Abstract
Background:
Sexual minority (gay, lesbian, and bisexual) individuals experience elevated mood disorders and suicidality compared to their heterosexual counterparts. However, to date, these sexual orientation disparities have yet to be examined among middle childhood-aged participants.
Methods:
Data were employed from the baseline wave of the Adolescent Brain Cognitive Development (ABCD) study, a U.S. representative sample. Population-level weighting was utilized, resulting in an analytic sample of N = 8,204,013 (nunweighted = 4,519) children between the ages of 9 and 10 years: with 70,952 (nunweighted = 43) identifying as sexual minories (0.9% of the population). Structured clinical interviews were used to assess mood disorders (i.e., depressive and bipolar disorders) and suicidality. Sexual orientation (sexual minority vs. heterosexual) was examined as the focal independent variable.
Results:
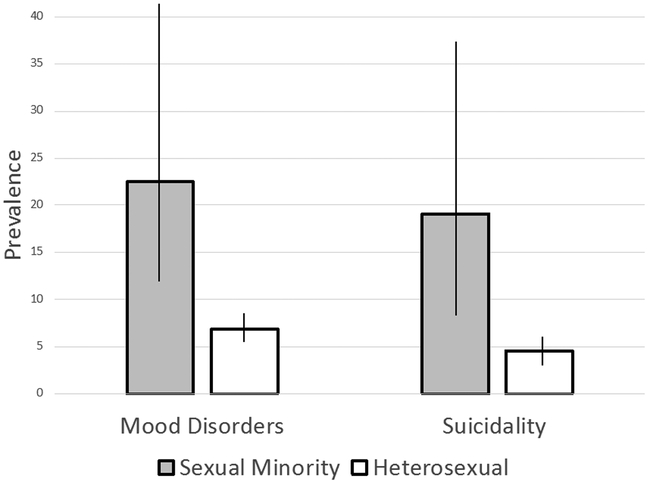
The overall prevalence of mood disorders was 7.1%. Sexual minority children (22.5%) possessed a higher rate than heterosexual children (6.9%). The overall prevalence of suicidality was 4.8%; sexual minority children (19.1%) possessed a higher rate than heterosexual children (4.6%).
Limitations:
Sexual orientation assessment did not include attraction, and thus, results may represent a lower bound estimate of sexual minorities.
Conclusions:
Sexual orientation disparities in mood disorders and suicidality appear to develop as early as middle childhood. Clinicians are encouraged to assess sexual orientation among children as young as 9-10 years old, and provide appropriate normalization of sexual orientation, and referrals for mental health treatment, as indicated.
Keywords: sexual orientation, children, mood disorders, suicide, sexual minority
Introduction
Sexual minorities (e.g., gay, lesbian, bisexual individuals) experience significantly elevated psychiatric morbidity compared to heterosexuals (e.g., Herek & Garnets, 2007; Stone et al., 2014). These psychiatric disparities have been noted among adolescents (Stone et al., 2014) and adults (Herek & Garnets, 2007). Specifically, nationally-representative and meta-analytic studies have demonstrated that sexual minorities experience elevated rates of mood disorders (e.g., depressive and bipolar disorders; Kerridge et al., 2017), and suicidality (Miranda-Mendizábal et al., 2017). However, less is known about whether these mental health disparities exist in middle childhood. Examining health disparities in middle childhood is important, as there is emerging work suggesting that minority sexual orientation may be identified at younger ages. Therefore, identifying if mental health disparities are evident at younger ages is crucial for determining the optimal developmental point for intervention. Thus, the aim of the current study is to examine the prevalence of mood disorders and suicidality as a function of sexual orientation among a U.S.-representative sample of 9 to 10-year-old children. Consistent with extant literature on sexual orientation health disparities, it is hypothesized that sexual minority children will experience significantly elevated rates of mood disorders and suicidality compared to heterosexual children.
Methods
Data were collected in 2016-2017 from the Adolescent Brain Cognitive Development (ABCD) study (Volkow et al., 2018), a U.S. representative sample of 9 to 10-year-old children. The broad aims of the ABCD study are to explore the development and health among children from age 9 through early adulthood, by assessing environmental, genetic, neurological, biological, psychiatric, and behavioral variables. Sexual orientation was defined from child responses to a computer-based question (with research assistant guidance): “Are you gay or bisexual?” Possible response options were “Yes,” “Maybe,” “No,” and “I do not understand this question.” Consistent with previous operational definitions of sexual minority status (Mustanski et al., 2014; Ott et al., 2011), responses of “Yes” and “Maybe” were coded as probable sexual minority; all other responses were coded as heterosexual. Mood disorders and suicidality were assessed via the youth version of the computerized Kiddie Schedule for Affective Disorders and Schizophrenia (KSADS; Kaufman et al., 1997; Kobak & Kaufman, 2015), a structured diagnostic interview based on the Diagnostic and Statistical Manual of Mental Disorders—5th Edition (DSM-5). Given their developmental stage, trained research assistants supported participants in completing the interview (Barch et al., 2018). Current mood disorders (i.e., depressive and bipolar disorders) and suicidality (i.e., self-injurious behaviors, desire to be dead, suicidal thoughts, and suicide attempts) were assessed and binary variables were created denoting presence vs. absence of a given construct. Post-stratification weights for demographics, socioeconomic measures, and family relationships were employed to match the 2010 U.S. Census; thus, results are presented based upon population-level estimates. The total population was N = 8,204,013 (nunweighted = 4,519), with 70,952 (nunweighted = 43) sexual minorities (0.9% of the population; 1.2% among girls; 0.6% among boys).
Results
Regarding children’s sexual minority status, 0.24% (nunweighted = 11; Npopulation = 19,553) reported “Yes;” 0.63% (nunweighted = 32; Npopulation = 51,398) reported “Maybe;” 75.43% (nunweighted = 3,402; Npopulation = 6,188,308) reported “No;” and 23.70% (nunweighted = 1,074; Npopulation = 1,944,753) reported “I do not understand the question.” The overall prevalence of mood disorders was 7.1% (95% CI: 6.3%, 8.0%), with sexual minority children (22.5%; 95% CI: 10.4%, 42.1%) possessing a higher rate than heterosexual children (6.9%; 95% CI: 6.1%, 7.8%), adjusted F = 6.4, p = .01; OR = 3.9 (95% CI: 1.5, 9.8). The overall prevalence of suicidality was 4.8% (95% CI: 4.1%, 5.5%), with sexual minority children (19.1%; 95% CI: 8.7%, 36.9%) possessing a higher rate than heterosexual children (4.6%; 95% CI: 4.0%, 5.4%), adjusted F = 8.2, p = .004; OR = 4.8 (95% CI: 1.9, 12.1). See Figure 1.
Figure 1.
Prevalence of mood disorders and suicidality by sexual orientation
Discussion
The current study is the first known attempt to assess sexual orientation health disparities among middle childhood-aged participants. Data were gathered from a recently-released, U.S. representative sample of 9-10-year-old children. Consistent with data on adolescent (Miranda-Mendizábal et al., 2017; Stone et al., 2014) and adult sexual minorities (Herek & Garnets, 2007; Kerridge et al., 2017) results highlight substantial psychiatric health disparities among sexual minority children. Specifically, sexual minority children are at elevated odds of experiencing mood disorders and suicidality compared to their heterosexual counterparts, with large effect size estimates revealed. Indeed, the magnitude of disparities revealed is similar, if not larger, than previously reported findings among sexual minority adolescents (Zaza et al., 2016) and adults (Kerridge et al., 2017). Taken together with existing studies on sexual minority adolescents and adults, the results of the current study suggest that sexual orientation-related mental health disparities are evident in childhood and potentially persist through adolescence and adulthood.
Although the mechanisms of this association were not tested in the current study, sexual minority stress theory (Meyer, 2003) may offer a useful framework. This theory underscores both distal-level (e.g., victimization, prejudice, and discrimination) and proximal-level (e.g., internalized homonegativity, sexual orientation concealment, and expectations of rejection) factors in development of mental health disparities among sexual minorities. That is, the model argues that elevated rates of psychiatric disorders are not the result of inherent psychopathology amongst sexual minorities, but rather, a result of anti-gay rhetoric and institutional policies which can subsequently lead to maladaptive internal processes (e.g., social avoidance, rumination, fear of negative evaluation, negative cognitive schemas about the self, hopelessness; Hatzenbuehler, 2009). Although the sexual minority stress model offers one theoretical perspective to view the results of the current study, to date, we are unaware of published studies which have tested this model in middle childhood.
The current study is not without limitations. Although the ABCD cohort is novel in assessing sexual orientation at an early age, currently there are no data on the reliability of this sexual orientation assessment. However, this item is face valid, and by including the response option of “I do not understand this question” does not force children into responding affirmatively or negatively. Future research with subsequent waves of data from the cohort will be important in exploring the developmental trajectories of sexual orientation identity. Further, the baseline wave of ABCD did not include assessment of other salient aspects of sexual orientation, such as attraction or behavior; the former may be particularly relevant for measuring sexual orientation among children this age. Additionally, while the KSADS has a long history of demonstrating strong psychometric properties (e.g., Kaufman et al., 1997), the computerized version used in the current study was created specifically for the purposes of the ABCD cohort, and psychometric evaluation of this version is ongoing (Kobak & Kaufman, 2015). Lastly, although the sampling approach allows for generalizability to all 9 to 10-year-old U.S. children, the unweighted counts of sexual minority participants were rather modest, which resulted in wide confidence intervals for the prevalence of mood disorders and suicidality in this group. Thus, some caution should be made in generalizing these findings given the potential for lack of precision in point estimates.
The results from the current study may inform clinical practice. While sensitive, results suggest that sexual orientation can be assessed among children as young as 9-10 years old. It is possible that not all children in this age range will possess the requisite cognitive skills to respond to this assessment; however, as the results from the current study underscore, children this young who respond with “yes” or “maybe” are at substantial risk for mood disorders and suicidality. Clinicians may also be in a unique position of influence, as previous studies indicate that most sexual minority youth have not disclosed their sexual orientation to their primary caregivers (Rosario et al., 2009). Thus, clinicians can serve as a crucial figure, normalizing children’s sexual orientation, assessing mood and suicidality, and providing appropriate referrals for mental health treatment, as indicated (Committee on Adolescence, 2013; Frankowski, 2004; Hadland et al., 2016).
Data from the baseline wave of the ABCD cohort indicate that sexual orientation can be assessed among children as young as 9-10 years old. Moreover, children who identity as sexual minorities are at substantially increased odds of experiencing mood disorders and suicidality. Clinicians are encouraged to consider adopting assessment of sexual orientation as part of routine care, as sexual minority status appears to be a robust marker of risk for psychiatric health disparities among children.
Acknowledgments:
Data used in the preparation of this article were obtained from the Adolescent Brain Cognitive Development (ABCD) Study (https://abcdstudy.org), held in the NIMH Data Archive (NDA). This is a multisite, longitudinal study designed to recruit more than 10,000 children age 9-10 and follow them over 10 years into early adulthood. The ABCD Study is supported by the National Institutes of Health and additional federal partners under award numbers U01DA041022, U01DA041028, U01DA041048, U01DA041089, U01DA041106, U01DA041117, U01DA041120, U01DA041134, U01DA041148, U01DA041156, U01DA041174, U24DA041123, and U24DA041147. A full list of supporters is available at https://abcdstudy.org/federal-partners.html. A listing of participating sites and a complete listing of the study investigators can be found at https://abcdstudy.org/principal-investigators.html. ABCD consortium investigators designed and implemented the study and/or provided data but did not necessarily participate in analysis or writing of this report. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or ABCD consortium investigators. The ABCD data repository grows and changes over time. The ABCD data used in this report came from DOI:10.15154/1412097. DOIs can be found at https://ndar.nih.gov/study.html?id=500.
References
- Barch DM, Albaugh MD, Avenevoli S, Chang L, Clark DB, Glantz MD, …Sher KJ (2018). Demographic, physical and mental health assessments in the adolescent brain and cognitive development study: Rationale and description. Developmental Cognitive Neuroscience, 32, 55–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Adolescence. (2013). Office-based care for lesbian, gay, bisexual, transgender, and questioning youth. Pediatrics, 132, 297–313. [DOI] [PubMed] [Google Scholar]
- Frankowski BL, & Committee on Adolescence. (2004). Sexual orientation and adolescents. Pediatrics, 113, 1827–1832. [DOI] [PubMed] [Google Scholar]
- Hadland SE, Yehia BR, & Makadon HJ (2016). Caring for LGBTQ youth in inclusive and affirmative environments. Pediatric Clinics of North America, 63, 955–969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzenbuehler ML (2009). How does sexual minority stigma “get under the skin?” A psychological mediation framework. Psychological Bulletin, 135, 707–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herek GM, & Garnets LD (2007). Sexual orientation and mental health. Annual Review of Clinical Psychology, 3, 353–375. [DOI] [PubMed] [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, ….Ryan N (1997). Schedule for Affective Disorder and Schizophrenia for School-Age Children-Present and Lifetime version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry, 36, 980–988. [DOI] [PubMed] [Google Scholar]
- Kerridge BT, Pickering RP, Saha TD, June Ruan W, Patricia Chou S, Zhang H, …Hasin DS (2017). Prevalence, sociodemographic correlates and DSM-5 substance use disorder and other psychiatric disorders among sexual minorities in the United States. Drug & Alcohol Dependence, 170, 82–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak KA, & Kaufman J (2015). KSADS-comp Center for Telepsychology. Madison, WI. [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129, 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda-Mendizábal A, Castellvi P, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, …Alonso J (2017). Sexual orientation and suicidal behavior in adolescents and young adults: systematic review and meta-analysis. British Journal of Psychiatry, 211, 77–87. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Van Wagenen A, Birkett M, Eyster S, & Corliss HL (2014) Identifying sexual orientation health disparities in adolescents: Analysis of pooled data from the Youth Risk Behavior Survey, 2005 and 2007. American Journal of Public Health, 104, 211–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott MQ, Corliss HL, Wypij D, Rosario M, & Austin SB (2011). Stability and change in self-reported sexual orientation identity in young people: Application of mobility metrics. Archives of Sexual Behavior, 40, 519–532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosario M, Schrimshaw EW, & Hunter J (2009). Disclosure of sexual orientation and subsequent substance use and abuse among lesbian, gay, and bisexual youths: Critical role of disclosure reactions. Psychology of Addictive Behaviors, 23, 175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stone DM, Luo F, Ouyang L, Lippy C, Hertz MF, & Crosby AE (2014). Sexual orientation and suicide ideation, plans, attempts, and medically serious attempts: Evidence from local Youth Risk Behavior Surveys 2001-2009. American Journal of Public Health, 104, 262–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow ND, Koob GF, Croyle RT, Bianchi DW, Gordon JA, Koroshetz WJ, …Weiss SRB (2018). The conception of the ABCD study: From substance use to a broad NIH collaboration. Developmental Cognitive Neuroscience, 32, 4–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zaza S, Kann L, & Barrios LC (2016). Lesbian, gay, and bisexual adolescents: population estimate and prevalence of health behaviors. JAMA, 316, 2355–2356. [DOI] [PMC free article] [PubMed] [Google Scholar]