Introduction
Despite substantial efforts over the last 15 years to increase the proportion of patients starting dialysis with an arteriovenous fistula, 80% of patients with incident ESKD and 20% of patients with prevalent ESKD in the United States still use a central venous catheter (CVC) for vascular access (1). Catheter-related bloodstream infection (CRBSI) is the most serious complication in patients on hemodialysis with prolonged CVC dependence (2). We describe two patients to illustrate strategies for the diagnosis and treatment of dialysis CRBSI.
Patient 1
A 28-year-old man with HIV infection on antiretroviral therapy and hemodialysis with a tunneled CVC presented to the emergency department with fever (38.8°C), rigors, tachycardia (101 beats per minute), and leukocytosis (12,730 cells per 1 μl). There was no purulence at the CVC exit site. Blood cultures were drawn, and empirical vancomycin and ceftazidime were administered for suspected CRBSI. Symptoms resolved after the initial dose of antibiotics. Blood cultures grew Stenotrophomonas maltophilia sensitive to ceftazidime. After a 3-week course of postdialysis ceftazidime and a ceftazidime catheter lock, surveillance cultures were negative, and the catheter was salvaged.
Patient 2
A 57-year-old woman with hypertension and diabetes on hemodialysis via a tunneled CVC due to multiple failed vascular accesses was hospitalized with fever (38.2°C) and a 1-week history of progressive, severe low-back pain. After blood cultures were obtained, she received empirical vancomycin and ceftazidime for presumed CRBSI. Blood cultures grew methicillin-sensitive Staphylococcus lugdunensis. Ceftazidime was discontinued, and she remained on vancomycin with each dialysis session. Persistent fever and severe back pain prompted computerized tomography, which revealed spondylodiscitis of the T10–T11 and L3–L4 spine. Transthoracic echocardiogram showed no cardiac vegetations. Her fever resolved, repeat blood cultures were negative, and her back pain improved after 1 week. She was discharged home to receive a 6-week course of intravenous vancomycin with dialysis.
Six weeks later she reported poor appetite, weight loss, and difficulty walking. Magnetic resonance imaging showed worsening T10–T11 vertebral destruction and central stenosis. Repeat computerized tomography showed a new vertebral fracture, progressive spondylodiscitis, and a paraspinal abscess at the T11–T12 level, which was treated with surgical debridement. Bone biopsy culture grew S. lugdunensis, but blood cultures remained negative. Intravenous cefazolin was initiated for treatment of the metastatic infection. Over the ensuing 3 months, the patient had recurrent admissions due to severe back pain. She did not develop permanent neurologic sequelae but required extensive rehabilitation, and she never recovered to her baseline functional status. The CVC was maintained until it became dysfunctional 9 months after the initial diagnosis of CRBSI.
Discussion
The risk of CRBSI increases with the duration of CVC dependence. A study of 472 patients initiating hemodialysis with a CVC observed CRBSI in 35%, 54%, and 79% of patients at 3, 6, and 12 months, respectively (3). The risk of CRBSI was not associated with patient age, sex, race, diabetes, vascular disease, heart failure, or CVC laterality. A subsequent study reported that CRBSI was less likely in older patients with a CVC (4). HIV-positive patients are not at increased risk of developing CRBSI compared with HIV-negative patients, but they are more likely to have polymicrobial infections (5).
The clinical presentation of CRBSI is variable, with fever and rigors occurring most frequently. In a series of 184 patients with CRBSI, presenting symptoms consisted of fever (with or without rigors) in 47% and rigors alone in 33%. The remaining 20% had neither fever nor rigors, but they exhibited other findings, such as malaise, encephalopathy, hypotension, or exit site drainage (6). Among patients with suspected CRBSI, blood cultures confirm the diagnosis in 60%–75% of patients. Approximately one third of patients with CRBSI require hospitalization.
The majority (40%–80%) of CRBSIs are caused by a Gram-positive organism, including coagulase-negative Staphylococci, Staphylococcus aureus, and Enterococcus (2). A broad spectrum of Gram-negative bacteria accounts for 20%–30% of patients. Staphylococcal CRBSIs are frequently methicillin resistant. If CRBSI is suspected, empirical antibiotic coverage of both Gram-positive and Gram-negative organisms with vancomycin and ceftazidime should be initiated promptly after blood cultures have been obtained (2). Peripheral blood cultures are frequently impractical in patients on dialysis; blood cultures obtained from the dialysis circuit or catheter lumen are an acceptable alternative (7).
The severity of presentation and clinical consequences of CRBSI are related to the infecting organism. In one large series, hospitalization for CRBSI was required in 53% of patients with S. aureus infection, 30% of those with Enterococcus, 23% of those with Staphylococcus. epidermidis, and only 17% of those with a Gram-negative bacteria (6). Septic shock and metastatic infections were rare complications, most often observed in patients with S. aureus CRBSI. In another study of 113 patients with S. aureus CRBSI, 10% developed metastatic infection, including endocarditis, osteomyelitis, or septic arthritis (8). Notably, these complications occurred almost exclusively in patients whose fever persisted 48 hours after antibiotic initiation. In a subsequent series of 64 patients with Enterococcus CRBSI, metastatic infection occurred in only 6% (9).
Uncomplicated CRBSI
Our first patient responded quickly to systemic antibiotics and did not develop metastatic infection. For uncomplicated CRBSI, 2–3 weeks (4 weeks for S. aureus) of systemic antibiotics tailored to the reported sensitivities are generally sufficient to treat the infection. Adjuvant antibiotic lock with the same antibiotic may be used to eradicate catheter biofilm and permit effective clearance of the organism while allowing for salvage of the CVC.
Complicated CRBSI
Our second patient developed metastatic infection from S. lugdunensis, a unique coagulase-negative Staphylococci with virulence similar to that of S. aureus, and it is always considered a pathogen. Treatment of complicated CRBSI with sepsis, persistently positive blood cultures, or metastatic infection (e.g., endocarditis, septic arthritis, epidural abscess, or osteomyelitis) requires a longer course of antibiotics (6–8 weeks) compared with uncomplicated CRBSI; β-lactams (bactericidal) are superior to vancomycin (bacteriostatic) for treating methicillin-sensitive S. aureus infections and should be given preferentially, especially in patients with metastatic infection (10). Experts recommend catheter removal in the setting of hemodynamic instability, candidemia, resistant microorganisms, or metastatic infections (5%–10% of patients) (2). Catheter exchange with creation of a new tunnel if there is evidence of exit site infection is a reasonable alternative to catheter removal in certain patients needing to preserve the catheter site due to limited vascular access options. In the second patient, the patient should have been treated with a β-lactam on first diagnosis on the basis of culture sensitivities; likewise, the catheter should have been removed or exchanged after she was found to have a metastatic infection. An earlier orthopedic intervention may have also helped.
Conclusions
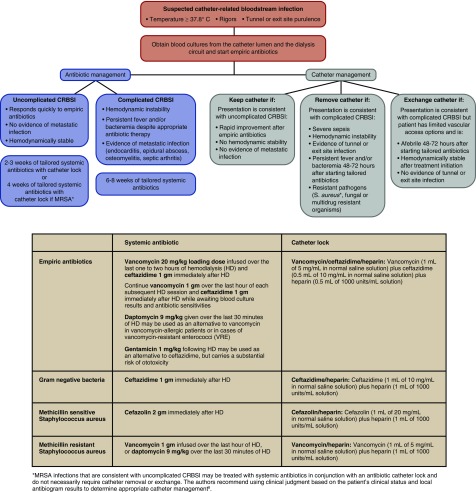
CRBSI is a frequently encountered complication of hemodialysis catheters. The likelihood of developing CRBSI at just 6 months of catheter use exceeds 50%. Although complicated CRBSI is relatively rare, hospitalization, infectious disease consultation, a search for metastatic complications, and a systematic treatment strategy minimize the risk of severe and potentially life-threatening consequences (Figure 1). After blood cultures have been obtained from a patient with suspected CRBSI, initial therapy should include broad spectrum antibiotic coverage until blood culture growth and sensitivities are available. A relatively short (2–3 week) course of tailored systemic antibiotics with an adjuvant antibiotic catheter lock is reasonable in uncomplicated CRBSI. A longer (6–8 week) course of tailored antibiotic therapy with catheter removal or exchange is more appropriate in patients with complicated CRBSI.
Figure 1.
Recommended algorithm for the diagnosis and treatment of dialysis catheter-related bloodstream infections (CRBSIs). MRSA, Methicillin-sensitive Staphylococcus aureus; S. aureus, Staphylococcus aureus.
Disclosures
None.
Acknowledgments
C.A.F. is supported by grant T32 DK007545-31 from the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK). M.A. is supported by grant 1R21DK104248-01A1 from the NIDDK.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
References
- 1.United States Renal Data System: USRDS 2017 Annual Data Report, Vol. 2, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease, 2017 [Google Scholar]
- 2.Allon M: Dialysis catheter-related bacteremia: Treatment and prophylaxis. Am J Kidney Dis 44: 779–791, 2004 [PubMed] [Google Scholar]
- 3.Shingarev R, Barker-Finkel J, Allon M: Natural history of tunneled dialysis catheters placed for hemodialysis initiation. J Vasc Interv Radiol 24: 1289–1294, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Murea M, James KM, Russell GB, Byrum GV 3rd, Yates JE, Tuttle NS, Bleyer AJ, Burkart JM, Freedman BI: Risk of catheter-related bloodstream infection in elderly patients on hemodialysis. Clin J Am Soc Nephrol 9: 764–770, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mitchell D, Krishnasami Z, Allon M: Catheter-related bacteraemia in haemodialysis patients with HIV infection. Nephrol Dial Transplant 21: 3185–3188, 2006 [DOI] [PubMed] [Google Scholar]
- 6.Al-Solaiman Y, Estrada E, Allon M: The spectrum of infections in catheter-dependent hemodialysis patients. Clin J Am Soc Nephrol 6: 2247–2252, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quittnat Pelletier F, Joarder M, Poutanen SM, Lok CE: Evaluating approaches for the diagnosis of hemodialysis catheter-related bloodstream infections. Clin J Am Soc Nephrol 11: 847–854, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maya ID, Carlton D, Estrada E, Allon M: Treatment of dialysis catheter-related Staphylococcus aureus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis 50: 289–295, 2007 [DOI] [PubMed] [Google Scholar]
- 9.Peterson WJ, Maya ID, Carlton D, Estrada E, Allon M: Treatment of dialysis catheter-related Enterococcus bacteremia with an antibiotic lock: A quality improvement report. Am J Kidney Dis 53: 107–111, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim SH, Kim KH, Kim HB, Kim NJ, Kim EC, Oh MD, Choe KW: Outcome of vancomycin treatment in patients with methicillin-susceptible Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 52: 192–197, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]