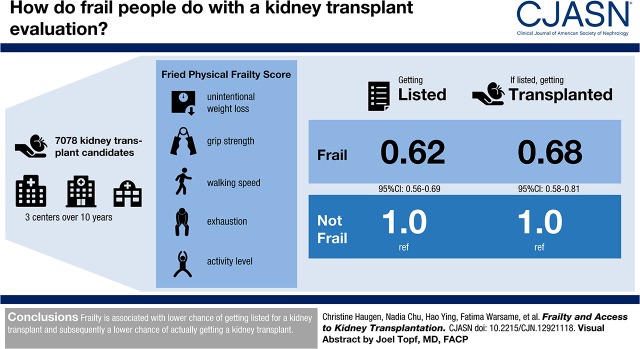
Visual Abstract
Keywords: outcomes; renal dialysis; kidney transplantation; Walking Speed; Accidental Falls; Outpatients; Prospective Studies; Frailty; Weight Loss; risk factors; Incidence; Kidney Failure, Chronic; Comorbidity; hospitalization; Transplants; Cognition; Hand Strength; Counseling
Abstract
Background and objectives
Frailty, a syndrome distinct from comorbidity and disability, is clinically manifested as a decreased resistance to stressors and is present in up to 35% of patient with ESKD. It is associated with falls, hospitalizations, poor cognitive function, and mortality. Also, frailty is associated with poor outcomes after kidney transplant, including delirium and mortality. Frailty is likely also associated with decreased access to kidney transplantation, given its association with poor outcomes on dialysis and post-transplant. Yet, clinicians have difficulty identifying which patients are frail; therefore, we sought to quantify if frail kidney transplant candidates had similar access to kidney transplantation as nonfrail candidates.
Design, setting, participants, & measurements
We studied 7078 kidney transplant candidates (2009–2018) in a three-center prospective cohort study of frailty. Fried frailty (unintentional weight loss, grip strength, walking speed, exhaustion, and activity level) was measured at outpatient kidney transplant evaluation. We estimated time to listing and transplant rate by frailty status using Cox proportional hazards and Poisson regression, adjusting for demographic and health factors.
Results
The mean age was 54 years (SD 13; range, 18–89), 40% were women, 34% were black, and 21% were frail. Frail participants were almost half as likely to be listed for kidney transplantation (hazard ratio, 0.62; 95% confidence interval, 0.56 to 0.69; P<0.001) compared with nonfrail participants, independent of age and other demographic factors. Furthermore, frail candidates were transplanted 32% less frequently than nonfrail candidates (incidence rate ratio, 0.68; 95% confidence interval, 0.58 to 0.81; P<0.001).
Conclusions
Frailty is associated with lower chance of listing and lower rate of transplant, and is a potentially modifiable risk factor.
Introduction
Frailty is characterized by decreased physiologic reserve and resistance to stressors and was initially studied in community-dwelling older adults (1). Additionally, frailty has been well described in patients of all ages with ESKD. Up to 35% of patients on hemodialysis are frail, and frailty is associated with falls (2), hospitalizations (3–5), poor cognitive function (6), poorer health-related quality of life (7), and mortality (3,5,8). Furthermore, up to 20% of kidney transplant recipients are frail, and frailty is associated with poor outcomes after kidney transplant, such as delirium (9), delayed graft function (10), longer length of stay (11), early hospital readmission (12), immunosuppression intolerance (13), lower health-related quality of life (14), and mortality (15). However, despite poor outcomes for frail kidney transplant candidates and recipients, clinicians are unable to identify frail patients (16), and patients also have difficulty reporting their frailty status (17).
Frailty at evaluation may be associated with lower access to kidney transplantation because of known poor outcomes while on the waitlist (18) and after surgery (9,11–15,19). Quantification of the association between frailty and access to kidney transplantation is imperative because an increased number of older adults undergo kidney transplantation (20), and these recipients are more likely to be frail (15). Thus, identification of robust older kidney transplant candidates is important for improved post-transplant outcomes. It is likely that frailty is associated with lower access to kidney transplantation, similar to other demographic factors that are associated with lower access to kidney transplantation, including age (21,22), sex (23–25), and race (26). Notably, frailty is a potentially modifiable candidate characteristic, unlike age, sex, or race, and could be improved before kidney transplantation, thus allowing for the improvement of candidates (27). Characterization of the relationship of frailty and access to kidney transplantation may lend insight toward improvement in access to kidney transplantation for patients with ESKD (28).
To better understand the role of frailty with access to transplantation in patients with ESKD who are referred for kidney transplantation evaluation, we used a prospective cohort to quantify the association of frailty with time to kidney transplant listing, waitlist mortality, and transplant rate. Additionally, to test whether frailty could explain age, sex, or race disparities, thus we explored interactions between frailty and each characteristic for each outcome, in separate models.
Materials and Methods
Study Design
This was a prospective, longitudinal cohort study of 7078 adult (age ≥18 years) participants with ESKD who were being evaluated for transplantation at the Johns Hopkins Hospital, Baltimore, Maryland (September 2009 to February 2018; n=3278), Methodist Specialty and Transplant Hospital, San Antonio, Texas (May 2015 to February 2018; n=3515), and University of Michigan, Ann Arbor, Michigan (January 2015 to May 2016; n=285). We measured frailty at the time of evaluation, as described below. Additional participant characteristics that are consistent with data collected in the national registry of transplant recipients (Scientific Registry of Transplant Recipients [SRTR]) were also assessed at this time or abstracted from the transplant evaluation medical record (age, sex, race, ethnicity, cause of ESKD, blood type [A, B, AB, or O], dialysis vintage, and body mass index [BMI]). Race/ethnicity was self-reported and collected as white/non-Hispanic, black, white/Hispanic, Asian, or other. Two participants with missing BMI, cause of ESKD, and blood type were excluded from the analyses. The Johns Hopkins Institutional Review Board (NA_00015758), the Methodist Specialty and Transplant Hospital Institutional Review Board (IRB IS 00000435), and the University of Michigan Institutional Review Board (HUM00088077) approved the study. The clinical and research activities being reported are consistent with the principles of the Declaration of Istanbul as outlined in the Declaration of Istanbul on Organ Trafficking and Transplant Tourism.
Frailty
We studied the physical frailty phenotype as defined by Fried et al. (1) and validated in older adults (1,12,29–39) and in ESKD and kidney transplant populations (2,3,6,7,9–13,15,18,40,41). The Fried physical frailty phenotype was on the basis of five components: shrinking (self-report of unintentional weight loss of >10 pounds in the past year, on the basis of dry weight), weakness (grip strength below an established cut-off on the basis of sex and BMI), exhaustion (self-report), low activity (kilocalories per week below an established cut-off), and slowed walking speed (walking time of 15 feet below an established cut-off by sex and height) (1). Each of the five components was scored as 0 or 1, representing the absence or presence of that component. The aggregate frailty score was calculated as the sum of the component scores (range, 0–5); frailty was defined as a score of ≥3. The physicians at Johns Hopkins Hospital and University of Michigan were not aware of the frailty assessment results at time of evaluation, but the physicians at Methodist Specialty and Transplant Hospital were aware of the frailty assessment at the selection committee meeting.
Time to Kidney Transplant Listing
Among participants with ESKD who were not listed for kidney transplant at the time of frailty evaluation (n=5423), time to kidney transplant listing was defined as the time from clinic evaluation date to active placement on the kidney transplant waitlist or censoring on March 1, 2018 and estimated at 6 months and 1 and 3 years using the Kaplan–Meier method by frailty status. The Kaplan–Meier method was used to create unadjusted cumulative incidence curves of kidney transplant listing by frailty status. The log-rank test of equality was used to compare unadjusted cumulative incidence curves. Cox proportional hazards model were used to estimate the chance of kidney transplant listing by frailty status, then adjusted for potential confounders, including participant age, sex, race, and transplant center. Proportional hazards assumptions were confirmed with visual inspection of complementary log-log plots and Schoenfeld residuals. To test whether association between frailty status and time to kidney transplant listing varied by participant age, race/ethnicity, or sex, an interaction between participant age (age <65 versus age ≥65 years), race/ethnicity (black versus nonblack), or sex (women versus men) and frailty status in separate models was explored using Wald tests.
Waitlist Mortality
Among participants with ESKD who were listed (kidney transplant candidates) (n=4552), the risk of waitlist mortality was estimated at 6 months and 1, 3, and 5 years using a competing risk framework by frailty status (42). Also, a competing risk framework was used to create unadjusted cumulative incidence curves of waitlist mortality by frailty status. Kidney transplant was considered a competing risk for waitlist mortality, and the time origin was date of kidney transplant listing with censoring date on March 1, 2018. Subhazard ratios of waitlist mortality by frailty status were obtained using the Fine and Gray method for competing risks, and these models were adjusted for potential confounders, including age, sex, race/ethnicity, BMI, cause of ESKD, blood type, dialysis vintage, and center, on the basis of covariates used in the SRTR model for waitlist mortality (42). To test whether the association of waitlist mortality and frailty varied by participant age, sex, or race/ethnicity (as described above), an interaction between participant each characteristic and frailty status was explored in separate models using Wald tests.
Transplant Rate
Among active waitlist kidney transplant candidates (n=4552), transplant rates were estimated at 6 months and 1, 3, and 5 years, using a competing risk framework by frailty status. A competing risk framework was used to create unadjusted cumulative incidence curves of kidney transplantation by frailty status. We report cumulative incidence of kidney transplant treating waitlist mortality as competing risk. Incidence rate ratios of kidney transplantation by frailty status were obtained using Poisson regression, and person-time was calculated from date of kidney transplant listing to date of kidney transplant, mortality, or censoring on March 1, 2018. Poisson models were adjusted for potential confounders, including age, sex, race/ethnicity, BMI, cause of ESKD, blood type, dialysis vintage, and center. To test whether the association of transplant rate and frailty varied by participant age, race/ethnicity, or sex (as described above), an interaction between each participant characteristic and frailty status in separate models was explored using Wald tests.
Statistical Analyses
Comparison of candidate characteristics at kidney transplantation evaluation were performed using chi-squared test for categorical variables and t tests for continuous variables. All analyses were two-tailed and α was set at 0.05. All analyses were performed using Stata v14.2/MP (College Station, TX).
Sensitivity Analyses
To check whether the inferences for the association of frailty and waitlist mortality and transplant rate changed when not accounting for competing risks, we used Cox proportional hazard models to quantify the risk of waitlist mortality and kidney transplantation. Additionally, we added year of evaluation to all analyses to account for the fact that patients from Johns Hopkins Hospital were recruited over a longer period of time and account for temporal changes. Finally, we stratified the time to listing, waitlist mortality, and transplant rate analyses by transplant center (Johns Hopkins Hospital and University of Michigan versus Methodist) to see if inferences differed by center, given that Methodist was aware of the frailty assessments at the listing committee meetings.
Results
Study Population: Kidney Transplant Evaluation Participants
Among 5423 kidney transplant evaluation participants, the mean age was 54 years (SD 13; range, 18–89), 40% were women, and 34% were black. A total of 957 (18%) of the evaluation participants with ESKD were frail (Table 1). Frail evaluation participants were more likely to be older (56 versus 53 years; P<0.001) and be black (43% versus 32%; P<0.001) compared with nonfrail evaluation participants.
Table 1.
Cumulative incidence (%) of listing, waitlist mortality, and kidney transplantation
| Outcome by Frailty Status | n | Cumulative Incidence, % | Multivariable Models | ||||
|---|---|---|---|---|---|---|---|
| 6 mo | 1 yr | 3 yr | 5 yr | ||||
| Chance of listing | Adjusted HR (95% CI) | P value | |||||
| Nonfrail | 4466 | 47 | 56 | 62 | N/A | Reference | |
| Frail | 957 | 33 | 41 | 46 | N/A | 0.62 (0.56 to 0.69) | <0.001 |
| Risk of waitlist mortality | Adjusted SHR (95% CI) | P value | |||||
| Nonfrail | 3991 | 1 | 2 | 10 | 18 | Reference | |
| Frail | 561 | 2 | 4 | 18 | 33 | 1.70 (1.36 to 2.14) | <0.001 |
| Chance of kidney transplantation | Adjusted IRR (95% CI) | P value | |||||
| Nonfrail | 3991 | 14 | 21 | 35 | 43 | Reference | |
| Frail | 561 | 11 | 16 | 28 | 34 | 0.68 (0.58 to 0.81) | <0.001 |
Cox proportional hazards were adjusted for age, sex, and race for chance of kidney transplantation listing. Competing risk models were used to quantify the risk of waitlist mortality by frailty status in kidney transplant waitlist candidates. Transplant was treated as a competing risk, and models were adjusted for age, sex, race, body mass index, cause of ESKD, and blood type. Poisson regression was used to calculate the incidence rate ratio of kidney transplant and adjusted for age, sex, race, body mass index, cause of ESKD, and blood type. HR, hazard ratio; 95% CI, 95% confidence interval; N/A, not available; SHR, subhazard ratio; IRR, incidence rate ratio.
The prevalence of frailty among kidney transplant evaluation participants differed by center (P<0.001; Johns Hopkins Hospital, 21%; University of Michigan, 20%; and Methodist Specialty and Transplant Hospital, 11%). The average age among participants evaluated for kidney transplant varied by centers (P<0.001; Johns Hopkins Hospital, 55±14; University of Michigan, 54±14; and Methodist Specialty and Transplant, 52±13 years). Also, race/ethnicity varied between centers (P<0.001; Johns Hopkins Hospital, 48% black; University of Michigan, 24% black; and Methodist Specialty and Transplant, 11% black).
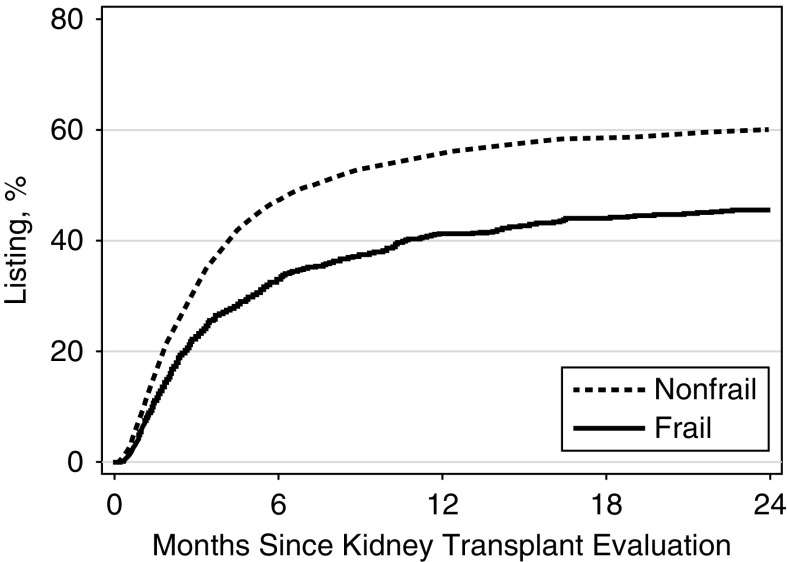
Time to Kidney Transplant Listing
Frail kidney transplant candidates were less likely to be listed (log-rank P<0.001) (Figure 1). Cumulative incidence of listing, in frail versus nonfrail kidney transplant candidates, was 33% versus 47% at 6 months, 41% versus 56% at 1 year, and 46% versus 62% at 3 years (Table 1). After adjustment, frail candidates were at a 38% lower chance of listing compared with nonfrail candidates (adjusted hazard ratio [aHR], 0.62; 95% confidence interval [95% CI], 0.56 to 0.69; P<0.001) (Table 1).
Figure 1.
Frailty is associated with decrease cumulative incidence of listing for kidney transplantation (log rank P<0.001). Cumulative incidence of listing for kidney transplantation in evaluation participants (n=5423) by frailty status.
The association between time to listing and frailty varied by participant race/ethnicity (P for interaction=0.002). Frail black candidates were 25% less likely to be listed than nonfrail black candidates (aHR, 0.75; 95% CI, 0.64 to 0.87; P<0.001); however, frail nonblack candidates were 46% less likely to be listed than nonfrail nonblack candidates (aHR, 0.54; 95% CI, 0.47 to 0.62; P<0.001). The association between time to listing and frailty did not vary by participant age (P for interaction=0.8) or sex (P for interaction=0.3).
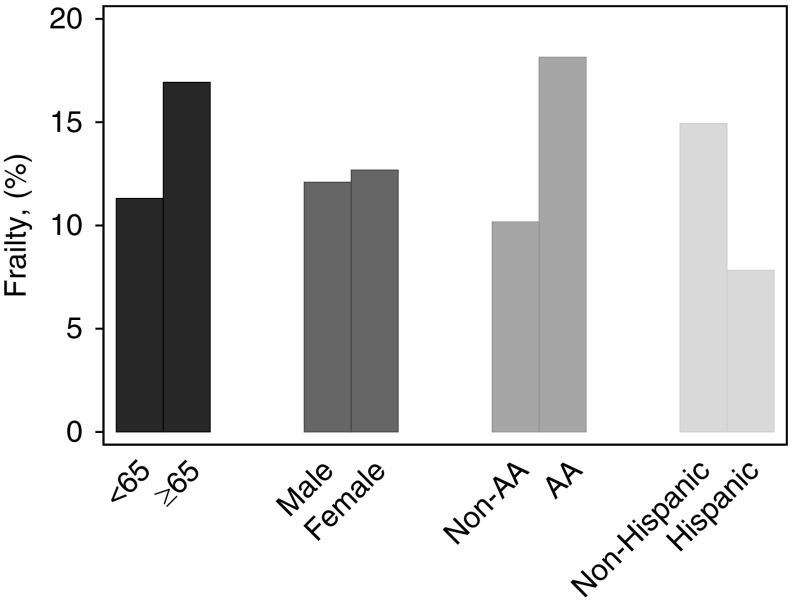
Study Population: Kidney Transplant Candidates
Of the 7078 participants with ESKD who were evaluated, 4552 were listed for kidney transplantation (kidney transplant candidates) during the study period. The mean age of kidney transplant candidates was 52 years (SD 13; range, 18–87 years). A total of 561 (12%) kidney transplant candidates were frail (Table 2). Frail kidney transplant candidates were more likely to be older (55±13 versus 52±13 years; P<0.001) and black (40% versus 25%; P<0.001), but were less likely to be Hispanic (23% versus 39%; P<0.001) than nonfrail kidney transplant candidates (Figure 2, Table 2). Frail kidney transplant candidates were more likely to have diabetes as cause of ESKD (43% versus 37%; P=0.01) (Table 2). Frail candidates had shorter average time on dialysis than nonfrail candidates (2.5±3.5 versus 3.3±3.5 years; P<0.001) (Table 2).
Table 2.
Demographics of 4552 waitlisted kidney transplant candidates by frailty status
| Demographics | Nonfrail, n=3991 | Frail, n=561 |
|---|---|---|
| Age, yra | 52 (13) | 55 (13) |
| Women, n (%) | 1570 (39) | 228 (41) |
| Body mass index, kg/m2a | 30 (6) | 30 (6) |
| Race/ethnicity, n (%) | ||
| White | 1299 (33) | 196 (35) |
| Black | 1007 (25) | 223 (40) |
| Hispanic | 1541 (39) | 131 (23) |
| Asian | 125 (3) | 10 (2) |
| Other | 19 (0.5) | (0.2) |
| Cause of kidney failure, n (%) | ||
| Hypertension | 943 (24) | 136 (24) |
| Diabetes mellitus | 1456 (37) | 241 (43) |
| Glomerular disease | 682 (17) | 79 (14) |
| Cystic disease | 273 (7) | 27 (5) |
| Other | 637 (16) | 78 (14) |
| Blood type, n (%) | ||
| A | 1182 (30) | 189 (34) |
| B | 595 (15) | 73 (13) |
| AB | 123 (3) | 19 (3) |
| O | 2091 (52) | 280 (50) |
| Dialysis vintage, yra | 3.3 (3.5) | 2.5 (3.5) |
| Fried frailty scorea | 1 (0.8) | 3 (0.5) |
Mean (SD).
Figure 2.
Prevalence of frailty is higher in older, black, and non-Hispanic candidates. AA, black participants.
The prevalence of frailty among kidney transplant candidates differed by center (P<0.001; Johns Hopkins Hospital, 18%; University of Michigan, 11%; and Methodist Specialty and Transplant Hospital, 7%). The average age varied between centers (P<0.001; Johns Hopkins Hospital, 54±13 years; University of Michigan, 52±14 years; and Methodist Specialty and Transplant Hospital, 51±12 years). Also, race/ethnicity varied between centers (P<0.001; Johns Hopkins Hospital, 45% black; University of Michigan, 21% black; and Methodist Specialty and Transplant Hospital, 11% black).
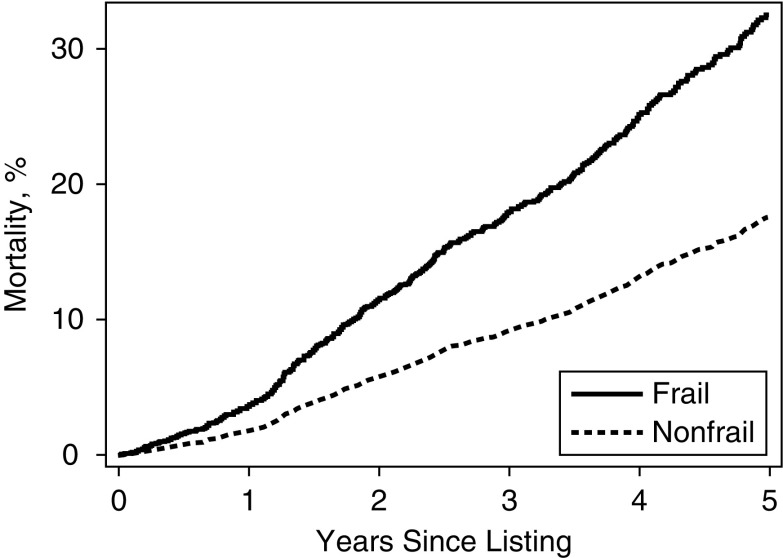
Waitlist Mortality
Waitlist mortality was higher in frail kidney transplant candidates (log-rank P<0.001) (Figure 3). The cumulative incidence of waitlist mortality for frail versus nonfrail kidney transplant candidates was 2% versus 1% at 6 months, 4% versus 2% at 1 year, 18% versus 10% at 3 years, and 33% versus 18% at 5 years after listing (Table 1). After adjustment, frail kidney transplant candidates had nearly 1.7-fold higher risk of waitlist mortality (adjusted subhazard ratio, 1.70; 95% CI, 1.36 to 2.14; P<0.001) compared with younger kidney transplant candidates (Table 1). The association between waitlist mortality and frailty did not vary by participant age (P for interaction=0.2), sex (P for interaction=0.7), or race (P for interaction=0.2).
Figure 3.
Frail kidney transplant candidates had a higher cumulative incidence of waitlist mortality (log rank P<0.001). Cumulative incidence of waitlist mortality in 4558 waitlisted participants by frailty status. Kidney transplant was considered a competing risk for waitlist mortality.
Transplant Rate
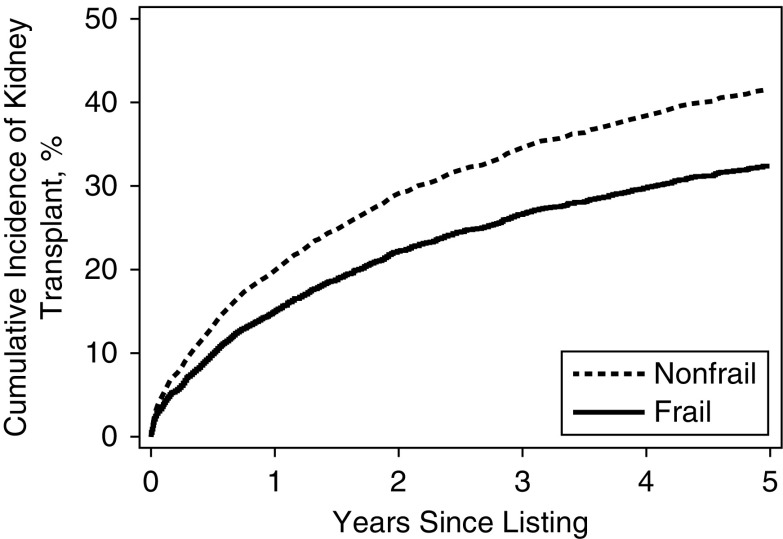
Of the 4552 candidates who were listed for kidney transplantation, 1612 (35%) underwent kidney transplantation during the study period. The cumulative incidence of kidney transplantation was lower among frail kidney transplant candidates (log-rank P<0.001) (Figure 4). The cumulative incidence of kidney transplantation for frail versus nonfrail kidney transplant candidates was 11% versus 14% at 6 months, 16% versus 21% at 1 year, 28% versus 35% at 3 years, and 34% versus 43% at 5 years (Table 1). After adjustment, frail kidney transplant candidates were 35% less likely to undergo kidney transplantation compared with nonfrail kidney transplant candidates (adjusted incidence rate ratio, 0.68; 95% CI, 0.58 to 0.81; P<0.001) (Table 1). The association between waitlist mortality and frailty did not vary by participant age (P for interaction=0.3), sex (P for interaction=0.9), or race (P for interaction=0.1).
Figure 4.
Frail kidney transplant candidates had a lower cumulative incidence of transplant (log rank P<0.001). Cumulative incidence of kidney transplantation in 4552 waitlisted participants by frailty status. Kidney transplant candidates only contributed time to the risk set while active on the waitlist. Waitlist mortality was considered a competing risk for kidney transplant.
Sensitivity Analyses
For the 4552 kidney transplant candidates, the inferences for the risk of waitlist mortality and transplant rate were similar when analyzed with Cox proportional hazard models. Frail kidney transplant candidates were at a 1.42-fold higher risk of waitlist mortality (aHR, 1.42; 95% CI, 1.14 to 1.79; P<0.001) and 33% lower chance of undergoing kidney transplantation (aHR, 0.67; 95% CI, 0.57 to 0.79; P<0.001). Additionally, after addition of the evaluation year to multivariable models, all inferences remained consistent. Finally, the inferences for the primary analyses did not change when stratified by center (Supplemental Table 1).
Discussion
In this prospective cohort of frailty including 7078 participants with ESKD, frail participants were more likely to be older (P<0.001), black (P<0.001), and have diabetes as the cause of ESKD (P=0.01) than nonfrail participants. Additionally, we found frail participants were 38% less likely to be listed for kidney transplantation (aHR, 0.62; 95% CI, 0.52 to 0.69), had a 1.7-fold higher risk of waitlist mortality (adjusted subhazard ratio, 1.70; 95% CI, 1.36 to 2.14), and were 32% less likely to undergo kidney transplantation (adjusted incidence rate ratio, 0.68; 95% CI, 0.58 to 0.81) compared with nonfrail participants even after accounting for age, sex, BMI, race/ethnicity, blood type, cause of ESKD, and dialysis vintage.
Our finding of a lower chance of listing in frail participants with ESKD, regardless of age, is important to consider with respect to previous studies demonstrated that as a patient with ESKD ages, their odds and relative rate of placement on the waitlist decreases (21,26). Frail participants were more likely to be older, but the association of frailty and listing did not vary by participant age. Importantly, frailty is a modifiable risk factor unlike age. We were able to build on these findings, demonstrating that the association between age and kidney transplant listing is modified by frailty status, such that regardless of age, frail participants are less likely to be listed. Improvement of frailty status through prehabilitation may increase access to kidney transplantation (28,43). Notably, the association of frailty and listing varied by race/ethnicity: frail black candidates were 25% less likely to be listed than nonfrail black candidates (aHR, 0.75; 95% CI, 0.64 to 0.87; P<0.001); however, frail nonblack candidates were 46% less likely to be listed than nonfrail nonblack candidates (aHR, 0.54; 95% CI, 0.47 to 0.62; P<0.001). Black participants were younger than nonblack participants in this cohort (54±13 versus 57±13 years; P=0.05), so this may contribute to the lesser association of frailty and race interaction in a lower chance of listing.
Our finding that higher waitlist mortality is associated with frailty confirms previous work by our group, assessing the association of frailty and inflammatory markers with waitlist mortally in kidney transplant candidates (18). However, we extended this to a larger, multicenter study population and further tested for an interaction between frailty and waitlist mortality with candidate age, race, and sex. Notably, the association of frailty and waitlist mortality does not differ by candidate age. This finding supports prior hypotheses that frailty represents physiologic age, rather than chronologic age, when considering patients of all ages for kidney transplant listing, and that frail candidates tend to do worse, ultimately affecting chances of kidney transplantation listing. It is likely that mortality is driven by biologic factors, such as frailty, that would affect candidates regardless of their age.
Our finding of lower kidney transplantation rate in frail versus nonfrail candidates, allowing for an interaction with candidate age, is important to consider in conjunction with previous studies that demonstrated older candidates are less likely to undergo kidney transplantation than younger candidates (21,26). We have added to these previous findings by describing the association of frailty and transplant rate in kidney transplant candidates, and our findings demonstrate that frailty status leads to a lower incidence of kidney transplantation, regardless of age.
Frailty was independently associated with higher risk of waitlist mortality and lower kidney transplantation rate. Importantly, these associations are present after accounting for standard confounders seen in patients with ESKD; factors that may confound the relationship with a clinician’s frailty assessment, and common characteristics that are collected as part of clinical practice and sometimes used as a surrogate for frailty, such as age, BMI, and dialysis vintage, were included as confounders in our adjusted models. Through our analyses, it is difficult to know if physicians were good at assessing frailty or noted other factors that are surrogates of frailty.
Strengths of this study include a large sample size cohort from three hospitals, prospective study design, and the measurement of frailty. The main limitation of this study is the number of centers included, so inferences must be limited to this context. However, to our knowledge, this is the largest study to date of frailty, listing practices, and outcomes on the kidney transplant waitlist. Another limitation is that there may be selection bias based on who is referred for kidney transplant evaluation from the community, but there is no way to quantify frailty in patients who were not referred for evaluation in the transplant center setting. Additionally, there may be regional variation in candidate selection on the basis of general nephrologist referral patterns in the communities.
In conclusion, frailty is associated with lower chance of listing, higher waitlist mortality, and lower incidence of kidney transplantation. Importantly, frailty (unlike age, sex, or race) is a potentially modifiable risk factor for poor outcomes, so optimization (e.g., through prehabilitation) when on dialysis would likely improve outcomes in this vulnerable group. This is crucial for clinicians to consider during kidney transplantation referral and evaluation, to identify patients who may benefit from prehabilitation and increase their physiologic reserve when waiting for kidney transplantation.
Disclosures
Dr. Desai reports grants and personal fees from Merck and Co., outside the submitted work. Dr. Bingaman, Dr. Brennan, Dr. Chu, Dr. Garonzik-Wang, Dr. Haugen, Dr. Holscher, Dr. Jones, Dr. McAdams-DeMarco, Dr. Norman, Dr. Segev, Dr. Warsame, Dr. Waslton, and Dr. Ying have nothing to disclose.
Supplementary Material
Acknowledgments
C.E.H., C.M.H., F.W., N.M.D., M.R.J., S.P.N., J.G.-W., J.D.W., D.L.S., and M.M.-D. contributed to the conception and design. C.E.H., H.Y., N.M.C, S.P.N., D.C.B., D.L.S., and M.M.-D. contributed to the acquisition of data or analysis and interpretation of the data. C.E.H., C.M.H., H.Y., F.W., N.M.D., N.M.C., K.R.J., M.R.J., S.P.N., D.C.B., J.G.-W., J.D.W., D.L.S., and M.M.-D. contributed to drafting the article or revising it critically for important intellectual content. C.E.H., C.M.H., H.Y., F.W., N.M.D., N.M.C., M.R.J., S.P.N., D.C.B., J.G.-W., J.D.W., D.L.S., and M.M.-D. approved the final version to be published and are accountable for all aspects of the work.
Funding for this study was provided by the National Institute of Diabetes and Digestive and Kidney Disease and the National Institute of Aging: grant numbers T32DK007732 (to C.E.H.), F32AG053025 (Principal Investigator: C.E.H.), F32DK109662 (Principal Investigator: C.M.H.), K23DK115908 01 (Principal Investigator: J.G.-W.), K24DK101828 (Principal Investigator: D.L.S.), R01AG055781 (Principal Investigator: M.M.-D.), R01DK114074 (Principal Investigator: M.M.-D.), and K01AG043501 (Principal Investigator: M.M.-D.).
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
Supplemental Material
This article contains the following supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.12921118/-/DCSupplemental.
Supplemental Table 1. Cumulative incidence (%) of listing, waitlist mortality, and kidney transplantation by frailty status, stratified by transplant center: Johns Hopkins Hospital (JHH), University of Michigan (UM), and Methodist Specialty Transplant Center.
References
- 1.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA; Cardiovascular Health Study Collaborative Research Group : Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci 56: M146–M156, 2001 [DOI] [PubMed] [Google Scholar]
- 2.McAdams-DeMarco MA, Suresh S, Law A, Salter ML, Gimenez LF, Jaar BG, Walston JD, Segev DL: Frailty and falls among adult patients undergoing chronic hemodialysis: A prospective cohort study. BMC Nephrol 14: 224, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAdams-DeMarco MA, Law A, Salter ML, Boyarsky B, Gimenez L, Jaar BG, Walston JD, Segev DL: Frailty as a novel predictor of mortality and hospitalization in individuals of all ages undergoing hemodialysis. J Am Geriatr Soc 61: 896–901, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Johansen KL, Dalrymple LS, Delgado C, Chertow GM, Segal MR, Chiang J, Grimes B, Kaysen GA: Factors associated with frailty and its trajectory among patients on hemodialysis. Clin J Am Soc Nephrol 12: 1100–1108, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bao Y, Dalrymple L, Chertow GM, Kaysen GA, Johansen KL: Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med 172: 1071–1077, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McAdams-DeMarco MA, Tan J, Salter ML, Gross A, Meoni LA, Jaar BG, Kao WH, Parekh RS, Segev DL, Sozio SM: Frailty and cognitive function in incident hemodialysis patients. Clin J Am Soc Nephrol 10: 2181–2189, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McAdams-DeMarco MA, Ying H, Olorundare I, King EA, Desai N, Dagher N, Lonze B, Montgomery R, Walston J, Segev DL: Frailty and health-related quality of life in end stage renal disease patients of all ages. J Frailty Aging 5: 174–179, 2016 [PMC free article] [PubMed] [Google Scholar]
- 8.Johansen KL, Dalrymple LS, Glidden D, Delgado C, Kaysen GA, Grimes B, Chertow GM: Association of performance-based and self-reported function-based definitions of frailty with mortality among patients receiving hemodialysis. Clin J Am Soc Nephrol 11: 626–632, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haugen CE, Mountford A, Warsame F, Berkowitz R, Bae S, Thomas AG, Brown CH 4th, Brennan DC, Neufeld KJ, Carlson MC, Segev DL, McAdams-DeMarco M: Incidence, risk factors, and sequelae of post-kidney transplant delirium. J Am Soc Nephrol 29: 1752–1759, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garonzik-Wang JM, Govindan P, Grinnan JW, Liu M, Ali HM, Chakraborty A, Jain V, Ros RL, James NT, Kucirka LM, Hall EC, Berger JC, Montgomery RA, Desai NM, Dagher NN, Sonnenday CJ, Englesbe MJ, Makary MA, Walston JD, Segev DL: Frailty and delayed graft function in kidney transplant recipients. Arch Surg 147: 190–193, 2012 [DOI] [PubMed] [Google Scholar]
- 11.McAdams-DeMarco MA, King EA, Luo X, Haugen C, DiBrito S, Shaffer A, Kucirka LM, Desai NM, Dagher NN, Lonze BE, Montgomery RA, Walston J, Segev DL: Frailty, length of stay, and mortality in kidney transplant recipients: A national registry and prospective cohort study. Ann Surg 266: 1084–1090, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.McAdams-DeMarco MA, Law A, Salter ML, Chow E, Grams M, Walston J, Segev DL: Frailty and early hospital readmission after kidney transplantation. Am J Transplant 13: 2091–2095, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McAdams-DeMarco MA, Law A, Tan J, Delp C, King EA, Orandi B, Salter M, Alachkar N, Desai N, Grams M, Walston J, Segev DL: Frailty, mycophenolate reduction, and graft loss in kidney transplant recipients. Transplantation 99: 805–810, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McAdams-DeMarco MA, Olorundare IO, Ying H, Warsame F, Haugen CE, Hall R, Garonzik-Wang JM, Desai NM, Walston JD, Norman SP, Segev DL: Frailty and postkidney transplant health-related quality of life. Transplantation 102: 291–299, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McAdams-DeMarco MA, Law A, King E, Orandi B, Salter M, Gupta N, Chow E, Alachkar N, Desai N, Varadhan R, Walston J, Segev DL: Frailty and mortality in kidney transplant recipients. Am J Transplant 15: 149–154, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Salter ML, Gupta N, Massie AB, McAdams-DeMarco MA, Law AH, Jacob RL, Gimenez LF, Jaar BG, Walston JD, Segev DL: Perceived frailty and measured frailty among adults undergoing hemodialysis: A cross-sectional analysis. BMC Geriatr 15: 52, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Van Pilsum Rasmussen S, Konel J, Warsame F, Ying H, Buta B, Haugen C, King E, DiBrito S, Varadhan R, Rodríguez-Mañas L, Walston JD, Segev DL, McAdams-DeMarco MA: Engaging clinicians and patients to assess and improve frailty measurement in adults with end stage renal disease. BMC Nephrol 19: 8, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAdams-DeMarco MA, Ying H, Thomas AG, Warsame F, Shaffer AA, Haugen CE, Garonzik-Wang JM, Desai NM, Varadhan R, Walston J, Norman SP, Segev DL: Frailty, inflammatory markers, and waitlist mortality among patients with end-stage renal disease in a prospective cohort study. Transplantation 102: 1740–1746, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Makary MA, Segev DL, Pronovost PJ, Syin D, Bandeen-Roche K, Patel P, Takenaga R, Devgan L, Holzmueller CG, Tian J, Fried LP: Frailty as a predictor of surgical outcomes in older patients. J Am Coll Surg 210: 901–908, 2010 [DOI] [PubMed] [Google Scholar]
- 20.McAdams-DeMarco MA, James N, Salter ML, Walston J, Segev DL: Trends in kidney transplant outcomes in older adults. J Am Geriatr Soc 62: 2235–2242, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wolfe RA, Ashby VB, Milford EL, Bloembergen WE, Agodoa LY, Held PJ, Port FK: Differences in access to cadaveric renal transplantation in the United States. Am J Kidney Dis 36: 1025–1033, 2000 [DOI] [PubMed] [Google Scholar]
- 22.Grams ME, Kucirka LM, Hanrahan CF, Montgomery RA, Massie AB, Segev DL: Candidacy for kidney transplantation of older adults. J Am Geriatr Soc 60: 1–7, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexander GC, Sehgal AR: Barriers to cadaveric renal transplantation among blacks, women, and the poor. JAMA 280: 1148–1152, 1998 [DOI] [PubMed] [Google Scholar]
- 24.Patzer RE, Plantinga LC, Paul S, Gander J, Krisher J, Sauls L, Gibney EM, Mulloy L, Pastan SO: Variation in dialysis facility referral for kidney transplantation among patients with end-stage renal disease in Georgia. JAMA 314: 582–594, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Salter ML, McAdams-Demarco MA, Law A, Kamil RJ, Meoni LA, Jaar BG, Sozio SM, Kao WH, Parekh RS, Segev DL: Age and sex disparities in discussions about kidney transplantation in adults undergoing dialysis. J Am Geriatr Soc 62: 843–849, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schold JD, Gregg JA, Harman JS, Hall AG, Patton PR, Meier-Kriesche HU: Barriers to evaluation and wait listing for kidney transplantation. Clin J Am Soc Nephrol 6: 1760–1767, 2011 [DOI] [PubMed] [Google Scholar]
- 27.Puts MTE, Toubasi S, Andrew MK, Ashe MC, Ploeg J, Atkinson E, Ayala AP, Roy A, Rodríguez Monforte M, Bergman H, McGilton K: Interventions to prevent or reduce the level of frailty in community-dwelling older adults: A scoping review of the literature and international policies. Age Ageing 46: 383–392, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McAdams-DeMarco MA, Ying H, Van Pilsum Rasmussen S, Schrack J, Haugen CE, Chu NM, Gonzalez Fernandez M, Desai N, Walston JD, Segev DL: Prehabilitation prior to kidney transplantation: Results from a pilot study. Clin Transplant 33: e13450, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bandeen-Roche K, Xue QL, Ferrucci L, Walston J, Guralnik JM, Chaves P, Zeger SL, Fried LP: Phenotype of frailty: Characterization in the women’s health and aging studies. J Gerontol A Biol Sci Med Sci 61: 262–266, 2006 [DOI] [PubMed] [Google Scholar]
- 30.Barzilay JI, Blaum C, Moore T, Xue QL, Hirsch CH, Walston JD, Fried LP: Insulin resistance and inflammation as precursors of frailty: The cardiovascular health study. Arch Intern Med 167: 635–641, 2007 [DOI] [PubMed] [Google Scholar]
- 31.Cappola AR, Xue QL, Fried LP: Multiple hormonal deficiencies in anabolic hormones are found in frail older women: The women’s health and aging studies. J Gerontol A Biol Sci Med Sci 64: 243–248, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leng SX, Hung W, Cappola AR, Yu Q, Xue QL, Fried LP: White blood cell counts, insulin-like growth factor-1 levels, and frailty in community-dwelling older women. J Gerontol A Biol Sci Med Sci 64: 499–502, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leng SX, Xue QL, Tian J, Walston JD, Fried LP: Inflammation and frailty in older women. J Am Geriatr Soc 55: 864–871, 2007 [DOI] [PubMed] [Google Scholar]
- 34.Newman AB, Gottdiener JS, Mcburnie MA, Hirsch CH, Kop WJ, Tracy R, Walston JD, Fried LP; Cardiovascular Health Study Research Group : Associations of subclinical cardiovascular disease with frailty. J Gerontol A Biol Sci Med Sci 56: M158–M166, 2001 [DOI] [PubMed] [Google Scholar]
- 35.Walston J, McBurnie MA, Newman A, Tracy RP, Kop WJ, Hirsch CH, Gottdiener J, Fried LP; Cardiovascular Health Study : Frailty and activation of the inflammation and coagulation systems with and without clinical comorbidities: Results from the cardiovascular health study. Arch Intern Med 162: 2333–2341, 2002 [DOI] [PubMed] [Google Scholar]
- 36.Xue QL, Bandeen-Roche K, Varadhan R, Zhou J, Fried LP: Initial manifestations of frailty criteria and the development of frailty phenotype in the women’s health and aging study II. J Gerontol A Biol Sci Med Sci 63: 984–990, 2008 [DOI] [PubMed] [Google Scholar]
- 37.Chang SS, Weiss CO, Xue QL, Fried LP: Association between inflammatory-related disease burden and frailty: Results from the Women’s Health and Aging Studies (WHAS) I and II. Arch Gerontol Geriatr 54: 9–15, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chang SS, Weiss CO, Xue QL, Fried LP: Patterns of comorbid inflammatory diseases in frail older women: The women’s health and aging studies I and II. J Gerontol A Biol Sci Med Sci 65: 407–413, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bandeen-Roche K, Seplaki CL, Huang J, Buta B, Kalyani RR, Varadhan R, Xue QL, Walston JD, Kasper JD: Frailty in older adults: A nationally representative profile in the United States. J Gerontol A Biol Sci Med Sci 70: 1427–1434, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McAdams-DeMarco MA, Isaacs K, Darko L, Salter ML, Gupta N, King EA, Walston J, Segev DL: Changes in frailty after kidney transplantation. J Am Geriatr Soc 63: 2152–2157, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McAdams-DeMarco MA, Ying H, Olorundare I, King EA, Haugen C, Buta B, Gross AL, Kalyani R, Desai NM, Dagher NN, Lonze BE, Montgomery RA, Bandeen-Roche K, Walston JD, Segev DL: Individual frailty components and mortality in kidney transplant recipients. Transplantation 101: 2126–2132, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fine JP, Gray RJ: A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94: 496–509, 1999 [Google Scholar]
- 43.Kobashigawa J, Dadhania D, Bhorade S, Adey D, Berger J, Bhat G, Budev M, Duarte-Rojo A, Dunn M, Hall S, Harhay MN, Johansen KL, Joseph S, Kennedy CC, Kransdorf E, Lentine KL, Lynch RJ, McAdams-DeMarco M, Nagai S, Olymbios M, Patel J, Pinney S, Schaenman J, Segev DL, Shah P, Singer LG, Singer JP, Sonnenday C, Tandon P, Tapper E, Tullius SG, Wilson M, Zamora M, Lai JC: Report from the American Society of Transplantation on frailty in solid organ transplantation [published online ahead of print December 1, 2018]. Am J Transplant 10.1111/ajt.15198 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.