This epidemiological study evaluates the association of primary care physician supply and both all-cause and cause-specific mortality by comparing US population and insurance claims data with data on density of primary care physicians and specialist physician density.
Key Points
Question
What is the association between primary care physician density and population-level mortality?
Findings
In this epidemiological study of US population data, every 10 additional primary care physicians per 100 000 population was associated with a 51.5-day increase in life expectancy. However, from 2005 to 2015, the density of primary care physicians decreased from 46.6 to 41.4 per 100 000 population.
Meaning
Greater primary care physician supply was associated with improved mortality, but per capita primary care physician supply decreased between 2005 and 2015.
Abstract
Importance
Recent US health care reforms incentivize improved population health outcomes and primary care functions. It remains unclear how much improving primary care physician supply can improve population health, independent of other health care and socioeconomic factors.
Objectives
To identify primary care physician supply changes across US counties from 2005-2015 and associations between such changes and population mortality.
Design, Setting, and Participants
This epidemiological study evaluated US population data and individual-level claims data linked to mortality from 2005 to 2015 against changes in primary care and specialist physician supply from 2005 to 2015. Data from 3142 US counties, 7144 primary care service areas, and 306 hospital referral regions were used to investigate the association of primary care physician supply with changes in life expectancy and cause-specific mortality after adjustment for health care, demographic, socioeconomic, and behavioral covariates. Analysis was performed from March to July 2018.
Main Outcomes and Measures
Age-standardized life expectancy, cause-specific mortality, and restricted mean survival time.
Results
Primary care physician supply increased from 196 014 physicians in 2005 to 204 419 in 2015. Owing to disproportionate losses of primary care physicians in some counties and population increases, the mean (SD) density of primary care physicians relative to population size decreased from 46.6 per 100 000 population (95% CI, 0.0-114.6 per 100 000 population) to 41.4 per 100 000 population (95% CI, 0.0-108.6 per 100 000 population), with greater losses in rural areas. In adjusted mixed-effects regressions, every 10 additional primary care physicians per 100 000 population was associated with a 51.5-day increase in life expectancy (95% CI, 29.5-73.5 days; 0.2% increase), whereas an increase in 10 specialist physicians per 100 000 population corresponded to a 19.2-day increase (95% CI, 7.0-31.3 days). A total of 10 additional primary care physicians per 100 000 population was associated with reduced cardiovascular, cancer, and respiratory mortality by 0.9% to 1.4%. Analyses at different geographic levels, using instrumental variable regressions, or at the individual level found similar benefits associated with primary care supply.
Conclusions and Relevance
Greater primary care physician supply was associated with lower mortality, but per capita supply decreased between 2005 and 2015. Programs to explicitly direct more resources to primary care physician supply may be important for population health.
Introduction
Primary care physicians are typically responsible for the prevention, diagnosis, management, and treatment of a wide array of conditions. When examining area-level differences in the availability of primary care services and average large-area health statistics (at the international and state levels, in particular), higher availability of primary care services within a health system has been correlated with lower all-cause and cause-specific mortality. However, these cross-sectional correlations generally did not control extensively for other health care and socioeconomic confounders.1,2,3,4,5,6 Consequently, the association of incremental increases in primary care physician supply with population-wide health outcomes remains heavily debated,7,8,9,10 and whether to invest in policies that specifically aim to increase primary care physician supply is an important question in health care reform across many high-income countries. In the United States, in the absence of such policies, market forces have reduced primary care supply relative to higher-income specialties.11,12,13,14
How primary care physician supply has changed at the local level during the past decade in the United States and the strength of the association between changes in primary care physician supply and mortality remain unclear. Addressing these uncertainties is important to understanding whether efforts to expand primary care physician supply have the potential to produce measurable population health improvements. Herein, we sought to test associations between population-level physician supply and population-level mortality indicators across the United States during 2005 to 2015.
Methods
Independent Variable
Primary care physicians were defined as the number of non–federally employed physicians younger than 75 years who were not hospital residents and whose major professional activity was outpatient care in general practice, family medicine, general internal medicine, or general pediatrics, per 100 000 population in each US county and the District of Columbia (N = 3142 counties).15 Primary care physician counts were obtained from the American Medical Association Physician Masterfile for 2005, 2010, and 2015,16 and population counts were obtained from the US Census Bureau.17 Data were analyzed from March to July 2018. This study was approved by the Stanford University Institutional Review Board, which waived informed consent.
Outcomes
Life-expectancy (the primary outcome) and cause-specific mortality (secondary outcomes) were derived from deidentified death records from the National Center for Health Statistics and population counts from the US Census Bureau, National Center for Health Statistics, and the Human Mortality Database to estimate age-standardized life expectancy at birth and cause-specific mortality in 2005, 2010, and 2014 (updated to 2015 with linear interpolation at the county level).18 Five major categories of cause of death were considered: cardiovascular disease, cancer, infectious diseases, respiratory tract diseases, and substance use or injury (ie, deaths from alcohol use, drug use, self-harm, and interpersonal violence).
Covariates
We considered covariates that may confound the association between primary care physician supply and mortality at the population level (Table 1). These covariates included the number of specialist physicians with principal activity as patient care, per 100 000 population (defined by primary specialty in the American Medical Association Masterfile)16; urban/rural designation17; percentage of people under the federal poverty threshold and median household income in 2015 US dollars19; educational attainment20; population age, sex, and race/ethnicity21; unemployment status22; percentage of individuals without health insurance23; number of hospital beds per 100 000 population24; percentage enrolled in Medicare25; indicators of geographic variation in inflation-adjusted costs of medical care26; age-adjusted percentage of adults who currently smoked tobacco and percentage of adults with current obesity27; number of days with maximum 8-hour average pollution concentration greater than the National Ambient Air Quality Standard28; and median home value in 2015 US dollars.20
Table 1. Characteristics of the Study Sample of 3142 US Counties, 2005-2015.
| Characteristic | Mean (95% CI) | |||
|---|---|---|---|---|
| 2005 | 2010 | 2015 | Within-County Change, 2005 to 2015a | |
| Independent Predictor Variables | ||||
| Physicians per 100 000 populationb | ||||
| Total | 114.6 (0.0 to 425.7) | 111.6 (0.0 to 434.9) | 112.8 (0.0 to 461.3) | −1.9 (−64.0 to 67.1) |
| Primary care | 46.6 (0.0 to 114.6) | 44.0 (0.0 to 113.7) | 41.4 (0.0 to 108.6) | −5.2 (−44.6 to 28.8) |
| Specialist | 68.0 (0.0 to 326.7) | 67.6 (0.0 to 327.5) | 71.3 (0.0 to 356.2) | 3.4 (−40.1 to 58.9) |
| Nonmetro area, % | 67.3 | 73.0 | 73.0 | 5.7 |
| Population in poverty, %c,d | 15.3 (5.6 to 31.4) | 16.8 (7.0 to 31.8) | 16.3 (6.9 to 32.0) | 1.0 (−4.2 to 5.6) |
| Median household income, 2015 $US | 54 038.4 (34 370.7 to 90 744.6) | 53 068.2 (34 523.4 to 87 779.4) | 48 600.6 (30 622.5 to 80 641.5) | −5448 (−15 011.1 to 6711.5) |
| Population with less than high school education, % | 17.8 (6.4 to 37.7) | 15.4 (5.5 to 32.3) | 13 (3.2 to 29.2) | −4.8 (−16.7 to 4.3) |
| Population ≥65 y, % | 14.8 (7.6 to 24.1) | 15.8 (8.5 to 25.2) | 18.0 (10.0 to 27.9) | 3.1 (−1.4 to 7.9) |
| Population female, % | 50.3 (45.1 to 53.0) | 49.8 (43.3 to 53.6) | 50.0 (43.9 to 52.8) | −0.3 (−3.1 to 1.5) |
| Population black, % | 9.0 (0.0 to 53) | 9.1 (0.2 to 53.1) | 9.3 (0.3 to 53.2) | 0.3 (−2.7 to 3.1) |
| Population Hispanic, % | 7.1 (0.5 to 46.9) | 8.1 (0.8 to 50.4) | 9.2 (0.9 to 53.6) | 2.1 (−0.1 to 7.5) |
| Unemployment rate, % | 5.6 (2.8 to 12.3) | 9.4 (3.7 to 17.5) | 5.7 (2.5 to 12.4) | 0.1 (−2.3 to 3.1) |
| Uninsured among persons aged <65 y, % | 25.0 (13.0 to 40.4) | 18.5 (9.3 to 30.7) | 12 (4.7 to 23.2) | −13.0 (−25.4 to −4.0) |
| Hospital beds per 100 000 population | 358.6 (0.0 to 1733.0) | 324.3 (0.0 to 1462.3) | 294.7 (0.0 to 1336.0) | −63.2 (−592.9 to 185.9) |
| Medicare enrollment, % | 16.3 (7.0 to 26.4) | 18.3 (8.7 to 28.2) | 20.6 (9.8 to 32.0) | 4.3 (−1.4 to 10.6) |
| Geographic variation in terms of per capita medical costs, 2015, $US | 8946.3 (5734.3 to 13 002.4) | 9395.5 (7311.4 to 12 394.6) | 9843.4 (7790.6 to 12 676.8) | 898.4 (−2914.8 to 4608.3) |
| Adult tobacco smoking, % | 17.9 (12.7 to 25.6) | 21.3 (11.0 to 33.0) | 21.3 (11.0 to 33.0) | 3.4 (−5.9 to 12.2) |
| Adult obesity, % | 27.5 (19.0 to 34.0) | 30.7 (21.0 to 39.0) | 32.1 (21.0 to 42.7) | 4.5 (−3.0 to 13.0) |
| High pollution days, % | 4.7 (0.0 to 24.3) | 1.3 (0.0 to 9.3) | 6.2 (0.0 to 34.6) | 1.5 (−16.5 to 26.3) |
| Median home value 2015, $US | 158 526.7 (60 822.4 to 462 389.7) |
143 960.4 (63 335.6 to 371 204.1) |
129 446.3 (55 081.0 to 293 371.5) |
−29 080.4 (−192 909.3 to 45 054.4) |
| Dependent Outcome Variables | ||||
| Life expectancy at birth, age-standardized years | 76.8 (72.5 to 80.5) | 77.7 (73.2 to 81.5) | 77.8 (72.9 to 82.0) | 1.0 (0.1 to 1.9) |
| Age-adjusted deaths per 100 000 population | ||||
| Cancer | 214.1 (162.2 to 271.7) | 204.2 (149.8 to 264.1) | 206.9 (148.2 to 273.6) | −7.2 (−21.9 to 8.0) |
| Cardiovascular disease | 317.2 (215.7 to 439.7) | 278.4 (185.4 to 397.2) | 277.6 (179.6 to 406.6) | −39.6 (−66.6 to −12.9) |
| Infectious diseases | 38.8 (22.2 to 63.2) | 34.6 (18.3 to 58.8) | 34.8 (17.0 to 61.4) | −4.0 (−9.9 to 2.7) |
| Respiratory tract diseases | 62.3 (38.1 to 93.1) | 62.1 (35.5 to 95.0) | 64.2 (34.3 to 102.2) | 1.8 (−7.5 to 13.7) |
| Substance use or injury | 30.4 (16.3 to 53.8) | 33.3 (17.4 to 59.8) | 35.5 (17.9 to 64.7) | 5.1 (−1.3 to 15.1) |
| Interpersonal violence | 5.3 (1.6 to 15.2) | 4.9 (1.5 to 14.6) | 5.0 (1.6 to 14.7) | −0.3 (−1.9 to 0.7) |
Owing to rounding of displayed values in the table, within-county differences may differ at the tenths place from a simple subtraction of the second and fourth columns.
Physician counts are specific to the subset of physicians who list patient care as their primary occupational activity.
Absolute percentage.
Determined at county level.
Statistical Analysis
Overview of Analytic Approach
Because primary care physician supply cannot be randomized, we undertook a series of analyses to examine the association between primary care supply and the study outcomes using observational data. Our approach was to use a primary analytic method and then test the robustness of the associations found using complementary methods that make different assumptions or interrogate different aspects of the question. P values were 2-sided, with α set to .05 to determine statistical significance. Analyses were performed in R version 3.4.3 (R Foundation for Statistical Computing), using the statistical code deposited at https://sdr.stanford.edu.
Owing to completeness of mortality surveillance at the county level and primary care physician supply being ultimately an area-level concept, our primary analysis was to examine whether changes in primary care and specialist density within a county were associated with changes in age-adjusted life expectancy and cause-specific mortality within that county after controlling for the above characteristics. Because counties might not conform to care-seeking patterns, we repeated these analyses using alternative geographic levels—the primary care service area (N = 7144) and the hospital referral region (N = 306), which were developed based on geographic patterns of care. We also conducted additional sensitivity analyses as described below to test robustness.
Primary Analysis Mixed-Effects Models
For our area-level analyses, we used a linear mixed model to regress life expectancy against the independent variables within each county, allowing intercepts (baseline outcomes) to vary among counties, time trends to vary across the study period, and slopes for the association between physician density and each outcome to vary among counties. A mixed model empirically estimates the within- vs between-county components of variation in each outcome. Standard errors were computed with an autoregressive correlation structure to account for serial correlation in outcomes across time within counties, with county population weights. We excluded from the analysis the less than 5% of counties with any missing variable. Further details of the mixed-effects models are provided in the eAppendix in the Supplement. To address individuals crossing county boundaries for medical care, we repeated the modeling using geographically weighted regression with the latitude and longitude of county centroid to account for potential regional patterns of utilization and flow across boundaries.29,30
Instrumental Variable Analysis
To address the possibility for unmeasured confounding in our primary analyses, we conducted instrumental variable analyses. An instrumental variable is a factor that influences the outcome (mortality) only through its influence on the predictor variable of interest (primary care physician supply) but is not subject to reverse causality from the outcome or omitted variable bias. For example, the federal Public Service Loan Forgiveness program forgives some loan payments for physicians who enter into public service, commonly nonprofit community clinics; it is considered the major financial policy inducement for selecting primary care.31 Although the loan forgiveness amount is fixed, the purchasing power of the forgiven amount varies widely by county (eg, influencing the ability to purchase a house). This instrument was found to be strong (first-stage F = 25.6) for predicting primary care density, but not specialist density (F = 7.2).We thus used changes in county purchasing power to predict changes in primary care physician supply (eFigures 5 and 6 in the Supplement) and in turn associate changes in supply with changes in mortality through this instrumental variable. Additional details on the instrumental variable approach are provided in the eAppendix in the Supplement. We performed a robustness check on the instrumental variable analysis using near-far matching,32 an analytic strategy that can strengthen the power of an instrument by matching counties that are similar in their key characteristics (Table 1) but different in their values of the instrumental variable to mimic a matched-pair randomized trial (eAppendix in the Supplement).
Individual-Level Analyses
Individual-level analyses with a second data source were performed to reduce the likelihood of ecological confounding using a national claims database linked to date of death from the Social Security Death Master File33 (Optum Clinformatics Data Mart, 2003 through 2016; 1 505 554 individuals). We performed a survival analysis by estimating the Kaplan-Meier survival rate of participants, adjusted for censoring, to determine the association between area-level primary care physician supply and individual-level life expectancy. The outcome was restricted mean survival time, which is the area under the survival curve, conditional on exposure to area-level primary care physician density (equations are given in the eAppendix in the Supplement).34 We adjusted for all area-level covariates in Table 1 as well as for individual-level age and sex. Characteristics of the individual participants in the sample are provided in eTable 1 in the Supplement. A subgroup analysis was also conducted, focusing on individuals who moved between zip codes as a quasi-random exposure to changes in primary care physician density (Supplement).35
Falsification Testing
A falsification test was performed by regressing the independent variables against a dependent outcome variable that would not be expected to have a significant association with primary care physician supply: mortality due to interpersonal violence (eg, murder).18 This test examined whether unobserved factors, such as the propensity for physicians to move to desirable areas, which may have features correlated with lower mortality rates, would produce false associations between primary care physician density and improved outcomes.
In addition, we calculated the E value,36 which estimates how strong unmeasured confounders (factors correlated with both primary care physician supply and life expectancy) would need to be to explain away the association between primary care physician density and life expectancy.
Sensitivity Analyses
Our analyses were also repeated after including nurse practitioners and physician assistants with a national provider identifier registration who reported working in primary care per their Medicare registration information.16,37 Nurse practitioners and physician assistants are not registered consistently or labeled consistently as primary care over time, and thus they were not included in the prespecified primary model because their inclusion could produce misclassification error and regression to the mean.
Results
Changes in Primary Care Physician and Specialist Density
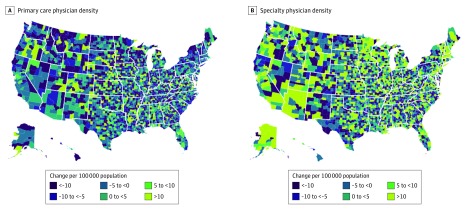
The total number of primary care physicians increased from 196 014 in 2005 to 204 419 in 2015. However, owing to disproportionate losses of primary care physicians in some counties and population increases in general, mean primary care physician supply decreased from 46.6 per 100 000 population in 2005 (95% CI, 0.0-114.6 per 100 000 population) to 41.4 per 100 000 in 2015 (95% CI, 0.0-108.6 per 100 000 population (Figure 1 and Table 1). Primary care physician supply per 100 000 population had a skewed distribution; 296 counties had no primary care physicians in 2015, whereas 128 counties had more than 100 per 100 000 population. Primary care physician supply declined more in rural than in urban counties on average (–7.0 per 100 000 population vs –2.6 per 100 000 population) but with broad changes in both (eFigure 1 in the Supplement). Owing to small populations, rural counties can appear to have large variations in primary care physician density; thus, the absolute changes were also analyzed and varied from a loss of 32 to a gain of 37 primary care physicians, with a median loss of 1.0 physician per county. Urban county primary care physician changes ranged from a loss of 179 to a gain of 405 primary care physicians, with a median gain of 1.0 physician per county. Primary care physician supply in either density or absolute terms did not disproportionately decrease by county poverty level or racial/ethnic demographic features (eFigures 1 and 7 in the Supplement). Density decreased by 4.2 physicians per 100 000 population at the primary care service area level (95% CI, –31.1 to 18.8 per 100 000 population), and by 4.4 per 100 000 population at the hospital referral region level (95% CI, –32.1 to 19.8 per 100 000 population).
Figure 1. Changes in Density of Primary Care and Specialist Physicians in 3142 US Counties, 2005-2015.
Concurrently, the number of specialist physicians increased from 699 989 in 2005 to 805 277 in 2015, corresponding to 68.0 per 100 000 population in 2005 to 71.3 per 100 000 population in 2015 (Figure 1, Table 1). In absolute terms, counties gained a mean (range) of 3.4 specialists (–359 to 1065 specialists) nationwide, but rural counties had no mean gain (eFigures 2 and 8 in the Supplement). Changes in primary care physician supply minimally correlated with changes in specialist physician supply (Pearson correlation coefficient, 0.14).
Associations Between Primary Care Physician Density and Life Expectancy
In adjusted regressions (Table 2), total physician supply, primary care physician supply, and specialist physician supply were associated with improved life expectancy.38 In fully adjusted models that accounted for both primary care and specialist physician supply, an increase of 10 primary care physicians per 100 000 population was associated with a 51.5-day increase in life expectancy (95% CI, 29.5-73.5 days; 0.2% increase) (Table 2), and a similar increase of 10 specialist physicians per 100 000 population was associated with a 19.2-day increase in life expectancy (95% CI, 7.0-31.3 days).38
Table 2. Results of Mixed-Effects Regressions Associating Physician Density and County-Level Covariates With Age-Standardized Life Expectancy at Birth in 3142 US Counties, 2005-2015.
| Variable | Change in Age-Standardized Life Expectancy (95% CI) | |||
|---|---|---|---|---|
| Model 1 (Total Physician Density) | Model 2 (Primary Care Physician Density) | Model 3 (Specialist Density) | Model 4 (Primary Care Physician and Specialist Density) | |
| Total physicians, per 100 000 populationa | 66.7 (47.5 to 85.8) | −NA | NA | NA |
| Covariate, per +10 physicians per 100 000b | 88.9 | NA | NA | NA |
| Primary care physicians, per 100 000 population | NA | 31.8 (17.7 to 45.9) | NA | 33.1 (19.0 to 47.3) |
| Covariate, per +10 physicians per 100 000b | NA | 49.7 | NA | 51.5 |
| Specialty physicians, per 100 000 population | NA | NA | 23.3 (9.3 to 37.3) | 20.6 (7.5 to 33.6) |
| Covariate, per +10 physicians per 100 000b | NA | NA | 21.7 | 19.2 |
| Metro area, change to nonmetro area, d | −54.6 (−79.8 to −29.5) | −55.8 (−81.0 to −30.7) | −51.0 (−76.5 to −25.6) | −54.2 (−79.4 to −29.0) |
| Population in poverty, d | −149.7 (−172.2 to −127.2) | −146.6 (−169.0 to −124.3) | −152.4 (−175.2 to −129.7) | −148.8 (−171.2 to −126.4) |
| Population with less than high school education, d | −59.5 (−73.5 to −45.5) | −58.1 (−71.9 to −44.3) | −59.4 (−73.5 to −45.3) | −58.1 (−72.0 to −44.3) |
| Female, d | −20.4 (−34.9 to −5.8) | −19.7 (−34.2 to −5.2) | −18.9 (−33.6 to −4.2) | −20.1 (−34.6 to −5.6) |
| Black, d | −409.4 (−448.9 to −370.0) | −406.5 (−445.8 to −367.2) | −408.6 (−448.4 to −368.8) | −411.9 (−451.2 to −372.6) |
| Hispanic, d | 185.9 (149.9 to 221.9) | 185.2 (149.3 to 221.1) | 185.1 (149.0 to 221.3) | 185.3 (149.4 to 221.1) |
| Unemployment rate, d | −13.7 (−28.2 to 0.8) | −14.1 (−28.6 to 0.3) | −15.6 (−30.2 to −0.9) | −14.1 (−28.5 to 0.4) |
| Hospital beds, per 100 000 population, d | −3.9 (−24.1 to 16.4) | −0.2 (−20.2 to 19.8) | −0.9 (−21.1 to 19.3) | −2.3 (−22.4 to 17.8) |
| Medicare enrollment, d | 106.4 (81.1 to 131.7) | 108.6 (83.5 to 133.7) | 111.0 (85.6 to 136.4) | 107.8 (82.6 to 132.9) |
| Per capita medical cost variation, d | 4.3 (−4.5 to 13.2) | 5.0 (−3.8 to 13.8) | 4.8 (−4.1 to 13.8) | 5.0 (−3.8 to 13.8) |
| Adult tobacco smoking, d | −52.8 (−63.4 to −42.3) | −52.6 (−63.1 to −42.1) | −54.0 (−64.6 to −43.4) | −52.3 (−62.8 to −41.8) |
| Adult obesity, d | −39.1 (−49.3 to −28.9) | −39.2 (−49.4 to −29.0) | −40.3 (−50.7 to −30.0) | −39.3 (−49.5 to −29.1) |
| High pollution days, d | −21.2 (−28.7 to −13.8) | −21.1 (−28.5 to −13.7) | −22.3 (−29.8 to −14.8) | −21.1 (−28.5 to −13.7) |
| Median home value, d | −22.0 (−42.4 to −1.6) | −22.5 (−42.7 to −2.3) | −19.9 (−40.4 to 0.7) | −23.2 (−43.5 to −3.0) |
Abbreviation: NA, not applicable.
All means and SDs calculated after log transformation. Total physician coefficient corresponds to the change from mean minus 1 SD (61.0 physicians) to mean plus 1 SD (68.5 physicians); primary care, to the change from mean minus 1 SD (27.3 physicians) to mean plus 1 SD (33.7 physicians); specialty, to the change from mean minus 1 SD (21.3 physicians) to mean plus 1 SD (32.0 physicians); population in poverty, to the change from mean minus 1 SD (13.4% poverty) to mean plus 1 SD (16.4% poverty); population with less than high school education, to change from mean minus 1 SD (13.1% less than high school) to mean plus 1 SD (16.3% less than high school); population female, to change from mean minus 1 SD (48.9% female) to mean plus 1 SD (51.0% female); population black, to change from mean minus 1 SD (1.4% black) to mean plus 1 SD (7.9% black); population Hispanic, to change from mean minus 1 SD (2.8% Hispanic) to mean plus 1 SD (7.8% Hispanic); unemployment rate to change from mean minus 1 SD (4.7% unemployed) to mean plus 1 SD (7.8% unemployed); hospital beds, to change from mean minus 1 SD (32.6 hospital beds) to mean plus 1 SD (61.2 hospital beds); Medicare enrollment, to change from mean minus 1 SD (17.2% enrolled) to mean plus 1 SD (19.9% enrolled); per capita medical cost variation, to change from mean minus 1 SD ($9268.5) to mean plus 1 SD ($9270.9); adult tobacco smoking, to change from mean minus 1 SD (18.0% smoking) to mean plus 1 SD (20.6% smoking); adult obesity, to change from mean minus 1 SD (28.5% obesity) to mean plus 1 SD (30.9% obesity); high pollution days, to change from mean minus 1 SD (0% of days) to mean plus 1 SD (5.4% of days); and median home value, from change from mean minus 1 SD ($126 825.2) to mean plus 1 SD ($126 828.5).
Continuous variables were log transformed and centered and scaled by 2 SDs, which allows coefficients for continuous covariates to reflect the change in the outcome variable given a change in the independent variable from its mean minus 1 SD to its mean plus 1 SD on the logged scale, correcting for right skew and enabling fair comparison of magnitudes among regression coefficients.38
To contextualize these results, the association of primary care physician density and life expectancy (+33.1 days of life expectancy for a 2-SD increase in physician density) was approximately one-fifth the magnitude of the association between poverty and life expectancy (148.8 days for a 2-SD increase), and approximately two-thirds the magnitude of the association between tobacco and life expectancy (52.3 days for a 2-SD increase; eTable 2, Table 2).38
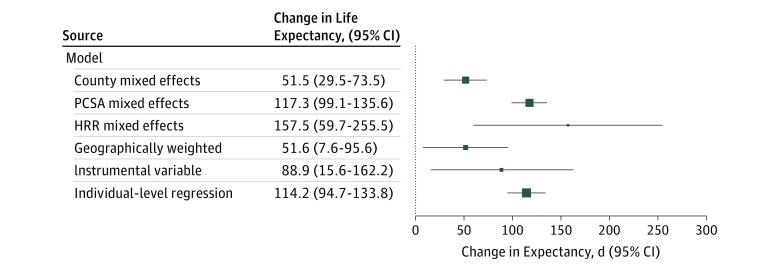
Analyses at alternative geographic levels revealed similar associations between primary care physician supply and life expectancy (Figure 2; increase of 51.5 days life expectancy per 10 additional physicians at the county level, an increase of 117.3 at the PCSA level, and an increase of 157.5 at the HRR level). The geographically weighted regression results also were consistent (Table 2; Figure 2).
Figure 2. Changes in Life Expectancy Associated With an Increase in 10 Primary Care Physicians per 100 000 Population Using Alternative Model Specifications.
Additional alternative specifications are available in the Supplement. Data to the right of 0 reflect an increase in life expectancy in days. Larger marker size indicates more concentrated distributions (lower variance). Error bars indicate 95% CIs. PCSA indicates primary care service area; HRR, hospital referral region.
Association Between Primary Care Physician Density and Cause-Specific Mortality
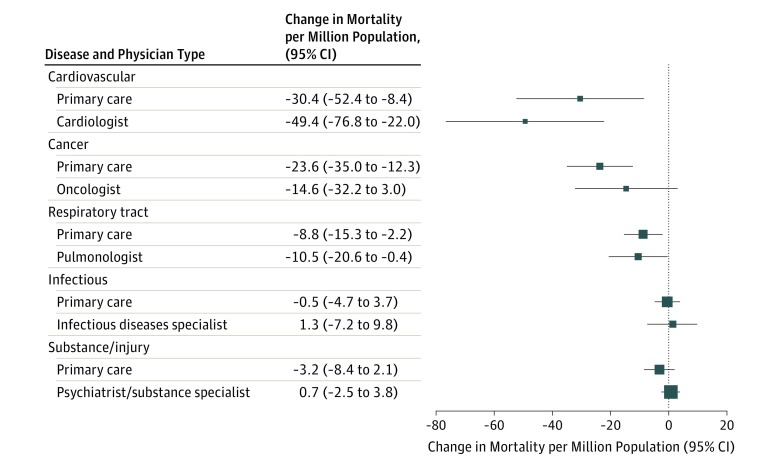
An increase of 10 primary care physicians per 100 000 population was associated with a reduction in cardiovascular mortality by 30.4 deaths per million (95% CI, –52.4 to–8.4; a 0.9% reduction), in cancer mortality by 23.6 deaths per million (95% CI, –35.0 to –12.3 deaths per million; 1.0% reduction), and in respiratory mortality by 8.8 deaths per million (95% CI, –15.3 to –2.2 deaths per million; a 1.4% reduction) after adjustment for covariates (Figure 3). Specialty physician supply was associated with significant reductions in cause-specific mortality for 2 groups: cardiologists and cardiovascular mortality (increase of 10 cardiologists associated with –49.4 deaths per million [95% CI, –76.8 to –22.0 deaths per million]) and pulmonologists and respiratory tract disease mortality (10 pulmonologists associated with –10.5 deaths per million [95% CI, –20.6 to –0.4 deaths per million]; Figure 3).
Figure 3. Changes in Cause-Specific Mortality Associated With an Increase in 10 Primary Care Physicians or 10 Specialist Physicians per 100 000 Population.
Data to the left of 0 indicate a decrease in mortality while data to the right of 0 indicate an increase in mortality in deaths per million population. Larger marker size indicates more concentrated distributions (lower variance). Error bars indicate 95% CI.
Instrumental Variable Analyses
An increase of 10 primary care physicians per 100 000 population was associated with an 88.9-day (95% CI, 15.6-162.2 days) increase in life expectancy in the instrumental variable analysis (Figure 2). The instrumental variable analysis also detected associations between primary care physician supply and lower cardiovascular, cancer, and respiratory mortality (eFigure 3 in the Supplement). Results were similar in the near-far matching analysis (eFigure 4 in the Supplement).
Individual-Level Analysis
In the individual-level analysis, survival time increased by 114.2 days (95% CI, 94.7-133.8 days) per decade of exposure to 10 more primary care physicians per 100 000 population (Figure 2). Results were also improved among a subgroup who moved between zip codes (eAppendix in the Supplement).
Falsification Testing
Increased primary care physician supply was not significantly associated with deaths from interpersonal violence. An increase of 10 primary care physicians per 100 000 population was associated with –0.5 death per million from violence (95% CI, –1.4 to 0.5 deaths per million).
The E value for the association between primary care physician supply and life expectancy was 131.2 days. This means that unmeasured confounders correlated with both primary care physician density and life expectancy would have to have strong associations with life expectancy (a 131.2-day increase in life expectancy is almost as great in magnitude as the association between poverty and life expectancy, Table 2) to explain away the observed association between primary care physician supply and life expectancy.38
Sensitivity Analyses
When including primary care nurse practitioners and physician assistants in the analysis, an increase in primary care clinician supply (physician, nurse practitioner, or physician assistant) by 10 per 100 000 population showed consistent results (increase in life expectancy, 36.4 days; 95% CI, –19.0 to 91.8 days), but the result was no longer statistically significant at the county level. Counties had a mean of 25.2 nurse practitioners and physician assistants in primary care per 100 000 population in 2005 (95% CI, 0.0-60.8 per 100 000 population) and 50.1 per 100 000 population in 2015 (0.0-141.1 per 100 000 population).
Discussion
Although the total number of primary care physicians has increased in the United States, owing to disproportionate rural losses and general population size increases, the distribution of US primary care physicians per 100 000 population has changed, leading to a net loss in mean primary care physician supply at the county level. Greater primary care physician supply was associated with lower population mortality, suggesting that observed decreases in primary care physician supply may have important consequences for population health. These findings were consistent across several analytic specifications that varied the unit of analysis, level of analyses, and statistical assumptions underpinning the analysis.
The results of this study reinforce findings from earlier cross-sectional studies evaluating data from the 1990s, which suggested associations at the health care system and state levels between primary care physician density, overall life expectancy, cardiovascular disease deaths, and cancer deaths.1,3,8,10,39,40 However, similar to another study,41 our results are driven by changes in density over time within counties, which reduces confounding by features of areas that might have affected earlier research. Our study included a larger number of control variables than previous analyses, including specialist physician supply and numerous health care, socioeconomic, environmental, and demographic features omitted from earlier studies. The largest decreases in cause-specific mortality associated with increased primary care physician density were for cardiovascular disease, cancer, and respiratory tract disease, conditions with strong evidence of amenability to primary care management or with delayed mortality conditional on early screening through primary care.8,10,31,42,43,44
Many believe that a well-functioning health care system requires a solid foundation of primary care. However, persistent payment disparities between primary care and procedural specialties continue to erode the US primary care physician workforce.45,46 Policy initiatives, such as Medicare’s Accountable Care Organization programs, that attempt to focus on population health and spending and thereby rely on primary care physicians continue to gain traction, but these programs fail to explicitly direct more resources to primary care physician supply, instead relying on the usual Medicare fee schedule. The Centers for Medicare & Medicaid Service’s Comprehensive Primary Care initiative invests more resources in primary care, and states such as Rhode Island and Oregon have substantially increased spending on primary care.47 Whether these initiatives will encourage more graduating medical students to enter primary care remains to be seen. Other forms of investment, such as the National Health Services Corps, the Teaching Health Centers program, and Title VII programs, also offer the opportunity to increase the density of primary care physicians, especially in underserved areas.
Limitations
Our study has important limitations. First, our main analysis was appropriately ecological, because we sought to identify relationships between population-level physician supply and population-level variations in mortality. However, to avoid the ecological fallacy, conclusions should not be drawn about individual-level effects of population-level associations. To help mitigate this limitation, we conducted individual-level analyses using private insurance data. Although not nationally representative, the individuals in the insurance data were from all 50 states, Washington, DC, and Puerto Rico, covering 61% of US zip codes. Second, there remains the possibility for unobserved confounding, because we cannot randomize people to areas with varied primary care physician supply. We sought to address this with instrumental variable analyses, but the instrumental variable analysis has its own assumptions. Finally, our analysis focused on primary care physician supply relative to population size because this is a key focus of current policies.48,49,50
Conclusions
Across a number of analytic approaches, greater primary care physician supply was associated with improved mortality outcomes. The decrease in primary care physician supply across US counties from 2005 to 2015 may have important population health implications. Future investigations should acquire data on the quality and comprehensiveness of primary care, types of primary care physician training and service delivery offerings, and effective access rather than just supply. In addition, future analyses should explore the dynamics of teamwork across primary care physicians and specialists in both traditional and alternative payment models to address how team-based approaches may affect mortality and other outcomes.
eAppendix.
eReferences
eTable 1. Characteristics of Individuals in the Claims Data, 2003-2016
eTable 2. Interaction Analyses
eFigure 1. Changes in Primary Care Physician Supply
eFigure 2. Changes in Specialist Physician Supply
eFigure 3. Instrumental Variable Regression Results for Cause-Specific Mortality
eFigure 4. Near-Far Matching Results for Cause-Specific Mortality
eFigure 5. County-Level Estimated Price Parities, 2015
eFigure 6. Distribution of the Instrumental Variable
eFigure 7. Regression Tree Analysis of Changes in Primary Care Physician Supply
eFigure 8. Regression Tree Analysis of Changes in Specialist Physician Supply
References
- 1.Shi L, Macinko J, Starfield B, Politzer R, Xu J. Primary care, race, and mortality in US states. Soc Sci Med. 2005;61(1):65-75. doi: 10.1016/j.socscimed.2004.11.056 [DOI] [PubMed] [Google Scholar]
- 2.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US States, 1980-1995. J Am Board Fam Pract. 2003;16(5):412-422. doi: 10.3122/jabfm.16.5.412 [DOI] [PubMed] [Google Scholar]
- 3.Shi L, Macinko J, Starfield B, Xu J, Politzer R. Primary care, income inequality, and stroke mortality in the United States: a longitudinal analysis, 1985-1995. Stroke. 2003;34(8):1958-1964. doi: 10.1161/01.STR.0000082380.80444.A9 [DOI] [PubMed] [Google Scholar]
- 4.Shi L, Macinko J, Starfield B, et al. Primary care, infant mortality, and low birth weight in the states of the USA. J Epidemiol Community Health. 2004;58(5):374-380. doi: 10.1136/jech.2003.013078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shi L, Starfield B. The effect of primary care physician supply and income inequality on mortality among blacks and whites in US metropolitan areas. Am J Public Health. 2001;91(8):1246-1250. doi: 10.2105/AJPH.91.8.1246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi: 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Friedberg MW, Hussey PS, Schneider EC. Primary care: a critical review of the evidence on quality and costs of health care. Health Aff (Millwood). 2010;29(5):766-772. doi: 10.1377/hlthaff.2010.0025 [DOI] [PubMed] [Google Scholar]
- 8.Campbell RJ, Ramirez AM, Perez K, Roetzheim RG. Cervical cancer rates and the supply of primary care physicians in Florida. Fam Med. 2003;35(1):60-64. https://www.ncbi.nlm.nih.gov/pubmed/12564867. Accessed May 30, 2018. [PubMed] [Google Scholar]
- 9.Chang C-H, Stukel TA, Flood AB, Goodman DC. Primary care physician workforce and Medicare beneficiaries’ health outcomes. JAMA. 2011;305(20):2096-2104. doi: 10.1001/jama.2011.665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Roetzheim RG, Gonzalez EC, Ramirez A, Campbell R, van Durme DJ. Primary care physician supply and colorectal cancer. J Fam Pract. 2001;50(12):1027-1031. https://www.ncbi.nlm.nih.gov/pubmed/11742602. Accessed May 30, 2018. [PubMed] [Google Scholar]
- 11.Weida NA, Phillips RL Jr, Bazemore AW. Does graduate medical education also follow green? Arch Intern Med. 2010;170(4):389-390. doi: 10.1001/archinternmed.2009.529 [DOI] [PubMed] [Google Scholar]
- 12.Chen C, Petterson S, Phillips RL, Mullan F, Bazemore A, O’Donnell SD. Toward graduate medical education (GME) accountability: measuring the outcomes of GME institutions. Acad Med. 2013;88(9):1267-1280. doi: 10.1097/ACM.0b013e31829a3ce9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Eden J, Berwick D, Wilensky G. Graduate Medical Education That Meets the Nation’s Health Needs. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- 14.Schoen C, Guterman S, Shih A, et al; the Commonwealth Fund. Bending the curve: options for achieving savings and improving value in U.S. health spending. 2007. https://www.commonwealthfund.org/publications/fund-reports/2007/dec/bending-curve-options-achieving-savings-and-improving-value-us. Accessed January 11, 2019.
- 15.Health Resources and Services Administration Area health resource files. https://data.hrsa.gov/data/download. Published 2017. Accessed April 2, 2018.
- 16.American Medical Association Physician Masterfile. American Medical Association. https://www.ama-assn.org/life-career/ama-physician-masterfile. Published 2016. Accessed April 2, 2018.
- 17.CDC/National Center for Health Statistics Urban rural classification scheme for counties. https://www.cdc.gov/nchs/data_access/urban_rural.htm. Published 2017. Accessed April 2, 2018.
- 18.Dwyer-Lindgren L, Bertozzi-Villa A, Stubbs RW, et al. Trends and Patterns of Geographic Variation in Mortality From Substance Use Disorders and Intentional Injuries Among US Counties, 1980-2014. JAMA. 2018;319(10):1013-1023. doi: 10.1001/jama.2018.0900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.US Census Bureau Small Area Income and Poverty Estimates (SAIPE) Program. https://www.census.gov/programs-surveys/saipe.html. Published 2017. Accessed April 2, 2018.
- 20.US Census Bureau American Community Survey (ACS). https://www.census.gov/programs-surveys/acs/. Published 2016. Accessed April 2, 2018.
- 21.US Census Bureau County population by characteristics: 2010-2017. https://www.census.gov/data/datasets/2017/demo/popest/counties-detail.html. Published 2017. Accessed April 2, 2018.
- 22.US Bureau of Labor Statistics Databases, tables and calculators by subject. https://data.bls.gov/timeseries/LNS14000000. Published 2018. Accessed April 2, 2018.
- 23.US Census Bureau Small Area Health Insurance Estimates (SAHIE) program. https://www.census.gov/programs-surveys/sahie.html. Published 2016. Accessed April 2, 2018.
- 24.American Hospital Association Annual survey database. http://www.ahadata.com/aha-annual-survey-database-asdb/. Published 2017. Accessed April 2, 2018.
- 25.Centers for Medicare & Medicaid Services Medicare enrollment dashboard. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/CMSProgramStatistics/Dashboard.html. Published 2016. Accessed April 2, 2018.
- 26.Centers for Medicare & Medicaid Services. Geographic variation public use files. https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/Medicare-Geographic-Variation/GV_PUF.html. Published 2017. Accessed April 2, 2018.
- 27.National Center for Chronic Disease Prevention and Health Promotion Behavioral risk factor surveillance system. https://www.cdc.gov/brfss/brfssprevalence/index.html. Published 2017. Accessed April 2, 2018.
- 28.Centers for Disease Control and Prevention National environmental public health tracking. https://www.cdc.gov/nceh/tracking/. Published 2017. Accessed April 2, 2018.
- 29.Gollini I, Lu B, Charlton M, Brunsdon C, Harris P. GWmodel: an R Package for exploring spatial heterogeneity using geographically weighted models. J Stat Softw. 2015;63(17). doi: 10.18637/jss.v063.i17 [DOI] [Google Scholar]
- 30.US Census Bureau 2015 US Gazetteer Files. 2015. https://www.census.gov/geo/maps-data/data/gazetteer2015.html. Accessed January 11, 2019. [Google Scholar]
- 31.Akinbami LJ, Moorman JE, Liu X. Asthma prevalence, health care use, and mortality: United States, 2005-2009. Natl Health Stat Report. 2011;(32):1-14. https://www.ncbi.nlm.nih.gov/pubmed/21355352. Accessed July 17, 2018. [PubMed] [Google Scholar]
- 32.Baiocchi M, Small DS, Lorch S, Rosenbaum PR. Building a stronger instrument in an observational study of perinatal care for premature infants. J Am Stat Assoc. 2010;105(492):1285-1296. doi: 10.1198/jasa.2010.ap09490 [DOI] [Google Scholar]
- 33.Schisterman EF, Whitcomb BW. Use of the Social Security Administration Death Master File for ascertainment of mortality status. Popul Health Metr. 2004;2(1):2. doi: 10.1186/1478-7954-2-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kim DH, Uno H, Wei LJ. Restricted mean survival time as a measure to interpret clinical trial results. JAMA Cardiol. 2017;2(11):1179-1180. doi: 10.1001/jamacardio.2017.2922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Finkelstein A, Gentzkow M, Williams H. Sources of geographic variation in health care: evidence from patient migration. Q J Econ. 2016;131(4):1681-1726. doi: 10.1093/qje/qjw023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the e-value. Ann Intern Med. 2017;167(4):268-274. doi: 10.7326/M16-2607 [DOI] [PubMed] [Google Scholar]
- 37.Centers for Medicare and Medicaid Services National Plan and Provider Enumeration System. Washington, DC: NPPES; 2018. [Google Scholar]
- 38.Gelman A. Scaling regression inputs by dividing by two standard deviations. Stat Med. 2008;27(15):2865-2873. doi: 10.1002/sim.3107 [DOI] [PubMed] [Google Scholar]
- 39.Shi L, Macinko J, Starfield B, Wulu J, Regan J, Politzer R. The relationship between primary care, income inequality, and mortality in US States, 1980-1995. J Am Board Fam Pract. 2003;16(5):412-422. doi: 10.3122/jabfm.16.5.412 [DOI] [PubMed] [Google Scholar]
- 40.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within Organization for Economic Cooperation and Development (OECD) countries, 1970-1998. Health Serv Res. 2003;38(3):831-865. doi: 10.1111/1475-6773.00149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chang C-H, O’Malley AJ, Goodman DC. Association between temporal changes in primary care workforce and patient outcomes. Health Serv Res. 2017;52(2):634-655. doi: 10.1111/1475-6773.12513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bunker JP. Medicine matters after all. J R Coll Physicians Lond. 1995;29(2):105-112. https://www.ncbi.nlm.nih.gov/pubmed/7595883. Accessed March 27, 2018. [PMC free article] [PubMed] [Google Scholar]
- 43.Mackenbach JP. The contribution of medical care to mortality decline: McKeown revisited. J Clin Epidemiol. 1996;49(11):1207-1213. doi: 10.1016/S0895-4356(96)00200-4 [DOI] [PubMed] [Google Scholar]
- 44.Ferrante JM, Gonzalez EC, Pal N, Roetzheim RG. Effects of physician supply on early detection of breast cancer. J Am Board Fam Pract. 2000;13(6):408-414. https://www.ncbi.nlm.nih.gov/pubmed/11117337. Accessed April 30, 2018. doi: 10.3122/15572625-13-6-408 [DOI] [PubMed] [Google Scholar]
- 45.Council on Graduate Medical Education Twentieth Report: Advancing Primary Care Rockville, MD: Health Resources and Services Administration; 2010.
- 46.Phillips R, Dodoo M, Petterson S, Xierali I, Bazemore A. Specialty and Geographic Distribution of the Physician Workforce: What Influences Medical Student & Resident Choices. Washington DC: Robert Graham Center; 2009. [Google Scholar]
- 47.Koller CF, Khullar D. Primary care spending rate—a lever for encouraging investment in primary care. N Engl J Med. 2017;377(18):1709-1711. doi: 10.1056/NEJMp1709538 [DOI] [PubMed] [Google Scholar]
- 48.Petterson SM, Liaw WR, Tran C, Bazemore AW. Estimating the residency expansion required to avoid projected primary care physician shortages by 2035. Ann Fam Med. 2015;13(2):107-114. http://www.annfammed.org/content/13/2/107.short. Accessed July 17, 2018. doi: 10.1370/afm.1760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.DesRoches CM, Buerhaus P, Dittus RS, Donelan K. Primary care workforce shortages and career recommendations from practicing clinicians. Acad Med. 2015;90(5):671-677. doi: 10.1097/ACM.0000000000000591 [DOI] [PubMed] [Google Scholar]
- 50.Xue Y, Greener E, Kannan V, Smith JA, Brewer C, Spetz J. Federally qualified health centers reduce the primary care provider gap in health professional shortage counties. Nurs Outlook. 2018;66(3):263-272.https://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=29685322&dopt=Abstract doi: 10.1016/j.outlook.2018.02.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix.
eReferences
eTable 1. Characteristics of Individuals in the Claims Data, 2003-2016
eTable 2. Interaction Analyses
eFigure 1. Changes in Primary Care Physician Supply
eFigure 2. Changes in Specialist Physician Supply
eFigure 3. Instrumental Variable Regression Results for Cause-Specific Mortality
eFigure 4. Near-Far Matching Results for Cause-Specific Mortality
eFigure 5. County-Level Estimated Price Parities, 2015
eFigure 6. Distribution of the Instrumental Variable
eFigure 7. Regression Tree Analysis of Changes in Primary Care Physician Supply
eFigure 8. Regression Tree Analysis of Changes in Specialist Physician Supply