ABSTRACT
This study aims to demonstrate a comprehensive understanding of the life experience of victims of medical accidents after medical accidents and medical litigations. A single victim of a medical accident participated in the study. Six upper categories were derived as the results: “frustration and anger toward medical accident occurrence,” “desolated struggle for medical litigation,” “distrust of medical litigation related legal profession,” “accepting myself with a disability caused by a medical accident,” “a life with far more unexpected challenges as an athlete with disabilities,” and “find new meaning after the medical accident.” The participant was experiencing physical and psychological distress in the process of accepting the medical accident and the disability. In addition, the participant was exposed to the secondary psychological distress from the medical profession, lawyer, and legal profession in the peculiar situation of medical litigation, and to the third psychological distress in life living as a disabled person.
KEYWORDS: Victim of medical accident, patient safety, disclosure of patient safety incidents, case study, medical litigation
Introduction
Medical practice is an act of good faith that alleviates and cures a patient’s suffering. There are, however, inevitably risks associated with medical practices, which can lead to unexpected medical accidents (Park, 2011). Ock, (2014) defines a medical accident as “Any accident that occurs in the entire process of medical practice such as diagnosis, examination, and treatment of a patient in a medical institution irrespective of whether the medical staff is negligent or not.” This definition highlights value-neutral terms that demonstrate all accidents that may occur in medical practice without evaluating mistakes a medical practitioner made (Ock, 2014).
The American Psychiatric Association (APA) defines a traumatic event as events experiencing an actual death or threat of death; experiencing, witnessing, or confronting a severe injury; and the individual with the traumatic experience suffer from strong fear, helplessness, and horror (American Psychiatric Association, 1994). Medical accidents are known to precipitate severe trauma along with physical and psychological shocks to primarily experienced patients and other parties including medical professions as they are unexpected accidents occurred during the course of medical treatment (Kim, 2012; Ock, 2016). Among the parties, the victim of the medical accident with direct physical and psychological damages is called the first victim. It indicates that the first victim of the medical accident experiences psychological difficulties besides physical ones as the result of the traumatic event. In addition, the first victim lives in strenuous reality as he/she suffers from physical damages caused by the medical accident as well as medical litigation to disclose causes of the accident. Medical litigation requires judgment of medical expertise and skills. As the current law grants the victim a burden of proving medical malpractice, a medical accident involves long-standing disputes and litigation, not just an accident itself (Kang, Kim, Sung, & Mok, 2013). Therefore, a victim of a medical accident encounters a prolonged medical litigation with sudden physical injury along with long-term psychological and physical difficulties caused by a medical accident.
The research on victims of medical accidents is constrained to perform multifariously for the delicacy of the subject and the difficulty of selecting and sampling participants. Moreover, since the exact status of the medical accident is not apprehended, the status is indirectly predicted by in the legal term “medical dispute.” According to the Statistical Yearbook of Arbitration (2017), about 40,000 medical dispute counselling sessions are held annually in Republic of Korea (hereinafter Korea), and the number has been accelerating(Korea Medical Dispute Mediation and Arbitration Agency, 2017). As the debate about patient-centeredness in Korea is heightened, medical disputes are expected to increase gradually.
Despite the number of cases and the seriousness of the accidents to the people concerned, the system in Korea is mainly focused on the treatment of the medical disputes (Lee, Kim, & Lee, 2014). Although the medical malpractice death of famous singer Shin Hae-cheol in 2014 became the occasion of medical accident damage relief and medical dispute settlement law enactment (Newspaper, 2016; Yonhapnewstv, 2016), victims protesting in the National Assembly or in front of the medical institutions can be commonly observed in Korea. They suffer from long-term difficulties caused by medical accidents (Kukmin ilbo, 2018; Yonhapnewtv, 2017). Unfortunately, the researches in Korea related to the experiences and difficulties of victims of medical accidents have not progressed in diversified ways. Kim, Lee, Choi, & Sohn (2017) discovered that 171 out of 180 victims of medical accidents (95%) were identified with complete Post Traumatic Stress Disorder (PTSD) symptoms (Kim et al., 2017). The severity of PTSD symptoms was significantly higher than those who experienced traumatic events such as breast cancers, HIV, domestic violence, traffic accidents, bereavement, war, earthquake, and burn. This finding highlights that a medical accident is a serious trauma that causes an extreme high level of PTSD symptoms to the victim. However, in-depth understanding of the specific experiences and difficulties of victims of medical accidents has not been extensively analyzed.
This study aims to provide comprehensive understanding of how a first victim of a medical accident with a medical litigation experience lives his/her life, copes with the life situations, and attempts to solve the problem. In particular, the research signifies general experience of medical litigation after a medical accident and overcoming process of the psychological and physical struggles. This research is expected to contribute a more practical approach to establish the direction of psychological and social intervention for the medical accident based on the understanding of the substantial experiences of the victims of the medical accident. The specific research problems are as follows.
“What kind of struggles does a victim who has been physically injured in a medical accident experience during the course of medical litigation and how does he/she overcomes it?”
Method and analysis
Research method
Qualitative case study is a suitable method for understanding the complexity of a situation and the specificity of its behaviour (John, 2017; Kim, Park, Park, Son, & Sin, 2009; You, Jeong, Kim, & Kim, 2016). The study aim is to understand the life experiences of a single victim of medical accident who has endured a medical litigation. Medical accident and medical litigation are unique and unfamiliar experiences. First victims of medical accidents often suffer from long-standing medical litigations, and if injuries due to medical accidents were permanent, the difficulties last a lifetime. As a consequence, the case of this study is different from other common event. In other words, the qualitative case study method is utilized to understand the experience of the physically damaged parties through medical accidents more comprehensively.
Participant
We recruited first victims of medical accidents as participants in this study. The first victims of medical accidents include not only patients who directly experienced the medical accidents bust also the families of the patients. However, the criteria for selecting participants for this study are as follows: A person who have suffered physical disability due to a medical accident and have experienced medical accident litigations. The criteria for exclusion are as follows: First, bereaved families who lost their families in medical accidents. Second, the victim who was not physically injured due to a medical accident. Third, the person who have no experience of medical accident litigation.
The purposive sampling was exercised to select the participants who coincided with the research purpose. Specifically, one of the researchers discovered a participant unintentionally through a sports article on a Korean portal site. The article contained the participant’s the medical accident, the medical litigation and verdict, and subsequent life as an athletic. The researcher contacted the participant via her social network account and briefly communicated the purpose and contents of the research. After the short conversation via social network, the researcher explained the details of the research face-to-face and received consent from the participant. Table I provides brief information on the participant.
Table I.
Characteristics of the research participant.
| Sex | Age | Occupation | Time of Occurrence Medical accident | Medical Accident Damages | Medical Litigation Period | Medical Litigation Verdict |
|---|---|---|---|---|---|---|
| F | Mid-30 s | Athlete | July 2004 | Paraplegia | 6 years | 20%win |
Table II provides brief information on the occurrence of medical accidents of the research participant.
Table II.
Occurrence of medical accident.
| Summer of 2014, the 20-year-old research participant was a student who was training to become a model. The participant who was preparing for a model competition during freshmen year summer vacation visited a hospital to realign the neglected forward head posture. In order to receive Frollo’s treatment, Frollo should be injected into the muscle area of the side of the vertebrae. A doctor made a medical mistake by injecting the injection in the wrong spot. Immediately after the injection, the participant felt abnormality in her left arm and soon her entire body became paralyzed. Afterwards, the participant’s senses were partially recovered but she was suspected of permanent impairment. Since then, the participant has been diagnosed with paraplegia albeit she has received persistent rehabilitation treatment. |
Data collection method and procedure
A multiplicative data sources were used in accordance with the characteristics of qualitative case study aimed at comprehensively understanding the case. First, the data were collected through in-depth interviews with the participant. Considering the ethical aspects of the study, the researcher thoroughly explained the purpose and details of the study to the participant and received the participant’s voluntary consent to participate in the research and to record the in-depth interviews. The interview was conducted at the participant’s house and training facility where she can talk with comfort. The length of the interview varies from at least 1 hour 45 minutes to at most 2 hours 15 minutes. The number of face-to-face in-depth interviews was performed three times. In-depth interview guideline made a based on the participants’ broadcast video and online articles. In addition, interview guideline contained semi-structured questions about experiences of life after the medical accident (Pyo, 2018). The adequacy of the interview questions was evaluated by a professor from the department of counselling and one of the researchers who is a professor in medical field. The specific interview questions are as follows. First, “Explain how the medical accident occurred.” Second, “How was the problem solving process after the medical accident?” Third, “What psychological, physical and social changes occurred after the medical accident?” Fourth, “What was the hardest part of the problem solving process after experiencing the medical accident?” Fifth, “How did the occurrence of the medical accident affect yourself and associated others?”
In addition to the interview materials, various information such as news footage and news reports were collected to comprehend the life experiences of the participant (Table III). Data collection was performed from June 2016 to April 2017.
Table III.
Data collection process.
| N | Data type | Date | Amount of data |
|---|---|---|---|
| 1 | Broadcast video | March, 2010 | 1 broadcast video |
| 2 | Online article | June, 2016 | 1 online article |
| 3 | Online article | August, 2016 | 1 online article |
| 4 | Online article | September, 2016 | 7 online articles |
| 5 | Online article | October, 2016 | 4 online articles |
| 6 | In-depth interview | January 17th, 2017 | 2 h 3 mins |
| 7 | In-depth interview | March 24th, 2017 | 1 h 45 mins |
| 8 | In-depth interview | May 10th, 2017 | 2 h 15 mins |
Analysis method and procedure
Data materials for the analysis include in-depth interview transcripts, the participant’s news report videos and articles transcripts. The analysis team consisted of one doctor in medicine and one master in counseling. With qualitative research experiences, they collected and analyzed the data. First, through in-depth interviews, transcribed data were segmented into meaning units in order to understand the meanings that the participant referred through repeatedly reading the transcriptions. Then, based on the segmented semantic units, main experiences were apprehended according to the temporal flow of the participants. At this stage, the participant’s experiences were categorized into a contextual dimension by integrating various data sources. After several in-depth interviews, researcher 1 conducted an analytical note and the results were reviewed by researcher 2, and revised after a sufficient discussion process when a disagreement was presented. In the process, the categorization work was completed through guidance and consultation of one professor of qualitative research in the field of counseling. Last, researchers confirmed that the experiences from in-depth interviews and those mentioned in the participants’ online articles and broadcast video match.
Validation of research
For the validity of the study, four criteria of Guba and Lincoln (1989) were examined: factual value, applicability, neutrality, and consistency. In order to secure the factual value of the research, the researcher attempted to establish a bond with the participant through social network messaging, phone-calling, and text messaging in advance (Guba & Lincoln, 1989). In the process of in-depth interviews, the researcher enabled the participant to disclose her experiences in comfort through sufficient interview time. In addition, the researcher tried to collect diverse materials such as news videos and articles related to the participant in advance for triangulation. Specifically, we reviewed participants’ one broadcast video, 13 online articles, and 3 times in-depth interviews. As a result, we have found common results through these three data sources, and have concluded an integrated conclusion. Furthermore, in the process of analysis, the participant was asked to confirm whether the participant’s empirical statements corresponded with the researcher’s analysis. In order to establish the applicability of the study, data saturation, in which no additional data are available in the data collection and analysis process, was evaluated. In order to establish the neutrality of the research, the researcher clarified his/her understanding and assumptions and conducted iterative discussion within the research team for the purpose of discontinuing the judgment by excluding the subjectivity of the researcher in analyzing the interviews and data. In order to maintain the consistency of the research, the entire process from data collection to data analysis was described in detail and efforts were made to comply with the research methods and procedures. The results of the research were revised through repeated confirmation with one doctor in the field of medicine who had undergone multiple qualitative researches. This was reviewed by a professor of qualitative research in the field of counselling. The overall strategies for ensuring the validity of the research are summarized in Figure 1.
Figure 1.
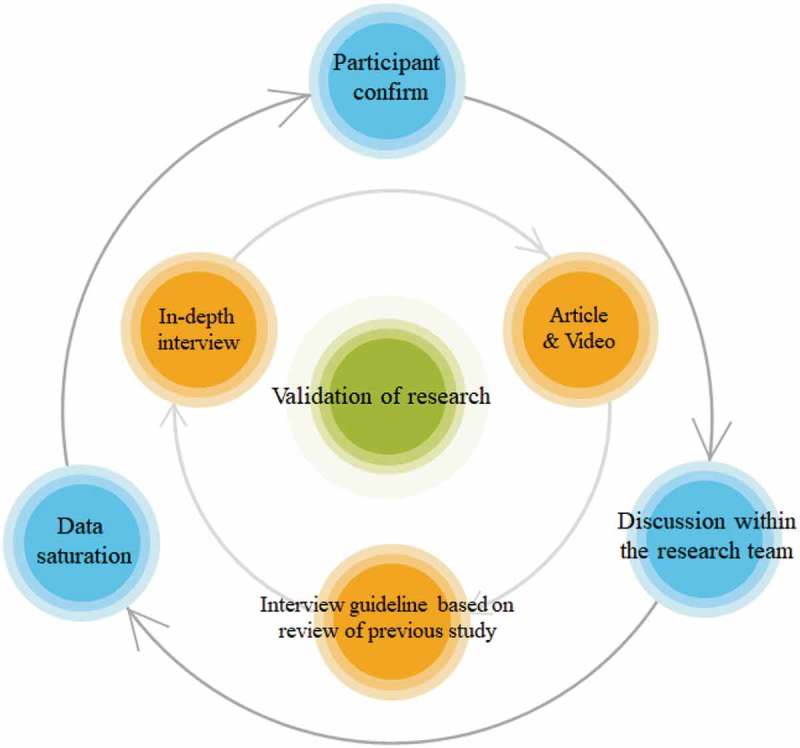
The process for validation of research.
Ethical considerations
This study was proceeded after the approval of IRB (IRB No: S2016-2008-0001) from the Institutional Review Board of A Hospital.
Findings
The main experiences of the participant of the study after the medical accident were searched for meanings in the context, and the central experiences were derived through the process of organizing them. A total of 293 semantic units, 22 subcategories, and 6 upper categories are presented as shown in Table IV through the process of restructuring the participant’ experience.
Table IV.
Structure of the analysis results.
| Subcategory | Upper Category |
|---|---|
| Resentment of the medical accident | Frustration and anger towards medical accident occurrence |
| Rage towards the medical staff’s response after the medical accident | |
| Tremendous effort required for the medical litigation | Desolated struggle for the medical litigation |
| A patient and caregivers who are required to ask the medical staff to provide the data to prove the medical error | |
| Medical malpractice difficult to prove | |
| Feeling regrettable towards people who talk lightly of medical litigation | |
| Medical litigation for solving lament, not money | Distrust of medical litigation-related legal profession |
| Medical litigation that should not be left to a lawyer | |
| Feeling regrettable of the litigation process and result | |
| Distrust of people involved in medical litigation | |
| Isolated life ascribable to medical litigation | Accepting myself with a disability caused by a medical accident |
| Feeling agonize over new career path | |
| Changes in values in women’s life after the medical accident | |
| A life restrained by family due to disability | |
| Discomfort of everyday life to that still cannot adapted | A life with far more unexpected challenges as an athlete with disabilities |
| Struggles to become an athlete | |
| Inevitable lifetime chronic pain as an athlete | |
| Secondary difficulties caused by associated people with low understanding of disability | |
| An invisible disability becoming an obstacle in a life as an athlete | Find new meaning after the medical accident |
| Trying to live healthier as a disabled person | |
| Helping others using my experience | |
| Need for concern and countermeasure to medical accidents |
Frustration and anger towards medical accident occurrence
The participant had a grudge against the incident itself that a medical accident occurred to her. “Why was it me? What would my life would have been like if I had not had a medical accident?” These unanswered questions, even after a decade has passed, was still tormenting the participant with resentment and anger in one corner of the participant’s mind.
“I always wonder what kind of life I could have lived without my disability. There are things I want to accomplish, but I suppress them. And I want to accept things I can take from this… But there are things that are annoying, frustrating… I can’t swallow those because it can’t be resolved… I get so angry…”
(Retrieved from the third transcription of the participant)
The participant living an inconceivable life tried one-person demonstrations in unjust and frustrated minds, but nobody was interested. The result of “20% partial victory” did not understand the participant’s frustration and anger: it only caused the participant to become more distressed because of the doubts about 80% of the reasons for the disability.
“Then who caused the accident? 80% is my fault. My fault for going to the hospital. Although I didn’t go there for an illness…”
(Retrieved from the third transcription of the participant)
Participant once again experienced a wounded heart by medical staff’s treatment of the medical accident before the resentment of the medical accident was abated. Although the participant who was 20 years old was paralyzed due to medical error of the medical staff, the attitudes of the medical staff to the participant changed with time. In the early days of the accident, the medical staff who acknowledged his mistakes and became responsible gradually changed their attitude. They would suspect whether the participant was feigning the illness or said they would take a responsibility if their negligence was recognized through the trial. Moreover, after the statute of limitations was over, they impudently responded that they were not liable to any accusations. These inhuman responses of the medical staff to the medical accident caused the participant to be indignant.
“I received a confirmation from the doctor to admit the medical malpractice. He said he had a medical accident and I received confirmation that he would be responsible for it. But at first, he paid me for my hospital bill. Because he made a verbal promise as well.. But after six months, I got a call from the hospital. My mom visited that hospital and from then on they said they can’t pay me, not even a dime, so I should do it by the law…”
(Retrieved from the first transcription of the participant)
“(His actions) disgusted me… I want to make this person responsible for his mistake.. I can’t see him feeling that much of guilt of making the mistake or living in a righteous way… After a while, it became someone else’s problem. It’s funny that he is living without any guilty conscious… He is back at his hospital like the old days and examining patients now… So I tried to file a criminal complaint..”
(Retrieved from the first transcription of the participant)
Desolated struggle for the medical litigation
The participant went to the hospital for realigning the forward head posture, not for a visit to the hospital for the purpose of treating an illness. Therefore, the participant who was convinced that she had a disability after the injection accident proceeded to the medical litigation. However, in the case of a medical accident, the medical case against the medical staff’s fault and the degree of it was formidable. The nature of medical accidents, the long process of dispute and requiring judgment on unfamiliar medical terminology and specialized knowledge and technology are typical cases of a medical litigation. However, due to the current law of Korea, the victim has the burden of proving medical malpractice. For this reason, she had to live her life fiercely, preparing for a lawsuit before accepting the disability.
The Participant received several medical examinations to reveal the cause of the disability for the purpose of the medical litigation. Contrary to now, when the lesion is obvious, the exact lesion did not appear at that time. She still wondered about this circumstance. At that time, the results of the tests were not clear, so she sent out requests to other university hospitals; but the results did not change. The doctors were reluctant to make a identification on the disability, saying the results were not clear. She doubted the perjury of the medical staff during the process, but there was no way to prove it.
“I got re-examed at Hospital A and Hospital B. Likewise, there was no appearance of disability. But it seemed like a disability. So, I received a reassessment after 3 years (from them). It does not come out on the MRI, it does not come out of the EMG.. I was normal on all the tests… But now I’m done with the litigation. At the C hospital, a few years later, I got retested and the disability aspects were in EMG and on MRI.”
(Retrieved from the first transcription of the participant)
“Now that the medical litigation is over, the statute of limitation is over… I was told that my disability comes out like this or that… Some doctors might say that unlike the past, it was odd that the exact lesion appeared today and that it could have been a wrong result back then. But it was difficult (for the doctor who made the mistake) to tell because of the power relationship of the doctors’ organization.”
(Retrieved from the first transcription of the participant)
On the basis of the unclear lesion results, the opponent aggravated that the psychological factors of the participant were the cause of the disorder. She voluntarily received a psychiatric evaluation to prove that the source of her disability was not due to the psychological factors. She was outraged that not only she had a disability, but also greatly hurt by the opponent’s claim that the cause of disability was her own. She could not understand the psychiatric evaluation process. She was kept under surveillance for two weeks in the hospital while disconnected from the outside world. The medical staff was unethical, ignoring requests from the participant with disability. She assumed that the purpose of the unethical actions of the medical staff was to adversely affect her mental emotions; so she tried hard not to give what they wanted.
“I wanted to take a shower, but they wouldn’t let me. They said I have to wait because they were busy, but then they said they need to get a permission from the doctor. (..) They took my wheelchair away too, but I couldn’t contact them or anything. What if I had to go to a restroom… So I did something like, I fell off the bed to the floor and I opened the (restroom) door.. A camera in the hospital room was recording all the time, and they told me to do everything like peeing and pooping there… So I promised to myself that when I get out, I am going to make them pay for all of these… I requested for the surrvalliance camera footage because I have to submit it to the Human Rights Commission. and court ordered them to release it as well. But they didn’t give it to me. They said the camera was broken at that time. It was done like that.”
(Retrieved from the first transcription of the participant)
The medical litigation shook down not only the personal life of the participant but also her family’s life. The unpredictable litigation schedules made it impossible for her to concentrate on the workouts she had begun for the rehabilitation purpose. In addition, the medical litigation, which requires tremendous amount of money, yielded financial difficulties in her family. Even her brother asked her opinion on him dropping out of college and make money. She could not afford the rehabilitation costs even with the borrowed money from her close relatives. The entire family was exhausted with the growing debt and disagreement between her parents.
“How do I live and go through rehabilitation when I have no money… A doctor told me that six months to a year is crucial period in rehabilitation, but who would pay for both the rehabilitation and litigation? I’ve been through all the hardship there possibly is. I went through possibly all the examinations that exist… massive amount of money went in to all of it.”
(Retrieved from the first transcription of the participant)
Distrust of medical litigation-related legal profession
The lawyer hired for the medical litigation was exceedingly confident that it would not have much trouble as the medical staff recognized his fault. The lawyer’s attitude, however, changed as the length of the litigation was prolonged. He applied the law in wrong way, failed to make a criminal complaint after the statute of limitations, and only discussed about money even before the verdict was made; the participant had to change her lawyer in the midst of the trial. She only received a 20% partial suits win although the litigation was seemed to favour her. After the verdict, the lawyer quit without any contingent fee and went away; he could not bear facing her. After a long consideration, she visited other lawyers and discussed a retrial. However, they told her to forget about the case and move on with her life as the 20% partial award was more than enough in their opinions.
“After five years of trials, I have two years to ask for a retrial. I don’t even know if my retrial demand will go through,, I don’t know if I can go through another trial if my demand is accepted. The lawyers told to me just forget about it,, just move on with my life,, They said 20% award is a really big deal apparently.”
(Retrieved from the first transcription of the participant)
The trial process was also left a big scar to the participant. The court declared comparative negligence referring precedent that was not related to her medical accident. The trial was conducted focusing only on the injury caused by a needle without considering the side effects of the drug. As a result, the court claimed that a paralyzed lesion of the lower half of the body was not clearly confirmed and found 20% partial win. She tried to appeal her resentfulness to the judge. However, the judge said that if he were her, he would not have made such a case. He also made preposterous comment that he would pray for her to walk. Immeasurably hurt by his words, she filed an application to challenge the judge.
“I told the judge while crying; If I were your family, would you have done this? How could you only listen to the opponent? Would you have done the same if your family was going through this? Then he said, if it were him, if it were him, he wouldn’t have make a case like this. (…) He said I can walk. He would pray for me to walk, so if I try hard, I can walk. So I filed an application to challenge the judge.”
(Retrieved from the first transcription of the participant)
Accepting myself with a disability caused by a medical accident
The participant became paralyzed by the medical accident at a peak of her youth—20 years old. The intense process of obtaining the disability and medical litigation at the young age made her life isolated. The participant who liked grooming gradually stopped going out as she felt that she could not keep up with the trend. The daily life that was discomforted by the disability disconnected her social interaction. Her friends’ kind consideration—came to her place to hang out or picked her up to go out—made her rather uncomfortable. She refrained herself from having a romantic relationship with a new person with fear that her unordinary life would not be understood by others. In the process of accepting the disability, she became helpless and wandered. She said that she still has some lingering attachment as her life has changed a lot due to the medical accident.
“Before I was injured, I enjoyed applying manicure and grooming. But when I tried to do it like the old days, it was so hard. After my injury, I tried to hang out with my friends, but it made me so annoyed. Because it was so hard. It would never be the same like before. My hands… My make-up was not right and I couldn’t even get dressed. (..) So I ended up giving up one by one.”
(Retrieved from the third transcription of the participant)
“To be honest, I have lots of resentments. My life has changed a lot because of this. If I got a proper compensation, if I go through the rehab, my body wouldn’t have been so damaged like this…”
(Retried from the third transcription of the participant)
For the participant preparing the model contest, the parole sentence for the lower half was no different from the death sentence. The dream of blooming age of 20 was cruelly frustrated by the medical accident. She did let herself become a prisoner of her own pain, however. As the rehabilitation and medical litigation were proceeded, she discovered her family’s debt. She in the face of life with disability was deeply concerned about their future. Through the financial difficulties caused by the rehabilitation and litigation, she has chosen a new career path in sports that also serve as the rehabilitation.
“I had to make a decision. Make decision about my job, and I had to exercise. I heard that if I work out, I do not have to go to the hospital to do my rehab. I focused on it because it seemed a better fit for me. I also heard that there are people who get pension as an Olympian… I thought that was also a possibility.”
(Retrieved from the second transcription of the participant)
The unexpected paralysis of the lower extremities changed the value of life as a woman for the participant. She received some ridiculous questions about her ability to give a birth at a date. Through this process, as a woman with disability, she lost her confidence in marriage and childbirth. She was constantly experiencing internal conflicts in fear of failure as she desired the marriage and childbirth.
“My seriously involved partner also asked me, he had no choice but to ask. (He said) It’s quite uncomfortable to ask, but can you give a birth or something like that, (…) It’s different from an ordinary situation because I have a disability. So I tend to talk about stuff that you don’t normally discuss at a first date. It was harder for me.. It was uncomfortable to meet someone naturally… Being open like that as well…”
(Retrieved from the third transcription of the participant)
Disability was more difficult for the participant who had an independent personality. Life with family was inseparable as she needed assistants even when she tried to cross a threshold. Different notions towards the disability sometimes made her family interfere with her life more than necessarily. Sometimes she was alone when she actually was in need of assistants. Moreover, her family also suffered conflicts during the medical litigation as it took more than six years. They were all exhausted and sometimes blamed each other. She felt a sense of disenchantment as she could not live on her own despite the enduring conflicts. The life of the family, which was constrained after the medical accident, was on a transition period as they were walking on a thin ice. The brief medical accident was affecting herself and her family’s life forever.
“My family fought a lot everyday. There was no solution. I couldn’t do anything… I was trapped for six years…”
(Retrieved from the first transcription of the participant)
“We all dwelled on what went wrong. My dad reproached my mom saying that why she suggested that specific hospital… My mom discovered the hospital first and we used to went there together when the accident happened… (Dad said) It happened because of you (mom)… He said something like that to her… Everybody was furious, and got tired and more tired… Dad on his own… Mom on her own… Everybody had a lot of mental stress… It was a quite difficult for them afterwards.”
(Retrieved from the third transcription of the participant)
A life with far more unexpected challenges as an athlete with disabilities
Life as an athlete was more than challenging. She experienced extreme frustration for injuries and financial difficulties as an athlete. She had to receive help from another athlete’s assistant as she could not afford to hire one for a long-distance training. She obtained a torn ligament and had to couch-surf at other person’s place as she had no regular income. She suffered conflicts with her coach as he did not comprehend her disability and made a financial demand for so-called training purpose. As she refused the demand, the coach showed absurd behaviours such as excluded her from the player’s list and more to her. Even after she transferred to another team, the coach with authority gave her new team disadvantages. Nothing came easy for her.
“I often got frustrated and become lethargic. I sometimes ask myself, what am I doing? I do that a lot. It gets hard when, (…) I have thoughts that I wish I have enough financial support and some mind to spare… I want to enjoy it (playing), but I cannot do that…”
(Retrieved from the third transcription of the participant)
“My previous team coach contacted my new coach to not accept me. My new coach can’t stop me from coming to the practice. But he won’t let me play with the team. So people involved in the team management were torn in between. My new coach said something like this. ‘I can’t stop you from coming here, but it’s going to be difficult to let you join us. I am sorry but it has to be done.’ He told me straightforward.”
(Retrieved from the second transcription)
As an athlete, chronic pain became a part of the participant’s endurance. She was also given a wrong degree of disability due to her invisible disability. Her training load was drastically increased to set good records as she received the wrong degree of disability. Significantly increased training load resulted chronic pain. As the pain spot was disclosed, holding a racket was beyond excruciating and it affected the performance. The degree of disability was only readjusted only after repeated reexaminations. Although the high-intensity training was altered after the adjustment, the participant’s body was already broken.
“When the pain spot is opened and it is touched by something, it hurts so much that I get goose bumps all over my body. I was told that I have to live with it as it is, although it hurts even with light touch. My joints are swollen and I can’t even hold the racket… My hands are in so much pain. It gets swollen, and it gets worse in the morning…”
(Retrieved from the second transcription of the participant)
The participant was emotionally damaged by the people involved in the sports regulation and management with their low understanding of her disability. She received the third the degree of disability with her invisible disability although her disability degree was close to the second one. With the degree of disability confirmation, her pain was not understood by the sports team officials. They forcefully applied training to her without understanding the physical condition of her, and as a result her muscles were all twisted. Nevertheless, she did not give up; she worked her fullest and achieved good records. Her degree of disability was adjusted to the second degree of disability after the reexamination. Some of her colleagues, however, had revolting perspectives of her or even criticized her as she already accomplished good records with the third degree of disability. The invisible disability became an obstacle to her life as an athlete.
“(I was told that) If I don’t get the skill, it’s my lost. (They told me to) Make it work. They didn’t get it. (They said) I can’t do it because I didn’t try it. (…) I told them it’s impossible, but they didn’t acknowledge it. They kept thinking that I need to lift up heavy things. They said I should let my knotted muscles as they are. But they weren’t knotted. Later I went to the hospital and found out that my muscles were all twisted. The muscles were stuck together like stones… A doctor loosened it with an injection. ”
(Retrieved from the second transcription of the participant)
Find new meaning after the medical accident
The participant has been living an extremely challenging life during the medical litigation and as an athlete after a medical accident. Love for herself and family was the reason why she did not fall even when she was fatigued sometimes. She vowed to change herself as she realized that the difficult environment would not be modified easily. She attempted to find meaning in her still unadapted life as a disabled person, instead of feeling resentment to the medical accident. Although it was a stagnant process, she claimed that her attitude towards life has gradually changed, unlike the gloom past. In addition, with the thought of her family’s support during the hardship, she could overcome and conquer whenever she felt defeated. She has been striving a zealous life to a be a dignified person with independence from her family. It took a long time for it to happen, but she wants to live healthier with the disabled.
“When it is hard, I have a sense of purpose… When my nephew was first born, I decided to live a life that was not shameful in front of him. It’s hard to see the end, so I do one step at a time. Sometimes it was too slow, getting farther away, and there was another crisis… It was hard. But I don’t want to depend on my parents when I get tired, I think to myself, I am almost there… To not see myself being dependent on my brother and my parents, I calm my mind down and overcame it. I think I overcame those processes.”
(Retrieved from the second transcription of the participant)
She wanted to pay all the blessings and helps that she has received forward with a kind-hearted responsibility. She felt pity whenever she encountered disabled people who wanted to give up on their lives; while there are disabled ones with good fortune ahead of them. Ambivalent feeling of empathy and frustration overwhelmed her as she witnessed people of disability who were constrained themselves in a rigid frame for their disability.
“I also wanted to finish my life, but when I see them being trapped in their own box, I felt some sorry and pity. I get a sense like ‘Why would they do that?’, I also have this notion of ‘because they are disabled’, but it’s not because they have disabilities. Regular people are also like that, but people with disabilities have big scars in their heart, so it give me pain to witness people with disabilities, including myself, in a closed box. I have been trying to give them a hand, but they weren’t able to really accept it, if they accept my help, I could do something for them. I wonder what could I do to help at least a little bit.”
(Retrieved from the third transcription of the participant)
“I think it’s good to do things that can have a good social impact.”
(Retrieved from the third transcription of the participant)
As the participant looked back at the six years of the medical litigation, she realized the entire process was no more than a journey without a map. She suffered hardships from medical and legal professions as well as disability-related compensation through the medical litigation. This process has led her to think that the hospital liability insurance system such as the traffic accident insurance is necessary as most of the medical accidents are caused by a doctor’s mistake. Despite a considerable number of medical accidents, it was regrettable that there was not a proper system related to the medical accident damage. She claimed that it is necessary to devote time on the issue and create countermeasures to improve the current circumstance.
“This country takes no part in the mediation. So, people who experienced a medical accident are repeatedly defeated again and again. (…) A medical license should be suspended if a doctor makes a serious mistake. There is no such thing. They (doctors) have a tight bond and have a way to get out. The whole system was built to victimize the people who were already hurt. So I think it’s best to make liability insurance mandatory. It is the lives of the parties that are directly connected to it. If the doctors make a severe mistake, they should be in a permanent suspension.”
(Retrieved from the first transcription of the participant)
Discussion
The purpose of this study is to understand how victims of medical accidents with medical litigation experiences live lives after medical accidents. It also attempts to demonstrate an overall comprehension of how the victims endeavour to manage problems facing their lives. The study is to suggest ways of intervention for the victims of medical accidents. Qualitative case study of Stake (1995) was applied to understand the special case of the experiences of the victim of medical accident (Stake, 1995). Data sources such as in-depth interviews with the victim who experienced physical injury in the medical accident and various medical cases and records were analyzed. As the results of the analysis, the experience of life after the accident of the medical accident for the victim of the medical accident were divided into six major experiences: “frustration and anger toward medical accident occurrence,” “desolated struggle for medical litigation,” “distrust of medical litigation related legal profession,” “accepting myself with a disability caused by a medical accident,” “a life with far more unexpected challenges as an athlete with disabilities,” and “find new meaning after the medical accident.” The main results are as follows.
First, the participant was judged to have paraplegia due to the unexpected the medical accident. She was experiencing a deep resentment towards the medical accident as she had to live as a disabled person for a lifetime due to the sudden accident. In addition, the attitude of the medical staff who did not speak frankly about the symptoms of her immediately after the medical accident gave a great psychological impact on her. Moreover, she experienced sadness, frustration, anxiety and depression that were difficult to cope with until she was diagnosed with her disability. The attitude of the medical staff that admitted his mistake at the time of the medical accident but changed gradually turned out to put her in anger and confusion. As a result, she had to deal with the practical difficulty of the medical litigation due to the obligation to disclose the occurrence of the medical accident and the medical staff’s fault before accepting her disability. In general, victims experiencing PTSD experience physical disturbances of sleep, cardiovascular, respiratory, musculoskeletal and neurological symptoms (McFarlane, Atchison, Rafalowicz, & Papay, 1994; Yu & Lee, 2012), and feelings of anxiety, social anxiety, loss of emotional control, avoidance, guilt, depressive symptoms, feeling of depreciation and more (Aimal, Lars, & Trond, 2011; Seo, Park, & Cho, 2015; Yang, Lee, Choi, & Kim, 2012; Yu & Lee, 2012). According to the study by Kim and colleagues (2017), the victims of medical accidents were selected as the complete PTSD symptom level after the incident, and the symptom severity of PTSD was significantly higher than those of other victims (Kim et al., 2017). This means that participants experienced avoidance, resentment, depression, and feeling of depreciation after a medical accident had PTSD due to the accident itself.
In addition, Pyo (2018) claimed that families affected by a medical accident experience complex feelings such as guilt, anxiety, and anger due to unclear details of medical accidents (Pyo, 2018). They were struggling with a particular process of medical litigation, with a sense of guilt, longing for the person who left, and responsibility to reveal the cause of death as the remaining family. This is similar to the experience of suffering from anger and anxiety by seeing the medical staff who blamed the psychological factors of the participant for the cause of the disability due to the unclear disability lesion. Moreover, the experience of going through the lawsuit with a desperate need to identify the cause with deep resentment of the medical accident resembles the previous study result (Pyo, 2018).
The participant who has been impaired by the unexpected accident was desperate and instinctive as she desired to clarify the cause of the accident. When faced with an unacceptable reality, it is possible to move to the next stage of confronting and accepting the reality only with a clear awareness of a situation. She remained, however, trapped at the moment of medical accident, despite the fact that over 10 years passed after the defensive attitude of the medical staff; they blamed the cause of the medical accident to her and did not clarify it distinctly. Experiences from the time of the disability diagnose immediately after the medical accident caused complex physical and psychological difficulties for her, resulting in negative results. Therefore, in order to prevent such negative consequences, it is necessary to provide a victim with an accurate explanation of the cause of an accident and an occurrence of an accident in an event of the medical accident. If a clear explanation by medical staff is provided institutionally to enable the victim of the medical accident to understand the occurrence of the incident, such as the “Disclosure of Patient Safety Incidents” system in some countries, the secondary psychological distress experienced by the victim will be alleviated (Ock, Choi, Jo, & Lee, 2017a; Ock, Kim, Jo, & Lee, 2016; Ock, Lim, Jo, & Lee, 2017b).
Second, the participant began the medical litigation to identify the cause of the unclear medical accident. She, however, said that the long-term litigation was the most frustrating experience without clear reasons for her disability after the medical accident. She experienced a change of beliefs in society as well as personal frustration. The defensive attitude of the medical staff exposed in the course of the medical litigation, the unfaithful attitude of the lawyer, and the inhuman and incomprehensible trial of the legal system contributed into her experiences. This experience is also similar to the result of the families suffering from medical accidents who experience distrust in the legal field in the course of medical litigation (Pyo, 2018).
Since a victim (plaintiff) is responsible for verifying a medical malpractice in the Korean legal system, the participant had to make a lot of effort to understand the medical accident. However, it is difficult to obtain professional medical information by the general public. In the reality that most of the evidences must be collected from the opponent; the only thing she could lean on was her lawyers and legal professions. Unfortunately, she suffered from the trial due to the careless mistakes of her lawyer. He told her to have a faith in him but was lack of understanding in medical litigation. In addition, her social beliefs were changed by experiencing unreasonable judging issues of the court and inhuman response to her. Taking this into consideration, attorneys need to manage the case based on an accurate understanding of a medical litigation, and they are required to hold an attitude to strive their best during the long litigation. Moreover, the legal profession needs to be more fair and transparent, and there is a need to refer to the precise precedent in the case of legal disputes over medical malpractice.
Third, the participant suffered from paraplegia resulted by the medical accident. Life as a disabled has frustrated her numerously. Ten years later, she still faces difficulties in everyday life. She has been repeatedly exposed to complex psychological distress such as fear, anxiety, resentment, and shame, as well as simple physical difficulties. She also encountered a change in social beliefs during the medical litigation for a period of six years. Long-term exposure to negative events that conflict with her basic beliefs can lead to Post Traumatic Embitterment Disorder (PTED). PTED is a reactive disorder caused by a specific environment or a negative experience that can occur in everyday life (Ko, Han, & Chae, 2014). She obtained a disability after the medical accident and languished in the inconsistency; it is between the basic beliefs and the events as unfair to the experiences she suffered during the medical litigation. This may result in the participant complaining of resentment, anger, and helplessness, similar to the symptoms of PTED, which continue negative emotions for unresolved dissonance (Ko et al., 2014).
She continued to rehabilitate to alleviate the exposed physical pain but disregarded the invisible psychological difficulties that were accumulated. Ignoring the psychological difficulties may result into intensified physical and psychological difficulties. A psychological recovery support program for this purpose could solve the followings: it will help to solve the psychological difficulties that the victim has suffered and to establish a positive self-image for the participant who lives an unexpected life as a person with disability. In the western countries such as the USA, the psychological trauma recovery support program has developed to apply to “the second victim” (Edrees et al., 2016). The second victims are medical staffs who caused a medical accident and they also experience psychological or physical difficulties similar to those of the first victim (Seys et al., 2013). However, psychological trauma recovery support program for first victims are not yet discussed. It is necessary to develop and apply a psychological recovery support program for first victims of medical accidents by referring to the programs for second victims and other types of programs, such as victims of crime.
The limitations and suggestions of this study are as follows. First, the study considered the difficulties of selecting participants due to the nature of medical accidents and medical litigations by taking the purposive sampling. As the purpose of this study was to comprehend the experiences of the victims of medical accidents in depth, a single qualitative case study methodology focusing only on one victim is appropriate. However, it was difficult to understand the experiences of various victims of medical accidents in multifaceted perspectives. In future studies, it is suggested to understand the experiences of the victims of medical accidents in more comprehensive terms considering the followings: the degree of damage caused by the medical accident, the suitability of the case, and the length of the litigation. Second, this study highlighted the experience of the victim who suffered the physical and permanent injury in the medical accident. Further research will help to establish a more systematic understanding of medical accidents by exploring the experiences of the first victims who have overcome them through treatment after being injured in a medical accident.
Biographies
Jeehee Pyo is a researcher with a master's degree in counseling and is interested in qualitative study and victims of medical accidents.
Minsu Ock is a assistant professor at University of Ulsan College of Medicine and is interested in qualitative study, victims of medical accidents, and healthy life expectancy.
Young-Joo Han is a associate Professor at Korea Counseling Graduate University and is interested in qualitative study.
Funding Statement
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (No. 2018R1C1B6005186).
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Aimal H., Lars W., & Trond H. (2011). psychiatric disorders and functional impairment among disaster victims after exposure to a natural disaster A population based study. Journal of Affective Disorders, 128, 135–12. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association (1994). Diagnostic and statistical manual of mental disorder (4th ed.). Washington, DC: Author. [Google Scholar]
- Edrees H., Connoers C., Paine L., Norvell M., Taylor H., & Wu A. W. (2016). Implementing the RISE second victim support programme at the Johns Hopkins Hospital: A case study. BMJ open, 6(9), e011708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guba E. G., & Lincoln Y. S. (1989). Fourth generation evaluation. Sage: Newbury Park: California. [Google Scholar]
- John W. C. (2017). Qualitative inquiry and research design: Choosing among five approacher (3rd ed.). Thousand Oaks, CA: Sage publications. [Google Scholar]
- Kang E. S., Kim J. M., Sung D. H., & Mok N. H. (2013). Review and improvement of alternative medical dispute resolution through case studies. Korea Journal of Hopital Management, 18(3), 106–125. [Google Scholar]
- Kim E. G. (2012). An analysis on the crisis management pr about medical dispute with a grounded theory. Korean Society For Journalism And Communication Studies, 8(3), 53–107. [Google Scholar]
- Kim N. Y., Lee S. R., Choi Y. E., & Sohn Y. W. (2017). Post Traumatic Stress Disorder (PTSD) in medical accident patients - the interaction effect of clinicians” explanation and attitude and social support. The Korean Journal of Culture and Social Issues, 23(2), 215–237. [Google Scholar]
- Kim Y. O., Park S. M., Park S. Y., Son M., & Sin K. S. (2009). How to conduct qualitative research. Seoul: Kyobobook. [Google Scholar]
- Ko H. S., Han C. S., & Chae J. H. (2014). Understanding of Posttraumatic Embitterment Disorder (PTED). Anxiety and Mood, 10(1), 3–10. [Google Scholar]
- Korea Medical Dispute Mediation and Arbitration Agency (2017). 2016 statistical yearbook of medical conflicts and arbitration. Seoup, Korea: Author. [Google Scholar]
- Kukmin ilbo (2018). Ewha Womans University Mokdong, Conflict over medical staff detention. 4.03.
- Lee W., Kim S. Y., & Lee M. J. (2014). Application of malpractice cause analysis tools for preventing repeat medical accident. Korean Journal of Medicine and Law, 22(1), 22–42. [Google Scholar]
- McFarlane A. C., Atchison M., Rafalowicz E., & Papay P. (1994). Physical symptoms in post-traumatic stress disorder. Journal of Psychiatric Research, 38, 715–726. [DOI] [PubMed] [Google Scholar]
- Newspaper S. (2016). Shin hae-cheol laws’ begin 30 days. Medical Dispute Mediation Process Start without Hospital Consent, 11, 22. [Google Scholar]
- Ock M. (2014). Development and evaluation of case review form for detecting adverse events (Master’s thesis) University of Ulsan College of Medicine. [Google Scholar]
- Ock M. (2016). Evaluating the feasibility of introducing open disclosure of patient safety incidents (Doctoral dissertation) University of Ulsan College of Medicine. [Google Scholar]
- Ock M., Choi E. Y., Jo M. W., & Lee S. I. (2017a). General public’s attitudes toward disclosure of patient safety incidents in Korea: Results of disclosure of patient safety incidents surveyⅠ. Journal of Paitent Safety. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ock M., Kim H. J., Jo M. W., & Lee S. I. (2016). Perceptions of the general public and physicians regarding open disclosure in Korea. BMC Medical Ethics, 17, 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ock M., Lim S. Y., Jo M. W., & Lee S. I. (2017b). Frequency, expected effects, obstacles, and facilitators of disclosure of patient safety incidents: A systematic review. Journal of Preventive Medicine and Public Health = Yebang Uihakhoe Chi, 50(2), 68–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park J. Y. (2011). Social recognition of medical accident. Journal of the Korean Medical Association, 54(10), 1000–1002. [Google Scholar]
- Pyo, J., Han, Y. J., Ock, M. (2018). A qualitative case study on the medical litigation experience of bereaved families due to medical accident. Korean Journal of Counseling, 19(5), 25–49. [Google Scholar]
- Seo Y. S., Park J. S., & Cho A. R. (2015). Review of assessment inventories for clinical disorders and symptoms caused by mass trauma events. Korean Journal of Counseling, 16(3), 557–580. [Google Scholar]
- Seys D., Wu A. W., Gerven E. V., Vleugels A., Euwema M., Pannella M., & Vanhaecht K. (2013). Health care professionals as second victims after adverse events: A systematic review. Evaluation and the Health Professions, 36(2), 135–162. [DOI] [PubMed] [Google Scholar]
- Stake R. E. (1995). The art of case study research. Thousand Oaks, CA: Sage. [Google Scholar]
- Yang M. H., Lee E. I., Choi J. W., & Kim H. J. (2012). PTSD and related factors among dispatched firefighters to rescue sites after the great Japanese earthquake (Running head: Dispatched firefighters’PTSD). Korean Journal of Occupational and Environmental Medicine, 24(2), 167–179. [Google Scholar]
- Yonhapnewstv (2016). ‘Shin Hae-cheol law’.. Serious medical accident, automatic dispute settlement commencement. 11.29.
- Yonhapnewtv (2017). A woman’s abdominal pain with cesarean section operation.. Gauze was found on her stomach 08.31.
- You G. W., Jeong J. W., Kim Y. S., & Kim H. B. (2016). Qualitative research methods. Seoul: PYbook. [Google Scholar]
- Yu M., & Lee J. (2012). The case study of play therapy for a sexual abused girl with PTSD. The Society for Cognitive Enhancement and Intervention, 3(2), 1–18. [Google Scholar]


