Abstract
Objectives:
To optimally select chronic pain patients for different treatments, it is of interest to identify patient characteristics that might moderate treatment effect. Our aim was to evaluate the impact of possible moderators on the effect of acupuncture treatment using a large data set.
Methods:
We used data from an individual patient data meta-analysis of high-quality randomized trials of acupuncture for chronic headache and migraine, osteoarthritis, and back, neck and shoulder pain. Using meta-analytic trial-level and patient-level regression analyses, we explored the impact of five documented patient characteristics (patients’ age at baseline, gender, pain duration, baseline pain severity and baseline psychological distress) on the effect of acupuncture.
Results:
A total of 39 trials met the inclusion criteria: 25 use sham acupuncture controls (n = 7,097) and 25 non acupuncture controls (n = 16,041). Of the five patient characteristics analyzed, only baseline pain severity was found to potentially moderate the treatment effect of acupuncture, with patients reporting more severe pain at baseline experiencing more benefit from acupuncture compared to either sham control or non acupuncture control. Baseline psychological distress showed small treatment moderating effects, and results for gender were inconsistent. There was no strong evidence that age or duration of pain influenced the response to acupuncture.
Discussion:
Of five patient characteristics tested, we found only baseline severity of pain to potentially moderate the effect of acupuncture treatment. For clinical practice, the evidence from this analysis does not justify stratifying chronic pain patients into subgroups that should or should not receive acupuncture on the basis of these five characteristics. Future acupuncture trials should assess other potentially important effect moderators.
Keywords: Effect moderators, Acupuncture, chronic pain, meta-analysis
Introduction
Acupuncture is commonly used to manage patients with chronic pain, and recent individual patient data meta-analyses including over 23,000 patients1 demonstrated that it to be more effective than both sham acupuncture and non-acupuncture control. However, acupuncture has only small specific effects1 and like all available treatments, it does not work for every chronic pain patient. To date, it is not well known whether and which baseline patient characteristics moderate the treatment effect of acupuncture. Such knowledge could be helpful for providing more stratified care by identifying the patients for whom acupuncture is likely to have the greatest effect. Knowledge about treatment-effect moderators can inform the development of clinical prediction rules and models of stratified care that target treatment to patient subgroups based on their likely response to specific treatment,2 ‘fast tracking’ patients to appropriate treatment and increasing healthcare efficiency.3
Indeed, the development of Comparative Effectiveness Research4 highlights the need to identify possible characteristics for stratified care. However, trials are typically designed to have sufficient power to test a primary hypothesis and therefore are underpowered for moderator analyses.5,6 To detect characteristics that modify the effect of treatment on the primary outcome, the sample size needs to be at least four times larger than that for the primary hypothesis.7 Our large database,1 with individual patient data from nearly 40 randomized trials, could overcome this problem and allow us to explore potential acupuncture treatment effect moderators. The trials included in this dataset are high quality trials from different countries; the UK, Germany, Sweden, Spain and USA. Overall the dataset has good external validity, because it includes trials involving different acupuncture providers (acupuncturists, physiotherapists and medical doctors), different control groups (sham acupuncture, usual care, guideline-based care and no treatment) and different acupuncture treatment protocols (standardized, semi-standardized and fully individualized). Elsewhere we have examined characteristics of acupuncture that moderate treatment effects.8 Here we evaluate patient and pain characteristics as well as psychological distress as potential moderating factors for acupuncture treatment.
Materials and Methods
Included Trials
Trials included in the dataset and used for these analyses were identified through a systematic literature review that has been previously described.1,9 The analysis included trials of acupuncture for chronic pain published prior to December 31, 2015 wherein allocation concealment was determined unambiguously to be adequate. Eligible pain types were non-specific back or neck pain of at least four weeks duration, shoulder pain, chronic headache or osteoarthritis. This search resulted in the identification of potentially 44 randomized trials.
Data Acquisition
Individual patient data were obtained from only 39 trials. Data on the trial-level characteristics of the acupuncture intervention were obtained directly from trialists. Twenty-six trials had a sham acupuncture control group, and twenty-five trials had a non-acupuncture control group. One trial with both sham acupuncture and no acupuncture control arms was excluded from the sham acupuncture analysis due to a high risk of bias due to unblinding.10
Outcome
The primary outcome used for this analysis was the primary outcome defined by the study authors. For the 39 trials, 22 used a pain measure as primary outcome, the other trials used measures on function or an index measure that combines both. However, if the primary outcome as defined by the study authors was categorical, we used a continuous measure of pain taken at the same time point as the original outcome. To make the various outcome measurements comparable between different trials, the primary endpoint outcome for each trial was standardized by dividing by pooled standard deviation.
Potential treatment moderators
The following five baseline patient characteristics were consistently available in the dataset and were explored as potential acupuncture treatment moderators: age at baseline, gender, pain duration, pain severity and psychological distress. All 39 trials collected data on baseline pain, with three trials reporting none of the other patient characteristics. Twenty trials had data on all five patient characteristics. Information on pain duration was provided by the patient and collected at the start of the trials. Trials that only provided information on pain duration in categories (i.e. more or less than 5 years) were not included in these analyses. Baseline pain severity was measured using the same methods as the outcome variable. Baseline pain scores were standardized by dividing by the pooled standard deviation of the measure among the controls, separately for each trial. The measure used to capture baseline psychological distress varied by trial and included the mental component from the 12 and 36-item Short Form Health Survey (SF-12 & SF-36) and the Hospital Anxiety and Depression Scale (HADS). One trial that measured baseline depression on a three-point scale (inconspicuous, borderline, and conspicuous depression)11 was excluded since all other measures were on a continuous scale. In order to combine the different measures, scores were standardized in the same way as the outcome variable, by dividing by pooled standard deviation.
Statistical Methods
We used two different statistical approaches to determine whether our findings were sensitive to the method of analysis. In the trial-level meta-analytic approach, we created a linear regression for each trial as for the main analysis of effect size, but also included the patient characteristic and an interaction term between the characteristic and treatment allocation. The coefficient and standard error for the interaction term represents the change in the outcome score in standard deviations associated with the patient characteristic in the acupuncture treatment group. The coefficient and standard error were then entered into a meta-analysis, using the Stata command metan. For example, this trial-level analysis addresses questions about effect moderation such as: “Do patients who are older have a better or worse response to acupuncture compared to control treatment than younger patients?” Analyses were conducted separately for sham and non-acupuncture controls. A sensitivity analysis was conducted excluding a set of three outlying trials,12–14 as described in the main publication.
In the second approach, using the patient-level, instead of testing for effect moderation in each trial and combining the results into a meta-analysis, we combined the 39 trials and ran a single regression model for each control arm comparison (non-acupuncture and sham acupuncture controls). The regression model included treatment arm, patient characteristic, the interaction between treatment and patient characteristic, and trial as a fixed effect covariate. A sensitivity analysis was performed using the same model adjusted for pain type (headache, osteoarthritis, low back pain and neck pain, or shoulder pain), rather than by individual trial.
To model the effects of baseline pain on acupuncture treatment effect, we created separate models for acupuncture and control treatment groups, predicting change in pain score in terms of baseline pain. Restricted cubic splines with knots at the tertiles were used to allow for non-linearity. All analyses were conducted using Stata 13 (Stata Corp., College Station, TX).
Results
Depending on the analyses, between 11 trials (n=3,828 patients) and 25 trials (n=14,222) were included. The effects of the five baseline patient characteristics on acupuncture treatment effect from the trial-level meta-analysis are shown in Table 1. In trials with a non-acupuncture control, pain intensity, gender and psychological distress were found to significantly moderate the treatment effect of acupuncture, but there were no significant effects of age or duration of pain. The estimates reported in the table are the standardized difference in the effect of acupuncture compared to controls for each characteristic; a positive β indicates a larger effect of acupuncture compared to controls for patients with the given characteristic versus the referent level of the characteristic. For instance, the β of 0.034 for baseline psychological distress means that a patient with psychological distress one standard deviation higher than the mean will experience an improvement in pain from acupuncture of 0.034 standard deviations more than average. Because the average effect size for acupuncture compared to a non-acupuncture control is approximately 0.50 standard deviations, this means that the moderating effects of psychological distress and gender are relatively small. The acupuncture moderating effect of baseline pain is somewhat larger: the more severe the pain, the relatively greater the reduction in pain for those patients receiving acupuncture in comparison to control treatments. For example, a patient with baseline pain 2 SD more severe than the mean, experienced about 1.5 times (0.50 effect size + (2 SD × β 0.151) = 0.802 = approximately 1.5 fold effect) the benefit of acupuncture compared to a patient with a baseline pain score at the mean (Figure 1).
Table 1. Trial-Level Fixed-Effects Meta-Analysis.
The β can be interpreted as the difference in the effect of acupuncture in standard deviations. For instance, the β of −0.079 for male gender in trials with non acupuncture control means that, on average, the difference between acupuncture and non acupuncture was 0.079 standard deviations lower for men
| FIXED EFFECTS: Coefficients for interaction terms | ||||||||
|---|---|---|---|---|---|---|---|---|
| ACUPUNCTURE VS. NON-ACUPUNCTURE | ACUPUNCTURE VS. SHAM | |||||||
| Number of trials included | β | 95% CI | p | Number of trials included | β | 95% CI | p | |
| Baseline pain intensity (per 1 SD) | 25 | 0.151 | 0.126, 0.177 | <0.0001 | 25 | 0.073 | 0.030, 0.117 | 0.001 |
| Excluding outlying trials | 22 | 0.073 | 0.027, 0.119 | 0.002 | ||||
| Age (per 10 years) | 25 | −0.012 | −0.033, 0.008 | 0.2 | 22 | 0.030 | −0.010, 0.069 | 0.14 |
| Excluding outlying trials | 19 | 0.022 | −0.019, 0.064 | 0.3 | ||||
| Male | 25 | −0.079 | −0.134, −0.024 | 0.005 | 22 | 0.151 | 0.052, 0.250 | 0.003 |
| Excluding outlying trials | 19 | 0.152 | 0.049, 0.255 | 0.004 | ||||
| Duration (per 5 years) | 18 | −0.002 | -0.017, 0.014 | 0.8 | 16 | 0.005 | −0.027, 0.037 | 0.8 |
| Excluding outlying trials | 13 | 0.002 | −0.031, 0.035 | 0.9 | ||||
| Baseline psychological distress (per 1 SD) | 20 | 0.034 | 0.007, 0.061 | 0.013 | 13 | −0.022 | −0.077, 0.033 | 0.4 |
| Excluding outlying trials | 11 | −0.018 | −0.074, 0.039 | 0.5 | ||||
Figure 1:
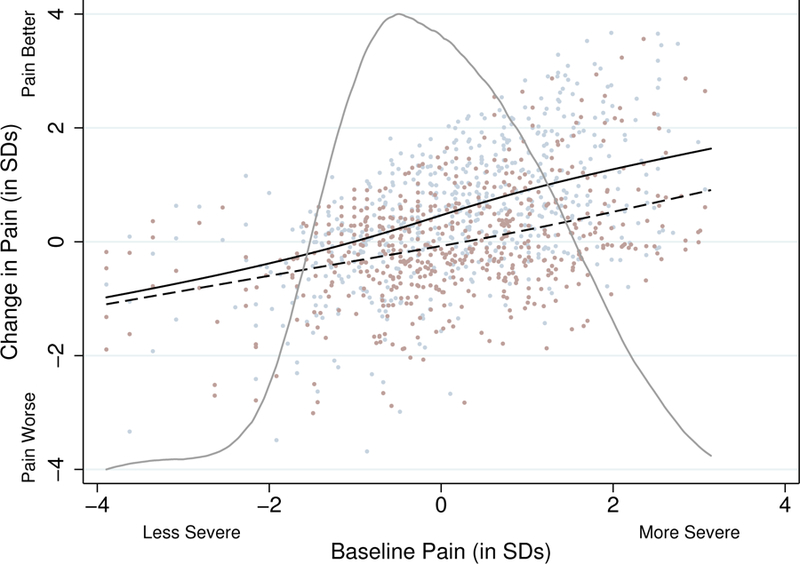
Change in pain from baseline in non-acupuncture controlled trials
When comparing acupuncture to sham acupuncture, baseline pain intensity and gender remained statistically significant moderators of the treatment effect of acupuncture. By contrast psychological distress was not a treatment effect moderator when the comparison group was sham acupuncture. Interestingly, the acupuncture moderating effect of gender appears reversed, with men receiving greater reductions in pain than women, showing that the treatment moderating effect of gender is not consistent throughout the analyses. Moreover, age and duration of pain were not statistically significant effect moderators.
In the patient-level regression analysis (Table 2), these results were similar to the meta-analytic model for trials with non-acupuncture control groups. However, among these trials, there was some evidence that the difference between acupuncture and non-acupuncture treatment was larger for older patients, although this did not reach conventional levels of statistical significance (β 0.018 per 10 years of age, 95% CI −0.001, 0.037, p=0.066).
Table 2. Patient-Level Regression Analysis for Effect Moderators, adjusting for trial.
The β can be interpreted as the difference in the effect of acupuncture in standard deviations. For instance, the β of −0.057 for male gender in trials with non acupuncture control means that, on average, the difference between acupuncture and non acupuncture was 0.057 standard deviations lower for men.
| Regression Coefficients for Interaction Terms | ||||||||
|---|---|---|---|---|---|---|---|---|
| ACUPUNCTURE VS. NO ACUPUNCTURE | ACUPUNCTURE VS. SHAM | |||||||
| Number of trials (patients) included | β | 95% CI | p | Number of trials (patients) included | β | 95% CI | p | |
| Baseline pain intensity (per 1 SD) | 25 (14,222) | 0.139 | 0.118, 0.159 | <0.0001 | 25 (6,597) | 0.033 | 0.009, 0.057 | 0.006 |
| Excluding outlying trials | 22 (5,985) | 0.015 | −0.010, 0.039 | 0.2 | ||||
| Age (per 10 years) | 25 (14,218) | 0.018 | −0.001, 0.037 | 0.066 | 22 (6,392) | 0.024 | −0.006, 0.053 | 0.11 |
| Excluding outlying trials | 19 (5,780) | 0.013 | −0.017, 0.042 | 0.4 | ||||
| Male | 25 (14,222) | −0.057 | −0.114, −0.001 | 0.047 | 22 (6,398) | 0.137 | 0.039, 0.234 | 0.006 |
| Excluding outlying trials | 19 (5,786) | 0.176 | 0.076, 0.276 | 0.001 | ||||
| Duration (per 5 years) | 18 (12,386) | −0.005 | −0.020, 0.010 | 0.5 | 16 (4,572) | −0.026 | −0.055, 0.003 | 0.081 |
| Excluding outlying trials | 13 (3,960) | 0.001 | −0.029, 0.031 | 0.9 | ||||
| Baseline psychological distress (per 1 SD) | 20 (12,531) | 0.030 | 0.004, 0.056 | 0.025 | 13 (4,031) | 0.054 | 0.005, 0.103 | 0.031 |
| Excluding outlying trials | 11 (3,828) | 0.012 | −0.039, 0.062 | 0.7 | ||||
In sham-controlled trials, the β values for interaction terms and p-values were similar for both models for most characteristics. While significant in both models, the β value for the interaction between baseline pain and treatment group was smaller in the patient-level regression model (β 0.033 per 1SD vs β 0.075 per 1 SD). The β value for this interaction was smaller and non-significant after excluding outlying trials (β 0.015 per 1SD, p=0.2). The association between baseline pain and pain change scores for both acupuncture and sham acupuncture groups are shown in Figure 1 and 2. There was evidence of an interaction in the patient-level regression models for two characteristics that were not seen in the meta-analytic models. First, there was some evidence that pain duration moderated acupuncture treatment effect in the regression model (β −0.026, 95% CI −0.055, 0.003, p=0.081), although this did not meet conventional levels of statistical significance and was sensitive to the exclusion of outlying trials (p=0.9). Second, baseline psychological distress significantly moderated the effect of acupuncture (β 0.054, 95% CI 0.005, 0.103, p=0.031). This association is, however, small and was also highly sensitive to the exclusion of outlying trials (p=0.7). The patient-level models that adjusted for pain type rather than trial produced results consistent with the other two analyses (data not shown).
Figure 2:
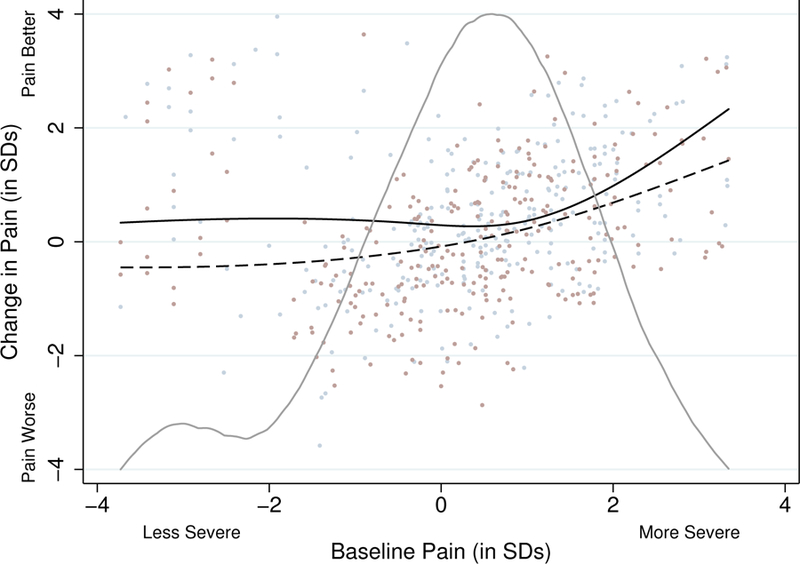
Change in pain from baseline in sham-controlled trials
We found that female patients who received acupuncture did better than males in trials with non-acupuncture control groups, while male acupuncture patients did better in trials with sham acupuncture controls. In an attempt to explain this finding, we performed several exploratory analyses. The first sensitivity analysis included only trials that used both non-acupuncture and sham acupuncture control arms. A total of 11 trials were included in this analysis: 3,792 patients in the analysis of non-acupuncture control trials, and 4,246 patients in the analysis of sham controlled trials. In the analysis of sham controlled trials, both the meta-analysis (β 0.159, 95% CI 0.039, 0.278, p=0.009) and the patient-level regression (β 0.194, 95% CI 0.078, 0.311, p=0.001) found a large benefit of acupuncture in male patients compared to females. In non acupuncture control trials, the meta-analysis (β 0.000, 95% CI −0.125, 0.126, p > 0.9) and the patient-level regression (β 0.068, 95% CI −0.059, 0.195, p=0.3) found no evidence of effect moderation based on gender. However, effect sizes for both patient-level regression analyses indicated a benefit of acupuncture for males, and the effect size in sham controlled trials was consistent with the main analysis, indicating that the differential effect of gender seen in the main analysis is likely driven by the four large Acupuncture in Routine Care (ARC) trials from Germany. These trials with a total of 10,106 patients had only a non-acupuncture control group and found that women had an improved response to acupuncture compared to men.15
To investigate this further, we then performed a sensitivity analysis excluding those 10,106 patients. In this sensitivity analysis, the β for the interaction between gender and acupuncture group from the meta-analysis for non-acupuncture control was again non-significant and close to the null (β −0.003, 95% CI −0.106, 0.101, p > 0.9). In the patient-level regression model, the β for the 5,202 patients remaining in the analysis was in the same direction as the effect seen in sham trials, but the effect size was small compared to the effect seen in the sham analysis and was not statistically significant (β 0.036, 95% CI −0.069, 0.140, p=0.5).
In previous papers8,9 we found evidence that an increased number of acupuncture needles or acupuncture treatment sessions could improve the benefit of acupuncture. Based on our analysis which found an increased benefit of acupuncture for those with higher baseline pain, we then investigated whether patients with the highest levels of baseline pain received higher doses of acupuncture, that is, whether the association between baseline pain and outcome was confounded by patients reporting high pain levels being given more acupuncture. We created linear regression models with baseline pain severity as a covariate for two outcomes: average number of acupuncture needles used per session and total number of acupuncture sessions. Models were created separately for each trial and included only patients in the acupuncture group. Since only patients in the acupuncture group were eligible, both non-acupuncture and sham acupuncture-controlled trials were included. For each outcome, the coefficient and standard error for baseline pain were saved out from each trial and entered into a meta-analysis.
We found a statistically but not clinically significant association between baseline pain and number of acupuncture sessions, with an overall estimate of an additional 0.10 sessions associated with a 1SD increase in baseline pain (95% CI 0.04, 0.15, p=0.001). There was no evidence of an association between baseline pain and average number of needles used per session (0.014 needles per 1SD increase in baseline pain, 95% CI −0.16, 0.19, p=0.9).
Discussion
Findings
Patients with chronic pain participating in acupuncture trials respond differently to the acupuncture treatment. We evaluated five possible acupuncture treatment effect moderators. By using individual patient data meta-analyses on a large international data set of randomized trials we were able to conduct well-powered analyses. Furthermore, we employed several secondary analyses to check our results for robustness.
Of the five patient variables available in the dataset, only baseline pain severity was found to have a consistent moderating effect on acupuncture outcomes, patients reporting more severe pain at baseline experiencing more benefit from acupuncture than comparison treatments. The size of these effects varied with the control groups used: larger effects were observed when patients were not blinded to the intervention. Age or duration of pain do not seem to moderate the response to acupuncture. In several analyses, baseline psychological distress showed small acupuncture treatment moderating effects. The most inconsistent results were found for gender showing that men benefit more from acupuncture in sham controlled trials and women more in non-acupuncture group controlled trials. Sensitivity analyses showed that the moderating effect of female gender was mainly driven by four large open label trials from one country and not consistent for other trials.
Advantages and limitations
Our results are based on a very large dataset consisting of high quality randomized trials from different countries, providers and acupuncture protocols. In contrast to typical meta-analyses, individual patient data allows for sensitivity analyses with adjustment for the trial and type of chronic pain to examine the robustness of our conclusions. To identify possible characteristics associated with patients that could lead to stratified care, we wanted to examine as many possible characteristics. The main limitation was data availability. We could only examine the five baseline variables (age, gender, pain duration, pain severity and psychological distress) that were available in a standardised format for most of the trials. Additional patient characteristics that might plausibly influence acupuncture effect, for instance, presence of neuropathic pain, were not measured in the primary trials. Other patient characteristics, such as psychological distress, were measured using inconsistent endpoints, requiring that they had to be combined in a sub-optimal manner. For instance, we examined the properties of psychological distress overall, rather than, examining anxiety and depression separately. In an observational cohort study of 1591 low back pain patients consulting in primary care a considerable overlap in psychological measures commonly used in low back pain research was confirmed.16 Yet other important patient characteristics, that potentially may be moderators of the effects of acupuncture compared to other treatments such as level of education, pain catastrophizing and self-efficacy could not be examined in the analyses, because these constructs were collected in very different ways in different studies and were not collected at all in many trials. However, results of a pooled analysis using four German-based trials, all of which are included in our study, found that level of education predicted the outcome independent of the intervention and was therefore not an acupuncture effect moderator.15 Because the number of older adults in the data set was limited, the findings that the difference between acupuncture and non-acupuncture treatment might be larger for older adults should be interpreted with caution.
Comparison with other studies
We found that patients with more severe pain at baseline improved more from acupuncture treatment than those with lower levels of pain, compared to other treatments. Previous studies have reported baseline pain to predict the outcome independent of the intervention and not, as in our current analysis, as a treatment effect moderator.15,17,18 Such trials explained effects in terms of regression to the mean, or to floor effects at baseline, which diminish the possibility of improvements in pain levels as a result of treatment. Overall the evidence for mediating factors for treatments in musculoskeletal pain populations is still limited.19
In these meta-analyses, baseline psychological distress was a statistically significant treatment effect moderator in several analyses. Patients with greater psychological distress at baseline experienced greater benefit from acupuncture. This is the first time this effect has been identified for acupuncture treatment. However, the effect is small and of questionable clinical relevance. As a result, exclusion of patients with low psychological distress from acupuncture treatment or acupuncture trials cannot be justified.
That age and pain duration did not moderate the treatment outcome is in agreement with previous acupuncture studies.15 The influence of gender on pain reduction was inconsistent and seemed to depend on the types of trials included into the analyses. When excluding the large German trials with a non-acupuncture control it seems that men benefit more, however, this was mainly based on sham-controlled data. Because of the inconsistency of the data and the overall small size of the treatment moderating effect the current evidence does not justify using gender as stratification factor in clinical practice.
Implications for research and practice
Future acupuncture trials should assess other potentially important effect moderators, such as treatment outcome expectation20 and pain self-efficacy21, that were only available for very few trials in our data set. Future trials should also assess objective variables that might either serve directly as acupuncture treatment effect moderators (e.g., whether pain is predominately neuropathic or nociceptive) or serve as markers of treatment effect, such as cytokines or genetics. For clinical practice the current evidence provides no justification for stratifying patients in groups that should or should not receive acupuncture.
Acknowledgments
Funding source: The Acupuncture Trialists’ Collaboration is funded by an R21 (AT004189I and an R01 (AT006794) from the National Center for Complementary and Alternative Medicine at the National Institutes of Health to Dr. Vickers) and by a grant from the Samueli Institute. Dr. MacPherson’s work on this project was funded in part by the National Institute for Health Research (NIHR) under its Programme Grants for Applied Research scheme (RP-PG-0707–10186). Prof. Foster, an NIHR Senior Investigator, was supported through an NIHR Research Professorship (RP-011–015). The views expressed in this publication are those of the author(s) and not necessarily those of the National Center for Complementary and Alternative Medicine, NHS, NIHR, or the Department of Health in England. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the report.
Acupuncture Trialists’ Collaboration Members
Claire Allen, BA, Evidence Aid, Oxford, United Kingdom.
Brian Berman, MD, University of Maryland School of
Medicine and Center for Integrative Medicine, Baltimore, Maryland
Benno Brinkhaus, MD, Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center, Berlin, Germany.
Remy Coeytaux, MD, PhD, Department of Community and Family Medicine, Duke University, Durham, North Carolina.
Hans-Christoph Diener, MD, PhD, Department of Neurology, University of Duisburg-Essen, Germany.
Heinz G. Endres, MD, Ruhr-University Bochum, Bochum, Germany.
Nadine E. Foster, DPhil, BSc(Hons), Arthritis Research UK Primary Care Centre, Research Institute of Primary Care and Health Sciences, Keele University, Newcastle-under-Lyme, Staffordshire, England.
Michael Haake, MD, PhD, Department of Orthopedics and Traumatology, SLK Hospitals, Heilbronn, Germany.
Rana S. Hinman, PhD, University of Melbourne, Melbourne, Australia.
Dominik Irnich, MD, Multidisciplinary Pain Centre, Department of Anesthesiology, Ludwig-Maximilians- Universität München (LMU Munich),Germany.
Wayne B. Jonas, MD, Samueli Institute, Alexandria, Virginia.
Kai Kronfeld, PhD, Interdisciplinary Centre for Clinical Trials (IZKS Mainz), University Medical Centre Mainz, Mainz, Germany.
Lixing Lao, PhD, University of Maryland and Center for Integrative Medicine, Baltimore, Maryland.
George Lewith, MD, FRCP, Primary Care and Population Sciences, Faculty of Medicine, University of Southampton, Southampton, England.
Klaus Linde, MD, Institute of General Practice, Technical University Munich, Munich, Germany.
Hugh MacPherson, PhD, Professor of Acupuncture Research, Department of Health Sciences, University of York, York, England.
Eric Manheimer, MS, Center for Integrative Medicine, University of Maryland Baltimore, Maryland
Dieter Melchart, MD, PhD, Competence Centre for Complementary Medicine and Naturopathy, Technical University Munich, Munich, Germany.
Albrecht Molsberger, MD, PhD, German Acupuncture Research Group, Duesseldorf, Germany.
Karen J. Sherman, PhD, MPH, Group Health Research Institute, Seattle, Washington.
Maria Suarez-Almazor, MD, PhD, M.D. Anderson Cancer Center, Houston, Texas.
Hans Trampisch, PhD, Department of Medical Statistics and Epidemiology, Ruhr-University Bochum, Germany.
Jorge Vas, MD, PhD, Pain Treatment Unit, Dos Hermanas Primary Care Health Center (Andalusia Public Health System), Dos Hermanas, Spain.
Andrew J. Vickers (collaboration chair), DPhil, Memorial Sloan Kettering Cancer Center, New York, New York.
Peter White, PhD, School of Health Sciences, University of Southampton, England.
Lyn Williamson, MD, MA (Oxon), MRCGP, FRCP, Great Western Hospital, Swindon, United Kingdom.
Stefan N. Willich, MD, MPH, MBA, Institute for Social Medicine, Epidemiology and Health Economics, Charité University Medical Center, Berlin, Germany.
Claudia M. Witt, MD, MBA, Institute for Complementary and Integrative Medicine, University of Zurich and University Hospital Zurich, Zurich, Switzerland; Institute for Social Medicine, Epidemiology and Health Economics, Charite-Universitätsmedizin, Berlin, Germany; Center for Integrative Medicine, University of Maryland School of Medicine, Baltimore, Maryland
Contributor Information
Claudia M. Witt, University of Zurich and University Hospital Zurich, Zurich, Switzerland; Institute for Social Medicine, Epidemiology, and Health Economics, Charité – Universitätsmedizin Berlin, corporate member of Freie Universität Berlin, Humboldt-Universität zu Berlin, and Berlin Institute of Health, Berlin, Germany; University of Maryland School of Medicine, Baltimore, Maryland.
Emily A. Vertosick, Memorial Sloan Kettering Cancer Center, New York, NY.
Nadine E. Foster, Keele University, Staffordshire, UK.
George Lewith, University of Southampton, Southampton, UK.
Klaus Linde, Technical University Munich, Germany.
Hugh MacPherson, University of York, York, UK.
Karen J. Sherman, Kaiser Permanente Washington Health Research Institute and University of Washington, Seattle, WA.
Andrew J. Vickers, Memorial Sloan Kettering Cancer Center, New York, NY.
References
- 1.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172(19):1444–1453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Foster NE, Hill JC, O’Sullivan P, Hancock M. Stratified models of care. Best practice & research Clinical rheumatology 2013;27(5):649–661. [DOI] [PubMed] [Google Scholar]
- 3.Hingorani AD, Windt DA, Riley RD, et al. Prognosis research strategy (PROGRESS) 4: stratified medicine research. BMJ 2013;346:e5793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Conway PH, Clancy C. Comparative-Effectiveness Research -- Implications of the Federal Coordinating Council’s Report. N Engl J Med 2009;361(328):330. [DOI] [PubMed] [Google Scholar]
- 5.Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine 1976;29(11):1167–1172. [DOI] [PubMed] [Google Scholar]
- 6.Underwood MR, Morton V, Farrin A. Do baseline characteristics predict response to treatment for low back pain? Secondary analysis of the UK BEAM dataset [ISRCTN32683578]. Rheumatology (Oxford, England) 2007;46(8):1297–1302. [DOI] [PubMed] [Google Scholar]
- 7.Brookes ST, Whitely E, Egger M, Smith GD, Mulheran PA, Peters TJ. Subgroup analyses in randomized trials: risks of subgroup-specific analyses; power and sample size for the interaction test. J Clin Epidemiol 2004;57(3):229–236. [DOI] [PubMed] [Google Scholar]
- 8.MacPherson H, Maschino AC, Lewith G, Foster NE, Witt C, Vickers AJ. Characteristics of acupuncture treatment associated with outcome: an individual patient meta-analysis of 17,922 patients with chronic pain in randomised controlled trials. PloS one 2013;8(10):e77438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vickers AJ, Vertosick EA, Lewith G, et al. Acupuncture for chronic pain: update of an individual patient data meta-analysis. J Pain 2018;19(5):455–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinman RS, McCrory P, Pirotta M, et al. Acupuncture for chronic knee pain: a randomized clinical trial. JAMA 2014;312(13):1313–1322. [DOI] [PubMed] [Google Scholar]
- 11.Irnich D, Behrens N, Molzen H, et al. Randomised trial of acupuncture compared with conventional massage and “sham” laser acupuncture for treatment of chronic neck pain. BMJ 2001;322(7302):1574–1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vas J, Mendez C, Perea-Milla E, et al. Acupuncture as a complementary therapy to the pharmacological treatment of osteoarthritis of the knee: randomised controlled trial. Bmj 2004;329(7476):1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vas J, Ortega C, Olmo V, et al. Single-point acupuncture and physiotherapy for the treatment of painful shoulder: a multicentre randomized controlled trial. Rheumatology (Oxford) 2008;47(6):887–893. [DOI] [PubMed] [Google Scholar]
- 14.Vas J, Perea-Milla E, Mendez C, et al. Efficacy and safety of acupuncture for chronic uncomplicated neck pain: a randomised controlled study. Pain 2006;126(1–3):245–255. [DOI] [PubMed] [Google Scholar]
- 15.Witt CM, Schützler L, Lüdtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clin J Pain 2011;27(6):550–555. [DOI] [PubMed] [Google Scholar]
- 16.Campbell P, Bishop A, Dunn KM, Main CJ, Thomas E, Foster NE. Conceptual overlap of psychological constructs in low back pain. Pain 2013;154(9):1783–1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sherman KJ, Cherkin DC, Ichikawa L, et al. Characteristics of patients with chronic back pain who benefit from acupuncture. BMC Musculoskelet Disord 2009;10(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Glazov G The influence of baseline characteristics on response to a laser acupuncture intervention: an exploratory analysis. Acupunct Med 2010;28(1):6–11. [DOI] [PubMed] [Google Scholar]
- 19.Mansell G, Kamper SJ, Kent P. Why and how back pain interventions work: what can we do to find out? Best practice & research Clinical rheumatology 2013;27(5):685–697. [DOI] [PubMed] [Google Scholar]
- 20.Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain 2007;128(3):264–271. [DOI] [PubMed] [Google Scholar]
- 21.MacPherson H, Tilbrook H, Richmond S, et al. Alexander Technique lessons or acupuncture sessions for persons with chronic neck pain: a randomized trial. Annals of internal medicine 2015;163(9):653–662. [DOI] [PubMed] [Google Scholar]


