goal of training is to create a safety culture of awareness and proactive action.
Recommendations for fatigue risk management
There is no one best solution that will fit all workplaces. An effective fatigue management system requires cooperation, collaboration and a shared responsibility from management and workers.
Embed fatigue risk management within the broader Safety Management System:
Manage fatigue like any other hazard
Predict, measure, monitor and intervene
Assess what fatigue mitigation mechanisms are already in place. Introduce new interventions one at a time, and evaluate its effectiveness
Start with “small wins” to gain building success and momentum. This will also build stakeholder relations and trust
Build a healthy culture, in part through engaging the workers in forming creative solutions rather than imposing the solutions onto the workers.
Take advantage of the scientifically-validated tools already in existence and participate in developing new materials which are tailored for specific audiences (e.g. workers, OHS professionals, management, policy makers).
Incorporate competency-based training at all levels (managers, employees).
For additional information about fatigue risk management please refer to Lerman et al.20), Gander et al.107) and the consensus paper from Honn et al. in this edition of Industrial Health.
Conclusions
Fatigue is a complex, multi-faceted construct that can result from many occupational and non-occupational sources. As such, detecting and managing it in terms of occupational health and safety can be challenging. However, while it cannot be eliminated, it can be mitigated effectively at a systems level through cooperation and input from various stakeholders (e.g. employers, workers, occupational health and safety professionals, policy makers). Determining an acceptable level of fatigue is specific to each workplace, thus there is no one solution that can work across all situations. Rather, it is the responsibility and goal of all stakeholders to understand and utilize available controls at various levels, and evaluate program effectiveness over time to ensure controls meet changing needs.
References
- 1.Wong IS, McLeod CB, Demers PA. (2011) Shift work trends and risk of work injury among Canadian workers. Scand J Work Environ Health 37, 54–61. [DOI] [PubMed] [Google Scholar]
- 2.Wagstaff AS, Sigstad Lie JA. (2011) Shift and night work and long working hours—a systematic review of safety implications. Scand J Work Environ Health 37, 173–85. [DOI] [PubMed] [Google Scholar]
- 3.Lombardi DA, Folkard S, Willetts JL, Smith GS. (2010) Daily sleep, weekly working hours, and risk of work-related injury: US National Health Interview Survey (2004–2008). Chronobiol Int 27, 1013–30. [DOI] [PubMed] [Google Scholar]
- 4.Tucker P, Folkard S .(2012) Working time, health and safety: a research synthesis paper. ILO, Geneva. [Google Scholar]
- 5.Akerstedt T, Folkard S, Portin C. (2004) Predictions from the three-process model of alertness. Aviat Space Environ Med 75 Suppl, A75–83. [PubMed] [Google Scholar]
- 6.Williamson A, Lombardi DA, Folkard S, Stutts J, Courtney TK, Connor JL. (2011) The link between fatigue and safety. Accid Anal Prev 43, 498–515. [DOI] [PubMed] [Google Scholar]
- 7.Caruso CC. (2014) Negative impacts of shiftwork and long work hours. Rehabil Nurs 39, 16–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Caruso C, Hitchcock R, Russo J, Schimt J. (2004) Overtime and extended work shifts: recent findings on illness, injuries and health behaviours. DHHS/NIOSH Publication No. 2004–143.
- 9.IARC Working Group on the Evaluation of Carcinogenic Risks to Humans (2010) Painting, firefighting, and shiftwork. IARC Monogr Eval Carcinog Risks Hum 98, 9–764. [PMC free article] [PubMed] [Google Scholar]
- 10.Ansiau D, Wild P, Niezborala M, Rouch I, Marquié JC. (2008) Effects of working conditions and sleep of the previous day on cognitive performance. Appl Ergon 39, 99–106. [DOI] [PubMed] [Google Scholar]
- 11.Machi MS, Staum M, Callaway CW, Moore C, Jeong K, Suyama J, Patterson PD, Hostler D. (2012) The relationship between shift work, sleep, and cognition in career emergency physicians. Acad Emerg Med 19, 85–91. [DOI] [PubMed] [Google Scholar]
- 12.Tadinac M, Sekulić A, Hromatko I, Mazul-Sunko B, Ivancić R. (2014) Age and individual sleep characteristics affect cognitive performance in anesthesiology residents after a 24-hour shift. Acta Clin Croat 53, 22–30. [PubMed] [Google Scholar]
- 13.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. (2003) The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep 26, 117–26. [DOI] [PubMed] [Google Scholar]
- 14.Marquié JC, Tucker P, Folkard S, Gentil C, Ansiau D. (2015) Chronic effects of shift work on cognition: findings from the VISAT longitudinal study. Occup Environ Med 72, 258–64. [DOI] [PubMed] [Google Scholar]
- 15.Wong IS, Dawson D, Van Dongen HPA. (2019) International consensus statements on non-standard working time arrangements and occupational health and safety. Ind Health 57, 135–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dawson D, Searle AK, Paterson JL. (2014) Look before you sleep: evaluating the use of fatigue detection technologies within a fatigue risk management system for the road transport industry. Sleep Med Rev 18, 141–52. [DOI] [PubMed] [Google Scholar]
- 17.Reason J .(1997) Managing the Risks of Organizational Accidents. Routledge, New York. [Google Scholar]
- 18.Dawson D, McCulloch K. (2005) Managing fatigue: it’s about sleep. Sleep Med Rev 9, 365–80. [DOI] [PubMed] [Google Scholar]
- 19.Satterfield BC, Van Dongen HPA. (2013) Occupational fatigue, underlying sleep and circadian mechanisms, and approaches to fatigue risk management. Fatigue 1, 118–36. [Google Scholar]
- 20.Lerman SE, Eskin E, Flower DJ, George EC, Gerson B, Hartenbaum N, Hursh SR, Moore-Ede M, American College of Occupational and Environmental Medicine Presidential Task Force on Fatigue Risk Management (2012) Fatigue risk management in the workplace. J Occup Environ Med 54, 231–58. [DOI] [PubMed] [Google Scholar]
- 21.Coplen M, Sussman D. (2000) Fatigue and alertness in the United States railroad industry part II: Fatigue research in the office of research and development at the federal railroad administration. Transp Res, Part F Traffic Psychol Behav 3, 221–8. [Google Scholar]
- 22.Federal Motor Carrier Safety Administration / Department of Transportation Electronic code of Federal regulations. Title 49: Transportation. Part 395: Hours of service of drivers. Electronic code of federal regulations. 2017. https://www.ecfr.gov/cgi-bin/retrieveECFR?gp=1&ty=HTML&h=L&mc=true&=PART&n=pt49.5.395. Accessed April 2017.
- 23.Clark L. (1999) The politics of regulation: a comparative—historical study of occupational health and safety regulation in Australia and the United States. Aust J Public Adm 58, 94–104. [Google Scholar]
- 24.Berg P, Appelbaum E, Bailey T, Kalleberg AL. (2004) Contesting time: international comparisons of employee control of working time. Ind Labor Relat Rev 57, 331–49. [Google Scholar]
- 25.Asgari B, Pickar P, Garay V. (2016) Karoshi and Karou-jisatsu in Japan: causes, statistics and prevention mechanisms. Asia Pac Bus Econ Perspect 4, 49–72. [Google Scholar]
- 26.Folkard S, Tucker P. (2003) Shift work, safety and productivity. Occup Med (Lond) 53, 95–101. [DOI] [PubMed] [Google Scholar]
- 27.Folkard S, Akerstedt T. (2004) Trends in the risk of accidents and injuries and their implications for models of fatigue and performance. Aviat Space Environ Med 75 Suppl, A161–7. [PubMed] [Google Scholar]
- 28.Folkard S, Lombardi DA. (2006) Modeling the impact of the components of long work hours on injuries and “accidents”. Am J Ind Med 49, 953–63. [DOI] [PubMed] [Google Scholar]
- 29.Folkard S. (1997) Black times: temporal determinants of transport safety. Accid Anal Prev 29, 417–30. [DOI] [PubMed] [Google Scholar]
- 30.Hänecke K, Tiedemann S, Nachreiner F, Grzech-Sukalo H. (1998) Accident risk as a function of hour at work and time of day as determined from accident data and exposure models for the German working population. Scand J Work Environ Health 24 Suppl 3, 43–8. [PubMed] [Google Scholar]
- 31.Lombardi DA, Sorock GS, Hauser R, Nasca PC, Eisen EA, Herrick RF, Mittleman MA. (2003) Temporal factors and the prevalence of transient exposures at the time of an occupational traumatic hand injury. J Occup Environ Med 45, 832–40. [DOI] [PubMed] [Google Scholar]
- 32.Nachreiner F, Akkermann S, Haenecke K .(2000) Fatal accident risk as a function of hours into work. In: Hornberger S, Knauth P, Costa G, Folkard S, (Eds.)Shiftwork in the 21st Century. Arbeitswissenschaft in der betrieblichen Praxis, 19–24, Peter Lang GmbH, Berlin. [Google Scholar]
- 33.Arlinghaus A, Lombardi DA, Courtney TK, Christiani DC, Folkard S, Perry MJ. (2012) The effect of rest breaks on time to injury—a study on work-related ladder-fall injuries in the United States. Scand J Work Environ Health 38, 560–7. [DOI] [PubMed] [Google Scholar]
- 34.Bhatia N, Murrell KF. (1969) An industrial experiment in organized rest pauses. Hum Factors 11, 167–74. [DOI] [PubMed] [Google Scholar]
- 35.Jones E. (1918) The administration of industrial enterprises: with special reference to factory practice. Longmans, Green and Company, Asheville. [Google Scholar]
- 36.Wyatt S, Fraser J. (1925) TStudies in repetitive work with special reference to rest pauses. IFRO Report 32, London. [Google Scholar]
- 37.Tucker P, Lombardi D, Smith L, Folkard S. (2006) The impact of rest breaks on temporal trends in injury risk. Chronobiol Int 23, 1423–34. [DOI] [PubMed] [Google Scholar]
- 38.Chen C, Xie Y. (2014) Modeling the safety impacts of driving hours and rest breaks on truck drivers considering time-dependent covariates. J Safety Res 51, 57–63. [DOI] [PubMed] [Google Scholar]
- 39.Chen C, Xie Y. (2014) The impacts of multiple rest-break periods on commercial truck driver’s crash risk. J Safety Res 48, 87–93. [DOI] [PubMed] [Google Scholar]
- 40.Totterdell P, Spelten E, Smith L, Barton J, Folkard S. (1995) Recovery from work shifts: how long does it take? J Appl Psychol 80, 43–57. [DOI] [PubMed] [Google Scholar]
- 41.European CommissionWorking Time Directive 2003/88/EC. 2003 http://ec.europa.eu/social/main.jsp?catId=706&langId=en&intPageId=205. Accessed January, 2017.
- 42.Watson NF, Badr MS, Belenky G, Bliwise DL, Buxton OM, Buysse D, Dinges DF, Gangwisch J, Grandner MA, Kushida C, Malhotra RK, Martin JL, Patel SR, Quan SF, Tasali E, Twery M, Croft JB, Maher E, Barrett JA, Thomas SM,, Heald JL, Consensus Conference PanelNon-Participating ObserversAmerican Academy of Sleep Medicine Staff (2015) Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med 11, 591–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Knauth P. (1997) Changing schedules: shiftwork. Chronobiol Int 14, 159–71. [DOI] [PubMed] [Google Scholar]
- 44.Dawson D, Reid K. (1997) Fatigue, alcohol and performance impairment. Nature 388, 235. [DOI] [PubMed] [Google Scholar]
- 45.Lamond N, Dawson D. (1999) Quantifying the performance impairment associated with fatigue. J Sleep Res 8, 255–62. [DOI] [PubMed] [Google Scholar]
- 46.Williamson AM, Feyer AM. (2000) Moderate sleep deprivation produces impairments in cognitive and motor performance equivalent to legally prescribed levels of alcohol intoxication. Occup Environ Med 57, 649–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Falleti MG, Maruff P, Collie A, Darby DG, McStephen M. (2003) Qualitative similarities in cognitive impairment associated with 24 h of sustained wakefulness and a blood alcohol concentration of 0.05%. J Sleep Res 12, 265–74. [DOI] [PubMed] [Google Scholar]
- 48.Roehrs T, Burduvali E, Bonahoom A, Drake C, Roth T. (2003) Ethanol and sleep loss: a “dose” comparison of impairing effects. Sleep 26, 981–5. [DOI] [PubMed] [Google Scholar]
- 49.Rouch I, Wild P, Ansiau D, Marquié JC. (2005) Shiftwork experience, age and cognitive performance. Ergonomics 48, 1282–93. [DOI] [PubMed] [Google Scholar]
- 50.Sallinen M, Kecklund G. (2010) Shift work, sleep, and sleepiness—differences between shift schedules and systems. Scand J Work Environ Health 36, 121–33. [DOI] [PubMed] [Google Scholar]
- 51.International Labour (1988) Office International Labour Conference 76th session (Report IV (1), Night Work). ILO, Geneva.
- 52.Åkerstedt T, Kecklund G, Gillberg M, Lowden A, Axelsson J. (2000) Sleepiness and days of recovery. Transp Res, Part F Traffic Psychol Behav 3, 251–61. [Google Scholar]
- 53.Kecklund G, Akerstedt T, Goranson B, Soderberg K .(1994) Omlaggning av skiftschema: konsekvernser for vdbefnnande, hilsa, somn, vakenhet och arbetstrivsel. Resulta- trapport 2: FrAgeformuliir, dagbok och halsoundersokening. In: Stress Research Reports. Stockholm. [Google Scholar]
- 54.Short MA, Agostini A, Lushington K, Dorrian J. (2015) A systematic review of the sleep, sleepiness, and performance implications of limited wake shift work schedules. Scand J Work Environ Health 41, 425–40. [DOI] [PubMed] [Google Scholar]
- 55.Health and Safety Executive The development of a fatigue/risk index for shiftworkers. HSE Research Report Series #446. 2006. http://www.hse.gov.uk/research/rrpdf/rr446.pdf. Accessed September, 2017.
- 56.Arora VM, Georgitis E, Woodruff JN, Humphrey HJ, Meltzer D. (2007) Improving sleep hygiene of medical interns: can the sleep, alertness, and fatigue education in residency program help? Arch Intern Med 167, 1738–44. [DOI] [PubMed] [Google Scholar]
- 57.Chen PH, Kuo HY, Chueh KH. (2010) Sleep hygiene education: efficacy on sleep quality in working women. J Nurs Res 18, 283–9. [DOI] [PubMed] [Google Scholar]
- 58.Suzuki E, Tsuchiya M, Hirokawa K, Taniguchi T, Mitsuhashi T, Kawakami N. (2008) Evaluation of an internet-based self-help program for better quality of sleep among Japanese workers: a randomized controlled trial. J Occup Health 50, 387–99. [DOI] [PubMed] [Google Scholar]
- 59.Nishinoue N, Takano T, Kaku A, Eto R, Kato N, Ono Y, Tanaka K. (2012) Effects of sleep hygiene education and behavioral therapy on sleep quality of white-collar workers: a randomized controlled trial. Ind Health 50, 123–31. [DOI] [PubMed] [Google Scholar]
- 60.Kaku A, Nishinoue N, Takano T, Eto R, Kato N, Ono Y, Tanaka K. (2012) Randomized controlled trial on the effects of a combined sleep hygiene education and behavioral approach program on sleep quality in workers with insomnia. Ind Health 50, 52–9. [DOI] [PubMed] [Google Scholar]
- 61.Kakinuma M, Takahashi M, Kato N, Aratake Y, Watanabe M, Ishikawa Y, Kojima R, Shibaoka M, Tanaka K. (2010) Effect of brief sleep hygiene education for workers of an information technology company. Ind Health 48, 758–65. [DOI] [PubMed] [Google Scholar]
- 62.DeJoy DM. (2005) Behavior change versus culture change: divergent approaches to managing workplace safety. Saf Sci 43, 105–29. [Google Scholar]
- 63.Cooper M. (2009) Behavioral safety interventions: a review of process design factors. Saf Manag (February), 36–46. [Google Scholar]
- 64.Holbrook MI, White MH, Hutt MJ. (1994) Increasing awareness of sleep hygiene in rotating shift workers: arming law-enforcement officers against impaired performance. Percept Mot Skills 79, 520–2. [DOI] [PubMed] [Google Scholar]
- 65.Rosekind MR, Gregory KB, Mallis MM. (2006) Alertness management in aviation operations: enhancing performance and sleep. Aviat Space Environ Med 77, 1256–65. [DOI] [PubMed] [Google Scholar]
- 66.Scott LD, Hofmeister N, Rogness N, Rogers AE. (2010) An interventional approach for patient and nurse safety: a fatigue countermeasures feasibility study. Nurs Res 59, 250–8. [DOI] [PubMed] [Google Scholar]
- 67.Morin CM, Hauri PJ, Espie CA, Spielman AJ, Buysse DJ, Bootzin RR. (1999) Nonpharmacologic treatment of chronic insomnia. An American Academy of Sleep Medicine review. Sleep 22, 1134–56. [DOI] [PubMed] [Google Scholar]
- 68.Rosekind MR, Gander PH, Gregory KB, Smith RM, Miller DL, Oyung R, Webbon LL, Johnson JM. (1996) Managing fatigue in operational settings 2: An integrated approach. Behav Med 21, 166–70. [DOI] [PubMed] [Google Scholar]
- 69.Tepas DI. (1993) Educational programmes for shiftworkers, their families, and prospective shiftworkers. Ergonomics 36, 199–209. [Google Scholar]
- 70.Neuberger GB. (2003) Measures of fatigue: the fatigue questionnaire, fatigue severity scale, multidimensional assessment of fatigue scale, and short form-36 vitality (energy/fatigue) subscale of the short form health survey. Arthritis Rheum 49 S5, S175–83. [Google Scholar]
- 71.Aaronson LS, Teel CS, Cassmeyer V, Neuberger GB, Pierce J, Press AN, Williams PD, Wingate A. (1999) State of the science defining and measuring fatigue. J Nurs Scholarsh 31, 45–50. [DOI] [PubMed] [Google Scholar]
- 72.Bayly M, Fildes B, Regan M, Young K. (2007) Review of crash effectiveness of intelligent transport systems. Emergency 3. [Google Scholar]
- 73.Kerick S, Metcalf J, Feng T, Ries A, McDowell K .(2013) Review of fatigue management technologies for enhanced military vehicle safety and performance. Report ARL-TR-6571. Technical Report; U.S. Army Research Laboratory.
- 74.Palmer K, Cox R.A (2000) general framework for assessing fitness for work. In: Palmer K, Cox R, Brown I (Eds.), Fitness for Work: the Medical Aspects, 4th Ed., 1–20, Oxford University Press. [Google Scholar]
- 75.Serra C, Rodriguez MC, Delclos GL, Plana M, Gómez López LI, Benavides FG. (2007) Criteria and methods used for the assessment of fitness for work: a systematic review. Occup Environ Med 64, 304–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Bergasa LM, Nuevo J, Sotelo MA, Barea R, Lopez ME. (2006) Real-time system for monitoring driver vigilance. IEEE Trans Intell Transp Syst 7, 63–77. [Google Scholar]
- 77.D’Orazio T, Leo M, Guaragnella C, Distante A. (2007) A visual approach for driver inattention detection. Pattern Recognit 40, 2341–55. [Google Scholar]
- 78.Dinges DF, Mallis MM, Maislin G, Powell JW., IV 1998) Evaluation of techniques for ocular measurement as an index of fatigue and as the basis for alertness management. Washington DC. http://trid.trb.org/view.aspx?id=647942. Accessed January, 2017.
- 79.American Academy of Sleep Medicine (2005) International classification of sleep disorders, diagnostic and coding manual. 2nd Ed. American Academy of Sleep Medicine, Westchester. [Google Scholar]
- 80.Abtahi S (2012) Driver drowsiness monitoring based on yawning detection. MS Thesis. University of Ottawa; 2012. https://ruor.uottawa.ca/bitstream/10393/23295/1/Abtahi_Shabnam_2012_thesis.pdf. Accessed February, 2017.
- 81.Xue T, Nan N, Fan M, Yong J .(2009) Head pose estimation using isophote features for driver assistance systems. Proceedings of the IEEE Intelligent Vehicles Symposium. Xi’an, China.
- 82.Murphy-Chutorian E, Trivedi MM. (2010) Head pose estimation and augmented reality tracking: an integrated system and evaluation for monitoring driver awareness. IEEE Trans Intell Transp Syst 11, 300–11. [Google Scholar]
- 83.Nakamura T, Matsuda T, Maejima A, Morishima S .(2013) Driver drowsiness estimation using facial wrinkle feature. 40th International Conference and Exhibition on Computer Graphics and Interactive Techniques, 20, Anaheim, California.
- 84.Nasoz F, Ozyer O, Lisetti C, Finkelstein N .(2002) Multimodal affective driver interfaces for future cars. Proceedings of the tenth ACM international conference on Multimedia, 319–22, Juan les Pins, France.
- 85.Lal SKL, Craig A. (2001) A critical review of the psychophysiology of driver fatigue. Biol Psychol 55, 173–94. [DOI] [PubMed] [Google Scholar]
- 86.Derosière G, Dalhoumi S, Perrey S, Dray G, Ward T. (2014) Towards a near infrared spectroscopy-based estimation of operator attentional state. PLoS One 9, e92045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kang HB. (2013) Various approaches for driver and driving behavior monitoring: A review. Proc IEEE Int Conf Comput Vis Workshops, 616–23. [Google Scholar]
- 88.Yu X. (2009) Real-time nonintrusive detection of driver drowsiness. Univesrity of Minnesota Center for Transportation Studies. Technical report # CTS 09–15. [Google Scholar]
- 89.Baek HJ, Chung GS, Kim KK, Park KS. (2012) A smart health monitoring chair for nonintrusive measurement of biological signals. IEEE Trans Inf Technol Biomed 16, 150–8. [DOI] [PubMed] [Google Scholar]
- 90.Lee B, Chung W. (2012) Multi-classifier for highly reliable driver drowsiness detection in Android platform. Biomed Eng Appl Basis Commun 24, 147–54. [Google Scholar]
- 91.Torkkola K, Massey N, Wood C. (2004) Driver inattention detection through intelligent analysis of readily available sensors. IEEE Int Conf Intell Transp Syst, 326–31. [Google Scholar]
- 92.Liu CC, Hosking SG, Lenné MG. (2009) Predicting driver drowsiness using vehicle measures: recent insights and future challenges. J Safety Res 40, 239–45. [DOI] [PubMed] [Google Scholar]
- 93.Wylie C, Shultz T, Miller J, Mittler M, Mackie R (1996)Commercial motor vehicle driver fatigue and alertness study: technical summary. FHWA-MC-97–001. [Google Scholar]
- 94.Uno H. (2003) Detecting decline in arousal level using combined physiological and behavioral measures. JARI Res J 25, 315–8. [Google Scholar]
- 95.Otmani S, Pebayle T, Roge J, Muzet A. (2005) Effect of driving duration and partial sleep deprivation on subsequent alertness and performance of car drivers. Physiol Behav 84, 715–24. [DOI] [PubMed] [Google Scholar]
- 96.Sahayadhas A, Sundaraj K, Murugappan M. (2012) Detecting driver drowsiness based on sensors: a review. Sensors (Basel) 12, 16937–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ingre M, Åkerstedt T, Peters B, Anund A, Kecklund G. (2006) Subjective sleepiness, simulated driving performance and blink duration: examining individual differences. J Sleep Res 15, 47–53. [DOI] [PubMed] [Google Scholar]
- 98.Yang G, Lin Y, Bhattacharya P. (2010) A driver fatigue recognition model based on information fusion and dynamic Bayesian network. Inf Sci Ny 180, 1942–54. [Google Scholar]
- 99.Balkin TJ, Horrey WJ, Graeber RC, Czeisler CA, Dinges DF. (2011) The challenges and opportunities of technological approaches to fatigue management. Accid Anal Prev 43, 565–72. [DOI] [PubMed] [Google Scholar]
- 100.Hartley L, Horberry T, Mabbott N, Krueger GP. (2000) Review of fatigue detection and prediction technologies. [Google Scholar]
- 101.Cabon P, Deharvengt S, Grau JY, Maille N, Berechet I, Mollard R. (2012) Research and guidelines for implementing Fatigue Risk Management Systems for the French regional airlines. Accid Anal Prev 45 Suppl, 41–4. [DOI] [PubMed] [Google Scholar]
- 102.Enform Canada (2015) Fatigue Risk Management: A Program Development Guide. Calgary, AB; http://www.enform.ca/resources/detail/38/fatigue-management. Accessed March, 2017.
- 103.Randolph SA. (2015) Fatigue risk management. Workplace Health Saf 63, 236. [DOI] [PubMed] [Google Scholar]
- 104.Steege LM, Pinekenstein BJ, Rainbow JG, Arsenault Knudsen É. (2017) Addressing occupational fatigue in nurses: current state of fatigue risk management in hospitals, part 2. J Nurs Adm 47, 484–90. [DOI] [PubMed] [Google Scholar]
- 105.Wong LR, Flynn-Evans E, Ruskin KJ. (2018) Fatigue risk management: the impact of anesthesiology residents’ work schedules on job performance and a review of potential countermeasures. Anesth Analg 126, 1340–8. [DOI] [PubMed] [Google Scholar]
- 106.Eiter BM, Steiner L, Kelhart A. (2014) Application of fatigue management systems: small mines and low technology solutions. Min Eng 66, 69–75. [PMC free article] [PubMed] [Google Scholar]
- 107.Gander P, Hartley L, Powell D, Cabon P, Hitchcock E, Mills A, Popkin S. (2011) Fatigue risk management: Organizational factors at the regulatory and industry/company level. Accid Anal Prev 43, 573–90. [DOI] [PubMed] [Google Scholar]
- 108.Gander PH, Mangie J, Van Den Berg MJ, Smith AAT, Mulrine HM, Signal TL. (2014) Crew fatigue safety performance indicators for fatigue risk management systems. Aviat Space Environ Med 85, 139–47. [DOI] [PubMed] [Google Scholar]
- 109.International Air Transport Association Fatigue Management Guide for Airline Operators. Montreal, Canada; 2015. https://www.iata.org/publications/Documents/Fatigue-Management-Guide_Airline%20Operators.pdf. Accessed May, 2017.
- 110.International Civil Aviation Organization Fatigue Risk Management Manual for Regulators 2012. Edition. https://www.icao.int/safety/fatiguemanagement/FRMS Tools/Doc 9966-FRMS Manual for Regulators.pdf. Accessed May, 2017.
- 111.Martin-Gill C, Higgins JS, Van Dongen HPA, Buysse DJ, Thackery RW, Kupas DF, Becker DS, Dean BE, Lindbeck GH, Guyette FX, Penner JH, Violanti JM, Lang ES, Patterson PD. (2018) Proposed performance measures and strategies for implementation of the fatigue risk management guidelines for emergency medical services. Prehosp Emerg Care 22 S1, 102–9. [DOI] [PubMed] [Google Scholar]
- 112.American Public Transportation Association Safety Management System Manual: Public Passenger Transportation Systems (2016) www.trbtss.org/wp-content/uploads/2016/03/APTA-Safety-Management-System-Manual.pdf. Accessed May, 2017.
- 113.Federal Aviation Administration Safety Management System Components (2017) https://www.faa.gov/about/initiatives/sms/explained/components/. Accessed May, 2017.