Abstract
Objective
Far out syndrome is compression and entrapment of the L5 nerve root in the extraforaminal area between the hypertrophied L5 transverse process and the sacral ala. The purpose of this study was to describe the technique of unilateral biportal endoscopic decompression for far out syndrome and to analyze early clinical results after endoscopic decompression.
Methods
The authors consecutively performed operative treatments for 16 patients with unilateral extraforaminal entrapment of the L5 nerve root (far out syndrome) using percutaneous biportal endoscopies. We included only patients who were followed more than six months after surgery. Demographic characteristics, operative time, concomitant herniated disc, and surgical complications were investigated. Clinical outcomes were evaluated using modified MacNab criteria, the visual analogue scale (VAS) for legs, and the Oswestry Disability Index (ODI).
Results
Among 16 patients, a total of 14 cases with 4 males and 10 females were included in the study. The mean leg VAS and the ODI were significantly improved after unilateral biportal endoscopic surgery. Concomitant extraforaminal disc herniation was associated with a favorable outcome (p<0.05). Abdominal pain in the immediate postoperative period occurred in 2 patients. Abdominal pain was completely resolved with conservative management in both patients.
Conclusion
We were able to achieve successful decompression of unilateral extraforaminal entrapment of the L5 nerve root using unilateral biportal endoscopic surgery. A unilateral biportal endoscopic approach may be considered as an alternative surgical treatment for far out syndrome.
Keywords: Bertolotti syndrome, Lumbosacral transitional vertebra, Laminectomy, Endoscopy, Lumbar
INTRODUCTION
Far out syndrome is the compression and entrapment of the L5 nerve root in the extraforaminal area between the hypertrophied L5 transverse process and the sacral ala [1-4]. The condition was first described by Wiltse et al. [4] in 1984. The syndrome is one of the manifestations of lumbosacral transitional vertebrae which is seen in 4% to 30% of the adult population [3,5]. The lumbosacral transitional vertebrae was classified into four types. Type I is associated with hypertrophied L5 transverse process, and types II and IV are associated with a pseudo-articulation between the L5 transverse process and the sacral ala, which makes them prone to degenerative changes leading to facet arthrosis and extraforaminal compression of the L5 nerve root [3,5].
The initial treatment for far out syndrome is conservative management, including analgesics, rest, and pain block procedures [2,6]. The lack of symptom improvement after conservative management is an indication for surgery [7]. Minimally-invasive decompressive surgery, instead of lumbar fusion surgery, has been performed for the treatment of far out syndrome [8-10]. Microscopic decompression has been performed to treat far out syndrome or Bertolotti syndrome [2,7]. Recently, as techniques and endoscopic surgical instruments have progressed, a full endoscopic approach has been attempted for lumbar foraminal and extraforaminal lesions, instead of microscopic surgery [10-13]. We attempted to perform endoscopically assisted decompression for the unilateral extraforaminal entrapment of L5, also called far out syndrome, using a unilateral biportal endoscopic approach (Fig. 1) [13]. The purpose of this study was to describe the technique for unilateral biportal endoscopic decompression of far out syndrome and to analyze early clinical results after biportal endoscopic decompression.
Fig. 1.

Intraoperative overview of unilateral biportal endoscopic surgery.
MATERIALS AND METHODS
From March 2016 to November 2018, the authors consecutively performed operative treatments for 16 patients with unilateral extraforaminal entrapment of the L5 nerve root using unilateral biportal endoscopic surgery (Fig. 1). We included only patients who were followed more than 6 months after surgery.
Far out syndrome was diagnosed using magnetic resonance imaging (MRI), including foraminal T2 weighted images (Fig. 2). We surgically treated only patients who presented with refractory unilateral leg pain in spite of conservative management.
Fig. 2.
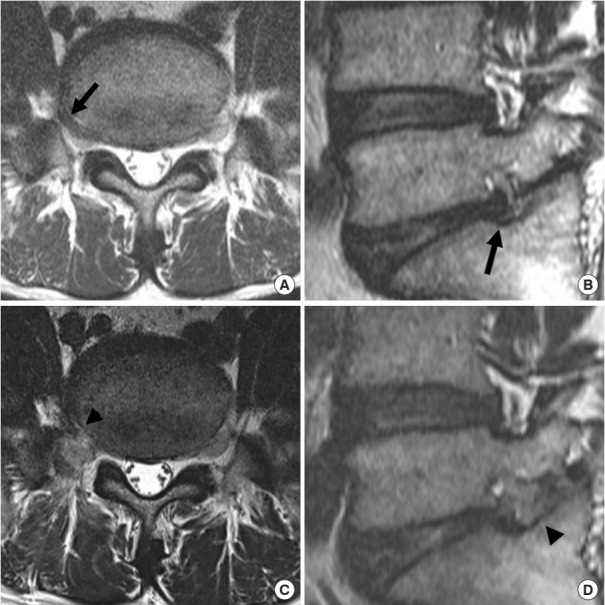
A 53-year-old male patient presented with right-sided leg pain. (A, B) The axial and oblique T2-weighted magnetic resonance (MR) images show extraforaminal entrapment of the L5 nerve root with disc protrusion (black arrows). This patient was treated by a unilateral biportal endoscopic approach. (C, D) The postoperative MR images reveal complete decompression of the L5 nerve root after unilateral biportal endoscopic surgery (black arrowheads).
Demographic characteristics, operative time, follow-up period, amount of estimated blood loss, concomitant herniated disc, and surgical complications were investigated. Clinical outcomes were evaluated using modified MacNab criteria, a visual analogue scale (VAS) for legs, and the Oswestry Disability Index (ODI). We classified excellent and good grades on the modified MacNab criteria as favorable outcomes. Postoperative MRI with foraminal views was evaluated on postoperative day 1 for optimal neural decompression of the L5 root (Figs. 2, 3).
Fig. 3.
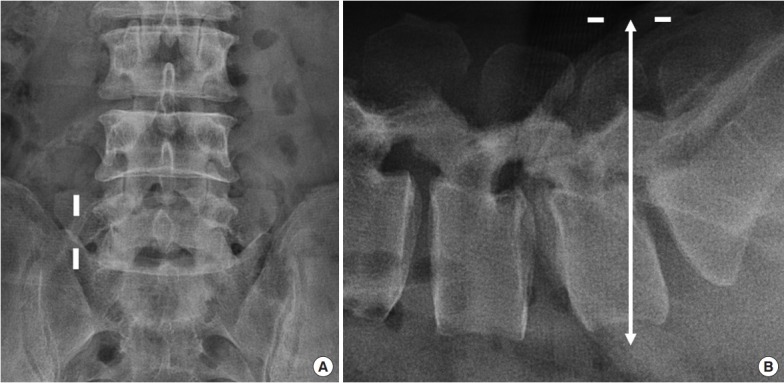
Skin incision points for the 2 portals. (A) Two channels were made at 1 cm lateral to the lateral border of the pedicle of L5–S1 in the anterior-posterior view. (B) Portals were made 1 cm below and 1 cm above the midpoint of the foramen (white arrow) in the lateral view. Generally, the upper portal was made around the pedicle of L5 and the lower portal was made around the upper endplate of S1 in the lateral C-arm view.
This study was approved by the Institutional Review Board (IRB) of Wiltse Memorial Hospital (2019-05). Written informed consent was waived by the IRB.
1. Indications
The following are indications for surgery: (1) Unilateral radiating leg pain in the L5 dermatome refractory to conservative management; (2) Temporary improvement of unilateral radicular pain after a selective L5 root blocking procedure; (3) MRI evidence of the extraforaminal compression of L5 with the presence of lumbosacral transitional vertebrae, without another identifiable pain source; (4) No segmental instability, spondylolysis, or spondylolisthesis of L5–S1.
2. Surgical Procedures
1) General concept
The technique of unilateral biportal endoscopic surgery utilized 2 portals; one portal was for an endoscope channel for visualization and the second portal was a working channel only for the use of surgical instruments (Fig. 1). Both endoscopic specialized instruments and the standard instruments for spine surgery were used in this procedure, unlike one portal endoscopy which requires specialized instruments. The irrigation fluid was drained from the endoscopic portal to the working portal. The continuous irrigation of fluid maintained clear endoscopic visualization and prevented bleeding.
2) Patient position and anesthesia
This approach was performed under general anesthesia or epidural anesthesia. We preferred a prone position using a frame to reduce abdominal pressure.
3) Skin incisions
Two skin incisions were made under C-arm fluoroscopic guidance. First, we marked the pedicle of L5 and S1, the disc space, and the transverse process of L5 under C-arm guidance. The skin incisions were made at 1 cm lateral to the lateral border of the pedicle of L5–S1 in the anteriorposterior view (Fig. 3A). And, we made 2 portals, 1 cm above and 1 cm below the midpoint of the foramen in the lateral C-arm fluoroscopic view (Fig. 3B). Generally, the upper portal was made around the pedicle of L5 and the lower portal was made around the upper endplate of S1 in the lateral C-arm view. Our recommendation was to use the dominant hand for the working portal and the nondominant hand for the endoscopic portal. In the case of a leftside approach by a right-handed surgeon, the cranial left portal was usually the endoscopic portal and the caudal right portal was a working portal. And, the case of a right-side approach, the cranial right portal was usually the working portal and the caudal left portal was the endoscopic portal. After making the working portal, we usually inserted a sheath for the working portal (Fig. 1). If a working sheath was inserted, the outflow from the saline irrigation was well maintained and the surgical instruments were smoothly inserted into the working portal. The point of landing and joining of the 2 portals was over the ipsilateral transverse process of L5.
4) Endoscopic decompressive procedures
A dissection was performed to expose the transverse process, mamillary process, isthmus, lateral border of superior articular process, and ala using radiofrequency (RF) probes. The caudal portion of the L5 transverse process, the lateral portion of the facet, and the sacral ala were clearly exposed and identified. Drilling began at the L5 transverse process. The lower portion of the transverse process and the lateral portion of the isthmus and the facet wall were partially removed with a diamond burr. Bone bleeding was controlled with RF or bone wax. Then, using a combination of angled curette and Kerrison punches, the foraminal ligament was removed to expose the underlying L5 exiting nerve root. The foraminal part of the exiting L5 root was clearly exposed. The superior portion of the ala was removed from medial to lateral along the course of the nerve. Lastly, pseudo-arthrosis between the transverse process and the sacral ala were drilled out and removed for decompression of the extraforaminal part of the L5 nerve root. In cases with an associated disc herniation, disc particles were removed using pituitary forceps. The L5 exiting root was checked from the foraminal to the extraforaminal area with various sizes of nerve hooks to test for any residual compression. Finally, a drainage catheter was inserted through the working portal (Supplementary video clip 1).
5) Wound closure
After the subcutaneous layer was approximated with absorbable suture materials, skin glue materials were applied to the skin.
3. Statistical Analyses
Statistical analyses were performed using a Fisher exact test and Wilcoxon signed rank test. A p<0.05 was considered to be statistically significant. R 3.1.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analyses.
RESULTS
Among 16 patients, a total of 14 cases with 4 males and 10 females were included in the study with an average age of 59.5±7.2 years. The mean follow-up period was 11.0±5.0 months (Table 1).
Table 1.
Clinical parameters of patients
| Characteristic | Value |
|---|---|
| Sex, male:female | 4:10 |
| Age (yr) | 59.5±7.2 |
| Follow-up period (mo) | 11.0±5.0 |
| Estimated blood loss (mL) | 85.0±29.5 |
| Operation time (min) | 72.8±15.5 |
| VAS of leg | |
| Preoperative | 8.4±1.1 |
| Postoperative | 2.8±1.4 |
| ODI | |
| Preoperative | 60.2±5.5 |
| Postoperative | 22.1±3.4 |
| MacNab criteria | |
| Excellent | 3 |
| Good | 7 |
| Fair | 3 |
| Poor | 1 |
| Complication | |
| Abdominal pain (perirenal fluid collection) | 2 (1) |
Values are presented as number or mean standard deviation.
VAS, visual analogue scale; ODI, Oswestry Disability Index.
Postoperative MR images revealed optimal neural decompression of the L5 nerve root in all patients (Figs. 2, 4). The mean operative time was 72.8±15.5 minutes and the mean estimated blood loss was 85.0±29.5 mL (Table 1). VAS of the legs improved from 8.4±1.1 to 2.8±1.4 and the ODI improved from 60.2±5.5 to 22.1±3.4 at the final follow-up. The modified MacNab criteria were excellent in 3 (21.4%), good in 7 (50%), fair in 3 (21.4%), and poor in 1 (7%) (Table 1). One case with a poor outcome showed improvement of radicular pain in the immediate postoperative period. However, this patient’s radicular pain and claudication were reaggravated 2 months postoperatively. Of the 14 cases, 7 patients had an associated extraforaminal disc herniation of the L5–S1 around the alar area. All 7 patients with extraforaminal disc herniation had favorable outcomes (excellent or good) after surgery. Concomitant extraforaminal disc herniation was associated with a favorable outcome (p<0.05).
Fig. 4.
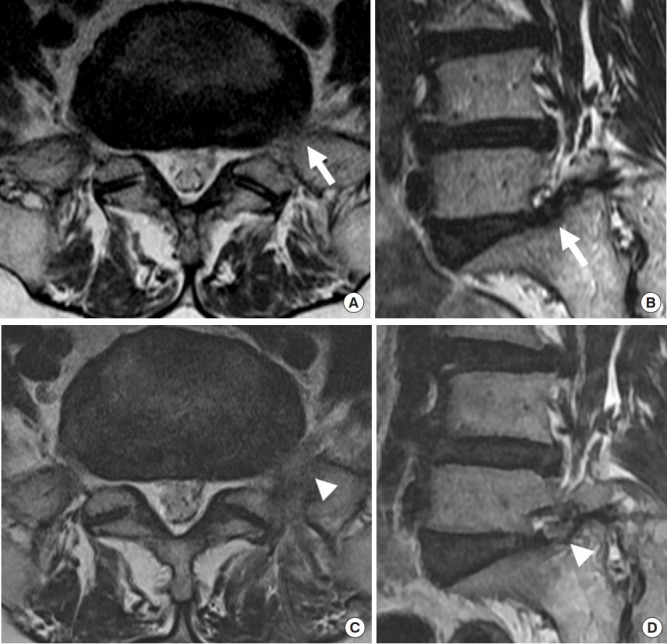
A 62-year-old female patient complained of left radicular leg pain. (A, B) The axial and oblique T2-weighted magnetic resonance images depict the extraforaminal entrapment of the L5 nerve root by disc protrusion and pseudo-arthrosis (white arrows). (C, D) After endoscopic surgery, the L5 nerve root was completely decompressed (white arrowheads) (Supplementary video clip 1).
Abdominal pain was experienced by some patients in the immediate postoperative period. Two patients complained of abdominal pain immediately after surgery. A postoperative computed tomography (CT) scan of the abdomen revealed perirenal fluid collection in 1 patient (Fig. 5). Abdominal pain was completely resolved with conservative management within 3 hours in both patients.
Fig. 5.
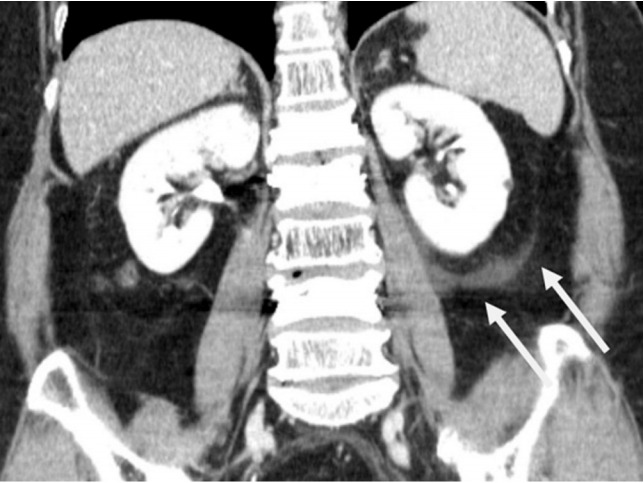
A 62-year-old female patient presented with abdominal pain immediately after surgery. Abdominal coronal computed tomography scan image shows left retroperitoneal fluid collection (arrows; perirenal area). Abdominal pain was completely resolved after conservative management. This patient was discharged without any problems.
DISCUSSION
Pseudo-articulation or fusion between the transverse process of L5 and sacral ala causes extraforaminal entrapment of the L5 nerve root. Extraforaminal entrapment of the L5 nerve root produces radicular pain of the buttock and leg [2,3]. Radiologic diagnosis of symptomatic extraforaminal entrapment of the L5 nerve root is difficult [14]. Conventional axial and sagittal MR images may not provide adequate information for symptomatic far out syndrome [1,15,16]. Diffuse tensor images and oblique coronal images have been used for the radiological diagnosis of extraforaminal entrapment of the L5 nerve root [1,15]. In our study, we used oblique foraminal MRI to diagnose far out syndrome. Oblique foraminal MRIs were modified to include oblique coronal T2-weighted images. The oblique foraminal images were taken perpendicular to the intervertebral foramen and demonstrated an L5 nerve root exiting from the foraminal to the extraforaminal area of L5–S1. We suggest that an oblique foraminal MRI view might provide additional diagnostic information for extraforaminal lesions. CT, simple X-rays, and bone scintigraphy are also important for the diagnosis of far out syndrome [2,3,5]. Transient relief of radicular pain after a selective L5 root block may be an important finding in the diagnosis of far out syndrome [5,7].
Wiltse et al. [4] first described far out syndrome and its surgical treatment. Since then, nonfusion decompressive surgeries have been performed for the treatment of far out syndrome. Minimally invasive decompressive surgeries have been attempted in patients with far out syndrome and Bertolotti syndrome. Previously published articles have described favorable clinical outcomes after microscopic decompressive surgeries. Recently, fully endoscopic approaches have been used for the surgical treatment of foraminal lesions [10]. We tried decompressive surgery for far out syndrome using a unilateral biportal endoscopic approach. The unilateral biportal endoscopic approach used 2 channels. The working portal was only used as a channel for surgical instruments, including general spinal instruments, as well as specialized endoscopy instruments. Moreover, the handling of spinal operative instruments was easier than the uniportal endoscopic surgeries [13]. Therefore, we suggested that the surgical achievement of unilateral biportal endoscopic surgery may be the same as for microscopic surgery [13]. Basically, the operative principle of biportal endoscopic decompressive surgery is the same as that of minimally-invasive microscopic decompression of the L5 nerve root. We achieved full decompression of the extraforaminal area around the lumbosacral transitional area between the ala and the transverse process.
The basic structural alteration in this condition is an enlarged L5 transverse process which forms a false joint with the ala of the sacrum lateral to the foramen. The L5 nerve root is compressed between these 2 structures. Moreover, there may be an associated disc herniation which may cause the sudden aggravation of pain. The lower portion of the transverse process, sacral ala, and the pseudo-articulation between the ala and the transverse process should be partially removed for complete decompression of L5 entrapment from the foramen to the extraforaminal area. After decompression around the pseudo-articulation, concomitant extraforaminal disc herniation should be explored and removed for optimal decompression of the L5 nerve root. Extraforaminal disc herniation may newly induce or aggravate radicular leg pain in patients with lumbosacral transitional vertebrae [16]. Concomitant ruptured disc herniation was a predisposing factor for postoperative clinical outcomes in this study.
The percutaneous uniportal or biportal endoscopic approaches used continuous saline irrigation to maintain clear operative views and prevent bleeding. However, there is the possibility of retroperitoneal fluid collection by continuous saline irrigation in the paraspinal Wiltse approach. Retroperitoneal fluid collection can cause abdominal pain and discomfort. The barrier between the paraspinal and retroperitoneal area may be damaged when the pseudo-arthrosis around the ala is removed, which may result in retroperitoneal fluid collection. Two patients complained of abdominal pain immediately after surgery and in one of them, retroperitoneal fluid collection was identified on an abdominal CT scan (Fig. 5). Fortunately, the abdominal pain spontaneously resolved after conservative management, including bed rest and analgesics. Hence, it is our recommendation that decompression around pseudo-arthrosis between the transverse process and the sacral ala should be performed swiftly and completed within 30 minutes. Another precaution during the surgery is during discectomy in the L5–S1 area. The common iliac vasculature is in close proximity to the anterior surface of the disc. Hence, the careful use of pituitary forceps is warranted in this area to avoid vascular injury. We have not experienced dural tears, nerve root injuries, or infection after endoscopic decompression.
Unilateral biportal endoscopic approaches have the benefits of minimally-invasive surgery, including the minimization of trauma to the posterior muscle and ligamentous structures, reduction of postoperative pain, and acceleration of postoperative recovery. However, the steep learning curve of endoscopic surgery, the technical difficulty, and the possibility of incomplete decompression are disadvantages of endoscopic approaches compared to microsurgery. Therefore, we suggest that it is necessary to acquire sufficient microscopic surgical experience before initiating the use of endoscopic decompression for far out syndrome. Although endoscopic approaches have better clinical aspects than open surgery, patients with instability or bilateral radicular leg pain should be considered for treatment with fusion surgery.
The limitations of the study were small sample size, a relatively short follow-up duration, and the retrospective nature of the study. However, our results showed that unilateral biportal endoscopic surgery may be considered as a feasible option for surgical treatment of far out syndrome in select cases.
CONCLUSION
Unilateral extraforaminal entrapment of the L5 nerve root may be successfully decompressed by unilateral biportal endoscopic surgery. A unilateral biportal endoscopic approach may be considered as an alternative for endoscopic decompression of far out syndrome. Minimal soft tissue dissection, minimal blood loss, excellent magnification, and visualization of the pathology are advantages of the procedure.
Acknowledgments
The views expressed in this article represent those of the authors and no other entity or organization.
Footnotes
The authors have nothing to disclose.
SUPPLEMENTARY MATERIAL
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.1938026.013.v1.
Supplementary video clip 1: Intraoperative video of unilateral biportal endoscopic decompression for left sided far out syndrome. Left L5 exiting nerve root was completely decompressed from foraminal to extraforaminal area after endoscopic decompressive surgery.
REFERENCES
- 1.Takeuchi M, Wakao N, Kamiya M, et al. Lumbar extraforaminal entrapment: performance characteristics of detecting the foraminal spinal angle using oblique coronal MRI. A multicenter study. Spine J. 2015;15:895–900. doi: 10.1016/j.spinee.2015.02.011. [DOI] [PubMed] [Google Scholar]
- 2.Holm EK, Bünger C, Foldager CB. Symptomatic lumbosacral transitional vertebra: a review of the current literature and clinical outcomes following steroid injection or surgical intervention. SICOT J. 2017;3:71. doi: 10.1051/sicotj/2017055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nardo L, Alizai H, Virayavanich W, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology. 2012;265:497–503. doi: 10.1148/radiol.12112747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiltse LL, Guyer RD, Spencer CW, et al. Alar transverse process impingement of the L5 spinal nerve: the far-out syndrome. Spine (Phila Pa 1976) 1984;9:31–41. doi: 10.1097/00007632-198401000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Jancuska JM, Spivak JM, Bendo JA. A review of symptomatic lumbosacral transitional vertebrae: Bertolotti’s syndrome. Int J Spine Surg. 2015;9:42. doi: 10.14444/2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Glémarec J, Varin S, Cozic C, et al. Efficacy of local glucocorticoid after local anesthetic in low back pain with lumbosacral transitional vertebra: a randomized placebo-controlled double-blind trial. Joint Bone Spine. 2018;85:359–63. doi: 10.1016/j.jbspin.2017.05.003. [DOI] [PubMed] [Google Scholar]
- 7.Li Y, Lubelski D, Abdullah KG, et al. Minimally invasive tubular resection of the anomalous transverse process in patients with Bertolotti’s syndrome: presented at the 2013 Joint Spine Section Meeting: clinical article. J Neurosurg Spine. 2014;20:283–90. doi: 10.3171/2013.11.SPINE13132. [DOI] [PubMed] [Google Scholar]
- 8.Sasaki M, Aoki M, Matsumoto K, et al. Middle-term surgical outcomes of microscopic posterior decompression for far-out syndrome. J Neurol Surg A Cent Eur Neurosurg. 2014;75:79–83. doi: 10.1055/s-0032-1327443. [DOI] [PubMed] [Google Scholar]
- 9.Tschugg A, Tschugg S, Hartmann S, et al. Far caudally migrated extraforaminal lumbosacral disc herniation treated by a microsurgical lateral extraforaminal transmuscular approach: case report. J Neurosurg Spine. 2016;24:385–8. doi: 10.3171/2015.7.SPINE15342. [DOI] [PubMed] [Google Scholar]
- 10.Paudel B, Kim HS, Jang JS, et al. Percutaneous full endoscopic treatment of Bertolotti syndrome: a report of three cases with technical note. J Neurol Surg A Cent Eur Neurosurg. 2017;78:566–71. doi: 10.1055/s-0037-1598173. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Kim HS, Kapoor A, et al. Feasibility of full endoscopic spine surgery in patients over the age of 70 years with degenerative lumbar spine disease. Neurospine. 2018;15:131–7. doi: 10.14245/ns.1836046.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Heo DH, Kim JS, Park CW, et al. Contralateral sublaminar endoscopic approach for removal of lumbar juxtafacet cysts using percutaneous biportal endoscopic surgery: technical report and preliminary results. World Neurosurg. 2019;122:474–9. doi: 10.1016/j.wneu.2018.11.072. [DOI] [PubMed] [Google Scholar]
- 13.Heo DH, Quillo-Olvera J, Park CK. Can percutaneous biportal endoscopic surgery achieve enough canal decompression for degenerative lumbar stenosis? Prospective case-control study. World Neurosurg. 2018;120:e684–9. doi: 10.1016/j.wneu.2018.08.144. [DOI] [PubMed] [Google Scholar]
- 14.Heo DH, Kim SW, Chang HH, et al. Usefulness of oblique lumbar magnetic resonance imaging for nerve root anomalies and extraforaminal entrapment lesions. Asian Spine J. 2018;12:423–7. doi: 10.4184/asj.2018.12.3.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kitamura M, Eguchi Y, Inoue G, et al. A case of symptomatic extra-foraminal lumbosacral stenosis (“far-out syndrome”) diagnosed by diffusion tensor imaging. Spine (Phila Pa 1976) 2012;37:E854–7. doi: 10.1097/BRS.0b013e318249537f. [DOI] [PubMed] [Google Scholar]
- 16.Tschugg A, Tschugg S, Hartmann S, et al. Far caudally migrated extraforaminal lumbosacral disc herniation treated by a microsurgical lateral extraforaminal transmuscular approach: case report. J Neurosurg Spine. 2016;24:385–8. doi: 10.3171/2015.7.SPINE15342. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary video clip 1 can be found via https://doi.org/10.14245/ns.1938026.013.v1.
Supplementary video clip 1: Intraoperative video of unilateral biportal endoscopic decompression for left sided far out syndrome. Left L5 exiting nerve root was completely decompressed from foraminal to extraforaminal area after endoscopic decompressive surgery.


