Abstract
Introduction:
Health guidelines suggest that pregnant women should participate in daily physical activity, yet rarely do they meet these guidelines. Means to enhance accessibility of physical activity for pregnant women are required, and yoga has been suggested as a possible method to enhance women’s sense of confidence and competence with physical activity. In this pilot study, our primary aim is to evaluate pregnant women’s perceptions about their lived experience of an intervention which integrates a low-intensity form of physical activity, yoga, into prenatal care; our secondary aim is to evaluate changes in participants’ self-efficacy for physical activity and time spent in physical activity over time.
Methods:
Held in an outpatient obstetrics department of an urban hospital system in the United States, this pilot study enrolled 16 pregnant women to participate in the intervention throughout their pregnancy. We explored participants’ lived experience of the intervention using qualitative methods (phenomenology). Means, variances, and covariances were calculated for the 2 measures (self-efficacy and time spent in physical activity) over the intervention period.
Results:
Qualitative findings from focus groups suggest that it is acceptable for prenatal yoga to be integrated into group prenatal care classes and women reported increased confidence with physical activity during pregnancy. Participants did not consider the intervention to fit within the traditional definition of exercise. Women reported increased amounts of time spent in physical activity from baseline to the end of pregnancy, but there were no statistically significant changes in self-efficacy over time.
Discussion:
The integration of gentle physical activity into the group prenatal care model warrants further attention for potential benefits with regard to maternal physical and mental wellness.
Keywords: pregnancy, physical activity, yoga
Introduction
The American College of Obstetricians and Gynecologists (ACOG) recommends 20 to 30 minutes of physical activity on at least five days per week for pregnant women, unless the individual has contraindications (eg, preterm rupture of membranes, cervical insufficiency, placenta previa).1 However, cross-sectional data from sources such as the National Health and Nutrition Examination Survey and others report that less than 20% of pregnant women engage in activity at that level.2-4 Despite frequent contact with health-care providers during pregnancy, many women report a lack of knowledge and/or self-efficacy for engaging in physical activity or identify other barriers such as lack of time and lack of facilities/resources.5-7
Research is warranted to evaluate methods to help pregnant women increase physical activity, even light-intensity activity. One such method is to expose women to activities which increase a sense of confidence and competence with activity.8 Prenatal yoga is a form of low-intensity mindful physical activity that could be a “gateway” to increased motivation for physical activity.9-12 Women have expressed interest in prenatal yoga because it is gentle, seems to be a safe form of physical activity, and can occur in a group-based supportive environment.11,13-15 Although studies have emerged recently that evaluate behavioral/ physical activity interventions focused on weight management in pregnancy,16,17 few studies to date have evaluated the integration of an light-intensity physical activity intervention within an existing model of prenatal care. Hence, the primary goal of this pilot study was to explore women’s perceptions about their experiences with the integration of prenatal yoga into routine CenteringPregnancy prenatal sessions (Centering Pregnancy Care Plus Yoga [CPC + Y]). The second aim of the study was to explore preliminary effects of CPC + Y on time spent in physical activity over time and on women’s self-efficacy for physical activity.
Methods
The study protocol was reviewed and approved by the institutional review board of Virginia Commonwealth University. Conducted in the obstetrics department of the university’s health system, this pilot study used an embedded mixed-methods approach. Eligible participants were adult, English-speaking pregnant women who were participating in CPC for prenatal care with no ACOG contraindications to physical activity. After informed consent and enrollment, participants engaged in the CPC + Y intervention, involving a 30-minute manualized yoga session taught by experienced prenatal yoga instructors, at the end of each CPC meeting.
For aim 1 (participants’ experiences with intervention), focus groups were held at the 6-weeks postpartum visit in the obstetrics office, using questions focused on the phenomenon of physical activity during pregnancy. A phenomenological qualitative approach was used for the analysis of this qualitative data, with initial analyses by 2 authors (P.K. and C.A.); to enhance rigor, a third author (S.M.) provided an independent review and we used participant checking to confirm themes.18-20 For aim 2 (preliminary effects of CPC + Y), means, variances, covariances, and 95% confidence intervals were calculated for the pre-/post-data time points and a Wilcoxon Signed-Rank Test was conducted. The Physical Activity Self-Efficacy Scale (PASES) is an 8-question scale which contains items about self-management of physical activities and social support regarding physical activity.21,22 The Pregnancy Physical Activity Questionnaire (PPAQ) was used to determine amount of time of engagement in physical activity.23
Results
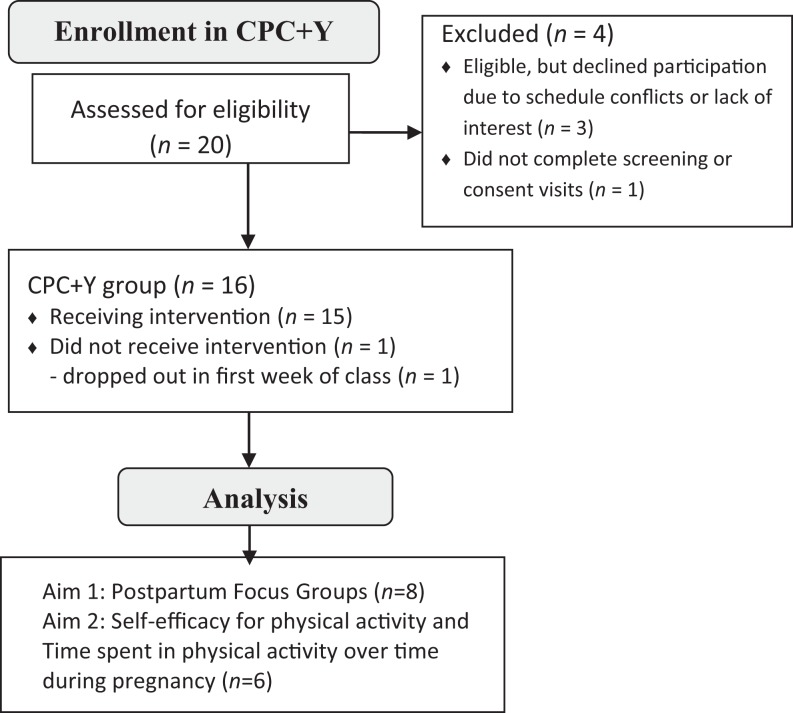
The study involved 16 women who participated in the CPC + Y intervention, 50% of which were white and 50% were black/African American, at a mean age of 29.3 (6.5); see Figure 1 for the CONSORT diagram. Most participants were married (n = 10; 63%) and had a part- or full-time job. All participants had at least a high-school education or equivalent and reported at least weekly physical activity prior to starting the study.
Figure 1.
CONSORT diagram.
Aim 1: Evaluate the Lived Experience of Participants With CPC + Y
Eight postpartum women were able to participate in the focus groups holding their 6-week old infants in their laps. Two key themes arose from the focus group discussions: First, participants reported uncertainty about safe exercise during pregnancy and were relieved that prenatal yoga was offered as an activity. One participant reported that the yoga classes started here and I could see what was okay…and what wasn’t okay to push the limit with. Participants felt a sense of relief that they could engage in the yoga classes in a safe environment and that they knew the classes were appropriate because their clinicians were aware of their participation. Multiple participants suggested that the yoga classes served as a motivator to engaging in other physical activity outside of class. For example, one women expressed that the participation in the CPC + Y classes helped provide motivation to add an additional yoga class to her week: I started going to the yoga class on Tuesday mornings and these classes introduced me to that and it was a great way for me to stay active and know what was okay for me to do. Of note, participants felt that the classes were too short and gentle to be considered true exercise. As suggested by one participant: It was only 30 minutes and I would have liked for it to be even longer; several participants echoed this sentiment stating that they desired more time in class.
Second, participants found that physical activity in the form of yoga integrated with CPC was extremely convenient. For example, one participant stated having it at the end of our Centering session made it really convenient for those of us who were able to stay afterwards, that made it really helpful. For this and several other participants, the novelty of yoga as a physical activity which was easily integrated into their prenatal care schedule was an exciting prospect when learning about the study. She stated she was excited to sign up once she realized, there’s a free yoga class that’s conveniently timed right after our prenatal appointment. Despite the convenience of integrating yoga into the prenatal care schedule, several participants mentioned that the schedule and timing could benefit from some adjustments in terms of end-time or conflict with children’s school schedules.
Aim 2: Explore Preliminary Effects of CPC + Y
With regard to time spent in physical activity, the mean and median number of days active in past week (PPAQ1) and number of days active in usual week (PPAQ2) scores for the intervention participants who completed the baseline and end-of-intervention visits (n = 6) are presented in Table 1. There were no significant differences in activity in the past week (PPAQ1; P = .125) nor activity in a typical week (PPAQ2; P = 1.000). There was a trend in increased amount of time participants engaged in physical activity, from a mean of 4.58 h/wk in early pregnancy to 7.21 h/wk in late pregnancy (P = .0938). There were no significant changes over time in PASES.
Table 1.
Self-Efficacy for Physical Activity and Time Spent in Physical Activity.
| Measures | Baseline (Early Pregnancy), n = 6 | End of Intervention (Late Pregnancy), n = 6 | P Valuea | Effect Size | ||||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median | (Min, Max) | Mean (SD) | Median | (Min, Max) | |||
| Self-Efficacy for Physical Activity (PASES) | 26.50 (3.27) | 26.00 | (23.00, 32.00) | 25.67 (1.75) | 25.00 | (24.00, 29.00) | 0.8750 | 0.2246 |
| Number of days physically active for at least 30 minutes in past week (days; PPAQ-1) | 4.33 (1.97) | 4.00 | (2.00, 7.00) | 5.17 (1.47) | 5.50 | (3.00, 7.00) | 0.1250 | 1.1069 |
| Number of days physically active for at least 30 minutes in a typical week (days; PPAQ-2) | 4.67 (1.63) | 4.50 | (3.00, 7.00) | 4.67 (1.63) | 4.50 | (3.00, 7.00) | 1.0000 | 0.0001 |
| Duration of time per week during this trimester of pregnancy engaged in physical activity (hours; sum of PPAQ-3 to -9) | 4.58 (3.89) | 3.00 | (1.50, 11.00) | 7.21 (4.47) | 6.13 | (3.00, 15.75) | 0.0938 | 1.0242 |
Abbreviation: PPAQ, Pregnancy Physical Activity Questionnaire.
aWilcoxon Signed-Rank Test.
Discussion
This study’s qualitative findings suggest that participants perceive the integration of prenatal yoga into group prenatal as feasible and acceptable. Participants in this study reported that group-based classes increased feelings of safety surrounding physical activity during pregnancy. Historically, pregnant women were advised to abstain from physical activity,24 and despite that several organizations have promoted healthy physical activity in pregnancy for weight management and stress relief,25,26 there remains confusion about what activities are “safe” during pregnancy and many women lack self-efficacy for physical activity.13,27 Participants expressed appreciation for the integration of yoga with prenatal yoga to address this uncertainty about safety.
The quantitative results from this study did not reveal significant changes over time, but participants reported trending increased amounts of physical activity from early to late pregnancy. With regard to the lack of changes over time in self-efficacy for physical activity, there are several possible explanations for these findings. Although the women reported enjoying the yoga sessions integrated into the CPC groups and perceived it to be beneficial or their healthy and the health of their baby, they did not view it as a regular form of “exercise” or physical activity, particularly given that the class was only 30 minutes. Similar results were found in a previous study reporting women viewed yoga as a low-intensity and relaxing exercise.11 Future research should include a consideration of yoga as a form of physical activity and should evaluate the appropriateness of the measures (eg, PASES, PPAQ) in this population.
Although this study used innovative approaches to understand an area that is under studied, it has some limitations: the small sample size, lack of randomized control group, and representation of 2 racial/ethnic groups (white and black/African American) presents limitations to internal and external validity. However, this was designed to be a pilot study with the primary goal of evaluating acceptability and determining intervention effects to support the development of a future randomized controlled trial. We recommend that future randomized controlled studies should include a comparison group that may control for time and attention, recruitment of a racially/ethnically heterogeneous sample population, and an appropriately powered sample size to account for the natural variability of physical activity in pregnant women.
Conclusion
Prenatal yoga integrated into group prenatal care was overall well-received by the women who participated and has the potential to be integrated on a wider scale in order to reach more women. Although there were minimal changes in quantitative outcome measures over time, participants in the intervention reported increased amounts of physical activity from early to late pregnancy. Prenatal yoga as a form of gentle physical activity warrants further attention for the possibility of integrating into group prenatal care and for its potential benefits with regard to maternal physical and mental wellness. Future research is required to evaluate whether and how yoga completed in a group may also contribute to positive physical activity experiences and contribute to physical activity self-efficacy and enhance motivation for future physical activity.
Acknowledgments
The authors would like to acknowledge Prachi Desai, Kirsten Olsen, and Tamala Gondwe for their assistance with the study and in the preparation of this manuscript. The authors honor the memory of Dr. Saba Masho.
Author Biographies
Patricia Kinser, PhD, WHNP-BC, RN, FNAP, FAAN is an associate professor at the Virginia Commonwealth University School of Nursing with a research, teaching, and practice focus on integrative health interventions for enhancing wellness in women across the life span.
Nancy Jallo, PhD, RNC, FNP-BC, WHNP-BC, CNS, is an associate professor at the Virginia Commonwealth University School of Nursing. Her biobehavioral research is focused on perinatal stress and anxiety in women and infants, including the development and testing of interventions to improve health and wellness outcomes.
Leroy Thacker, PhD, is an associate professor in the Virginia Commonwealth University Department of Biostatistics and collaborates on numerous projects with colleagues in the School of Nursing.
Christine Aubry, RN, is a research assistant at the Virginia Commonwealth University School of Nursing and a registered nurse at the Virginia Commonwealth University Health System.
Saba Masho, MD, MPH, DrPH, was a professor at the Virginia Commonwealth University, Department of Family Medicine and Population Health, Division of Epidemiology. She died in 2018 after a rich and productive career focused on the health and well-being of women and their families.
Authors’ Note: This study was registered on clinicaltrials.gov as NCT02873481.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by a Sigma Theta Tau International/Southern Nursing Research Society Grant (PI: Kinser); VCU School of Nursing Internal Grand Funding (PI: Kinser); the National Institute on Minority Health and Health Disparities (5P60MD002256, PI: Strauss).
ORCID iD: Patricia Kinser  https://orcid.org/0000-0001-9319-8922
https://orcid.org/0000-0001-9319-8922
References
- 1. American College for Obstetricians and Gynecologists. ACOG Committee Opinion No. 650: physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126(6):e135–e142. doi:10.1097/AOG.0000000000001214. [DOI] [PubMed] [Google Scholar]
- 2. Gjestland K, Bo K, Owe KM, Eberhard-Gran M. Do pregnant women follow exercise guidelines? Prevalence data among 3482 women, and prediction of low-back pain, pelvic girdle pain and depression. Br J Sports Med. 2013;47(8):515–520. doi:10.1136/bjsports-2012-091344. [DOI] [PubMed] [Google Scholar]
- 3. Evenson KR, Wen F. National trends in self-reported physical activity and sedentary behaviors among pregnant women: NHANES 1999-2006. Prev Med (Baltim). 2010;50(3):123–128. doi:10.1016/j.ypmed.2009.12.015. [DOI] [PubMed] [Google Scholar]
- 4. Evenson KR, Wen F. Prevalence and correlates of objectively measured physical activity and sedentary behavior among US pregnant women. Prev Med (Baltim). 2011;53(1-2):39–43. doi:10.1016/j.ypmed.2011.04.014. [DOI] [PubMed] [Google Scholar]
- 5. Harrison CL, Brown WJ, Hayman M, Moran LJ, Redman LM. The role of physical activity in preconception, pregnancy and postpartum health. Semin Reprod Med. 2016;34(2):e28–e37. doi:10.1055/s-0036-1583530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Harrison AL, Taylor NF, Shields N, Frawley HC. Attitudes, barriers and enablers to physical activity in pregnant women: a systematic review. J Physiother. 2018;64(1):24–32. doi:10.1016/j.jphys.2017.11.012. [DOI] [PubMed] [Google Scholar]
- 7. Coll CVN, Domingues MR, Goncalves H, Bertoldi AD. Perceived barriers to leisure-time physical activity during pregnancy: a literature review of quantitative and qualitative evidence. J Sci Med Sport. 2017;20(1):17–25. doi:10.1016/j.jsams.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 8. Whaley DE. Seeing isn’t always believing: self-perceptions and physical activity behaviors in adults In: Weiss MR, ed. Developmental Sport and Exercise Psychology: A Lifespan Perspective. Morgantown, WV: Fitness Information Technology; 2004: 289–311. [Google Scholar]
- 9. Field T, Diego M, Delgado J, Medina L. Yoga and social support reduce prenatal depression, anxiety and cortisol. J Bodyw Mov Ther. 2013;17(4):397–403. doi:10.1016/j.jbmt.2013.03.010 [doi]. [DOI] [PubMed] [Google Scholar]
- 10. Reis PJ, Alligood MR. Prenatal yoga in late pregnancy and optimism, power, and well-being. Nurs Sci Q. 2014;27(1):30–36. doi:10.1177/0894318413509706 [doi]. [DOI] [PubMed] [Google Scholar]
- 11. Babbar S, Porter BW, Williams KB. The impact of prenatal yoga on exercise attitudes and behavior: teachable moments from a randomized controlled trial. Int J Yoga Therap. 2017;27(1):37–48. [DOI] [PubMed] [Google Scholar]
- 12. Kinser P, Masho S. “Yoga was my saving grace”: the experience of women who practice prenatal yoga. J Am Psychiatr Nurses Assoc. 2015;21(5). doi:10.1177/1078390315610554. [DOI] [PubMed] [Google Scholar]
- 13. Goodrich K, Cregger M, Wilcox S, Liu J. A qualitative study of factors affecting pregnancy weight gain in African American women. Matern Child Health J. 2013;17(3):432–440. doi:10.1007/s10995-012-1011-1 [doi]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kinser P, Masho S. “Yoga Was My Saving Grace”: the experience of women who practice prenatal yoga. J Am Psychiatr Nurses Assoc. 2015;21(5):319–326. doi:10.1177/1078390315610554. [DOI] [PubMed] [Google Scholar]
- 15. Kinser P, Williams C. Prenatal yoga. Guidance for providers and patients. Adv Nurse Pract. 2008;16(5):59. [PubMed] [Google Scholar]
- 16. Wilcox S, Liu J, Addy CL, et al. A randomized controlled trial to prevent excessive gestational weight gain and promote postpartum weight loss in overweight and obese women: Health In Pregnancy and Postpartum (HIPP). Contemp Clin Trials. 2018;66:51–63. doi:10.1016/j.cct.2018.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Garnaes KK, Morkved S, Salvesen O, Moholdt T. Exercise training and weight gain in obese pregnant women: a randomized controlled trial (ETIP Trial). PLoS Med. 2016;13(7):e1002079 doi:10.1371/journal.pmed.1002079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Cohen M, Kahn D, Steeves R. Hermeneutic Phenomenological Research: A Practical Guide for Nurse Researchers. Thousand Oaks, CA: Sage; 2000. [Google Scholar]
- 19. Giorgi A. The phenomenological movement and research in the human sciences. Nurs Sci Q. 2005;18(1):75–82. [DOI] [PubMed] [Google Scholar]
- 20. Thomas S, Pollio H. Listening to Patients: A Phenomenological Approach to Nursing Research and Practice. New York, NY: Springer; 2002. [Google Scholar]
- 21. Dishman RK, Hales DP, Sallis JF, et al. Validity of social-cognitive measures for physical activity in middle-school girls. J Pediatr Psychol. 2010;35(1):72–88. doi:10.1093/jpepsy/jsp031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Motl RW, Dishman RK, Trost SG, et al. Factorial validity and invariance of questionnaires measuring social-cognitive determinants of physical activity among adolescent girls. Prev Med (Baltim). 2000;31(5):584–594. doi:10.1006/pmed.2000.0735. [DOI] [PubMed] [Google Scholar]
- 23. Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a Pregnancy Physical Activity Questionnaire. Med Sci Sports Exerc. 2004;36(10):1750–1760. [DOI] [PubMed] [Google Scholar]
- 24. Perales M, Artal R, Lucia A. Exercise during pregnancy. JAMA. 2017;317(11):1113–1114. doi:10.1001/jama.2017.0593. [DOI] [PubMed] [Google Scholar]
- 25. Rasmussen K, Yaktine A, Institute of Medicine and National Research Council Committee to Reexamine IOM Pregnancy Weight Guidelines, eds. Weight Gain during Pregnancy: Reexamining the Guidelines. Washington, DC: National Academy of Sciences; 2009. doi:NBK32813. [Google Scholar]
- 26. Filhol G, Bernard P, Quantin X, Espian-Marcais C, Ninot G. International recommandations on physical exercise for pregnant women. Gynecol Obstet Fertil. 2014;42(12):856–860. doi:S1297-9589(14)00282-3. [DOI] [PubMed] [Google Scholar]
- 27. Chang MW, Nitzke S, Buist D, Cain D, Horning S, Eghtedary K. I am pregnant and want to do better but I can’t: focus groups with low-income overweight and obese pregnant women. Matern Child Health J. 2015;19(5):1060–1070. doi:10.1007/s10995-014-1605-x. [DOI] [PubMed] [Google Scholar]