Key Points
Question
What are the attitudes and decision making concerning invasive and noninvasive prenatal testing in women at high risk of fetal Down syndrome?
Findings
In a survey study of 2436 pregnant women in France participating in a randomized clinical trial, 4 clusters were identified with different attitudes toward risk taking and extent of information seeking. Decision making was in line with attitudes, and clinical and socioeconomic factors were likely associated with the attitudes identified.
Meaning
Aversion to ambiguity generated by incomplete information from noninvasive testing as well as aversion to risk of pregnancy loss due to invasive testing played a major role in shaping attitudes and decision making; therefore, pregnant women should receive extensive information on targeted abnormalities by both tests to aid informed decision making.
This survey study examines the attitudes of pregnant women in France at high risk of fetal Down syndrome toward invasive and noninvasive prenatal testing.
Abstract
Importance
Noninvasive prenatal testing (NIPT) using cell-free DNA in maternal blood is increasingly common compared with invasive testing (IT) in routine antenatal detection of Down syndrome (DS).
Objective
To assess attitudes and decision making in pregnant women facing a risk of fetal DS greater than 1 in 250 as established by combined first trimester screening at 11 to 14 weeks of gestation.
Design, Setting, and Participants
Survey study in which data were collected from pregnant women at high risk of fetal DS participating in a randomized clinical trial. Data were collected from April 8, 2014, to April 7, 2016, in 57 prenatal diagnosis centers in France. Data were analyzed in 2018.
Interventions
Data on attitudes were collected prior to offering randomization between NIPT and IT, whereas data on decision making and test results were collected as part of the clinical trial.
Main Outcome and Measures
The primary outcome related to attitudes. A hierarchical cluster analysis was conducted to identify clusters with contrasting attitudes. Logistic regression analyses were used to identify factors associated with attitudes.
Results
All 2436 consecutive women to whom the study was proposed (mean [SD] age, 36.3 [5.0] years) answered the questionnaire: 515 (21.1%) expressed preference toward IT with complete karyotyping, whereas 1843 (75.7%) favored NIPT with almost certain but limited information. Hierarchical cluster analysis yielded 4 different clusters that mainly differed in attitudes toward risk taking and extent of information seeking. Factors likely associated with attitudes driven by risk aversion were mostly age and religious beliefs (adjusted odds ratio [aOR], 1.03; 95% CI, 1.00-1.05; P = .03 and aOR, 1.62; 95% CI, 1.29-2.04; P < .001, respectively), whereas higher nuchal translucency measurements by ultrasonography were associated with attitudes driven by ambiguity aversion (aOR, 1.67; 95% CI, 1.27-2.20; P < .001). For attitudes involving both risk and ambiguity aversion at different extents, lower education was associated with highly valuing all possibilities of getting information on pregnancy, whereas higher education was associated with highly valuing information on fetal DS as a primary concern (aOR, 0.54; 95% CI, 0.44-0.67; P < .001 and aOR, 1.44; 95% CI, 1.20-1.74; P < .001, respectively). In all, decision making was in line with attitudes.
Conclusions and Relevance
Aversion to risk of fetal loss related to IT and aversion to ambiguity generated by incomplete information from NIPT played a major role in shaping attitudes and decision making. Informed decision making should require pregnant women at high risk of DS to receive extensive information on targeted abnormalities by both tests.
Introduction
Prenatal screening for Down syndrome (DS) is widely performed at 11 to 14 weeks of gestation by using a combination of maternal age, measurements of fetal nuchal translucency by ultrasonography, and maternal serum concentrations of free human chorionic gonadotropin and plasma protein A.1 Various cutoffs of risk have been chosen to offer invasive testing (IT) as a second step, usually between 1 in 100 and 1 in 300.1 More recently, noninvasive prenatal testing (NIPT) using cell-free DNA circulating in maternal plasma has emerged as an intermediate step within a conditional screening algorithm, as the positive predictive value of combined screening is around 1 in 16 for DS.2,3,4,5,6,7 In contrast with IT, which involves a risk of miscarriage but provides full information on all possible chromosomal abnormalities, NIPT carries no risk of miscarriage but only provides information on the targeted abnormalities and only in terms of very high likelihood of their presence or absence. Indeed, the accuracy of cell-free-DNA to detect DS is around 99% with a 0.1% false-positive rate, and IT is carried out to confirm a positive result.8 As a result, NIPT therefore involves both a risky, although almost certain, component about targeted abnormalities together with an uncertain component about nontargeted abnormalities. In addition to the well-known attractiveness of certainty in decision making (also known as the certainty effect9,10), presenting information involving both risky and uncertain components is known to trigger ambiguity aversion11,12 as a result of a preference for known risks (probabilities) over unknown risks.13 Decision making between IT and NIPT could therefore be driven by aversion toward ambiguous information as much as by IT-related pregnancy loss risk aversion.
The present study aimed to explore attitudes of pregnant women who are about to make their decision following positive combined screening for DS. Considering the question addressed about the possible role of ambiguity aversion in addition to risk aversion in shaping preferences and decision making, this study involved assessing attitudes, factors likely associated with attitudes, and consistency between attitudes and actual decision making in high-risk women invited to participate in a multicenter randomized trial of IT vs NIPT.14
Methods
Data on pregnant women’s attitudes were collected within the framework of a randomized clinical trial comparing risk and effectiveness of NIPT and IT at a national level, involving 57 prenatal diagnosis centers (ClinicalTrials.gov identifier NCT02127515). Women with a fetal DS gestation-specific risk of 1 in 250 or greater following combined screening were invited to enroll in the clinical trial. They received one-on-one extensive information and counseling on the significance of this result as well as on advantages and risks attached to both IT and NIPT options.14 More specifically, the information provided to all participants as to the risks and benefits of each group of the study included issues relating to culture failure and mosaicism with IT as well as the chance of false-negative results with NIPT. The extent of counselling was intended to minimize the role of the heterogeneity of women’s access to relevant information prior to prenatal screening. Pregnant women were then asked to fill out a self-administered electronic questionnaire on site (eAppendix in the Supplement) exploring their attitude toward IT and NIPT in this high-risk situation. They were then asked to participate in the randomized clinical trial comparing NIPT and IT. Participants provided written informed consent and the study received ethics committee approval as part of the multicenter randomized trial. This study followed the American Association for Public Opinion Research (AAPOR) reporting guideline.
Exclusion criteria were multiple pregnancies and nuchal translucency measurements over 3 mm, as this could be a marker of other submicroscopic chromosomal disorders that would not be detectable by NIPT and only by IT. Another exclusion criterion was the absence of medical coverage by the French national health insurance system. Women who declined to participate in the trial, whether they refused prior to randomization between IT vs NIPT or their randomized assignment to NIPT, still had the possibility of undergoing IT without extra charges because these women remained eligible for full coverage by the French national health insurance system. On the contrary, women who refused their randomized assignment to IT and then decided to undergo NIPT had to pay for it. As a result, opting for IT after negative NIPT led to pregnancy risk taking without financial cost, whereas declining IT to opt for NIPT did not involve pregnancy risk taking but was financially costly.
Questionnaire
In addition to sociodemographic characteristics, the questionnaire included 23 questions on decision making about DS screening, understanding of combined screening test results, and attitudes toward IT-related fetal loss as compared with the birth of a child with DS. Specifically, the questionnaire addressed attitudes about the trade-off between risk taking and extent of information seeking, preferences between carrying out IT and NIPT, preference-based measurements using visual analog scales (VAS; from 0-10 with higher or lower scores indicating stronger preference for IT or NIPT, respectively), and decisional attitudes. Risk of fetal loss related to IT was rated to be around 1% as it is mentioned on French informed consent forms. Lastly, clinical data were available from the trial, including nuchal translucency measurements, calculated risk of DS from combined screening, gravidity, parity, smoking status, and IT uptake and diagnosis of chromosomal abnormalities in previous pregnancies. Miscarriages in previous pregnancies were also identified.
Statistical Analysis
Women’s attitudes were assessed using a hierarchical cluster analysis15 aiming to allocate individuals to groups as suggested by the recorded data; these groups were therefore not defined a priori. Using the Euclidean metric to compute distances between individuals and to cluster them,16 the agglomerative hierarchical procedure first involved each observation to be a cluster by itself. Then, the 2 closest clusters were merged to form a new one, and this procedure was repeated until only 1 cluster was left.17 The optimum number of clusters was determined using a 2-fold criterion: minimization of the interindividual distances within a cluster (within-group homogeneity) and maximization of the distances between the centers of gravity of clusters (between-cluster heterogeneity). Individuals in a given cluster tended to be similar for the variables selected for analysis, while individuals with contrasting characteristics were allocated to different clusters. Typical patterns of attitudes were thus identified as a result of the hierarchical cluster analysis. Each cluster was characterized by the variables that contributed significantly to its formation, using P values calculated by multiscale bootstrap resampling methods. Because of collinearity issues between the variables relating to women’s preferences and associated VAS scores, VAS scores were used as an illustrative variable that was not involved in the calculations but was used to illustrate statistical results. The hierarchical cluster analysis was carried out using the SPAD software package (Coheris).
Statistical analysis also involved logistic regressions to assess the relative effects of various factors on women’s attitudes. All variables associated with a P value less than .10 in the univariate analyses were taken to be eligible for the multivariable analysis. Using a backward selection procedure, only variables remaining independently and significantly associated with the outcome with a 2-tailed P value less than .05 were kept in the final model.
Results
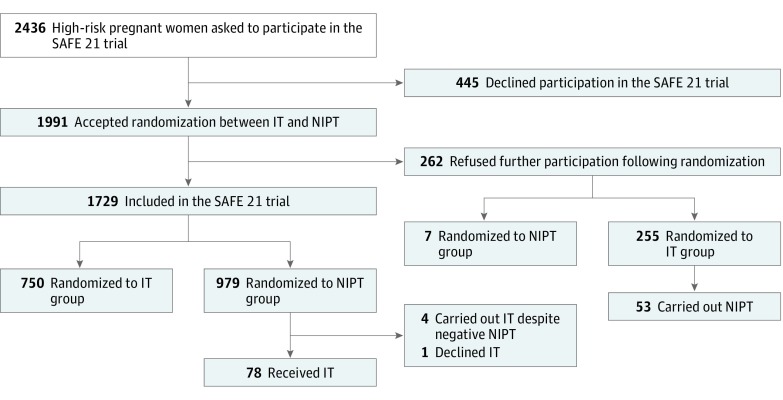
The present study was proposed to 2592 consecutive pregnant women at high risk for fetal DS from April 8, 2014, to April 7, 2016. Among these women, 33 declined to participate in the trial and refused to fill out the questionnaire, whereas 123 participated in the trial but did not fill out the questionnaire. As a result, 2436 questionnaires of consecutive pregnant women at high risk for DS were studied (Figure).
Figure. Participant Flowchart.
IT indicates invasive testing; NIPT, noninvasive prenatal testing.
Clinical and sociodemographic characteristics of the women together with their understanding of their own risk of fetal DS are presented in Table 1. Overall, mean (SD) maternal age was 36.3 (5.0) years, 12.6% had IT in a previous pregnancy, and 4.2% experienced fetal chromosomal abnormalities in a previous pregnancy. Fetal risk of DS ranged from 0.004 to 0.20 (mean, 0.01). In addition, two-thirds of the women reached at least upper secondary educational level, and about a third reported religion to be very or fairly important to them. Self-assessment of their level of risk for DS was consistent with the calculated risk from combined screening (P < .001): a 0.0203 average calculated risk was observed in the pregnant women who considered their risk as very high, whereas a 0.0101 and 0.0075 average calculated risk was associated to perceived risk as high or rather low, respectively. However, women with an educational level below secondary school graduation were more likely than others to consider their risk to be rather low (36.1% vs 21.2%; P < .001). In addition, women unable to appraise their level of risk were more likely to be at lower risk (mean risk at 0.0088 vs 0.0110; P = .02).
Table 1. Clinical and Sociodemographic Characteristics, Understanding of the Results of DS Combined Screening Test, and Attitudes Toward IT and NIPT of 2436 Pregnant Women at High Risk for Fetal DS.
| Characteristic | No (%) |
|---|---|
| Age, mean (SD), y | 36.3 (5.0) |
| Nuchal translucency measurement, mean (SD), multiple of the median | 0.6901 (0.5034) |
| DS risk: combined test results, mean (SD), multiple of the median | 0.0108 (0.0124) |
| No prior pregnancy | 604 (24.4) |
| Nulliparous | 799 (32.8) |
| Invasive testing in previous pregnancies | 306 (12.6) |
| Diagnosis of fetal chromosomal abnormalities in previous pregnancies | 103 (4.2) |
| Current smoker | 441 (18.1) |
| Time of inclusion with respect to first inclusion, mean (SD), d | 382.11 (182.433) |
| Educational level | |
| No education or primary education | 146 (6.0) |
| Lower secondary education | 449 (18.4) |
| Secondary education | 359 (14.7) |
| Upper secondary education | 435 (17.9) |
| Postsecondary and tertiary education | 1003 (41.2) |
| Missing | 44 (1.8) |
| Religion | |
| Very important | 289 (11.9) |
| Fairly important | 426 (17.5) |
| Not very important | 615 (25.2) |
| Not important at all | 1039 (42.6) |
| Missing | 67 (2.7) |
| Women’s understanding of combined test | |
| Rather low risk | 611 (25.1) |
| High risk | 1256 (51.6) |
| Very high risk | 347 (14.2) |
| Other: comments on screening and DS risk | 181 (7.4) |
| Missing | 41 (1.7) |
| Decision-making about biochemical screening | |
| Decided to carry it out before the option was proposed | 1030 (42.3) |
| Did not think about it before the option was proposed | 1000 (41.0) |
| Did not know about it before the option was proposed | 392 (16.1) |
| No opinion | 14 (0.6) |
| While awaiting the combined test results, anticipated decision about invasive testing? | |
| Yes | 726 (29.8) |
| No | 1680 (69.0) |
| No opinion | 30 (1.2) |
| Worst pregnancy outcome, in the women’s opinion | |
| Birth of a child with DS | 1371 (56.3) |
| Miscarriage due to invasive testing | 933 (38.3) |
| No opinion | 132 (5.4) |
| What is best? | |
| To take the risk of procedure-related fetal loss (occurring in approximately 1 woman in 100) and obtain certain information on all possible chromosomal abnormalities | 976 (40.1) |
| Not to take the risk of procedure-related fetal loss and get almost certain information (99% reliability) on DS only | 1388 (57.0) |
| No opinion | 72 (3.0) |
| Women’s preferences between IT and NIPT | |
| Neither IT nor NIPT | 29 (1.2) |
| NIPT | 1843 (75.7) |
| IT | 515 (21.1) |
| No opinion | 49 (2.7) |
| Visual analog scale score, mean (SD)a | 3.09 (3.25) |
| Decisional preferences after having been informed about the trial | |
| To decline both IT and NIPT | 25 (1.0) |
| To carry out NIPT if offered and to decline IT otherwise | 357 (14.7) |
| To carry out NIPT provided also carrying out IT | 1758 (72.2) |
| To carry out IT and to decline NIPT | 218 (8.9) |
| No opinion | 78 (3.2) |
| It is best to take the risk of procedure-related fetal loss rather than to be worried until the end of the pregnancy | |
| Strongly agree | 872 (35.8) |
| Rather agree | 1019 (41.8) |
| Rather disagree | 346 (14.2) |
| Strongly disagree | 182 (7.5) |
| No opinion | 17 (0.7) |
| Having carried out biochemical screening should lead women to undergo invasive testing if it is advised by their health care professional | |
| Strongly agree | 851 (34.9) |
| Rather agree | 986 (40.5) |
| Rather disagree | 372 (15.3) |
| Strongly disagree | 204 (8.4) |
| No opinion | 23 (0.9) |
| Invasive testing should be declined when termination of pregnancy is not an option in the case of DS | |
| Strongly agree | 713 (29.3) |
| Rather agree | 681 (28.0) |
| Rather disagree | 552 (22.7) |
| Strongly disagree | 466 (19.1) |
| No opinion | 24 (1.0) |
| Invasive testing should be carried out without considering the decisions that might be required following its results: everything in its own time | |
| Strongly agree | 607 (24.9) |
| Rather agree | 778 (31.9) |
| Rather disagree | 641 (26.3) |
| Strongly disagree | 389 (16.0) |
| No opinion | 21 (0.9) |
Abbreviations: DS, Down syndrome; IT, invasive testing; NIPT, noninvasive prenatal testing.
Visual analog scale from 0 to 10, with lower values indicating stronger preference for NIPT.
Attitudes Toward NIPT and IT
Using data relating to pregnant women’s attitudes (Table 1), the hierarchical cluster analysis yielded 4 different clusters. The variables characterizing each one of these clusters are presented in Table 2. The first cluster (10.3% [250 of 2436 respondents]) consisted of women who highly valued the possibility of getting all possible information on chromosomal abnormalities without any delay. These women reported more frequently than the others that they had anticipated the possibility of having to decide about IT in case of a high risk of DS (36.8% vs 28.8%; difference, 8.0%; 95% CI, 17.4%-14.6%; P = .006). Most of them considered the risk of IT-related fetal loss to be acceptable while providing access to all possible information on fetal chromosomal abnormalities (85.6% vs 34.9%; difference, 50.7%; 95% CI, 45.2%-55.2%; P < .001) and preventing further anxiety (52.0% vs 33.9%; difference, 18.1%; 95% CI, 11.4%-24.7%; P < .001). Women in this cluster expressed a clear-cut preference for IT (79.6% vs 14.5%; difference, 65.1%; 95% CI, 59.3%-70.1%; P < .001) and considered declining NIPT if offered (87.3% vs 0%; difference, 87.3%; 95% CI, 82.3%-91.0%; P < .001).
Table 2. Variables Contributing to Distinguishing Clusters of 2436 Pregnant Women at High Risk for Fetal DSa.
| Variable | Total, No. (%) | Cluster 1 (n = 250) | Cluster 2 (n = 485) | Cluster 3 (n = 1324) | Cluster 4 (n = 377) | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | P Value | No. (%) | P Value | No. (%) | P Value | No. (%) | P Value | ||
| Decided to carry out biochemical screening before it was proposed | 1030 (42.3) | 114 (45.6) | .16 | 174 (35.9) | .001 | 604 (45.6) | <.001 | 138 (36.6) | .008 |
| While awaiting the combined test results, anticipated the decision about invasive testing | 726 (29.8) | 92 (36.8) | .006 | 149 (30.7) | .33 | 384 (29.0) | .20 | 101 (26.8) | .08 |
| Decisional preferences | |||||||||
| To carry out IT and to decline NIPT | 218 (8.9) | 218 (87.3) | <.001 | 0 | <.001 | 0 | <.001 | 0 | <.001 |
| To carry out NIPT provided also carrying out IT | 1758 (72.2) | 0 | <.001 | 461 (95.1) | <.001 | 1297 (98.0) | <.001 | 0 | <.001 |
| To carry out NIPT and to decline IT | 357 (14.7) | 0 | <.001 | 10 (2.1) | <.001 | 0 | <.001 | 347 (92.0) | <.001 |
| The birth of a child with DS is a worse pregnancy outcome than IT-related miscarriage | 1371 (56.3) | 177 (70.8) | <.001 | 310 (63.9) | <.001 | 779 (58.8) | .003 | 105 (27.9) | <.001 |
| Strongly agreed that it is best to take the risk of IT-related fetal loss rather than to be worried until the end of the pregnancy | 872 (35.8) | 130 (52.0) | <.001 | 260 (53.6) | <.001 | 443 (33.5) | .004 | 39 (10.3) | <.001 |
| Strongly agreed that having carried out biochemical screening should lead women to undergo IT if advised | 851 (34.9) | 101 (40.2) | .04 | 283 (58.4) | <.001 | 406 (30.7) | <.001 | 61 (16.2) | <.001 |
| Strongly agreed that IT should be declined when termination of pregnancy is not an option in the case of DS | 713 (29.3) | 80 (32.0) | .19 | 130 (26.8) | .10 | 370 (27.9) | .07 | 133 (35.3) | .004 |
| Strongly agreed that IT should be carried out without considering the decisions that might be required following its results | 607 (24.9) | 65 (26.0) | .04 | 485 (100) | <.001 | 0 | <.001 | 57 (15.1) | <.001 |
| It is best to take the risk of IT-related fetal loss and get certain information on all possible chromosomal abnormalities | 976 (40.1) | 214 (85.6) | <.001 | 243 (50.1) | <.001 | 475 (35.9) | <.001 | 44 (11.7) | <.001 |
| Preference for IT over NIPTb | 515 (21.1) | 199 (79.6) | <.001 | 91 (18.8) | .08 | 204 (15.4) | <.001 | 21 (5.6) | <.001 |
| VAS score, mean (SD) | 3.09 (3.25) | 7.56 (2.81) | 3.15 (3.11) | 2.80 (2.81) | 1.09 (2.33) | ||||
| VAS scores ≥5 | 816 (33.5) | 223 (89.2) | <.001 | 184 (37.9) | .02 | 374 (28.2) | <.001 | 35 (9.3) | <.001 |
Abbreviations: DS, down syndrome; IT, invasive testing; NIPT, noninvasive prenatal testing; VAS, visual analog scale.
Cluster 1 was characterized by participants who wanted all possible information as soon as possible (250 women [10.3%]); cluster 2, participants who wanted all possibilities of getting information (485 women [19.9%]); cluster 3, participants who were primarily concerned with information on DS (1324 women [54.3%]); and cluster 4, participants characterized by aversion to risk of fetal loss (377 women [15.5%]).
The VAS scores are used as an illustrative variable.
The second cluster (19.91% [485 respondents]) included women who valued all possibilities of getting information on their pregnancy. They frequently stated, as in the previous cluster, that the birth of a baby with DS was a worse pregnancy outcome than IT-related fetal loss (63.9% vs 54.4%; difference, 9.5%; 95% CI, 4.5%-14.3%; P < .001) and that getting all possible information on chromosomal abnormalities was worth the risk of fetal loss (50.1% vs 37.6%; difference, 12.5%; 95% CI, 7.5%-17.6%; P < .001). While women in this cluster also deemed that having undergone DS screening should prompt women to carry out IT if offered (58.4% vs 29.1%; difference, 29.3%; 95% CI, 24.2%-34.1%; P < .001), they did not express clear-cut preference between IT and NIPT (18.8% vs 21.7%; difference, 2.9%; 95% CI, −1.3% to 6.8%; P = .08) and they accordingly viewed carrying out both NIPT and then IT as their preferred option (95.1% vs 66.5%; difference, 28.6%; 95% CI, 25.4%-31.3%; P < .001).
The third cluster (54.4% [1324 respondents]) included women who primarily valued getting information on fetal DS. Women in this cluster had decided more frequently than the others to undergo biochemical screening before it was even proposed (45.6% vs 38.3%; difference, 7.3%; 95% CI, 3.3%-11.3%; P < .001). Like in previous clusters, most women considered that the birth of a baby with DS was a worse pregnancy outcome than IT-related fetal loss (58.8% vs 53.2%; difference, 5.6%; 95% CI, 1.6%-9.6%; P = .003). However, all of them deemed that IT should not be undergone without considering the decisional implications (100% vs 45.4%; difference, 54.6%; 95% CI, 51.6%-57.5%; P < .001) and they also frequently stated that getting complete information on all possible chromosomal abnormalities was not worth the risk for the pregnancy (64.1% vs 54.9%; difference, 9.2%; 95% CI, 5.2%-13.1%; P < .001). While they expressed preference toward NIPT (84.6% vs 72.0%; difference, 12.6%; 95% CI, 9.2%-15.9%; P < .001), they did not reject the IT option at the time when they were offered to participate in the trial because nearly all considered carrying out IT following a negative NIPT (98.0% vs 41.5%; difference, 56.5%; 95% CI, 53.4%-59.5%; P < .001).
The fourth cluster (15.5% [377 respondents]) consisted of women whose attitudes appeared to be driven by aversion to the risk of IT-related fetal loss (72.1% vs 38.5%; difference, 33.6%; 95% CI, 28.3%-38.5%; P < .001). Accordingly, most of them would choose not to take any risk with the pregnancy and get information on DS only (88.3% vs 54.7%; difference, 33.6%; 95% CI, 28.3%-38.5%; P < .001). Women in this cluster expressed a clear-cut preference for NIPT (94.4% vs 76.0%; difference, 18.4%; 95% CI, 15.0%-21.2%; P < .001) and approximately one-third of them deemed that IT should be declined when termination of the pregnancy is not an option (35.3% vs 28.2%; difference, 7.1%; 95% CI, 1.9%-12.6%; P = .004).
Perceived values attached to IT and NIPT as rated with a VAS showed the highest scores for IT were found in cluster 1 (89.2% of VAS scores greater than 5 vs 27.1% in the other clusters; difference, 62.1%; 95% CI, 57.0%-66.0%; P < .001) while the lowest scores were found in cluster 4 (9.3% vs 37.9%; difference, 28.6%; 95% CI, 13.0%-19.5%; P < .001). Otherwise, women in cluster 2 had higher VAS scores than women in cluster 3, which was also consistent with more frequent ratings greater than 5 in cluster 2 (37.9% vs 28.2%; difference, 9.7%; 95% CI, 4.7%-14.8%; P = .02).
Factors Associated With Attitudes
The factors associated with women’s attitudes toward NIPT and IT are presented in Table 3. Women with higher nuchal translucency measurements by ultrasonography were more likely to be included in cluster 1 (adjusted odds ratio [aOR], 1.67; 95% CI, 1.27-2.20; P < .001), whereas cluster 2 was more likely to include women with lower educational levels (aOR, 0.54; 95% CI, 0.44-0.67; P < .001). Women in cluster 3 were characterized by higher educational levels (aOR, 1.44; 95% CI, 1.20-1.74; P < .001) and lower importance given to religion (aOR, 0.68; 95% CI, 0.57-0.82; P < .001). Lastly, older women (aOR, 1.03; 95% CI, 1.00-1.05; P = .03), those who described their own risk of DS as rather low (aOR, 1.34; 95% CI, 1.05-1.71; P = .02), and those with very or fairly strong religious beliefs (aOR, 1.62; 95% CI, 1.29-2.04; P < .001) were more likely to be included in cluster 4. Allocations to cluster 1 decreased slightly over time throughout the trial (aOR, 0.99; 95% CI, 0.99-0.99; P < .001), whereas allocations increased slightly over time in cluster 3 (aOR, 1.01; 95% CI, 1.00-1.01; P = .009).
Table 3. Factors Associated With Attitudes to NIPT and IT Among Women at High Risk for Fetal DSa.
| Factor | Cluster 1 (n = 250) | Cluster 2 (n = 485) | Cluster 3 (n = 1324) | Cluster 4 (n = 377) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. (%) | P Valueb | aOR (95% CI) | P Value | No. (%) | P Valueb | aOR (95% CI) | P Value | % or Mean (SD) | P Valueb | aOR (95% CI) | P Value | % Mean (SD) |
P Valueb | aOR (95% CI) | P Value | |
| Nuchal translucency measurement, mean (SD), multiple of the median | 0.8040 (0.4543) | <.001 | 1.67 (1.27-2.20) | <.001 | 0.6866 (0.4945) | .87 | 0.6798 (0.5101) | .27 | 0.6552 (0.5136) | .14 | ||||||
| Calculated risk from combined test | .06 | .98 | .84 | .06 | ||||||||||||
| ≥1 in 50 | 39 (15.6) | .02 | 55 (11.3) | .85 | 147 (11.1) | .90 | 29 (7.7) | .02 | ||||||||
| 1 in 100 to 1 in 50 [reference] | 41 (16.4) | 83 (17.1) | 233 (17.6) | 62 (16.5) | ||||||||||||
| <1 in 100 | 170 (68.0) | .98 | 347 (71.6) | .98 | 944 (71.3) | .56 | 286 (75.9) | .43 | ||||||||
| Women’s age, mean (SD), y | 35.7 (5.3) | .04 | 36.7 (5.0) | .07 | 36.1 (4.9) | .07 | 36.8 (5.1) | .03 | 1.03 (1.00-1.05) | .03 | ||||||
| IT in previous pregnancies | 30 (12.0) | .78 | 66 (13.6) | .44 | 167 (12.6) | .93 | 43 (11.4) | .46 | ||||||||
| Diagnosed fetal chromosomal abnormalities in previous pregnancies | 12 (4.8) | .64 | 24 (5.0) | .38 | 53 (4.0) | .55 | 14 (3.7) | .59 | ||||||||
| Previous pregnancy vs none | 61 (24.4) | .06 | 74 (15.3) | .005 | 0.74 (0.56-0.98) | .03 | 283 (21.4) | .04 | 66 (17.5) | .21 | ||||||
| Nulliparous vs multiparous | 82 (32.8) | .32 | 123 (25.4) | .01 | 411 (31.0) | .24 | 116 (30.8) | .74 | ||||||||
| >1 Fetal loss in previous pregnancies | 33 (13.2) | .04 | 0.69 (0.47-1.02) | .06 | 99 (20.4) | .11 | 225 (17.0) | .19 | 80 (21.2) | .07 | ||||||
| Women’s own understanding of their DS risk as rather low | 50 (20.0) | .05 | 138 (28.5) | .06 | 311 (23.5) | .048 | 112 (29.7) | .03 | 1.34 (1.05-1.71) | .02 | ||||||
| Education level at or above secondary school graduation | 197 (78.6) | .19 | 314 (64.7) | <.001 | 0.54 (0.44-0.67) | <.001 | 1039 (78.5) | <.001 | 1.44 (1.20-1.74) | <.001 | 281 (74.6) | .80 | ||||
| Religion very or fairly important | 78 (31.2) | .50 | 151 (31.1) | .34 | 341 (25.8) | <.001 | 0.68 (0.57-0.82) | <.001 | 145 (38.5) | <.001 | 1.62 (1.29-2.04) | <.001 | ||||
| Current smoker | 53 (21.2) | .18 | 86 (17.7) | .81 | 239 (18.1) | .94 | 63 (16.7) | .45 | ||||||||
| Time of inclusion, mean (SD), mo | 10.09 (5.86) | <.001 | 0.99 (0.99-0.99) | <.001 | 12.89 (5.91) | .18 | 12.84 (5.95) | .01 | 1.01 (1.00-1.01) | .009 | 12.80 (6.02) | .41 | ||||
Abbreviations: aOR, adjusted odds ratio; DS, down syndrome; IT, invasive testing; NIPT, noninvasive prenatal testing.
Cluster 1 was characterized by participants who wanted all possible information as soon as possible (250 women [10.3%]); cluster 2, participants who wanted all possibilities of getting information (485 women [19.9%]); cluster 3, participants who were primarily concerned with information on DS (1324 women [54.3%]); and cluster 4, participants characterized by aversion to risk of fetal loss (377 women [15.5%]).
P values from univariate logistic regressions.
Was Decision Making in Line With Attitudes?
Overall, pregnant women’s decisions were consistent with their attitudes (Table 4). Women who refused participation in the trial prior to randomization were primarily found to be included in cluster 1 (78.8% vs 11.3% distributed among the other clusters; P < .001). These women were mainly characterized with higher nuchal translucency measurements by ultrasonography (median at 0.80 vs 0.67; P = .003) and fewer experiences of fetal loss (13.2% of women in cluster 1 reporting 0 or 1 previous experience of fetal loss vs 9.9% in the other women; P = .001). As for refusal of randomized assignment to IT, the lowest rate was in cluster 1 (1.2%), while the highest was in cluster 4 (44.3%). In all, 43.2% of women in cluster 4, representing 6.7% of the surveyed women, declined to participate in the trial either before or after randomization. In addition, most women opting for NIPT after having declined IT were included in clusters 3 and 4 (60.4% and 22.6%, respectively, vs 17.0% for the other clusters; P < .001).
Table 4. Actual Decision-Making and Visual Analog Scale Values Attached to IT Depending on Clusters for 2436 Pregnant Women at High Risk for Fetal Down Syndromea.
| Decision | Total, No. (%) | Cluster 1 (n = 250) | Cluster 2 (n = 485) | Cluster 3 (n = 1324) | Cluster 4 (n = 377) | ||||
|---|---|---|---|---|---|---|---|---|---|
| No. (%) | P Value | No. (%) | P Value | No. (%) | P Value | No. (%) | P Value | ||
| Refused participation prior to randomization between IT and NIPT | 445 (18.3) | 197 (78.8) | <.001 | 52 (10.7) | <.001 | 146 (11.0) | <.001 | 50 (13.3) | .006 |
| Refused their randomized assignment to IT | 255 (10.5) | 3 (1.2) | <.001 | 34 (7.0) | .005 | 105 (7.9) | <.001 | 113 (30.0) | <.001 |
| Accepted their randomized assignment to: | |||||||||
| IT | 750 (30.8) | 26 (10.4) | <.001 | 176 (36.3) | .003 | 491 (37.1) | <.001 | 57 (15.1) | <.001 |
| NIPT | 979 (40.2) | 22 (8.8) | <.001 | 223 (46.0) | .004 | 579 (43.7) | <.001 | 155 (41.1) | .69 |
| Opted for NIPT after having declined ITb | 506 (20.8) | 5 (1.9) | .59 | 73 (15.1) | .67 | 799 (60.4) | <.001 | 85 (22.6) | <.001 |
Abbreviations: IT, invasive testing; NIPT, noninvasive prenatal testing.
Cluster 1 was characterized by participants who wanted all possible information as soon as possible (250 women [10.3%]); cluster 2, participants who wanted all possibilities of getting information (485 women [19.9%]); cluster 3, participants who were primarily concerned with information on DS (1324 women [54.3%]); and cluster 4, participants characterized by aversion to risk of fetal loss (377 women [15.5%]).
Calculations based on the 255 pregnant women who refused their randomized assignment to IT.
Discussion
The present study confirmed pregnant women’s preference toward NIPT18,19,20,21,22,23,24,25,26,27 and showed highly contrasted attitudes toward IT and NIPT in pregnant women at high risk of fetal DS by combined first-trimester screening. A clear-cut preference for IT (cluster 1) was associated with risk aversion to IT-related fetal loss being outweighed by aversion to ambiguous information on fetal chromosomal abnormalities other than DS, leading to lower VAS scores for NIPT. In contrast, clear-cut preference for NIPT (cluster 4) was expressed by women with strong aversion to IT-related risk of fetal loss, confirming previous findings18,19,24,25 and being consistent with highest VAS scores attached to NIPT. In between, attitudes in clusters 2 and 3 involved both risk aversion and ambiguity aversion to different extents.
In addition, pregnant women’s trade-offs between pregnancy risk taking and extent of information seeking were found to differ depending on DS risk levels. Women who considered their own risk of fetal DS following combined test results as being rather low were more likely to report strong aversion to IT-related risk (cluster 4). In contrast, those with higher nuchal translucency measurements were more likely to report strong aversion to ambiguity conveyed by NIPT results (cluster 1). While DS risk assessment is combining multiple parameters (age, nuchal translucency, and biochemical markers), a common behavioral bias, the base rate fallacy bias,28 could explain attitudes in cluster 1. Base rate fallacy bias occurs when focusing on specific information, ie, the ultrasonography component of DS risk, rather than on overall information on DS risk and making inferences about the outcome. As a result, ultrasonographic screening could shape high-risk women’s attitudes, just as age has been shown to shape attitudes toward IT among low-risk pregnant women.29 Otherwise, the present study mainly confirmed the role played by education and religious beliefs on attitudes.25,30
Relevance of risk aversion and ambiguity aversion in explaining attitudes was highlighted by high consistency of attitudes with decision-making. Women with clear-cut preference for IT (cluster 1) were also more likely to decline to participate in the clinical study, suggesting that these women acknowledged the uncertain component of the information provided by NIPT and expressed strong aversion to ambiguity generated by incomplete information from NIPT. Another main finding related to the fact that few women underwent IT despite negative NIPT results, although approximately 70% of women considered undergoing IT in addition to NIPT as their preferred option. While undergoing IT in addition to NIPT did not involve any monetary constraints, the possibility of base rate fallacy bias cannot be ruled out. Indeed, negative NIPT results could lead pregnant women to implicitly extrapolate on the other chromosomal abnormalities not targeted by NIPT. In view of the false reassurance possibly induced by negative NIPT results, further investigations should be conducted on the extent to which base rate fallacy bias truly affects pregnant women’s decisions. Otherwise, this study shows that the availability of NIPT may reduce the refusal rates for further testing,31 far from the commonly observed 20% rate of high-risk pregnant women’s refusal of IT when NIPT was not available.32,33,34 Lastly, this study also shows that approximately a third of pregnant women anticipated their decision in the case of high risk of DS21 and that older pregnant women attached higher value to NIPT than their younger counterparts.23
Limitations
Attitudes and behaviors were studied within the framework of a clinical trial, in which counseling is likely to have been homogeneous and consistent in informing pregnant women about their options.35 Informed decisions were therefore likely to have been facilitated, possibly beyond what would be seen in routine antenatal practice. Another limitation was that DS was the only chromosomal abnormality targeted by NIPT, although trade-offs between pregnancy risk taking and extent of information seeking are likely to stand unless NIPT targets all chromosomal abnormalities detectable using IT. Another limitation relates to the rapidly evolving field of molecular cytogenetics that has recently identified comparative genomic hybridization microarray to provide additional information to the standard karyotype following IT. Although complete information should include genomic hybridization microarray on trophoblast or amniotic fluid, this option was not considered in our study. A final limitation concerned the risk of miscarriage of 0.5% to 1.0% associated with IT that was included in the information provided. There is now strong evidence that this risk is likely to be overstated.14,36,37
Conclusions
The present study highlights the major role played by risk aversion and ambiguity aversion in shaping attitudes and decision making. Availability of NIPT imposes complex decisions and informed decision making that would require receiving extensive information on abnormalities targeted by both NIPT and IT. Genetic counseling goes beyond the trade-off between first-line combined screening and invasive procedure-related risk. While pregnant women have been shown to greatly differ in terms of extent of information seeking, tolerance for uncertainty, and pregnancy risk taking, counseling should involve listening to women’s preferences as to what they want to get out of prenatal testing.
eAppendix. Questionnaire
References
- 1.Alldred SK, Takwoingi Y, Guo B, et al. First trimester ultrasound tests alone or in combination with first trimester serum tests for Down’s syndrome screening. Cochrane Database Syst Rev. 2017;3:. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashoor G, Syngelaki A, Wagner M, Birdir C, Nicolaides KH. Chromosome-selective sequencing of maternal plasma cell-free DNA for first-trimester detection of trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):322.e1-. doi: 10.1016/j.ajog.2012.01.029 [DOI] [PubMed] [Google Scholar]
- 3.Palomaki GE, Deciu C, Kloza EM, et al. DNA sequencing of maternal plasma reliably identifies trisomy 18 and trisomy 13 as well as Down syndrome: an international collaborative study. Genet Med. 2012;14(3):296-305. doi: 10.1038/gim.2011.73 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sparks AB, Struble CA, Wang ET, Song K, Oliphant A. Noninvasive prenatal detection and selective analysis of cell-free DNA obtained from maternal blood: evaluation for trisomy 21 and trisomy 18. Am J Obstet Gynecol. 2012;206(4):319.e1-319.e9. doi: 10.1016/j.ajog.2012.01.030 [DOI] [PubMed] [Google Scholar]
- 5.Chiu RW, Akolekar R, Zheng YW, et al. Non-invasive prenatal assessment of trisomy 21 by multiplexed maternal plasma DNA sequencing: large scale validity study. BMJ. 2011;342:c7401. doi: 10.1136/bmj.c7401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrich M, Deciu C, Zwiefelhofer T, et al. Noninvasive detection of fetal trisomy 21 by sequencing of DNA in maternal blood: a study in a clinical setting. Am J Obstet Gynecol. 2011;204(3):205.e1-205.e11. doi: 10.1016/j.ajog.2010.12.060 [DOI] [PubMed] [Google Scholar]
- 7.Alberti A, Salomon LJ, Le Lorc’h M, et al. Non-invasive prenatal testing for trisomy 21 based on analysis of cell-free fetal DNA circulating in the maternal plasma. Prenat Diagn. 2015;35(5):471-476. doi: 10.1002/pd.4561 [DOI] [PubMed] [Google Scholar]
- 8.Gregg AR, Gross SJ, Best RG, et al. ACMG statement on noninvasive prenatal screening for fetal aneuploidy. Genet Med. 2013;15(5):395-398. doi: 10.1038/gim.2013.29 [DOI] [PubMed] [Google Scholar]
- 9.Kahneman D, Tversky A. Prospect theory: an analysis of decision under risk. Econometrica. 1979;47(2):263-292. doi: 10.2307/1914185 [DOI] [Google Scholar]
- 10.Allais M. Le comportement de l’homme rationnel devant le risque: critique des postulats et axiomes de l’Ecole americaine. Econometrica. 1953;21(4):503-546. doi: 10.2307/1907921 [DOI] [Google Scholar]
- 11.Ellsberg D. Risk, ambiguity, and the savage axioms. Q J Econ. 1961;75(4):643-669. doi: 10.2307/1884324 [DOI] [Google Scholar]
- 12.Han PK, Williams AE, Haskins A, et al. Individual differences in aversion to ambiguity regarding medical tests and treatments: association with cancer screening cognitions. Cancer Epidemiol Biomarkers Prev. 2014;23(12):2916-2923. doi: 10.1158/1055-9965.EPI-14-0872 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fox CR, Tversky A. Ambiguity aversion and comparative ignorance. Q J Econ. 1995;110(3):585-603. doi: 10.2307/2946693 [DOI] [Google Scholar]
- 14.Malan V, Bussières L, Winer N, et al. ; SAFE 21 Study Group . Effect of cell-free DNA screening vs direct invasive diagnosis on miscarriage rates in women with pregnancies at high risk of trisomy 21: a randomized clinical trial. JAMA. 2018;320(6):557-565. doi: 10.1001/jama.2018.9396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Milligan G. An examination of procedures for determining the number of clusters in a data set. Psychometrika. 1985;50:159-179. doi: 10.1007/BF02294245 [DOI] [Google Scholar]
- 16.Ward JH. Hierarchical grouping to optimize an objective function. J Am Stat Assoc. 1963;58:236-244. doi: 10.1080/01621459.1963.10500845 [DOI] [Google Scholar]
- 17.Anderberg MR. Cluster Analysis for Applications. New York, NY: Academic Press; 1973. [Google Scholar]
- 18.Hill M, Johnson JA, Langlois S, et al. Preferences for prenatal tests for Down syndrome: an international comparison of the views of pregnant women and health professionals. Eur J Hum Genet. 2016;24(7):968-975. doi: 10.1038/ejhg.2015.249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lewis C, Hill M, Silcock C, Daley R, Chitty LS. Non-invasive prenatal testing for trisomy 21: a cross-sectional survey of service users’ views and likely uptake. BJOG. 2014;121(5):582-594. doi: 10.1111/1471-0528.12579 [DOI] [PubMed] [Google Scholar]
- 20.van Schendel RV, Kleinveld JH, Dondorp WJ, et al. Attitudes of pregnant women and male partners towards non-invasive prenatal testing and widening the scope of prenatal screening. Eur J Hum Genet. 2014;22(12):1345-1350. doi: 10.1038/ejhg.2014.32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chan YM, Leung TY, Chan OK, Cheng YK, Sahota DS. Patient’s choice between a non-invasive prenatal test and invasive prenatal diagnosis based on test accuracy. Fetal Diagn Ther. 2014;35(3):193-198. doi: 10.1159/000356075 [DOI] [PubMed] [Google Scholar]
- 22.Lewis C, Silcock C, Chitty LS. Non-invasive prenatal testing for Down’s syndrome: pregnant women’s views and likely uptake. Public Health Genomics. 2013;16(5):223-232. doi: 10.1159/000353523 [DOI] [PubMed] [Google Scholar]
- 23.Verweij EJ, Oepkes D, de Vries M, van den Akker ME, van den Akker ES, de Boer MA. Non-invasive prenatal screening for trisomy 21: what women want and are willing to pay. Patient Educ Couns. 2013;93(3):641-645. doi: 10.1016/j.pec.2013.08.006 [DOI] [PubMed] [Google Scholar]
- 24.Hill M, Fisher J, Chitty LS, Morris S. Women’s and health professionals’ preferences for prenatal tests for Down syndrome: a discrete choice experiment to contrast noninvasive prenatal diagnosis with current invasive tests. Genet Med. 2012;14(11):905-913. doi: 10.1038/gim.2012.68 [DOI] [PubMed] [Google Scholar]
- 25.Tischler R, Hudgins L, Blumenfeld YJ, Greely HT, Ormond KE. Noninvasive prenatal diagnosis: pregnant women’s interest and expected uptake. Prenat Diagn. 2011;31(13):1292-1299. doi: 10.1002/pd.2888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Schendel RV, Page-Christiaens GC, Beulen L, et al. ; Dutch NIPT Consortium . Trial by Dutch laboratories for evaluation of non-invasive prenatal testing: part II—women’s perspectives. Prenat Diagn. 2016;36(12):1091-1098. doi: 10.1002/pd.4941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheng Y, Leung WC, Leung TY, et al. Women’s preference for non-invasive prenatal DNA testing versus chromosomal microarray after screening for Down syndrome: a prospective study. BJOG. 2018;125(4):451-459. doi: 10.1111/1471-0528.15022 [DOI] [PubMed] [Google Scholar]
- 28.Tversky A, Kahneman D. Evidential impact of base rates In: Daniel Kahneman PSAT, ed. Judgment under uncertainty: Heuristics and biases. New York, NY: Cambridge University Press; 1982:153-160. doi: 10.1017/CBO9780511809477.011 [DOI] [Google Scholar]
- 29.Grinshpun-Cohen J, Miron-Shatz T, Ries-Levavi L, Pras E. Factors that affect the decision to undergo amniocentesis in women with normal Down syndrome screening results: it is all about the age. Health Expect. 2015;18(6):2306-2317. doi: 10.1111/hex.12200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lewis C, Hill M, Chitty LS. A qualitative study looking at informed choice in the context of non-invasive prenatal testing for aneuploidy. Prenat Diagn. 2016;36(9):875-881. doi: 10.1002/pd.4879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chan YM, Leung WC, Chan WP, Leung TY, Cheng YK, Sahota DS. Women’s uptake of non-invasive DNA testing following a high-risk screening test for trisomy 21 within a publicly funded healthcare system: findings from a retrospective review. Prenat Diagn. 2015;35(4):342-347. doi: 10.1002/pd.4544 [DOI] [PubMed] [Google Scholar]
- 32.Spencer K. Second trimester prenatal screening for Down’s syndrome using alpha-fetoprotein and free beta hCG: a seven year review. Br J Obstet Gynaecol. 1999;106(12):1287-1293. doi: 10.1111/j.1471-0528.1999.tb08183.x [DOI] [PubMed] [Google Scholar]
- 33.Wald NJ, Kennard A, Hackshaw A, McGuire A. Antenatal screening for Down’s syndrome. J Med Screen. 1997;4(4):181-246. doi: 10.1177/096914139700400402 [DOI] [PubMed] [Google Scholar]
- 34.Crossley JA, Aitken DA, Berry E, Connor JM. Impact of a regional screening programme using maternal serum alpha fetoprotein (AFP) and human chorionic gonadotrophin (hCG) on the birth incidence of Down’s syndrome in the west of Scotland. J Med Screen. 1994;1(3):180-183. doi: 10.1177/096914139400100309 [DOI] [PubMed] [Google Scholar]
- 35.Bekker HL, Hewison J, Thornton JG. Applying decision analysis to facilitate informed decision making about prenatal diagnosis for Down syndrome: a randomised controlled trial. Prenat Diagn. 2004;24(4):265-275. doi: 10.1002/pd.851 [DOI] [PubMed] [Google Scholar]
- 36.Akolekar R, Beta J, Picciarelli G, Ogilvie C, D’Antonio F. Procedure-related risk of miscarriage following amniocentesis and chorionic villus sampling: a systematic review and meta-analysis. Ultrasound Obstet Gynecol. 2015;45(1):16-26. doi: 10.1002/uog.14636 [DOI] [PubMed] [Google Scholar]
- 37.Wulff CB, Gerds TA, Rode L, Ekelund CK, Petersen OB, Tabor A; Danish Fetal Medicine Study Group . Risk of fetal loss associated with invasive testing following combined first-trimester screening for Down syndrome: a national cohort of 147,987 singleton pregnancies. Ultrasound Obstet Gynecol. 2016;47(1):38-44. doi: 10.1002/uog.15820 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Questionnaire