Abstract
Renal capillary hemangiomas are rare and benign vascular tumors which are typically incidentally discovered on imaging. Surgical excision is often performed, as imaging appearance is similar to malignant lesions. Renal hemangiomas are typically solitary and unilateral. We present a rare case of multiple renal capillary hemangiomas in a patient with end-stage renal disease. Two hemangiomas were detected on imaging and 2 smaller hemangiomas were detected upon pathological evaluation, suggesting there may be a wider prevalence of smaller, radiographically-occult renal hemangiomas.
Keywords: Renal capillary hemangioma, End-stage renal disease
Introduction
Renal capillary hemangiomas are rare, often underrecognized, benign vascular tumors [1]. In small case series, these lesions have been associated with other diseases including end-stage renal disease, acquired cystic kidney disease, polycythemia, and renal cell carcinoma [2], [3], [4], [5], [6]. Patients may present with abdominal pain and hematuria, but are more commonly asymptomatic. Therefore, these tumors are often initially discovered incidentally on imaging. Renal hemangiomas pose diagnostic and clinical dilemmas because of similar radiologic characteristics to other lesions including renal cell carcinoma and angiosarcoma. Surgical excision is often indicated due to the similar appearance to malignant lesions or in cases of significant symptoms such as hemorrhage [7], [8], [9]. Definitive diagnosis is based on pathology demonstrating aggregates of capillary-sized vascular channels with CD31+ endothelial cells [1], [6]. We present a rare case of multiple renal capillary hemangiomas in a patient with end-stage renal disease.
Case presentation
A 23-year-old male with end-stage renal disease secondary to C1q-positive focal segmental glomerulosclerosis on hemodialysis was referred for complete abdominal ultrasound for renal pretransplant evaluation. He reported no abdominal pain or hematuria at prior clinical visits. His laboratory studies were only remarkable for longstanding anemia (Hgb 11.5 g/dL) and thrombocytopenia (111 × 103 per µL), with no red blood cells on urinalysis. Ultrasound demonstrated a 3.3 × 2.9 × 4.0 cm isoechoic mass with prominent peripheral flow in the mid-lower zone of the left kidney (Fig. 1).
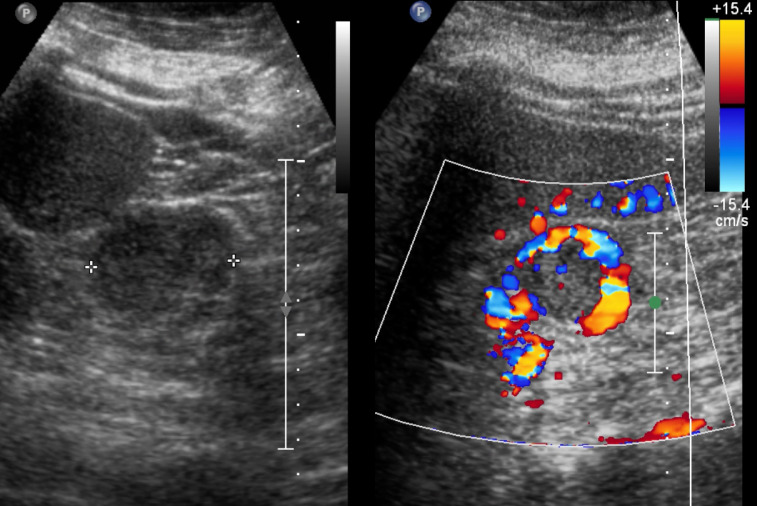
Fig. 1.
Ultrasound images of the left kidney without and with Doppler demonstrate a 4.0 cm isoechoic mass at the left mid-lower pole with peripheral Doppler flow.
A subsequent computed tomography examination with and without intravenous contrast demonstrated bilateral atrophic kidneys with 2 cortical-based lesions within the left kidney measuring up to 2.1 cm at the upper pole and 3.0 cm at the midzone. These lesions demonstrated noncontrast hypoattenuation (Fig. 2), arterial enhancement (Fig. 3), and central hypoattenuating areas that persisted on portal venous phase (Fig. 4), which raised concern for malignancy. After extensive discussion, the patient wished to defer biopsy and proceed with radical nephrectomy. The patient underwent an uncomplicated laparoscopic left radical nephrectomy and adjacent lymphadenectomy.
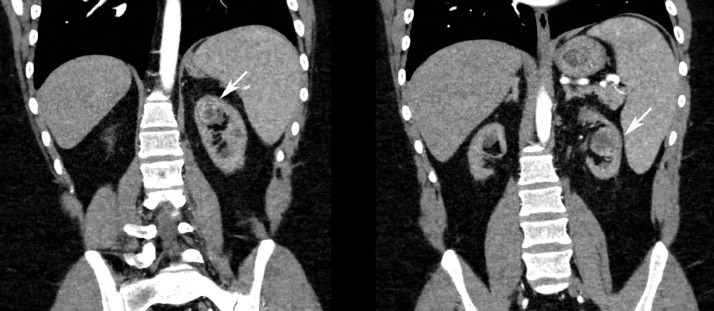
Fig. 2.
Noncontrast coronal CT images demonstrate hypoattenuating lesions in the left kidney upper pole and midzone.
Fig. 3.
Arterial phase contrast-enhanced coronal CT images demonstrate enhancing lesions in the left kidney upper pole and midzone with central hypoattenuating areas.
Fig. 4.
Portal venous phase contrast-enhanced coronal CT images demonstrate enhancing lesions in the left kidney upper pole and midzone with central hypoattenuating areas.
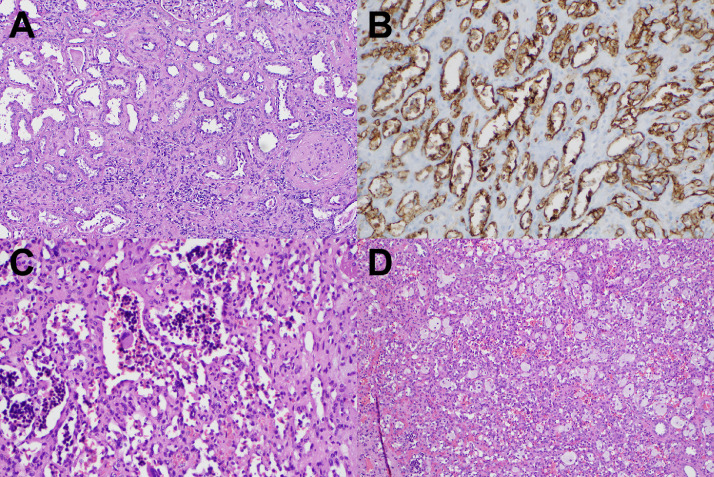
Surgical pathology demonstrated findings consistent with end-stage renal disease and 4 masses: in the mid-pole measuring up to 2.3 cm and located 3.2 cm from the renal vein, 4.2 cm from the urethral margin, and 0.4 cm from the cortex margin; at the lower pole measuring up to 1.1 cm and located 4.4 cm from the renal vein margin, 6.4 cm from the urethral margin, and 0.8 cm from the cortex margin; and 2 masses in the upper pole measuring up to 1.9 cm and 0.6 cm. The masses demonstrated characteristic histopathological features of benign capillary hemangioma (Fig. 5). There was no evidence of malignancy. At 3 month follow-up, the patient is doing well.
Fig. 5.
Histopathology demonstrates findings of end-stage renal disease including tubular thyroidization on hematoxylin and eosin staining (A), vascular prominence with CD31-positivity on immunohistochemical staining (B), characteristic appearance of hemangioma with associated foamy histiocytes on hematoxylin and eosin staining on high power (C), and low power magnification (D).
Discussion
Renal hemangiomas are exceptionally rare, with approximately 200 previously reported cases [1]. Renal hemangiomas are typically solitary and unilateral [6], [8]. However, in our case, 2 hemangiomas were detected on imaging, and 2 additional smaller peri-centimeter and sub-centimeter hemangiomas were detected only on pathological evaluation. These findings suggest there may be a wider prevalence of smaller, radiographically-occult renal hemangiomas. Previous studies have reported similarly radiographically occult hemangiomas in patients with ESRDs [1], [6]. This may suggest that the tumor may be more common than previously considered. Further research is needed to characterize the relationship between capillary hemangiomas and ESRD.
Renal hemangiomas present a clinical challenge, as differentiating them from malignant lesions is nearly impossible clinically and radiographically. It is especially challenging in ESRD patients because kidneys with chronic damage have a propensity to develop both benign vascular tumors and epithelial neoplasms [1]. Currently, imaging does little to alleviate the challenge. Ultrasound findings are nonspecific and do not aid in distinguishing renal hemangiomas from other tumors. It has been suggested that central hypoattenuation on computed tomography, which was present in our case, may indicate hemangioma as a differential consideration [5]. Given the lack of definitive imaging characteristics, biopsy or excision is necessary for final diagnosis. Our patient opted for radical nephrectomy given the presence of ESRD, planned renal transplant, and desire for definitive treatment of possible malignancy,
Further research is needed to explore the prevalence, associations, and radiographic characteristics of renal hemangiomas. In the interim, the possibility of a benign renal hemangioma should be considered in patients with vascular renal lesions, and counseling and treatment decisions made accordingly.
Footnotes
Declarations of interest: None.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2019.03.027.
Appendix. Supplementary materials
References
- 1.Büttner M., Kufer V., Brunner K., Hartmann A., Amann K., Agaimy A. Benign mesenchymal tumours and tumour-like lesions in end-stage renal disease. Histopathology. 2013;62:229–236. doi: 10.1111/j.1365-2559.2012.04349.x. [DOI] [PubMed] [Google Scholar]
- 2.Lee H.S., Koh B.H., Kim J.W. Radiologic findings of renal hemangioma: report of three cases. Korean J. Radiol. 2000;1:60–63. doi: 10.3348/kjr.2000.1.1.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown J.G., Folpe A.L., Rao P., Lazar A.J., Paner G.P., Gupta R. Primary vascular tumors and tumor-like lesions of the kidney: a clinicopathologic analysis of 25 cases. Am J Surg Pathol. 2010;34:942–949. doi: 10.1097/PAS.0b013e3181e4f32a. [DOI] [PubMed] [Google Scholar]
- 4.Leak B.J., Javidan J., Dagher R. A rare case of renal hemangioma presenting as polycythemia. Urology. 2001;57:975. doi: 10.1016/s0090-4295(01)00910-4. [DOI] [PubMed] [Google Scholar]
- 5.Beamer M., Love M., Ghasemian S. Renal capillary haemangioma associated with renal cell carcinoma and polycythaemia in acquired cystic disease. BMJ Case Rep. 2017;2017: doi: 10.1136/bcr-2017-220936. 975iv–v. bcr-2017-220936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kryvenko O.N., Haley S.L., Smith S.C., Shen S.S., Paluru S., Gupta N.S. Haemangiomas in kidneys with end-stage renal disease: a novel clinicopathological association. Histopathology. 2014;65:309–318. doi: 10.1111/his.12394. [DOI] [PubMed] [Google Scholar]
- 7.Mehta V., Ananthanarayanan V., Antic T., Krausz T., Milner J., Venkataraman G. Primary benign vascular tumors and tumorlike lesions of the kidney: a clinicopathologic analysis of 15 cases. Virchows Arch. 2012;461:669–676. doi: 10.1007/s00428-012-1333-9. [DOI] [PubMed] [Google Scholar]
- 8.Vasquez E., Aulivola B., Picken M., Milner J. Vol. 79. 2012. Capillary hemangioma masquerading as a renal artery pseudoaneurysm; pp. 987–989. (Urology). [DOI] [PubMed] [Google Scholar]
- 9.Oikawa M., Hatakeyama S., Hamano I., Tanaka T., Tanaka Y., Narita T. Capillary hemangioma in renal hilum; a case report. Hinyokika Kiyo. 2014;60:33–37. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.