This economic evaluation uses a large US claims database to assess the cost and utilization of targeted drug delivery and conventional medical management vs conventional medical management alone for treating cancer-related pain.
Key Points
Question
What are the cost and health care utilization for pain relief using fully implantable targeted drug delivery therapy with conventional medical management vs conventional medical management alone in patients with cancer?
Findings
In this economic evaluation of claims data on 536 patients from a large US payer database, use of targeted drug delivery and conventional medical management was associated with a significant overall cost savings of $63 498 in the 12 months after the index date and with significantly fewer inpatient visits, shorter inpatient length of stay, and fewer emergency department visits. In the short term, use of targeted drug delivery and conventional medical management was associated with significantly higher outpatient and lower inpatient costs.
Meaning
The findings suggest that use of targeted drug delivery and conventional medical management to treat cancer pain is associated with cost savings and should be considered in patients for whom oral opioids are inadequate or produce intolerable adverse effects.
Abstract
Importance
Targeted drug delivery (TDD) has potential for cost savings compared with conventional medical management (CMM). Despite positive clinical and economic evidence, TDD remains underused to treat cancer pain.
Objective
To assess the cost of TDD and CMM in treating cancer-related pain.
Design, Setting, and Participants
This retrospective economic evaluation using propensity score–matched analysis was conducted using MarketScan commercial claims data on beneficiaries receiving TDD and CMM or CMM only for cancer pain from January 1, 2009, to September 30, 2015. Participants were matched on age, sex, cancer type, comorbidity score, and pre-enrollment characteristics. Data analysis was performed from June 1 to September 30, 2017.
Main Outcomes and Measures
Total 2-, 6-, and 12-month costs, number of health care encounters, length of hospital stay, additional components of cost, and health care utilization.
Results
A total of 376 TDD and CMM patients (mean [SD] age, 51.88 [9.98] years; 216 [57.5%] female) and 4839 CMM only patients (mean [SD] age, 51.52 [11.16] years; 3005 [62.1%] female) were identified for study inclusion. After matching, 536 patients were included in the study: 268 patients in the TDD and CMM group and 268 in the CMM only group. Compared with CMM only, TDD and CMM was associated with mean total cost savings of $15 142 (95% CI, $3690 to $26 594; P = .01) at 2 months and $63 498 (95% CI, $4620 to $122 376; P = .03) at 12 months; cost savings at 6 months were not statistically different ($19 577; 95% CI, −$12 831 to $51 984; P = .24). The TDD and CMM group had fewer inpatient visits (2-month mean difference [MD], 1.0; 95% CI, 0.8-1.2; P < .001; 6-month MD, 1.3; 95% CI, 0.8-1.7; P < .001; 12-month MD, 2.3; 95% CI, 1.2-3.4; P < .001) and shorter hospital stays (2-month MD, 6.8 days; 95% CI, 5.0-8.7 days; P < .001; 6-month MD, 6.8 days; 95% CI, 3.1-10.5 days; P < .001; 12-month MD, 10.6 days; 95% CI, 2.9-18.3 days; P = .007). Use of CMM only was associated with greater opioid use at 12 months (MD, 3.2; 95% CI, 0.4-6.0; P = .03).
Conclusions and Relevance
Compared with CMM alone, TDD and CMM together were associated with significantly lower cost and health care utilization. The findings suggest that TDD is a cost-saving therapy that should be considered in patients with cancer for whom oral opioids are inadequate or produce intolerable adverse effects and should be expanded as health care systems transition to value-based models.
Introduction
In 2010, the National Cancer Institute estimated the yearly cost of cancer treatment in the United States at $125 billion, with a projected cost of $157 billion in 2020.1 The increase in projected costs reflects the aging US population and a 30% increase in cancer survivorship.2 To address this, the Centers for Medicare & Medicaid Services developed alternative oncology payment models to provide high-value care.3
Patients most frequently report pain, fatigue, and emotional distress as adverse effects of cancer.4 Pain is prevalent throughout the cancer life cycle and has been identified as a preventable reason for hospital admission.5 Pain was reported in 55.0% of patients undergoing active treatment, 39.3% of patients with cancer in remission, and 66.4% of patients with advanced, metastatic, or terminal disease.6 A previous study5 identified pain diagnoses as associated with 41.4% of emergency department (ED) visits by patients with cancer. Liberal systemic opioid use for cancer pain remains the standard of care despite increased health care utilization secondary to frequent adverse effects.7,8,9,10
Another treatment option is targeted drug delivery (TDD), which provides improved pain relief and reduced toxic effects at lower cost compared with systemic opioid therapy.11,12,13 Targeted drug delivery provides an alternate route of opioid administration, delivering a fraction of the systemic dose directly to the intrathecal space via an implanted infusion system. Randomized trial data showed that TDD provides better pain relief with fewer adverse effects compared with conventional medical management (CMM).12 The National Comprehensive Cancer Network recommends TDD as an option for patients who experience intolerable adverse effects or in whom systemic opioids are not effective.10 Most patients receiving TDD have previously been treated with CMM; however, not every patient treated with CMM is an appropriate TDD candidate. In addition, TDD does not replace all pain-related CMM but enables reduction or elimination of systemic opioids.14
A prior analysis13 of cost data from 2006 to 2010 compared TDD and CMM for cancer-related pain in 146 patients and found lower medical care utilization and total payments for patients who received TDD. Since that time, TDD administration has shifted from an inpatient to an outpatient setting. This shift may result in lower initial cost to implant a TDD system, which has the potential to increase long-term cost savings and warrants a new analysis of available cost data. In this study, we compared the cost and health care utilization of treating cancer-related pain with TDD and CMM vs CMM only using data from a large US claims database.
Methods
Data Source
This study used the Truven Health MarketScan Commercial Claims and Encounters Database from January 1, 2009, to September 30, 2015; data analysis was conducted from June 1 to September 30, 2017. This database captures deidentified, patient-level health data, including health care utilization, health care cost from a payer perspective, enrollment information, inpatient service, outpatient service, and outpatient prescriptions.15,16 Disease-related factors, such as cancer stage or pain scores, are not available in the data set and were therefore not included in the model used in this analysis. Patients were identified using Current Procedural Terminology (CPT) procedure codes and International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes available in the database. According to the US Department of Health and Human Services Office for Human Research Protections, institutional review board oversight was not necessary because the study did not involve interaction or intervention with individuals, and the database was deidentified in compliance with the Health Insurance Portability and Accountability Act.17 Therefore, no informed consent was required from the patients. The data include employer- and health plan–sourced administrative claims from more than 99 million individuals, including employees, spouses, and dependents covered by employer-sponsored private health care insurance.15,18 The data reflect actual treatment patterns and costs by linking paid claims and encounter data to detailed patient information across sites and types of practitioners nationwide.15 The study followed the Consolidated Health Economic Evaluation Reporting Standards (CHEERS) reporting guideline.
Study Population
As mentioned earlier, TDD is not a first-line treatment option. Patients identified in claims data as receiving TDD were considered to have severe uncontrolled pain, which is a payer coverage condition for this treatment. The selection criteria for the CMM group included codes for the diagnosis or treatment of uncontrolled pain or codes associated with opioid toxicity in an attempt to identify patients with a similar level of pain. Patients in the TDD and CMM group and the CMM only group were mutually exclusive.
Patients in the TDD and CMM group were included if (1) they had an inpatient or outpatient claim with the presence of a TDD system implantation (CPT code 62362) between January 1, 2009, and September 30, 2015 (the first observed TDD pump implant service date or replacement procedure in this period was the index date) and (2) a cancer diagnosis code was present (ICD-9-CM codes 140.xx-209.xx, 230.xx-234.xx, or 235.xx-239.xx) on a claim within 3 months before or on the index date. Patients receiving TDD were excluded if they had (1) a history of TDD, including pump programming, analysis, refill, or removal codes (CPT codes 62367, 62368, 62365, 62369, 62370, 95990, or 95991) occurring before the index date or (2) at least 1 diagnosis code of spasticity within 3 months before or on the index date. This exclusion was made based on the assumption that patients received TDD therapy for spasticity.
Patients receiving CMM were included if (1) they had an inpatient hospital claim, including cancer diagnosis codes, in any position on the claim (ICD-9-CM codes 140.xx-209.xx, 230.xx-234.xx, or 235.xx-239.xx) between January 1, 2009, and September 30, 2015 (the inpatient visit admission date was the index date); (2) the index inpatient hospital visit included at least 2 additional diagnosis codes for symptoms associated with uncontrolled cancer pain, including nausea and/or vomiting (ICD-9-CM codes 787.01-787.03), anorexia (ICD-9-CM code 783.0), cachexia (ICD-9-CM code 799.4), somnolence (ICD-9-CM code 780.09), constipation (ICD-9-CM code 564.0), fecal impaction (ICD-9-CM code 560.32), bowel obstruction (ICD-9-CM code 560.9), or decreased mental status (ICD-9-CM code 780.97); and (3) they had at least 1 opioid prescription filled in the 6 months before or on the index date. Patients receiving CMM were excluded if they had any evidence of TDD during the analysis period (CPT codes 62362, 62367, 62368, 62365, 62369, 62370, 95990, 95991, 62350, 62351, or 62355). All patients had continuous health care plan enrollment with drug coverage for a minimum of 6 months before and 2 months after the index date.
Study Design
A matched retrospective cohort study was conducted to analyze cost from the payer perspective. The baseline period was defined as the 6-month period before but not including the index date.
The follow-up periods were defined as 2, 6, and 12 months after and including the index date. These periods were selected to mirror the time points studied in the initial analysis performed with 2006 to 2010 cost data and another previous cost analysis.13 The health care utilization and payments for the matched pairs were compared for patients who had continuous health plan enrollment at each time point. Total insurer cumulative costs associated with all-cause health care utilization were calculated at 2, 6, and 12 months. All paid insurer costs were included regardless of associated health care utilization itemization. Inpatient hospital, outpatient hospital, ED, office, home, and other service visits were recorded. Length of stay was calculated. Number of prescriptions filled for select medications associated with pain relief or opioid-related complications was also reported.
A series of variables were measured during the baseline period for consideration in the matching process. Covariates included in the final model (Table 1) were chosen to maximize sample size while accounting for imbalances in patient characteristics. This approach allowed for better assessment of the treatment effect between TDD and CMM and CMM only and further controlled for pain severity, given the lack of pain scores in claims data. Matching characteristics were selected to best identify patients with similar demographics, cancer type, and treatment patterns for cancer and pain before the index date. Baseline variables included demographics, total payment, cancer type (eAppendix 1 in the Supplement), Charlson Comorbidity Index (eTable in the Supplement), physician specialties, chemotherapy and radiotherapy (eAppendix 2 in the Supplement), health care utilization, prescription drug use, and tumor treatment (eAppendix 3 in the Supplement).
Table 1. Patient Characteristics During Baseline Perioda.
| Characteristic | Before Propensity Score Matching | After Propensity Score Matching | ||||
|---|---|---|---|---|---|---|
| TDD and CMM Group (n = 376) | CMM Only Group (n = 4839) | P Value | TDD and CMM Group (n = 268) | CMM Only Group (n = 268) | P Value | |
| Age, mean (SD), y | 51.88 (9.98) | 51.52 (11.16) | .50 | 51.91 (10.20) | 52.27 (11.19) | .70 |
| Sex | ||||||
| Male | 160 (42.6) | 1834 (37.9) | .07 | 115 (42.9) | 116 (43.3) | .93 |
| Female | 216 (57.5) | 3005 (62.1) | 153 (57.1) | 152 (56.7) | ||
| Region | ||||||
| Northeast | 40 (10.6) | 605 (12.5) | <.001 | 30 (11.2) | 25 (9.3) | .90 |
| North Central | 132 (35.1) | 1248 (25.8) | 87 (32.5) | 88 (32.8) | ||
| South | 112 (29.8) | 2100 (43.4) | 83 (31.0) | 79 (29.5) | ||
| West | 90 (23.9) | 852 (17.6) | 67 (25.0) | 75 (28.0) | ||
| Unknown | 2 (0.5) | 34 (0.7) | 1 (0.4) | 1 (0.4) | ||
| Charlson Comorbidity Index | ||||||
| 0-2 | 88 (23.4) | 2105 (43.5) | <.001 | 75 (28.0) | 88 (32.8) | .66 |
| 3-7 | 41 (10.9) | 736 (15.2) | 35 (13.1) | 35 (13.1) | ||
| 8 | 156 (41.5) | 1316 (27.2) | 106 (39.6) | 97 (36.2) | ||
| >8 | 91 (24.2) | 682 (14.1) | 52 (19.4) | 48 (17.9) | ||
| Index year | ||||||
| 2009 | 28 (7.5) | 431 (8.9) | <.001 | 21 (7.8) | 23 (8.6) | .25 |
| 2010 | 59 (15.7) | 779 (16.1) | 42 (15.7) | 41 (15.3) | ||
| 2011 | 80 (21.3) | 858 (17.7) | 57 (21.3) | 45 (16.8) | ||
| 2012 | 84 (22.3) | 871 (18.0) | 60 (22.4) | 59 (22.0) | ||
| 2013 | 65 (17.3) | 728 (15.0) | 44 (16.4) | 40 (14.9) | ||
| 2014 | 54 (14.4) | 790 (16.3) | 39 (14.6) | 44 (16.4) | ||
| 2015 | 6 (1.6) | 382 (7.9) | 5 (1.9) | 16 (6.0) | ||
| No. of inpatient hospital visits, mean (SD) | 1.30 (1.55) | 0.28 (0.73) | <.001 | 0.93 (1.21) | 0.86 (2.00) | .66 |
| Time in hospital, mean (SD), d | 9.84 (15.60) | 0.81 (4.04) | <.001 | 5.80 (9.81) | 4.90 (13.22) | .37 |
| No. of emergency department visits, mean (SD) | 1.23 (2.27) | 0.90 (1.88) | .007 | 1.10 (2.42) | 0.90 (2.18) | .32 |
| No. of outpatient visits, mean (SD) | 14.81 (12.62) | 11.08 (11.43) | <.001 | 13.46 (12.16) | 11.48 (11.75) | .06 |
| Total payment, $ | 110 835 | 52 938 | <.001 | 86 008 | 75 375 | .17 |
| Chemotherapy | 153 (40.7) | 2057 (42.5) | .50 | 114 (38.4) | 102 (38.1) | .93 |
| Radiotherapy | 117 (31.1) | 1065 (22.0) | <.001 | 66 (24.6) | 57 (21.3) | .36 |
| Tumor treatmentsb | 33 (8.8) | 455 (9.4) | .71 | 18 (6.7) | 21 (7.8) | .62 |
| Biopsy | 136 (36.2) | 2642 (54.6) | <.001 | 97 (36.2) | 107 (39.9) | .37 |
| Oncologist visits | 176 (46.8) | 1771 (36.6) | <.001 | 117 (43.7) | 111 (41.4) | .60 |
| Pain specialist visits | 132 (35.1) | 121 (2.5) | <.001 | 62 (23.1) | 70 (26.1) | .42 |
| Certain drug usec | 258 (68.6) | 3189 (65.9) | .28 | 171 (63.8) | 169 (63.1) | .86 |
| Anticonvulsant use | 151 (40.2) | 653 (13.5) | <.001 | 97 (36.2) | 104 (38.8) | .53 |
| Antidepressant use | 200 (53.2) | 1452 (30.0) | <.001 | 139 (51.9) | 145 (54.1) | .60 |
| Anxiolytic drug use | 230 (61.2) | 2342 (48.4) | <.001 | 158 (59.0) | 155 (57.8) | .79 |
| Corticosteroid use | 156 (41.5) | 1834 (37.9) | .17 | 109 (40.7) | 92 (34.3) | .13 |
| Opioid or tramadol use | 354 (94.2) | 4815 (99.5) | <.001 | 253 (94.4) | 251 (93.7) | .72 |
| Hypertension drugs | 140 (37.2) | 1412 (29.2) | .001 | 97 (36.2) | 97 (36.2) | 1.0 |
| Diabetes drugs | 53 (14.1) | 571 (11.8) | .18 | 39 (14.6) | 47 (17.5) | .35 |
| Psychostimulants | 22 (5.9) | 97 (2.0) | <.001 | 15 (5.6) | 13 (4.9) | .70 |
| Metastatic disease | 239 (63.6) | 1907 (39.4) | <.001 | 151 (56.3) | 139 (51.9) | .30 |
| Multiple cancer diagnostic codes (not multiple primary cancers) | 274 (72.9) | 2797 (57.8) | <.001 | 177 (66.0) | 160 (59.7) | .13 |
| Cancer | ||||||
| Oral | 15 (4.0) | 368 (7.6) | .01 | 11 (4.1) | 8 (3.0) | .48 |
| Skin | 45 (12.0) | 373 (7.7) | .003 | 30 (11.2) | 27 (10.1) | .67 |
| Bone or bony | 168 (44.7) | 866 (17.9) | <.001 | 99 (37.0) | 89 (33.2) | .37 |
| Colorectal | 60 (16.0) | 498 (10.3) | <.001 | 37 (13.8) | 31 (11.6) | .44 |
| Pancreatic | 41 (10.9) | 276 (5.7) | <.001 | 27 (10.1) | 28 (10.5) | .89 |
| Digestive system | 168 (44.7) | 1403 (29.0) | <.001 | 105 (39.2) | 99 (37.0) | .59 |
Abbreviations: CMM, conventional medical management; TDD, targeted drug delivery.
Data are presented as number (percentage) of patients unless otherwise indicated.
Tumor treatment indicates whether patients have evidence of tumor ablation, excision, resection, or destruction during the baseline period, indicating active tumor treatment.
The patient was receiving prescription medication that is commonly used to address the adverse effects of long-term opioid use. For match purposes, these were combined into 1 variable (appetite enhancer, antiemetic, and laxative use).
Statistical Analysis
Descriptive analyses were performed to compare costs between TDD and CMM and CMM only during the baseline and follow-up periods. Patient demographics, comorbidities, clinical characteristics, health care utilization, payment, and prescription drug use were examined using the t test, χ2 test, or Fisher exact test. The t test was selected for data analysis because cost analysis is focused on assessing mean costs rather than medians; this approach for analyzing large public health data sets, even in cases of nonnormally distributed data, is supported in the published literature.19,20,21,22
Propensity score matching balanced the baseline characteristics between the 2 groups for patients with 2 months or more of postindex follow-up. A logistic regression model was used to estimate propensity scores for each patient; 32 baseline characteristic variables were included in the model. Matching on a large number of characteristics resulted in many patients being excluded from the analysis but ensured that comparisons made between the groups were appropriate. Variables were selected to best match patients receiving TDD and CMM and those receiving CMM only for similar treatments and health care utilization for cancer and pain care in the baseline period. Characteristics associated with cost, health care utilization, or pain treatment were selected based on our clinical experience. A sensitivity analysis was performed with a 20-characteristic model. This model resulted in unbalanced patient characteristics at some time points; according to the study protocol, the matching method used resulted in balanced characteristics at all periods. Patients receiving TDD and CMM and patients receiving CMM only were matched based on their propensity scores using the caliper criteria. A 1:1 propensity score matching without replacement algorithm was used. The t test was used to compare matched pairs for cost and health care utilization.
Patient attrition was expected given the cancer diagnosis and the nature of the data set; patient enrollment in the data set may be affected by insurance changes, employment changes, or death. As a result of patient attrition, baseline characteristics of the remaining postmatch study population were retested by group for patients who also had 6 and 12 months of follow-up data. No statistically significant differences were found between the 2 groups at any point; follow-up comparisons were appropriate.
The mean health services payments and utilization for the matched pairs were calculated and compared at 2, 6, and 12 months. All payer expenditures were adjusted to 2015 US dollars using the Medical Care Consumer Price Index.23 These cost estimates are inclusive of the cost of TDD implant on the index date.
All statistical tests used a 2-sided significance level of P < .05. All analyses were performed using SAS statistical software, version 9.2 (SAS Institute Inc).
Results
Patient Population
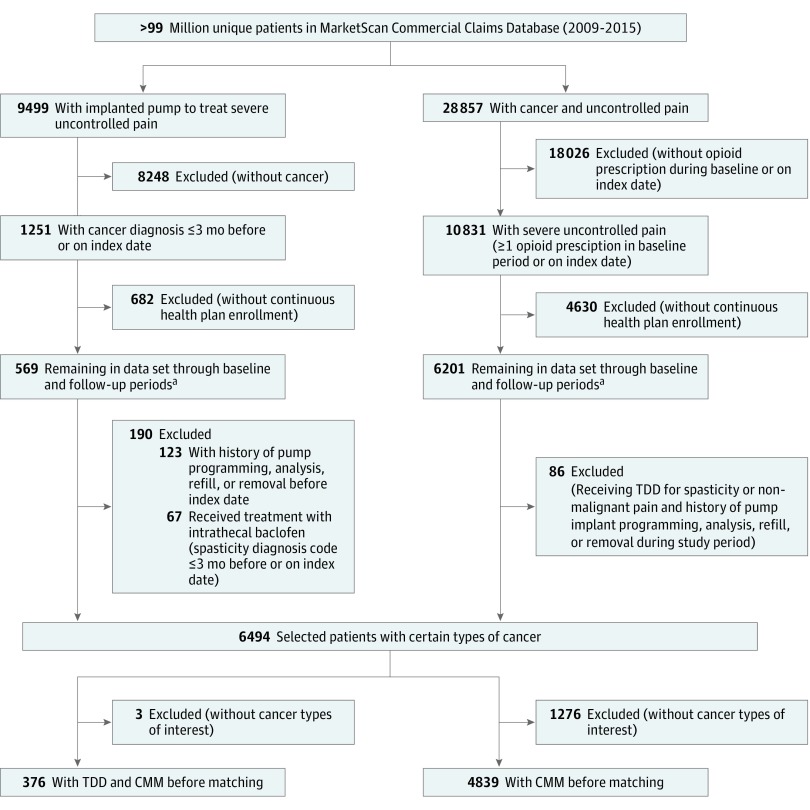
A total of 376 TDD and CMM patients (mean [SD] age, 51.88 [9.98] years; 216 [57.5%] female) and 4839 CMM only patients (mean [SD] age, 51.52 [11.16] years; 3005 [62.1%] female) were identified for study inclusion. The patient selection strategy is shown in Figure 1. A TDD system was implanted in 1251 patients with a cancer diagnosis within 3 months before or on their index date between January 1, 2009, and September 30, 2015. Of these, 376 patients met the inclusion criteria for the TDD and CMM population before matching (Table 1).
Figure 1. Patient Selection Strategy.
Patients in the targeted drug delivery (TDD) and conventional medical management (CMM) and CMM only groups before matching were selected according to the criteria described in the Study Population subsection of the Methods section.
aAt least 6 months continuous health plan enrollment before the index date and at least 2 months after the index date with prescription drug coverage.
A total of 710 637 patients were hospitalized with a cancer diagnosis between January 1, 2009, and September 30, 2015. A total of 10 831 patients (1.5%) had at least 2 additional diagnosis codes associated with uncontrolled pain on the index date and 1 or more opioid prescriptions in the baseline period. A total of 4839 patients met all inclusion criteria for the CMM population before matching (Table 1).
Prematch and Postmatch Baseline Characteristics and Study Population
A total of 5215 patients met the inclusion criteria before matching (376 in the TDD and CMM group and 4839 in the CMM group); baseline characteristics were not balanced (Table 1). Compared with the unmatched CMM population, the TDD and CMM population had statistically higher health care utilization and cost during the baseline period. After matching, 536 patients were identified (268 in the TDD and CMM group and 268 in the CMM only group); baseline characteristics were statistically similar.
During our study, 268 matched pairs were identified at the 2-month follow-up period. At 6 months, 151 patients receiving TDD and CMM and 162 receiving CMM only remained. At 12 months, 90 patients were receiving TDD and CMM and 98 were receiving CMM only.
Postmatch Follow-up Outcomes
Costs
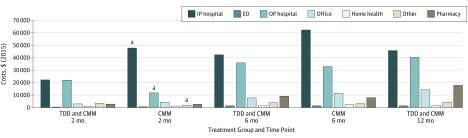
The TDD and CMM group had lower total costs than the CMM only group at 2 and 12 months. The mean cost difference at 2 months was $15 142 (95% CI, $3690-$26 594; P = .01), with a mean difference (MD) of $63 498 (95% CI, $4620-$122 376; P = .03) at 12 months. The cost difference at 6 months ($19 577; 95% CI, −$12 831 to $51 984; P = .24) was not statistically different. Compared with the CMM only group, the TDD and CMM group had significantly lower inpatient hospital costs (2-month MD, $25 479; 95% CI, $15 041 to $35 917; P < .001; 6-month MD, $19 820; 95% CI, −$8912 to $48 552; P = .18; 12-month MD, $49 104; 95% CI, −$1322 to $99 530; P = .06) (Table 2). Conversely, the patients receiving TDD and CMM had significantly higher outpatient hospital costs (2-month MD, $10 130; 95% CI, $6175-$14 086; P < .001) and other medical costs (2-month MD, $1735; 95% CI, $394-$3076; P = .01) than patients receiving CMM only at 2 months, although these costs were not significantly different subsequently. Office, home, ED, and outpatient pharmacy costs were not statistically different at any time point. Most all-cause costs occurred in the inpatient and outpatient hospital settings for both groups (Figure 2).
Table 2. Payments by Treatment Group During 12 Monthsa .
| Payment Type and Month | Payment, $ (2015) | P Value | ||||
|---|---|---|---|---|---|---|
| TDD and CMM Group | CMM Only Group, Median (IQR) | Mean Difference (95% CI) | ||||
| Mean (SD) | Median (IQR) | Mean (SD) | ||||
| Inpatient hospital | ||||||
| 2 | 22 268 (51 667) | 3127 (20 638) | 47 747 (47 747) | 22 801 (41 828) | 25 479 (15 041 to 35 917) | <.001 |
| 6 | 42 436 (150 614) | 9899 (32 364) | 62 256 (100 759) | 33 176 (64 719) | 19 820 (−8912 to 48 552) | .18 |
| 12 | 45 741 (173 371) | 10 612 (36 160) | 94 845 (176 626) | 41 786 (88 586) | 49 104 (−1322 to 99 530) | .06 |
| Outpatient hospital | ||||||
| 2 | 22 073 (25 538) | 13 109 (31 449) | 11 943 (20 841) | 3841 (11 620) | 10 130 (6175 to 14 086) | <.001 |
| 6 | 35 978 (42 157) | 19 359 (39 798) | 33 005 (54 200) | 10 989 (30 329) | 2974 (−7788 to 13 745) | .59 |
| 12 | 40 417 (41 149) | 29 463 (36 545) | 48 596 (79 724) | 19 786 (35 796) | 8180 (−9896 to 26 256) | .37 |
| Office | ||||||
| 2 | 3031 (6444) | 880 (2085) | 4294 (9216) | 669 (3746) | 1263 (−86 to 2613) | .07 |
| 6 | 7840 (14 336) | 2889 (5799) | 11 490 (22 562) | 2545 (9445) | 3650 (−528 to 7828) | .09 |
| 12 | 14 319 (28 494) | 5679 (9418) | 21 098 (36 651) | 5498 (12 370) | 6780 (−2627 to 16 187) | .16 |
| Home | ||||||
| 2 | 1 041(1041) | 0 (531) | 1302 (1302) | 0 (700) | 261 (−691 to 1213) | .59 |
| 6 | 1450 (2993) | 0 (1577) | 2446 (8738) | 0 (1333) | 996 (−441 to 2432) | .17 |
| 12 | 1836 (1836) | 183 (1808) | 3864 (3864) | 306 (2188) | 2028 (−644 to 4699) | .14 |
| Emergency department | ||||||
| 2 | 470 (1909) | 0 (167) | 678 (1835) | 0 (597) | 208 (−110 to 525) | .20 |
| 6 | 1414 (6906) | 0 (735) | 1442 (3407) | 250 (1441) | 28 (−1199 to 1255) | .96 |
| 12 | 1391 (2898) | 0 (967) | 2189 (6383) | 311 (1441)) | 798 (−613 to 2209) | .27 |
| Outpatient pharmacy | ||||||
| 2 | 2926 (4671) | 970 (2828) | 2723 (4682) | 989 (2587) | 204 (−590 to 998) | .61 |
| 6 | 9278 (14 445) | 3969 (8594) | 8106 (13 390) | 3053 (6928) | 1172 (−1924 to 4267) | .46 |
| 12 | 18 039 (29 334) | 7563 (15 913) | 13 333 (21 472) | 6654 (12 176) | 4706 (−2752 to 12 164) | .21 |
| Other medical costs | ||||||
| 2 | 3544 (3544) | 0 (1121) | 1809 (1809) | 36 (1049) | 1735 (394 to 3076) | .01 |
| 6 | 3982 (9306) | 213 (2136) | 3210 (9547) | 124 (1990) | 772 (−1328 to 2871) | .47 |
| 12 | 4469 (8218) | 851 (2959) | 5784 (20 000) | 506 (3098) | 1315 (−3034 to 5664) | .55 |
| Total medical and pharmacy costs | ||||||
| 2 | 55 353 (58 610) | 39 097 (45 309) | 70 495 (75 307) | 48 757 (61 356) | 15 142 (3690 to 26 594) | .01 |
| 6 | 102 377 (164 124) | 65 876 (94 526) | 121 954 (122 492) | 93 226 (117 399) | 19 577 (−12 831 to 51 984) | .24 |
| 12 | 126 211 (187 581) | 80 491 (122 852) | 189 709 (218 735) | 136 620 (158 267) | 63 498 (4620 to 122 376) | .03 |
Abbreviations: CMM, conventional medical management; IQR, interquartile range; TDD, targeted drug delivery.
The TDD sample sizes were 268 at 2 months, 151 at 6 months, and 90 at 12 months. The CMM sample sizes were 268 at 2 months, 162 at 6 months, and 98 at 12 months.
Figure 2. All-Cause Costs for the Targeted Drug Delivery (TDD) and Conventional Medical Management (CMM) Group and the CMM Only Group.
ED indicates emergency department; IP, inpatient; and OP, outpatient.
aStatistically significant differences for TDD and CMM compared with CMM only.
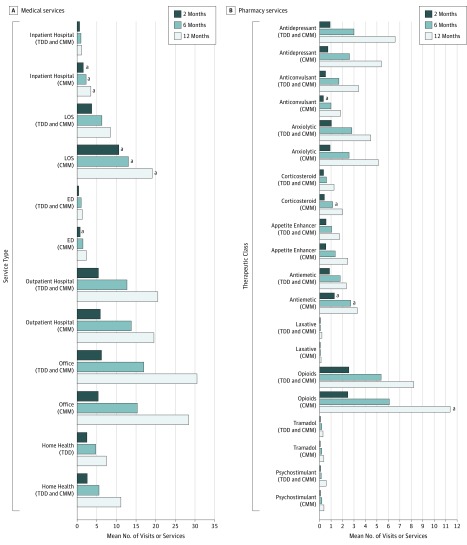
Medical Service Utilization
Patients receiving TDD and CMM had a significantly lower mean number of inpatient hospital visits (2-month MD, 1.0; 95% CI, 0.8-1.2; P < .001; 6-month MD, 1.3; 95% CI, 0.8-1.7; P < .001; 12-month MD, 2.3; 95% CI, 1.2-3.4; P < .001), shorter length of stay (2-month MD, 6.8 days; 95% CI, 5.0-8.7 days; P < .001; 6-month MD, 6.8 days; 95% CI, 3.1-10.5 days; P < .001; 12-month MD, 10.6 days; 95% CI, 2.9-18.3 days; P = .007), and fewer ED visits (2-month MD, 0.3; 95% CI, 0.2-0.5; P < .001) compared with those receiving CMM only (Figure 3A).
Figure 3. Medical Service and Pharmacy Utilization for the Targeted Drug Delivery (TDD) and Conventional Medical Management (CMM) Group and the CMM Only Group.
ED indicates emergency department; LOS, length of stay.
aStatistically significant differences for TDD and CMM compared with CMM only.
Pharmacy Utilization
The TDD and CMM group had a significantly lower mean number of corticosteroid (6-month MD, 0.5, 95% CI, 0.1-0.9; P = .006), antiemetic (2-month MD, 0.4; 95% CI, 0.1-0.7; P = .003; 6-month MD, 0.9; 95% CI, 0.1-1.7; P = .02), and opioid (12-month MD, 3.2; 95% CI, 0.4-6.0; P = .03) prescriptions compared with the CMM only group (Figure 3B). Conversely, the TDD and CMM group had a statistically higher mean number of anticonvulsant prescriptions (2-month MD, 0.2; 95% CI, 0.04-0.4; P = .02).
Discussion
Health care utilization and costs in the MarketScan database from 2009 to 2015 were analyzed for 536 patients with cancer-related pain. The TDD and CMM group had significant cost savings at 2 and 12 months and significantly lower total health care utilization than the CMM group at 2, 6, and 12 months. Important shifts in cancer care have occurred since 2006, when an earlier pilot study13 found lower utilization and costs for patients receiving TDD and CMM compared with patients receiving CMM only. Of note, the volume of inpatient services decreased, whereas the volume of lower-acuity services increased.24,25 Decreased inpatient hospitalizations for both groups may reflect overall changes in health care utilization since 2006 but still favored TDD and CMM over CMM only.
This matched retrospective analysis of a large payer database found that use of TDD and CMM was associated with a mean cost savings of $63 498 (P = .03) at 12 months. The primary cost drivers for both groups were hospital inpatient and outpatient categories.
At 2 months, TDD and CMM was already associated with an overall mean cost savings ($15 142, P = .01), with significantly lower inpatient hospital costs (mean cost difference, $25 479; 95% CI, $15 041-$35 917; P < .001) compared with CMM only (Table 2). Even with a significant total cost savings for TDD and CMM at 2 months, outpatient cost was significantly greater for TDD and CMM, suggesting that TDD implants were more likely administered in an outpatient service on the index date; no significant cost difference was found for hospital outpatient services at 6 or 12 months.
A previous study26 found that high-cost end-of-life cancer expenditures are primarily associated with emergency and inpatient care. In 2010, the United States had the highest incidence of intensive care unit admissions and hospital expenditures for patients with cancer older than 65 years who died of cancer across 7 developed countries.27 In our study, TDD and CMM had significantly lower utilization, with fewer inpatient hospital visits and shorter hospital stays at 2, 6, and 12 months. The number of visits to oncology and pain physicians, as well as the number of visits performed in the hospital outpatient or home health setting, were not significantly different between the matched groups at any period after the index date.
Cancer pain has been associated with high prescriptive opioid and adjuvant medication use.28 This study assessed pharmaceutical use by drug class and found that patients receiving TDD and CMM were prescribed fewer medications typically used to treat pain and opioid-induced complications. Data analysis and knowledge of physician prescribing patterns allowed us to assume that anticonvulsant use was higher at 2 months in the TDD and CMM group because of earlier introduction by pain management physicians. Corticosteroid use was higher in the CMM group at 6 months, possibly reflecting prescribing by oncology and palliative medicine physicians to treat pain and nausea and increase appetite. Opioid use was greater for CMM at 12 months, suggesting that TDD is associated with decreased systemic opioid use in surviving patients. Antidepressant and anxiolytic use increased in both groups over time, likely in association with worsening pain or emotional distress over diminished function, disease progression, and poor prognosis.
Smith et al12 found that patients receiving TDD and CMM had fewer medication-induced adverse effects than patients receiving CMM only. Rapid titration and low medication tolerance in the CMM group may result in adverse effects, which may require increased ED or hospital visits and frequent or long inpatient stays to control pain.
Cancer treatment improvements in the past 2 decades have been associated with increased survivorship, further compounding health care costs. In 2020, there will be an estimated 18 million cancer survivors.29 Opioids have many long-term health risks.9 Continued use of opioids is associated with increased health care cost and utilization. A previous study30 found that the opioid prescription rate among cancer survivors at least 5 years after diagnosis was 1.22 times higher than for matched patients without cancer. Worsening disability, loss of independence, or diminished intellectual and mental processing are associated with long-term systemic opioid therapy.9 Targeted drug delivery provides an alternative option for pain control in cancer survivors.
This study presents a direct medical cost assessment from the payer perspective. In addition to direct patient care costs, additional costs associated with subsequent informal care and productivity are relevant to considering the total cost of any therapy.31 Caregivers assume substantial personal, economic, and psychological burdens and are critically important partners for patients with cancer and practitioners. Access to and expense of clinical treatment, along with care beyond the clinical environment, prove to be substantial whether a patient lives independently or with their primary caregiver. Costs to consider include home care or caregiver support, lost wages, travel cost, and dependent care arrangements for other family members.32
The decision criteria for managing cancer pain are complicated because treatment planning for the best medical outcome includes assessment of patient and caregiver capacity to logistically, psychologically, and economically facilitate ongoing care access.33 Targeted drug delivery should be considered as an option to alleviate caregiver burden and limit societal cost.
The safety and efficacy of TDD for cancer pain treatment should also be considered. Results from a large multicenter registry study demonstrated that TDD was significantly associated with relieved baseline pain at 6 and 12 months after implantation, and quality of life (EQ-5D Index) significantly improved at 6 months.34 Long-term survivors demonstrated sustained quality-of-life improvement, with EQ-5D scores greater than 0.6 (with 1 indicating best health state) at 5 and 10 years after implantation. These clinical outcomes, combined with the robust financial savings, demonstrated within a year of starting therapy suggest that TDD offers clinical and economic value.
Society is faced with balancing costs and patient quality of life. This study highlights the challenges faced by payers and oncology practices managing patients with terminal, treatable, and treated cancers who have pain. Limited health care funds will increasingly affect medical decision making as the aging US and global populations continue to increase.
Limitations
This study has limitations. Mainly, MarketScan data are collected for billing purposes; information that does not influence reimbursement and coverage may not be reported. For example, cancer severity, quality-of-life scores, and death-related variables are not captured in claims data. However, based on patient characteristics and treatment patterns, we believe that this would not affect our results. In addition, it was unclear whether enrollment decline after index was attributable to death or a change in health care plans. It is also possible that propensity score matching did not account for unobserved selection bias because it can only control for the observed differences between groups. Factors such as pain scores and other multifactorial differences in both groups were not able to be analyzed with this data set. Also, this study used commercial insurance participants, which allows generalization to the larger US commercially insured population; further research is needed to explore other populations or health care systems.
Conclusions
Our study suggests that TDD is associated with reduced health care utilization and cost for patients with cancer pain. Increased use of TDD may also have the potential to reduce future health care cost and utilization associated with the expected incidence and survivorship of cancer in the United States. In addition, TDD may reduce long-term systemic opioid use and associated inherent risks among cancer survivors and society. Consideration of TDD for more patients with significant cancer-related pain may be associated with robust financial savings and improved quality of life.
eAppendix 1. Cancer Diagnosis Codes
eAppendix 2. Chemotherapy and Radiation Therapy
eAppendix 3. Tumor Ablation, Biopsy, Tumor Destruction, Tumor Excision, and Tumor Resection
eTable. Charlson Comorbidity Index
References
- 1.Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML. Projections of the cost of cancer care in the United States: 2010-2020. J Natl Cancer Inst. 2011;103(2):-. doi: 10.1093/jnci/djq495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bluethmann SM, Mariotto AB, Rowland JH. Anticipating the “silver tsunami”: prevalence trajectories and comorbidity burden among older cancer survivors in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1029-1036. doi: 10.1158/1055-9965.EPI-16-0133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kline RM, Bazell C, Smith E, Schumacher H, Rajkumar R, Conway PH. Centers for Medicare and Medicaid Services: using an episode-based payment model to improve oncology care. J Oncol Pract. 2015;11(2):114-116. doi: 10.1200/JOP.2014.002337 [DOI] [PubMed] [Google Scholar]
- 4.Patrick DL, Ferketich SL, Frame PS, et al. National Institutes of Health State-of-the-Science Conference statement: symptom management in cancer: pain, depression, and fatigue, July 15-17, 2002. J Natl Cancer Inst Monogr 2004(32):9-16. [DOI] [PubMed] [Google Scholar]
- 5.Panattoni LE, Fedorenko CR, Kreizenbeck KL, et al. The role of chronic disease in the costs of potentially preventable emergency department use during treatment: a regional study. J Clin Oncol. 2017;35(15):6505. doi: 10.1200/JCO.2017.35.15_suppl.6505 [DOI] [Google Scholar]
- 6.van den Beuken-van Everdingen MH, Hochstenbach LM, Joosten EA, Tjan-Heijnen VC, Janssen DJ Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage 2016;51(6):1070-1090, e1079. [DOI] [PubMed] [Google Scholar]
- 7.Paice JA, Ferrell B. The management of cancer pain. CA Cancer J Clin. 2011;61(3):157-182. doi: 10.3322/caac.20112 [DOI] [PubMed] [Google Scholar]
- 8.Cancer Pain Relief With A Guide to Opioid Availability 2nd ed. Geneva, Switzerland: World Health Organization; 1996. http://apps.who.int/iris/bitstream/10665/37896/1/9241544821.pdf. Accessed January 31, 2018.
- 9.Chou R, Turner JA, Devine EB, et al. The effectiveness and risks of long-term opioid therapy for chronic pain: a systematic review for a National Institutes of Health Pathways to Prevention Workshop. Ann Intern Med. 2015;162(4):276-286. doi: 10.7326/M14-2559 [DOI] [PubMed] [Google Scholar]
- 10.Swarm R, Abernethy AP, Anghelescu DL, et al. ; NCCN Adult Cancer Pain . Adult cancer pain. J Natl Compr Canc Netw. 2010;8(9):1046-1086. doi: 10.6004/jnccn.2010.0076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brogan SE, Winter NB, Abiodun A, Safarpour R. A cost utilization analysis of intrathecal therapy for refractory cancer pain: identifying factors associated with cost benefit. Pain Med. 2013;14(4):478-486. doi: 10.1111/pme.12060 [DOI] [PubMed] [Google Scholar]
- 12.Smith TJ, Staats PS, Deer T, et al. ; Implantable Drug Delivery Systems Study Group . Randomized clinical trial of an implantable drug delivery system compared with comprehensive medical management for refractory cancer pain: impact on pain, drug-related toxicity, and survival. J Clin Oncol. 2002;20(19):4040-4049. doi: 10.1200/JCO.2002.02.118 [DOI] [PubMed] [Google Scholar]
- 13.Stearns LJ, Hinnenthal JA, Hammond K, Berryman E, Janjan NA. Health services utilization and payments in patients with cancer pain: a comparison of intrathecal drug delivery vs. conventional medical management. Neuromodulation. 2016;19(2):196-205. doi: 10.1111/ner.12384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Caraway D, Walker V, Becker L, Hinnenthal J. Successful discontinuation of systemic opioids after implantation of an intrathecal drug delivery system. Neuromodulation. 2015;18(6):508-515. doi: 10.1111/ner.12318 [DOI] [PubMed] [Google Scholar]
- 15.Truven Heakth Analytics. Health Research Data for the Real World: The MarketScan Database (White Paper). Ann Arbor, MI: Truven Health Analytics; 2011. http://truvenhealth.com/portals/0/assets/PH_11238_0612_TEMP_MarketScan_WP_FINAL.pdf. Accessed August 21, 2017. [Google Scholar]
- 16.Truven Health Analytics. Commercial Claims and Encounters Medicare Supplemental (User Guide). Ann Arbor, MI: Truven Health Analytics; 2015. https://marketscan.truvenhealth.com/marketscanuniversity/userguide/2015%20MarketScanCCAE-MDCRUserGuide.pdf. Accessed August 21, 2017. [Google Scholar]
- 17.US Department of Health and Human Services Office for Human Research Protections. Human subject regulations decision charts. 2016. https://www.hhs.gov/ohrp/regulations-and-policy/decision-charts/index.html#c1. Accessed January 17, 2019.
- 18.Hansen L. The Truven Health MarketScan databases for life sciences researchers. 2017. https://truvenhealth.com/Portals/0/Assets/2017-MarketScan-Databases-Life-Sciences-Researchers-WP.pdf. Accessed August 21, 2017.
- 19.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320(7243):1197-1200. doi: 10.1136/bmj.320.7243.1197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Poncet A, Courvoisier DS, Combescure C, Perneger TV Normality and sample size do not matter for the selection of an appropriate statistical test for two-group comparisons. Methodology. 2016;12:61-71.
- 21.Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annu Rev Public Health. 2002;23:151-169. doi: 10.1146/annurev.publhealth.23.100901.140546 [DOI] [PubMed] [Google Scholar]
- 22.Fagerland MW. t-Tests, non-parametric tests, and large studies: a paradox of statistical practice? BMC Med Res Methodol. 2012;12:78. doi: 10.1186/1471-2288-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Medical care in U.S. city average, all urban consumers, not seasonally adjusted. 2017. https://data.bls.gov/timeseries/CUUR0000SAM?output_view=pct_12mths. Accessed February 27, 2019.
- 24.Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; March 13, 2015. http://www.medpac.gov/-documents-/reports. Accessed February 27, 2019.
- 25.Health Care Cost and Utilization Report: 2015 Washington, DC: Health Care Cost Institute; 2016. http://www.healthcostinstitute.org/report/2015-health-care-cost-utilization-report/. Accessed February 27, 2019.
- 26.Walsh B, Laudicella M. Disparities in cancer care and costs at the end of life: evidence from England’s National Health Service. Health Aff (Millwood). 2017;36(7):1218-1226. doi: 10.1377/hlthaff.2017.0167 [DOI] [PubMed] [Google Scholar]
- 27.Bekelman JE, Halpern SD, Blankart CR, et al. ; International Consortium for End-of-Life Research (ICELR) . Comparison of site of death, health care utilization, and hospital expenditures for patients dying with cancer in 7 developed countries. JAMA. 2016;315(3):272-283. doi: 10.1001/jama.2015.18603 [DOI] [PubMed] [Google Scholar]
- 28.Zuckerman IH, Davidoff AJ, Erten MZ, et al. Use of and spending on supportive care medications among Medicare beneficiaries with cancer. Support Care Cancer. 2014;22(8):2185-2195. doi: 10.1007/s00520-014-2187-2 [DOI] [PubMed] [Google Scholar]
- 29.Siegel R, DeSantis C, Virgo K, et al. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62(4):220-241. doi: 10.3322/caac.21149 [DOI] [PubMed] [Google Scholar]
- 30.Sutradhar R, Lokku A, Barbera L. Cancer survivorship and opioid prescribing rates: a population-based matched cohort study among individuals with and without a history of cancer. Cancer. 2017;123(21):4286-4293. doi: 10.1002/cncr.30839 [DOI] [PubMed] [Google Scholar]
- 31.Haltia O, Färkkilä N, Roine RP, et al. The indirect costs of palliative care in end-stage cancer: a real-life longitudinal register- and questionnaire-based study. Palliat Med. 2018;32(2):493-499. doi: 10.1177/0269216317729789 [DOI] [PubMed] [Google Scholar]
- 32.Lambert SD, Girgis A. Unmet supportive care needs among informal caregivers of patients with cancer: opportunities and challenges in informing the development of interventions. Asia Pac J Oncol Nurs. 2017;4(2):136-139. doi: 10.4103/2347-5625.204485 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzalo MB, House L, Santiago K, Buzaglo JS, Zaleta AK, Gupta NK. Access to care in cancer: barriers and challenges. J Clin Oncol. 2017;35(8):33. doi: 10.1200/JCO.2017.35.8_suppl.33 [DOI] [Google Scholar]
- 34.Stearns L. Targeted drug delivery (TDD) as a cancer-pain therapy option: registry safety and patient outcomes (ID 13337). Poster presented at: 22nd Annual Meeting of the North American Neuromodulation Society; January 17-20, 2019; Las Vegas, Nevada. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix 1. Cancer Diagnosis Codes
eAppendix 2. Chemotherapy and Radiation Therapy
eAppendix 3. Tumor Ablation, Biopsy, Tumor Destruction, Tumor Excision, and Tumor Resection
eTable. Charlson Comorbidity Index