ABSTRACT
Background: Narrative exposure therapy (NET) is a short-term psychological treatment for post-traumatic stress disorder (PTSD) that has been investigated in various contexts among traumatized refugees and other trauma survivors. Sustained treatment results have been reported, but the methodological quality of the trials needs a more thorough examination.
Objective: To evaluate the effectiveness of NET for survivors of trauma, using a quality assessment, an updated meta-analysis, and a meta-regression analysis.
Method: Following a systematic literature selection, the methodological quality of the included studies was assessed; Non-controlled and controlled effect sizes (Hedges’ g) were estimated using a random effects model. Predictor analyses were performed. Non-controlled effect sizes for PTSD and depression included symptom change at post-treatment and follow-up time-points. Controlled effect sizes included post-treatment comparisons of NET with non-active and active comparators: both trauma-focused (TF) and non-trauma-focused (non-TF) interventions.
Results: The selected studies showed high external validity; methodological quality was equivalent to other guideline-supported TF interventions. In 16 randomized controlled trials, involving 947 participants, large non-controlled effect sizes were found for PTSD symptoms, at post-treatment (g = 1.18, 95% confidence interval [0.87; 1.50]) and follow-up (g = 1.37 [0.96; 1.77]). For depression symptoms, medium non-controlled effect sizes were found, at post-treatment (g = 0.47 [0.23; 0.71]) and follow-up (g = 0.60 [0.26; 0.94]). Post-treatment, NET outperformed non-active comparators and non-TF active comparators for PTSD, but not the combined active comparators. For depression, NET only outperformed non-active comparators. Advancing age predicted better treatment results for PTSD and depression symptoms; a history of migration predicted smaller treatment results for depression symptoms.
Conclusions:The findings of this meta-analysis suggest that patients and providers may expect sustained treatment results from NET. Controlled comparisons with other guideline-supported TF interventions are not yet available.
KEYWORDS: Intervention, meta-analysis, narrative exposure therapy, NET, post-traumatic stress disorder, PTSD, treatment
HIGHLIGHTS
• Narrative exposure therapy is effective in post-traumatic stress disorder symptom reduction at post-treatment (g = 1.18) and follow-up (g = 1.37).• Treatment results are better for older adults.• Controlled comparisons with other guideline-supported trauma-focused interventions are not yet available.
Abstract
Antecedentes: la terapia de exposición narrativa (NET en sus siglas en inglés) es un tratamiento psicológico a corto plazo para el trastorno de estrés postraumático (TEPT) que ha sido investigado en diversos contextos entre refugiados traumatizados y otros sobrevivientes de traumas. Se han informado resultados sostenidos del tratamiento, pero la calidad metodológica de los ensayos requiere un examen más exhaustivo.
Objetivo: evaluar la efectividad de la NET para sobrevivientes de trauma, mediante una evaluación de la calidad, un metanálisis actualizado y un análisis de metarregresión.
Método: después de una selección sistemática de la literatura, se evaluó la calidad metodológica de los estudios incluidos; se estimaron los tamaños del efecto no controlados y controlados (g de Hedges), utilizando un modelo de efectos aleatorios. Se realizaron análisis predictivos. Los tamaños del efecto no controlados para el TEPT y la depresión incluyeron el cambio de los síntomas en los puntos de tiempo del postratamiento y del seguimiento. Los tamaños de los efectos controlados incluyeron las comparaciones postratamiento de la NET con comparadores no activos y activos: ambas intervenciones centradas en el trauma (TF en su sigla en inglés) y no enfocadas en el trauma (no TF).
Resultados: la calidad metodológica de los estudios incluidos varió de incierto a alto riesgo de sesgo. En los 16 ensayos controlados aleatorios (ECA), con 947 participantes, se encontraron tamaños grandes de efectos no controlados para los síntomas del TEPT, en el postratamiento (g = 1.18, intervalo de confianza del 95% [0.87; 1.50]), y el seguimiento (g = 1.37, [0.96; 1.77]). Para los síntomas de depresión, se encontraron tamaños medios de efectos no controlados: en el postratamiento (g = 0.47, [0.23; 0.71]) y el seguimiento (g = 0.60, [0.26; 0.94]). En los postratamientos, la NET superó a los comparadores no activos y los comparadores no TF activos para el TEPT, pero no a los comparadores activos combinados. Para la depresión, la NET solo superó a los comparadores no activos. La edad avanzada predijo mejores resultados de tratamiento para el TEPT y los síntomas de depresión; un historial de migración predijo resultados de tratamiento más pequeños para los síntomas de depresión.
Conclusiones: los hallazgos de este metanálisis sugieren que los pacientes y los proveedores pueden esperar resultados sostenidos del tratamiento de la NET. Hasta ahora, no se dispone de comparaciones controladas con otras intervenciones apoyadas por la guía de intervenciones de TF.
PALABRAS CLAVES: Intervencion, metanalisis, Terapia de exposicion narrativa, NET, Trastorno de Estrés Postraumatico, TEPT, Tratamiento
Abstract
背景:叙事暴露疗法(NET)是一种用于创伤后应激障碍(PTSD)的短期心理治疗方法,已在受创伤难民和其他创伤幸存者的各种背景下进行了考察。前人报告了持续治疗结果,但试验的方法学质量需要更彻底的检查。
目的:用质量评估、更新的元分析和元回归分析评估NET对创伤幸存者的有效性。
方法:在系统地选择文献后,对纳入的研究进行方法学质量评估;使用随机效应模型估计了未控制和经控制后的效应量(Hedges’g),并进行了预测指标分析。创伤后应激障碍和抑郁症的非控制效应大小包括治疗后和随访期的症状变化。控制效应量包括NET与非主动(non-active )和 主动(acitive)疗法的治疗后比较(创伤中心(TF)和非创伤中心(非TF)干预)。
结果:所纳入研究显示出高外部效度;方法学质量和其他有指南指导的TF疗法相当。在16项随机对照试验(RCT)中,包括947名被试。结果发现,PTSD症状的非控制效应量较大:治疗后(g = 1.18, 95%置信区间[0.87; 1.50])和随访期(g = 1.37, [0.96; 1.77])。对于抑郁症状,发现非控制效应量大小中等:治疗后(g = 0.47,[0.23; 0.71])和随访期(g = 0.60,[0.26; 0.94])。治疗后,NET表现优于PTSD的非主动疗法和非TF的主动疗法,但没有优于组合后的主动疗法。对于抑郁症,NET仅优于非主动疗法。年龄的增加预测创伤后应激障碍和抑郁症状的治疗效果会更好;迁移史预测抑郁症状的治疗效果更小。
结论:这项元分析的结果表明,患者和提供者或可以预期NET的持续疗效。目前尚无法与有指南支持的TF干预进行对照比较。
关键词: 干预, 元分析, 叙事暴露疗法, NET, 创伤后应激障碍, PTSD, 治疗
1. Introduction
Current geopolitical developments and worldwide migration crises stress the urgency of providing effective treatment to trauma-exposed refugees. Narrative exposure therapy (NET) (Schauer, Neuner, & Elbert, 2011), a short-term trauma-focused cognitive behaviour therapy (TFCBT), has been investigated with populations from different cultural and ethnic backgrounds (Palic & Elklit, 2011). These studies have primarily involved refugees and displaced persons with post-traumatic stress disorder (PTSD) (American Psychiatric Association [APA], 2000, 2013) from non-Western countries.
PTSD is a serious and demoralizing mental health disorder, burdening adaptation and development (McEwen, 2012). Prevalence rates range widely, from 2.7% in population surveys (Hauffa et al., 2011) to 30.6% among refugees worldwide (Steel et al., 2009). PTSD and depression frequently co-occur (Rytwinski, Scur, Feeny, & Youngstrom, 2013; Steel et al., 2009). Treatment guidelines recommend trauma-focused (TF) psychological treatment for PTSD (American Psychological Association [APA], 2017; National Institute for Clinical Excellence [NICE], 2005).
1.1. Narrative exposure therapy
NET is a standardized form of TF psychotherapy, embedding trauma exposure in an autobiographical context. The manual (Schauer et al., 2011) recommends four to 12 sessions of 90 minutes, depending on the number of traumatic events, and treatment focuses on imaginary trauma exposure and on reorganizing memories (Schnyder et al., 2015). Memories of traumatic events are hypothesized to form multiple fear networks dominated by sensory–perceptual information and lacking autobiographical information (Schauer et al., 2011). By connecting these anxiety-provoking implicit memories with episodic context, the autobiographic memory is rebuilt, allowing for reduction of anxiety (Schauer et al., 2011).
In NET, the therapist and the patient create a timeline of the patient’s life, followed by chronologically elaborating this timeline in subsequent sessions. At the end of therapy, the patient receives the written narrative as a documented testimony. Given its focus on the lifespan, NET is particularly suited to populations affected by multiple traumatic experiences (Schauer et al., 2011).
1.2. Research in context
Review findings indicated medium to large non-controlled effect sizes for NET with refugees and displaced persons (Gwozdziewycz & Mehl-Madrona, 2013; Lambert & Alhassoon, 2015; Robjant & Fazel., 2010), even in extremely insecure living conditions. Treatment gains for PTSD symptoms and comorbid disorders were found to be stable at follow-up. Treatment dropout was low (Mørkved et al., 2014), and provision of the intervention by trained counsellors was found to be feasible (Gwozdziewycz & Mehl-Madrona, 2013). Controlled effect sizes have been found to be in line with those of other guideline-supported interventions (Cusack et al., 2016; Watts et al., 2013). The methodological quality of the NET trials, however, has been questioned (Bisson, Roberts, Andrew, Cooper, & Lewis, 2013; Mundt, Wünsche, Heinz, & Pross, 2014; Patel, Kellezi, & Williams, 2014). These doubts suggest that the findings need more thorough investigation.
In the review literature on NET, some serious omissions were found. Some reviews were merely descriptive (Robjant & Fazel, 2010), while some were exclusively focused on low-resource settings (Mundt et al., 2014) or survivors of torture (Patel et al., 2014). Some missed important trials (Bisson et al., 2013; Patel et al., 2014) and others lacked information on comorbid depressive symptoms (Gwodzdziewizc & Mehl-Madrona, 2013) or follow-up effects (Lambert & Alhassoon, 2015). As yet, no PTSD guideline-supported comparators have been found (Gerger, Munder, & Barth, 2014; Nosè et al., 2017). Meanwhile, new NET trials have been added to the evidence base of NET, calling for evaluation.
In the current study, these gaps in the literature were addressed and several clinically important moderators were examined as predictors of treatment outcome (e.g. advancing age, gender, migration to Western countries, treatment dose, self-report assessments, language matching between participants and therapists, and the influence of providing NET by trained counsellors). In exposure treatment, participants’ advancing age was found to be associated with larger effects (Rizvi, Vogt, & Resick, 2009). Psychotherapy studies with more women were also found to have larger effects (Stenmark, Guzey, Elbert, & Holen, 2014; Tarrier, Sommerfield, Pilgrim, & Faragher, 2000; Watts et al., 2013). Migration to Western countries, leading to potential post-migration stressors (Li, Liddell, & Nickerson, 2016), may complicate treatment progression. A higher number of sessions was found to predict higher treatment effects (Lambert & Alhassoon, 2015). Treatment dose, capturing session length as well (Mørkved et al., 2014), has not yet been examined as a predictor. Contrasting findings existed for the influence of self-reported PTSD symptoms versus diagnostic interviews (Bisson et al., 2013; Lambert & Alhassoon, 2015) and language matching between participants and therapists (Dossa & Hatem, 2012; Lambert & Alhassoon, 2015; Nickerson, Bryant, Silove, & Steel, 2011; Patel et al., 2014). Finally, updating the evidence on the effectiveness of paraprofessional counsellors (Gwozdziewycz & Mehl-Madrona, 2013) was considered relevant.
1.3. Aims and hypotheses
The first aim of the present study was to assess the efficacy of NET in adults, as both non-controlled and controlled effect sizes. The second aim was to critically assess the methodological quality of the current evidence on NET and to inform clinicians about treatment outcome predictors, facilitating optimization of treatment response. PTSD and depression outcomes have been included, as have post-treatment and follow-up assessments. Comparisons included non-active and active (both non-TF and TF) comparators, followed by a meta-regression analysis of the moderators described above.
Consistent with meta-analytic findings, the methodological quality of the evidence was expected to be modest. NET was expected to show medium to large and sustained treatment effects regarding PTSD and depression outcomes. In addition, NET was expected to outperform non-active and active non-TF comparators for PTSD outcomes (Lambert & Alhassoon, 2015). According to direct comparisons of TF interventions (Brom, Kleber, & Defares, 1989; Nijdam, Gersons, Reitsma, De Jongh, & Olff, 2012; Ter Heide, Mooren, Van de Schoot, De Jongh, & Kleber, 2016), no significant differences were expected comparing NET with all active control conditions (non-TF and TF comparators). Finally, advancing age and female gender were hypothesized to predict larger treatment effects, while having migrated to Western countries was hypothesized to predict lower treatment effects. A higher treatment dose, self-reported PTSD symptoms, counsellors, and language matching were hypothesized to predict larger treatment effects.
2. Method
2.1. Search strategy and data sources
The literature search was conducted independently by the first author and a senior librarian. The search conformed to the Meta-Analysis Reporting Standards (MARS) guidelines (American Psychological Association [APA], 2010) and OvidSP software (2010) was used. The searched internet databases included the ACP Journal Club, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Database of Abstracts of Reviews of Effects, Health Technology Assessment, National Health Service Economic Evaluation Database, Ovid MEDLINE(R), Ovid MEDLINE(R) in-Process, Ovid MEDLINE(R) Daily Update, Psych INFO, and Published International Literature On Traumatic Stress (PILOTS). Trials published between 1 January 2004 (the first NET trial being published in 2004) and 30 April 2018 were included, and no language restrictions were applied. Search terms in titles and abstracts were: (‘narrative exposure therapy’ OR ‘NET’) AND (‘posttraumatic stress disorder’ OR ‘PTSD’) AND (‘treatment’ OR ‘intervention’). Additional studies were identified by cross-referencing.
2.2. Inclusion criteria and selection of studies
The search strategy targeted independent randomized controlled trials (RCTs) investigating NET outcomes (NET and its brief version, NET-R) compared with TF or non-TF comparators. Studies had to report at least one quantitative measure of PTSD assessed both pre- and post-treatment, and intention-to-treat analyses had to be applied.
2.3. Data extraction and coding
The included interventions were coded as NET or NET-R. Comparators were coded as active or non-active, and TF or non-TF interventions. If a trial included more than one comparison, the most active comparator was selected. PTSD outcome assessments were coded as diagnostic interviews or self-report instruments. Post-treatment and last follow-up effect sizes were computed. Treatment dropout indicated the percentage of participants leaving treatment prematurely. Inter-assessment correlations were obtained from the authors for all studies except for one trial. For that study, the averaged correlations of the other studies were included.
2.4. Quality appraisal
All studies were appraised using the Cochrane Collaboration’s tool for assessing risk of bias (Higgins et al., 2011), focusing on six domains threatening internal validity: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting and other bias. The risk of bias of each domain was judged as high, low, or unclear. Consistent with the GRADE framework (Higgins et al., 2011), for each study, the highest risk of bias was considered to determine the quality. Two independent assessors (the first author and a research assistant) agreed on 94% of the resulting scores, and remaining inconsistencies were resolved by a third independent assessor (the fourth author).
2.5. Data synthesis
2.5.1. Heterogeneity
To evaluate heterogeneity in the outcomes, Cochrane’s heterogeneity statistic (Q) was computed and tested for significance.
2.5.2. Effect size calculation
First, non-controlled (within-group) effect sizes were computed for the NET groups and control groups (post-treatment and last follow-up, the latter indicated as ‘follow-up’). In addition, the post-treatment effect sizes for NET were grouped according to the participants’ backgrounds. Secondly, controlled (between-groups) effect sizes were computed. All effect sizes were calculated in Hedges’ g. Positive signs indicated symptom reduction or treatment groups outperforming comparators.
2.5.3. Meta-analytic techniques
Effect sizes (random effects model) were computed using the Comprehensive Meta-Analysis program (CMA; version 2.0, 2005). All effect sizes were computed for PTSD outcomes and, if available, for depression outcomes. Publication bias, meaning preferential publication of striking findings, was evaluated by inspecting the funnel plots as implemented in CMA and using Egger’s test of the intercept to evaluate the significance of the bias. The random effects version of Duval and Tweedie’s trim-and-fill procedure (2000), as implemented in CMA, was used to estimate adjustments for the possible effects of publication bias. Finally, in a sensitivity analysis, each study was consecutively removed as a potential outlier to test its influence on the overall effect sizes.
2.6. Meta-regression analyses
Multiple regression analyses were performed to examine the effect of moderators on outcomes. SPSS version 23 (IBM Corp., Armonk, NY, USA), was used, with macros provided by Lipsey and Wilson (2001). For all analyses, the alpha level was set at p = .05. PTSD and depression symptom change at post-treatment were used as dependent variables. Seven potential predictors were specified as independent variables: age (sample mean), female gender (sample percentage), migration (1 = yes, 0 = no), treatment dose (number of sessions by session length, yielding total treatment time in minutes), matching languages (1 = yes, 0 = no), PTSD outcome (1 = diagnostic interview, 0 = self-report) and, finally, therapist’s training being professional or paraprofessional (1 = professional, 0 = paraprofessional). All variables were entered in the model at once. The contribution of all variables to the explained variance was evaluated by calculating R2.
3. Results
3.1. Study selection
From 182 eligible studies, 16 RCTs (denoted as k) were selected for the meta-analysis, using several steps. A primary search was conducted in July 2015 and repeated in January 2016; a secondary search was conducted in July 2016 and confirmed in September 2018. The selection process is presented in Figure 1.
Figure 1.
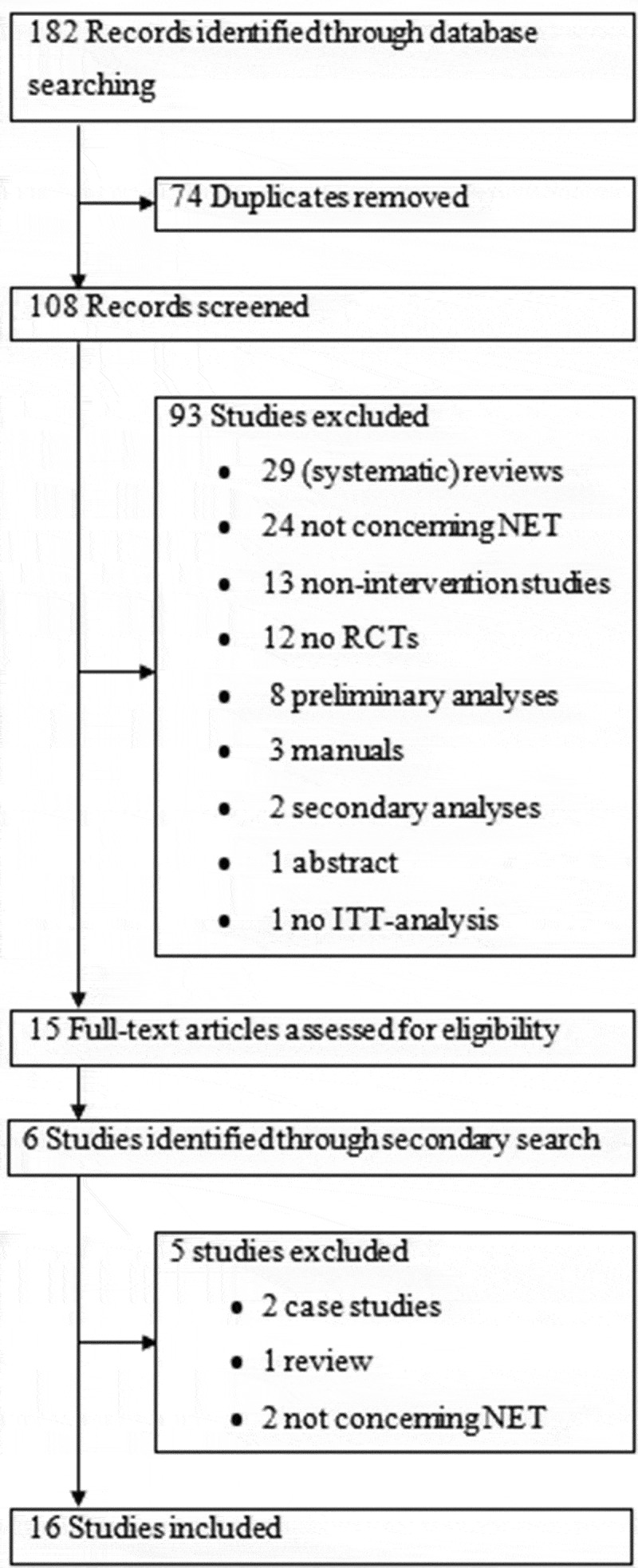
Selection of studies. NET, narrative exposure therapy; RCT, randomized controlled trial; ITT, intention-to-treat.
3.2. Study characteristics
As one study (Zang, Hunt, & Cox, 2014) included two comparisons (for NET and NET-R), the selection included 16 trials with 17 comparisons. Most NET samples (k = 13, 76.47%) were small, ranging from five to 29 participants; a minority (k = 4, 23.52%) ranged from 38 to 111 participants. Characteristics of the trials are listed in Table 1.
Table 1.
Characteristics of the included studies.
| Study name | N NET | Age | Male participants (%) | Treatment dose | Professionals | Outcome | Language | Migration | Dropout NET | Control |
|---|---|---|---|---|---|---|---|---|---|---|
| Alghamdi et al. 2015 | 17 | 28.7 | 100.00 | 360 | 1 | SR* | 1 | 0 | 0.00 | WLC* |
| Al-Hadethe et al. 2015 | 20 | 17.5 | 100.00 | 300 | 1 | SR | 1 | 0 | 0.05 | EFT* |
| Bichescu et al. 2007 | 9 | 68.9 | 100.00 | 600 | 1 | DI* | 1 | 0 | 0.00 | PED* |
| Ertl et al. 2011 | 29 | 18.66 | 44.8 | 840 | 0 | DI | 1 | 0 | 10.34 | Catch-up* |
| Hensel-Dittmann et al. 2011 | 15 | 36.4 | 57.14 | 900 | 1 | DI | 0 | 1 | 20.00 | SIT* |
| Hijazi et al. 2014 | 41 | 47.6 | 36.59 | 225 | 1 | SR | 1 | 1 | 4.88 | WLC |
| Jacob et al. 2014 | 38 | 40.0 | 10.53 | 960 | 0 | DI | 1 | 0 | 2.63 | WLC |
| Morath et al. 2014a | 17 | 27.29 | 58.82 | 1080 | 1 | DI | 0 | 1 | 0,00 | WLC |
| Morath et al. 2014b | 19 | 28.7 | 67.65 | 1080 | 1 | DI | 0 | 1 | 21.05 | WLC |
| Neuner et al. 2004 | 17 | 31.9 | 41.18 | 420 | 1 | SR | 0 | 0 | 5.88 | SC* |
| Neuner et al. 2008 | 111 | 34.4 | 49.55 | 540 | 1 | SR | 1 | 0 | 3.6 | TC* |
| Neuner et al. 2010 | 16 | 31.6 | 68.75 | 1055 | 1 | SR | 0 | 1 | 12.5 | TAU |
| Schaal et al. 2009 | 12 | 19.42 | 38.46 | 540 | 1 | DI | 0 | 0 | 0.00 | IPT* |
| Stenmark et al. 2013 | 51 | 34.51 | 66.67 | 900 | 1 | DI | 0 | 1 | 25.49 | TAU |
| Zang et al. 2013 | 11 | 56.64 | 22.72 | 360 | 1 | SR | 1 | 0 | 0.00 | WLC |
| Zang et al. 2014, NET* 2014 | 10 | 53.5 | 6.67 | 300 | 1 | SR | 1 | 0 | 0.00 | WLC |
| Zang et al. 2014, NET-R* 2014 | 10 | 56.5 | 6.67 | 270 | 1 | SR | 1 | 0 | 0.00 | WLC |
*Catch-up, academic catch-up programme; DI, diagnostic interview; EFT, emotional freedom techniques; IPT, interpersonal psychotherapy; NET, narrative exposure therapy; NET-R, NET – revised; PED, psychoeducation; TC, Trauma Counselling; SC, supportive counselling; SIT, stress inoculation training; SR, self-report; TAU, treatment as usual; WLC, waiting-list conditions.
3.3. Methodological quality
In most studies, the risk of bias was rated as unclear. In one study, the risk of bias was rated as high. With respect to blinding and allocation concealment, no evidence was reported that violation affected outcomes. Five studies (31%) were conducted by authors who were not involved in the development of NET.
The quality assessment data are included in Figure 2.
Figure 2.
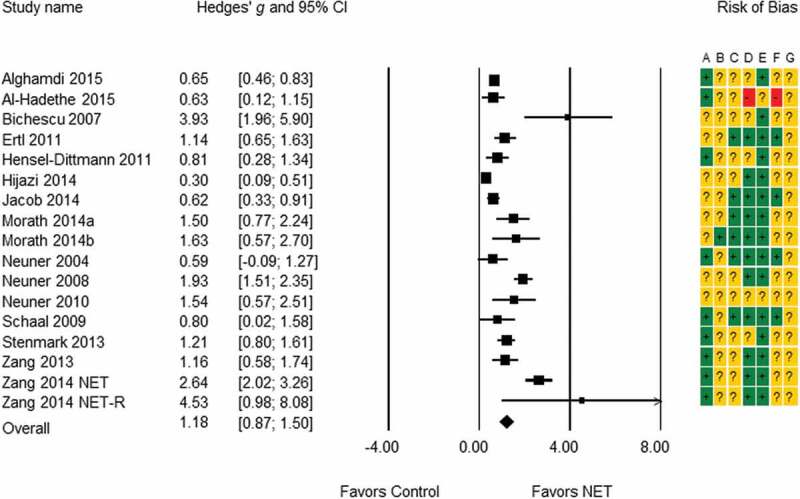
Mean effect sizes of narrative exposure therapy (NET) Hedges’ g [95% confidence interval]. Risk of Bias: A, random sequence generation; B, allocation concealment; C, blinding of participants and personnel; D, blinding of outcome assessment; E, incomplete outcome data; F, selective reporting; G, other bias. Ratings: +, low; ?, unclear; -, high.
3.4. Participants
The selected studies involved 947 individuals in nine countries; 443 (46.78%) participants were offered a NET intervention; 294 (31.05%) participated in an active control intervention, and 210 (22.18%) participated in a non-active control condition. Participants included adults (81.94%) and adolescents (18.06%); 456 participants (48.15%) were female. Mean age ranged from 17.50 to 68.90 years (M = 37.01, SD = 14.97). Eleven studies (68.75%) involved refugees or displaced persons, identified as refugees, including 783 ethnically diverse participants. Five studies (31.25%), involving 507 participants, were conducted in low-income regions (Ertl, Pfeiffer, Schauer, Elbert, & Neuner, 2011; Jacob, Neuner, Maedl, Schaal, & Elbert, 2014; Neuner et al., 2008; Neuner, Schauer, Klaschik, Karunakara, & Elbert, 2004; Schaal, Elbert, & Neuner, 2009). Six studies (37.50%), with 276 participants, involved migrated refugees or asylum seekers (identified as refugees as well) in Western countries (Hensel-Dittmann et al., 2011; Hijazi et al., 2014; Morath et al., 2014a, 2014b; Neuner et al., 2010; Stenmark, Catani, Neuner, Elbert, & Holen, 2013). All refugee studies included participants surviving multiple traumatic events or torture, the mean number ranging from 6.82 (SD = 2.09) to 19.85 (SD = 6.4). Consequently, those populations may be characterized by high problem complexity (Gerger et al., 2014). Finally, five studies (31.25%), including 164 individuals, involved non-refugee participants (Alghamdi, Hunt, & Thomas, 2015; Al Hadethe, Hunt, Al-Qaysi, & Thomas, 2015; Bichescu, Neuner, Schauer, & Elbert, 2007; Zang, Hunt, & Cox, 2013; Zang et al., 2014). Three of those studies (Alghamdi et al., 2015; Bichescu et al., 2007; Zang et al., 2013) reported multiple traumatic events as well.
3.5. Interventions
The mean number of sessions was 6.47 (SD = 3.17, range 3–12), mean session length was 97.06 minutes (SD = 17.68, range 75–135), and mean treatment dose was 631.18 minutes (SD = 316.51, range 225–1080).
3.6. Comparators
Comparators included non-active (k = 9; 56.25%) and active interventions (k = 8; 47.06%). The non-active comparators consisted of waiting lists. The active comparators included one intervention that could be considered TF (Neuner et al., 2008) and one study in which NET was compared with another TF intervention (Al Hadethe et al., 2015). The other active comparators included diverse psychosocial interventions. All comparators are listed in Table 1.
3.7. Outcomes
All studies reported group means; in addition, three studies reported individual change and eight studies reported remission of PTSD diagnosis. All studies reported reasons for dropout. In five studies, incidents of symptom increase were reported, with no indication of more adverse events among NET participants than in the control group being apparent. In one study, a suicide took place during follow-up in the control condition. None of the adverse events was attributed to treatment stress.
PTSD and depression severity were monitored with well-accepted diagnostic instruments. Time-points of post-treatment measurements varied from 2 to 26 weeks (M = 9.55, SD = 8.26). Time-points of the last follow-up measurements ranged from 9 to 52 weeks (M = 35.57, SD = 17.38). Treatment dropout from NET ranged from 0.00% to 25.49% (M = 5.85%, SD = 8.51%), whereas treatment dropout from the comparators ranged from 0.00% to 26.67% (M = 7.11%, SD = 9.56%).
3.8. Treatment effects
3.8.1. Effect sizes
For PTSD, the non-controlled effect sizes were found to be large at post-treatment (g = 1.18, 95% confidence interval [CI] [0.87; 1.50]) and sustained at follow-up (g = 1.35 [0.93; 1.77]). Controlled effect sizes for all active comparators (both TF and non-TF) were non-significant. For active non-TF comparators, controlled effect sizes were medium and significant (g = 0.43 [0.09; 0.78]); for non-active comparators, they were large and significant (g = 1.37 [0.66; 2.07]).
For depression, the non-controlled effect sizes were found to be medium at post-treatment (g = 0.47 [0.23; 0.71]) and sustained at follow-up (g = 0.60 [0.26; 0.94]). Controlled effect sizes for all active comparators (both TF and non-TF) were non-significant, and the same applied for active non-TF comparators. For non-active comparators, controlled effect sizes were medium to large and significant (g = 0.79 [0.48; 1.09]). The resulting effect sizes are presented in Table 2 and Figure 2.
Table 2.
Mean effect sizes of narrative exposure therapy (NET) on post-traumatic stress disorder (PTSD) and depression outcomes, in Hedges’ g.
| Effect sizes |
Heterogeneity |
|||||||
|---|---|---|---|---|---|---|---|---|
| k | Mean | −95% CI* | 95% CI | p- value | Q* | df* | p- value | |
| PTSD | ||||||||
| Non-controlled effect sizes | ||||||||
| Pre- to post-treatment | 17 | 1.18 | 0.87 | 1.50 | .000 | 117.41 | 16 | .000 |
| Pre-treatment to last follow-up | 15 | 1.35 | 0.93 | 1.77 | .000 | 94.77 | 14 | .000 |
| Controlled effect sizes | ||||||||
| All active comparators | 9 | 0.24 | −0.10 | 0.58 | .166 | 25.24 | 8 | .001 |
| Active non-TF comparators | 7 | 0.43 | 0.09 | 0.78 | .014 | 11.65 | 6 | .070 |
| Non-active comparators | 8 | 1.37 | 0.66 | 2.07 | .000 | 50.96 | 7 | .000 |
| All comparators | 17 | 0.69 | 0.33 | 1.06 | .000 | 92.33 | 16 | .000 |
| Depression | ||||||||
| Non-controlled effect sizes | ||||||||
| Pre- to post-treatment | 13 | 0.47 | 0.23 | 0.71 | .000 | 40.63 | 12 | .000 |
| Pre-treatment to last follow-up | 11 | 0.60 | 0.26 | 0.94 | .001 | 46.68 | 10 | .000 |
| Controlled effect sizes | ||||||||
| All active comparators | 7 | 0.17 | −0.31 | 0.64 | .497 | 22.70 | 6 | .001 |
| Active non-TF comparators | 6 | 0.33 | −0.05 | 0.70 | .088 | 9.84 | 5 | .080 |
| Non-active comparators | 6 | 0.79 | 0.48 | 1.09 | .000 | 5.47 | 5 | .361 |
| All comparators | 13 | 0.49 | 0.15 | 0.82 | .004 | 35.57 | 12 | .000 |
*Note.CI, confidence interval; Q, Cochrane’s heterogeneity statistic; df, degrees of freedom. All active comparators: Trauma focused comparators (Emotional Freedom Techniques and Trauma Counselling) plus active non-TF comparators; Active non trauma focused (non-TF) comparators, Academic Catch-up Programme; Interpersonal Psychotherapy; Psychoeducation; Stress Inoculation Training; Supportive Counselling, and Treatment as Usual. Non-active comparators, waiting list conditions.
To take into account the participants’ backgrounds, the mean non-controlled effect sizes at post-test were grouped with respect to refugees in their home regions (g = 1.03 [0.47; 1.60]), refugees in Western countries (g = 1.07 [0.55; 1.60]), and non-refugees (g = 1.66 [0.83; 2.48]). The mean numbers of participants in these subgroups were 41.40, 26.50, and 12.83, respectively. Finally, the non-controlled effect sizes of the comparators are presented in Table 3.
Table 3.
Mean non-controlled effect sizes of the comparators in Hedges’ g (g = 0.02 small; g = 0.05 medium; g = 0.08 large) (Cohen, 1992).
| Effect sizes |
Heterogeneity |
|||||||
|---|---|---|---|---|---|---|---|---|
| k | Mean | −95% CI* | 95% CI | p-value | Q* | df* | p-value | |
| All comparators | ||||||||
| PTSD* pre–post | 17 | 0.77 | 0.41 | 1.12 | .000 | 162.81 | 16 | .000 |
| PTSD pre–FU* | 12 | 1.08 | 0.55 | 1.62 | .000 | 95.48 | 11 | .000 |
| Depression pre–post | 13 | 0.34 | 0.08 | 0.59 | .010 | 43.18 | 12 | .000 |
| Depression pre–FU | 9 | 0.67 | 0.26 | 1.12 | .002 | 37.07 | 8 | .000 |
| Active comparators | ||||||||
| PTSD pre–post | 8 | 0.69 | 0.22 | 1.16 | .004 | 39.24 | 7 | .000 |
| PTSD pre–FU | 5 | 0.57 | −0.17 | 1.32 | .133 | 32.45 | 4 | .000 |
| Depression pre–post | 3 | 0.31 | −0.06 | 0.67 | .100 | 1.233 | 5 | .030 |
| Depression pre–FU | 3 | 0.47 | −0.10 | 1.04 | .108 | 3.79 | 2 | .150 |
| Active TF* comparators | ||||||||
| PTSD pre–post | 2 | 1.79 | 1.02 | 2.56 | .000 | 3.37 | 1 | .066 |
| PTSD pre–FU | 2 | 1.50 | 0.30 | 2.71 | .015 | 7.20 | 1 | .007 |
| Depression pre–post | 1 | 0.97 | 0.41 | 1.54 | .001 | 0.00 | 0 | 1.000 |
| Depression pre–FU | 1 | 1.14 | 0.50 | 1.79 | .001 | 0.00 | 0 | 1.000 |
| Non–active comparators | ||||||||
| PTSD pre–post | 9 | 0.19 | −0.08 | 0.47 | .163 | 35.10 | 8 | .000 |
| PTSD pre–FU | 7 | 1.40 | 0.54 | 2.26 | .001 | 71.23 | 6 | .000 |
| Depression pre–post | 7 | 0.05 | −0.09 | 0.19 | .498 | 1.32 | 6 | .97 |
| Depression pre–FU | 6 | 0.54 | −0.01 | 1.09 | .052 | 32.00 | 5 | .000 |
*PTSD, post-traumatic stress disorder; FU, follow-up; TF, trauma-focused; CI, confidence interval; Q, Cochrane’s heterogeneity statistic; df, degrees of freedom.
For PTSD, these effect sizes were found to be large at post-treatment (g = 0.77 [0.41; 1.12]) and sustained at follow-up (g = 1.08 [0.55; 1.62]). For depression, these effect sizes were found to be small at post-treatment (g = 0.34 [0.08; 0.59]) and sustained at follow-up (g = 0.67 [0.26; 1.12]).
3.8.2. Publication bias
For controlled effect sizes, visual inspection of the funnel plots did not suggest possible publication bias, for both time-points and both outcomes. Duval and Tweedie’s trim-and-fill procedure (2000) indicated unchanged results. For the non-controlled effect sizes of PTSD, however, seven studies were missing; and for the non-controlled effect sizes of depression, two studies were missing at post-treatment and three at follow-up. Imputed effect sizes for PTSD outcomes remained medium post-treatment (g = 0.71 [0.37; 1.06]) and at follow-up (g = 0.79 [0.37; 1.20]). Imputed effect sizes for depression outcomes were small post-treatment (g = 0.39 [0.14; 0.63]) and at follow-up (g = 0.36 [0.01; 0.71]).
3.8.3. Sensitivity analyses
For PTSD and depression outcomes, no study was found to exert a disproportionally large effect on the overall effect sizes, for both time-points, involving non-controlled and controlled effect sizes.
3.9. Predictor analyses
For PTSD, treatment results were predicted by advancing age, but not by the other moderators. The model explained 34% of the inter-study variance. The residual heterogeneity was found to be non-significant (residual Q = 22.04; df = 9; p = .088)
For depression, treatment results were predicted by advancing age and migration, but not by the remaining moderators. The model explained 97% of the inter-study variance. Residual heterogeneity was found to be non-significant (residual Q = 0.25; df = 7; p = .976). The details of the multiple regression analyses are presented in Table 4.
Table 4.
Meta-regression analyses relating mean age, being female, migration, treatment dose, matching languages, outcome, and therapist’s training to non-controlled effect sizes.
| PTSD* | |||||||
|---|---|---|---|---|---|---|---|
| Assessment | Moderator | R2* | Q* (df = 7) | B* | SE* | B* | p-value |
| Pre- to post treatment | .34 | 22.04 (9) | .088 | ||||
| Mean Age | 0.05 | 0.02 | 0.75 | .043 | |||
| Female Gender | −0.01 | 0.01 | −0.39 | .145 | |||
| Migration | −0.70 | 0.41 | −0.44 | .084 | |||
| Treatment Dose | 0.00 | 0.00 | 0.41 | .325 | |||
| Matching Languages | −0.48 | 0.60 | −0.30 | .421 | |||
| Outcome | −0.15 | 0.45 | −0.09 | .744 | |||
| Therapist’s Training | −0.33 | 0.72 | −1.18 | .643 | |||
| Depression | |||||||
| Pre- to post treatment | .97 | .82 (5) | .976 | ||||
| Mean Age | 0.3 | 0.14 | 0.99 | .039 | |||
| Female Gender | 0.00 | 0.01 | −0.04 | .993 | |||
| Migration | −0.46 | 0.19 | −0.60 | .018 | |||
| Treatment Dose | 0.00 | 0.00 | −0.22 | .793 | |||
| Matching Languages | −0.96 | 0.98 | −1.11 | .328 | |||
| Outcome | −0.22 | 0.36 | −0.26 | .548 | |||
| Therapist’s Training | 0.17 | 1.18 | 0.10 | .887 | |||
PTSD, post-traumatic stress disorder; R2, explained variance; Q, Cochrane’s heterogeneity statistic; df, degrees of freedom; B, intercept; SE, standard error; β, regression coefficient.
4. Discussion
4.1. Main findings
This meta-analysis shows that NET is effective in the reduction of PTSD and depression symptoms across diverse, predominantly war-affected refugee populations. Treatment results are better for older adults. NET was found to be superior to non-active comparators and active non-TF comparators. As yet, no controlled comparisons with other guideline-supported TF interventions were not available. The application of paraprofessional therapists and very low treatment doses in trials can be seen as strengthening external validity. Using the GRADE framework, the risk of bias in the primary studies was found to range from unclear to high.
4.2. Predictors
Advancing age predicted better treatment outcomes for PTSD and depression symptoms. These findings may be explained by the lifespan perspective of NET. Trauma exposure with several retellings may foster cognitive coherence, self-reflection, and restored meaning in life. Thus, it may appeal to the needs of older adults (Rizvi et al., 2009). Unexpectedly, a higher proportion of women did not show significant associations with treatment results. Such deviations from earlier findings may be explained by differences in sample size and sample specificity. The sample of Watts et al. (2013) contained nearly 10 times more participants than the present sample. In the study by Stenmark et al. (2014), male gender may have been influenced by violent offences. In the study by Tarrier et al. (2000), the female gender may have been influenced by psychoticism or treatment motivation. Migration to Western countries predicted smaller treatment results for depression, but not for PTSD. This finding implies that treatment response for PTSD is not influenced by post-migration stress. For the treatment of depression, however, NET appears to be less satisfying. Higher treatment dose showed no significant association with treatment results. This finding may encourage more research on NET with brief treatment formats. Outcome assessment did not predict treatment outcomes; neither did language matching. The latter finding supports that of Lambert and Alhassoon (2015). Although this finding may not take away methodologists’ concerns regarding assessments, it implies that the assistance of interpreters does not influence treatment outcomes. Similar conclusions were found for ethnic matching in providing mental healthcare to Mediterranean migrants in the Netherlands (Knipscheer & Kleber, 2004). Unexpectedly, treatment progression was not predicted by the therapist’s training. This finding supports the contribution of trained paraprofessionals as NET therapists, being highly relevant in low-resource settings.
4.3. Findings in context
The included NET trials have been conducted in various settings and, consequently, in different healthcare systems. NET for non-refugees was found to be highly efficacious, albeit involving notably smaller treatment groups than the other studies. Remarkably, NET trials with migrated refugees (treated in healthcare systems in Western countries) did not show higher mean effect sizes than those with refugees in their home regions. Apparently, refugees in Western countries did not benefit more from NET in the settings of those countries. This finding may be explained by the influence of time on persisting PTSD symptoms. In current network analyses of PTSD, a common factor (trauma) is assumed to cause the onset of PTSD (influenced by vulnerability and protecting variables), whereas the persistence of the disorder seems to be governed by a larger network of variables (Fried & Cramer, 2017). Although the scope of the present study does not allow for a direct comparison, it can be hypothesized that refugees resettled in Western countries on average suffer from chronic symptoms, potentially complicated by post-migration stressors, especially language barriers and the necessity to adjust to Western cultures (Li et al., 2016). Addressing those symptoms with the help of NET – focusing on the past – can be less efficacious than might be expected in high-quality healthcare systems. This finding may call for research investigating whether migrated refugees benefit as much from NET as from other guideline-supported TF interventions. To effectively treat resettled refugees in Western healthcare systems, individualized decisions are needed, based on comparative evidence of different TFCBT interventions or eye movement desensitization and reprocessing (EMDR). Some meta-analytic findings show effect sizes of TFCBT to be superior to those of the current study (Bradley, Greene, Russ, Dutra, & Westen, 2005; Watts et al., 2013). The findings of the current study are, however, in accordance with recent meta-analytic findings, involving participants with complex problems (Gerger et al., 2014) or refugees resettled in Western countries (Nosè et al., 2017). The results were also consistent with those involving survivors of childhood abuse (Ehring et al., 2014).
The comparators varied from waiting-list conditions to active psychosocial interventions. The active interventions suggested contextual face validity and credibility. By using the strict criteria of the GRADE framework for the evaluation of the trials, the assessment focused on the internal validity of the studies, providing rather conservative ratings. Factors of external validity included intended face validity and credibility of the comparators, the complexity of the difficulties within the target population, and the local circumstances.
The framework of GRADE reduces the overall methodological quality to the weakest qualification, which presents serious dilemmas in psychotherapy research. Whereas underrating the risks of bias may lead to accepting disappointing treatments, overrating such risks may withhold effective interventions from patients in need (Patel et al., 2014). As for NET, numerous studies, qualitatively equivalent to other psychotherapy research, conducted with high external validity, have supported evidence on the safety and efficacy of NET across various populations. Therefore, NET has been described as being of proven effectiveness (Jong, Knipscheer, Ford, & Kleber, 2014) and can be considered the psychotherapeutic treatment of choice in post-conflict settings.
4.4. Strengths and limitations
The present study is the first meta-analysis summarizing the current evidence base of NET. Its strengths include a systematic literature selection, a domain-based methodological quality appraisal, a differentiation between TF and non-TF control conditions, and, finally, the exploration of heterogeneity in the main outcomes by meta-regression analyses.
Simultaneously, this study has a number of limitations. First, restricted study quality limited the interpretation of results. This is not unexpected, since the majority of TFCBT interventions shares this qualification (Bisson et al., 2013; Patel et al., 2014). Secondly, the current absence of guideline-supported TF comparators presents a persisting research gap. Thirdly, the short mean length of follow-up intervals may be considered a limitation. In a long follow-up interval, the protection of the intervention against new traumatic exposure can be assessed. Fourthly, the findings regarding follow-up outcomes were based on fewer studies, limiting the conclusions about stability of follow-up results. Fifthly, the heterogeneity of the PTSD outcomes was only partly explained by the selected predictors. Furthermore, for the non-controlled effect sizes, the possibility of publication bias was suggested. This finding calls for extended research. Finally, the high frequency of a limited group of authors may present a risk of confounding on grounds of therapist effects and allegiance bias (Wampold et al., 2010).
4.5. Clinical implications
Notwithstanding shared methodological weaknesses, in recent guidelines TFCBT and EMDR are recommended as the most effective treatments for PTSD (Foa, 2009; Hamblen, Schnurr, Rosenberg, & Eftekhari, 2009). NET has been considered qualitatively comparable to those evidence-based trauma therapies (Hoge, 2011), and is currently included in the suggested interventions for treating PTSD in adults (APA, 2017).
Despite the need for caution in interpretation, this study’s findings provide evidence for empirically informed decision making in clinical practice and research policy. Providing NET to adults with high problem complexity may be expected to be safe and effective. Symptoms of depression require specific attention when treating refugees in Western countries. In clinical care, the findings imply that no reluctance is needed with regard to the provision of NET with interpreters. The same accounts for trained paraprofessionals providing NET in low-resource settings.
4.6. Future research
Although rigorous research methodology and the needs of clinical care in naturalistic settings may be hard to align, some research options can be outlined. To enhance the methodological quality of future research, larger samples should be used, and individual treatment results, including adverse developments, should be systematically reported. These recommendations also apply to the generalization of the results of non-refugee trials. To explain the residual heterogeneity for PTSD outcomes, more research is recommended on trauma-related variables such as traumatic load, which may influence treatment response (Lonergan, 2014), and clinical variables such as the influence of comorbid depression symptoms (Haagen, Ter Heide, Mooren, Knipscheer, & Kleber, 2017). In addition, to assess long-term treatment results, future research should preferably follow up patients for 2 years after the end of treatment (Bradley et al., 2005). Next, strengthening comparative evidence of NET relative to TF comparators would seem to be supportive. Direct comparisons, however, hardly yield clear differences (Tran & Gregor, 2016). More can be expected from studies with high-frequency measuring, which may reveal relevant information on response patterns or treatment strategies (Nijdam et al., 2012). Furthermore, the development of future NET research by independent research groups would strengthen the evidence for NET. Finally, applications of NET beyond refugee populations are awaiting qualitatively rigorous research.
5. Conclusions
Although the evidence regarding the treatment effects of NET must be interpreted with caution, this meta-analysis provides empirical support for the effectiveness of NET for traumatized and highly burdened populations, facilitating optimization of treatment response in clinical care.
Acknowledgments
Foundation Centrum ’45, partner in Arq Psychotrauma Expert Group, funded this study. The authors wish to thank the following persons for their contributions to this meta-analysis: Jonna Lind and Wouter de Nooij of Arq library; research assistants Hilde van de Beek, Heleen van Dinther, and Zeynep Karaca; and the authors replying to the requests for information.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Al Hadethe A., Hunt N., Al-Qaysi G., & Thomas S. (2015). Randomised controlled study comparing two psychological therapies for posttraumatic stress disorder (PTSD): Emotional freedom techniques vs. narrative exposure therapy (NET). Journal of Traumatic Stress Disorders & Treatment, 4(4). doi: 10.4172/2324-8947.1000145 [DOI] [Google Scholar]
- Alghamdi M., Hunt N., & Thomas S. (2015). The effectiveness of narrative exposure therapy with traumatised firefighters in Saudi Arabia: A randomised controlled study. Behaviour Research and Therapy, 66, 64–13. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed. (Text Revision)). Washington, DC: APA. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: APA. [Google Scholar]
- American Psychological Association (2010). Publication manual (6th ed.). Washington, DC: APA. [Google Scholar]
- American Psychological Association (2017). Clinical practice guideline for the treatment of posttraumatic stress disorder (PTSD) in adults. Retrieved from https://www.apa.org/ptsd-guideline/ptsd.pdf
- Bichescu D., Neuner F., Schauer M., & Elbert T. (2007). Narrative exposure therapy of political imprisonment-related chronic posttraumatic stress disorder. Behaviour Research and Therapy, 45(9), 2212–2220. [DOI] [PubMed] [Google Scholar]
- Bisson J. I., Roberts N. P., Andrew M., Cooper R., & Lewis C. (2013). Psychological therapies for chronic post-traumatic stress disorder (PTSD) in adults. The Cochrane Library 2013. doi: 10.1002/14651858.CD003388.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley R., Greene J., Russ E., Dutra M. A., & Westen D. (2005). A multidimensional meta-analysis of psychotherapy for PTSD. American Journal of Psychiatry, 162, 214–227. [DOI] [PubMed] [Google Scholar]
- Brom D., Kleber R. J., & Defares P. B. (1989). Brief psychotherapy for posttraumatic stress disorders. Journal of Consulting and Clinical Psychology, 57(5), 607–612. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1992). Quantitative methods in psychology. A power primer. Psychological Bulletin, 112, 155–159. [DOI] [PubMed] [Google Scholar]
- Cusack K., Jonas D. E., Forneris C. A., Wines C., Sonis J., Middleton J. C., & Gaynes B. N. (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–141. [DOI] [PubMed] [Google Scholar]
- De Jong K., De, Knipscheer J. W., Ford N., & Kleber R. J. (2014). The efficacy of psychosocial interventions for adults in contexts of ongoing man-made violence - A systematic review. Health, 6, 504–516. [Google Scholar]
- Dossa N. I., & Hatem M. (2012). Cognitive-behavioral therapy versus other PTSD psychotherapies as treatment for women victims of war-related violence: A systematic review. The Scientific World Journal, 1–19. doi: 10.1100/2012/181847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duvall S., & Tweedie R. (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56(2), 455–463. [DOI] [PubMed] [Google Scholar]
- Ehring T., Welboren R., Morina N., Wicherts J. M., Freitag J., & Emmelkamp P. M. G. (2014). Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clinical Psychology Review, 34, 645–657. [DOI] [PubMed] [Google Scholar]
- Ertl V., Pfeiffer A., Schauer E., Elbert T., & Neuner F. (2011). Community-implemented trauma therapy for former child soldiers in Northern Uganda. A randomized controlled trial. Journal of the American Medical Association, 306(5), 503–512. [DOI] [PubMed] [Google Scholar]
- Foa E. B. (2009). ISTSS-Treatment Guideline no.4. Cognitive-behavioral therapy for adults In Foa E. B., Keane T. M., Friedman M. J., & Cohen J. A. (Eds.), Effective treatments for PTSD (2nd ed.) (pp. 549–558). New York, NY: Guilford Press. [Google Scholar]
- Fried E. I., & Cramer A. O. J. (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12, 999–1020. [DOI] [PubMed] [Google Scholar]
- Gerger H., Munder T., & Barth J. (2014). Specific and non-specific psychological interventions for PTSD symptoms: A meta-analysis with problem complexity as a moderator. Journal of Clinical Psychology, 70(7), 601–615. [DOI] [PubMed] [Google Scholar]
- Gwozdziewycz M., & Mehl-Madrona L. (2013). Meta-analysis of the use of narrative exposure therapy for the effects of trauma among refugee populations. Permanente Journal, 17(1), 70–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haagen J. F. G., Ter Heide F. J. J., Mooren T. M., Knipscheer J. W., & Kleber R. J. (2017). Predicting PTSD treatment response in refugees: Multilevel analysis. British Journal of Clinical Psychology, 56(1), 69–83. [DOI] [PubMed] [Google Scholar]
- Hamblen J. L., Schnurr P. P., Rosenberg A., & Eftekhari A. (2009). A guide to the literature on psychotherapy for PTSD. Psychiatric Annals, 39, 348–354. [Google Scholar]
- Hauffa R., Rief W., Brähler E., Martin A., Mewes R., & Glaesmer H. (2011). Lifetime traumatic experiences and posttraumatic stress disorder in the German population results of a representative population survey. Journal of Nervous and Mental Disease, 199, 934–939. [DOI] [PubMed] [Google Scholar]
- Hensel-Dittmann D., Schauer M., Ruf M., Catani C., Odenwald M., Elbert T., & Neuner F. (2011). Treatment of traumatized victims of war and torture: A randomized controlled comparison of narrative exposure therapy and stress inoculation training. Psychotherapy and Psychosomatics, 80(6), 345–352. [DOI] [PubMed] [Google Scholar]
- Higgins J. P. T., Altman D. G., Gøtzsche P. C., Jüni P., Moher D., Oxman A. D., … Sterne J. A. C. (2011). The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. British Medical Journal, 343. doi: 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hijazi A. M., Lumley M. A., Ziadni M. S., Haddad L., Rapport L. J., & Arnetz B. B. (2014). Brief narrative exposure therapy for posttraumatic stress in Iraqi refugees: A preliminary randomized clinical trial. Journal of Traumatic Stress, 27(3), 314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoge C. W. (2011). Interventions for war-related posttraumatic stress disorder. Meeting veterans where they are. Journal of the American Medical Association, 306, 549–551. [DOI] [PubMed] [Google Scholar]
- Jacob N., Neuner F., Maedl A., Schaal S., & Elbert T. (2014). Dissemination of psychotherapy for trauma, spectrum disorders in postconflict settings: A randomized controlled trial in Rwanda. Psychotherapy and Psychosomatics, 83(6), 354–363. [DOI] [PubMed] [Google Scholar]
- Knipscheer J. W., & Kleber R. J. (2004). A need for ethnic similarity in the therapist-patient interaction? Mediterranean migrants in Dutch mental health care. Journal of Clinical Psychology, 60(6), 543–554. [DOI] [PubMed] [Google Scholar]
- Lambert J. E., & Alhassoon O. M. (2015). Trauma-focused therapy for refugees: Meta-analytic findings. Journal of Counseling Psychology, 62, 28–37. [DOI] [PubMed] [Google Scholar]
- Li S. Y., Liddell B. J., & Nickerson A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18(82). doi: 10.1007/s11920-016-0723-0 [DOI] [PubMed] [Google Scholar]
- Lipsey M. W., & Wilson D. B. (2001). Practical meta-analysis. Applied social research method series (Vol. 49). London: Sage Publications. [Google Scholar]
- Lonergan M. (2014). Cognitive behavioral therapy for PTSD: The role of complex PTSD on treatment outcome. Journal of Aggression, Maltreatment & Trauma, 23, 494–512. [Google Scholar]
- McEwen B. (2012). Brain on stress: How the social environment gets under the skin. Proceedings of the National Academy of Sciences, 109(2), 17180–17185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morath J., Gola H., Sommershof A., Hamuni G., Kolassa S., & Catani C. (2014a). The effect of trauma-focused therapy on the altered T cell distribution in individuals with PTSD: Evidence from a randomized controlled trial. Journal of Psychiatric Research, 54, 1–10. [DOI] [PubMed] [Google Scholar]
- Morath J., Moreno-Villanueva M., Hamuni G., Kolassa S., Ruf-Leuschner M., Schauer M., … Kolassa I.-T. (2014b). Effects of psychotherapy on DNA strand break accumulation originating from traumatic stress. Psychotherapy and Psychosomatics, 83(5), 289–297. [DOI] [PubMed] [Google Scholar]
- Mørkved N., Hartmann K., Aarsheim L. M., Holen D., Milde A. M., Bomya J., & Thorp S. R. (2014). A comparison of narrative exposure therapy and prolonged exposure therapy for PTSD. Clinical Psychology Review, 34, 453–467. [DOI] [PubMed] [Google Scholar]
- Mundt A., Wünsche P., Heinz A., & Pross C. (2014). Evaluating interventions for posttraumatic stress disorder in low and middle income countries: Narrative exposure therapy. Intervention, 12(2), 250–266. [Google Scholar]
- National Institute for Clinical Excellence (2005). Post-traumatic stress disorder: The management of PTSD in adults and children in primary and secondary care (Clinical Guideline 26). NICE Leicester, UK: Gaskell. [PubMed] [Google Scholar]
- Neuner F., Kurreck S., Ruf M., Odenwald M., Elbert T., & Schauer M. (2010). Can asylum-seekers with posttraumatic stress disorder be successfully treated? A randomized controlled pilot study. Cognitive Behaviour Therapy, 39(2), 81–91. [DOI] [PubMed] [Google Scholar]
- Neuner F., Onyut P. L., Ertl V., Odenwald M., Schauer E., & Elbert T. (2008). Treatment of posttraumatic stress disorder by trained lay counsellors in an African refugee settlement: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 76(4), 686–694. [DOI] [PubMed] [Google Scholar]
- Neuner F., Schauer M., Klaschik C., Karunakara U., & Elbert T. (2004). A comparison of narrative exposure therapy, supportive counselling, and psychoeducation for treating posttraumatic stress disorder in an African refugee settlement. Journal of Consulting and Clinical Psychology, 72(4), 579–587. [DOI] [PubMed] [Google Scholar]
- Nickerson A., Bryant R. A., Silove D., & Steel Z. (2011). A critical review of psychological treatments of posttraumatic stress disorder in refugees. Clinical Psychology Review, 31, 399–417. [DOI] [PubMed] [Google Scholar]
- Nijdam M. J., Gersons B. P., Reitsma J. B., De Jongh A., & Olff M. (2012). Brief eclectic psychotherapy v. eye movement desensitisation and reprocessing therapy for post-traumatic stress disorder: Randomised controlled trial. British Journal of Psychiatry, (3), 224–231. doi: 10.1192/bjp.bp.111.099234 [DOI] [PubMed] [Google Scholar]
- Nosè M., Ballette F., Bighelli I., Turrini G., Purgato M., Tol W., … Barbui C. (2017). Psychosocial interventions for post-traumatic stress disorder in refugees and asylum seekers resettled in high-income countries: Systematic review and meta-analysis. PLoS ONE, 12(2). doi: 10.1371/journal.pone.0171030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- OvidSP [Computer software]. Retrieved from http://ovidsp.ovid.com
- Palic S., & Elklit A. (2011). Psychosocial treatment of posttraumatic stress disorder in adult refugees: A systematic review of prospective treatment outcome studies and a critique. Journal of Affective Disorders, 131(1), 8–23. [DOI] [PubMed] [Google Scholar]
- Patel N., Kellezi B., & Williams A. C. D. C. (2014). Psychological, social and welfare interventions for psychological health and well-being of torture survivors (Review). The Cochrane Library, 11. doi: 10.1002/14651858.CD009317.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rizvi S. L., Vogt D. S., & Resick P. A. (2009). Cognitive and affective predictors of treatment outcome in cognitive processing therapy and prolonged exposure for posttraumatic stress disorder. Behaviour Research and Therapy, 47, 737–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robjant K., & Fazel M. (2010). The emerging evidence for narrative exposure therapy: A review. Clinical Psychology Review, 30, 1030–1039. [DOI] [PubMed] [Google Scholar]
- Rytwinski N. K., Scur M. D., Feeny N. C., & Youngstrom E. A. (2013). The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: A meta-analysis. Journal of Traumatic Stress, 26, 299–309. [DOI] [PubMed] [Google Scholar]
- Schaal S., Elbert T., & Neuner F. (2009). Narrative exposure therapy versus interpersonal psychotherapy. A pilot randomized controlled trial with Rwandan genocide orphans. Psychotherapy and Psychosomatics, 78, 298–306. [DOI] [PubMed] [Google Scholar]
- Schauer M., Neuner F., & Elbert T. (2011). Narrative exposure therapy. A short-term intervention for traumatic stress disorders after war, terror or torture (2nd, expanded ed.). Göttingen: Hogrefe & Huber Publishers. [Google Scholar]
- Schnyder U., Ehlers A., Elbert T., Foa E. B., Gersons B. P. R., Resick P. A., … Cloitre M. (2015). Psychotherapies for PTSD: What do they have in common? European Journal of Psychotraumatology, 6, 28186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steel Z., Chey T., Silove D., Marnane C., Bryant R. A., & Van Ommeren M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement. A systematic review and meta-analysis. Journal of the American Medical Association, 5, 537–548. [DOI] [PubMed] [Google Scholar]
- Stenmark H., Catani C., Neuner F., Elbert T., & Holen A. (2013). Treating PTSD in refugees and asylum seekers within the general health care system. A randomized controlled multicenter study. Behaviour Research and Therapy, 51(10), 641–647. [DOI] [PubMed] [Google Scholar]
- Stenmark H., Guzey I. C., Elbert T., & Holen A. (2014). Gender and offender status predicting treatment success in refugees and asylum seekers with PTSD. European Journal of Psychotraumatology, 5. doi: 10.3402/ejpt.v5.20803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarrier N., Sommerfield C., Pilgrim H., & Faragher B. (2000). Factors associated with outcome of cognitive-behavioural treatment of chronic post-traumatic stress disorder. Behaviour Research and Therapy, 38, 191–202. PII: S0005-7967(99)00030-3. [DOI] [PubMed] [Google Scholar]
- Ter Heide F. J. J., Mooren T. M., Van de Schoot R., De Jongh A., & Kleber R. J. (2016). Eye movement desensitisation and reprocessing therapy v. stabilisation as usual with refugees: Randomised controlled trial. British Journal of Psychiatry, 209(4), 311–318. [DOI] [PubMed] [Google Scholar]
- Tran U. S., & Gregor B. (2016). The relative efficacy of bona fide psychotherapies for posttraumatic stress disorder: A meta-analytical evaluation of randomized controlled trials. BMC Psychiatry, 16, 266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold B. E., Imel Z. E., Laska K. M., Benish S., Miller S. D., Del Re A. C., … Budge S. (2010). Determining what works in the treatment of PTSD. Clinical Psychology Review, 30, 923–933. [DOI] [PubMed] [Google Scholar]
- Watts B. V., Schnurr P. P., Mayo L., Young-Xu Y., Weeks W. B., & Friedman M. J. (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. Journal of Clinical Psychiatry, 74(6), e541–e550. [DOI] [PubMed] [Google Scholar]
- Zang Y., Hunt N., & Cox T. (2013). A randomised controlled pilot study: The effectiveness of narrative exposure therapy with adult survivors of the Sichuan earthquake. BMC Psychiatry, 13(41). doi: 10.1186/1471-244X-13-41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zang Y., Hunt N., & Cox T. (2014). Adapting narrative exposure therapy for Chinese earthquake survivors: A pilot randomised controlled feasibility study. BMC Psychiatry, 14(262). doi: 10.1186/s12888-014-0262-3 [DOI] [PMC free article] [PubMed] [Google Scholar]


