Abstract
Background:
Point of care tests (POCTs) for reproductive health conditions have existed for decades. Newer POCTs for syphilis, HIV and trichomonas are currently available and easy-to-use. We surveyed practicing ob-gyns to determine POCT current use and perceived obstacles to use.
Methods:
Between June and August 2016, 1000 members of the American College of OBGYN were randomly selected and invited to complete a Qualtrics survey: 600 were members of the Collaborative Ambulatory Research Network (CARN). Respondents who completed at least 60% of the survey were included in the analysis.
Results:
749 members had valid emails; 288 (39%) participated in and completed the survey. 70% were male, and average years practicing was 18. 30% reported diagnosing sexually transmitted infections (STIs) 1–2 times/week and 45% reported 1–2 times/month. POCTs used included pregnancy test (83%), urine dipstick (83%), wet mount test (79%) and the vagina pH test (54.8%). Few used Gram stain (5%) and stat RPRs (4%). Relatively newer FDA-approved POCTs were used less frequently with 25% reporting Affirm VPIII test use and only 10% using a rapid HIV test. The most common perceived barriers were the amount of reimbursement received for performing the test (61.9%) and the payment coverage from the patient (61.3%).
Conclusions:
U.S. ob-gyns rely on laboratory test results and traditional POCTs to diagnosis STDs. Future development and marketing of POCTs should consider not only ease and time of test performance but also cost of tests to the practice and the patient, as well as reimbursement.
Keywords: Point of Care Tests, Obstetricians, Gynecologists
Introduction
Point of care (POC) tests, sometimes referred to as rapid diagnostic tests or near patient tests, have become very sensitive and specific over the past decade, especially in diagnosing sexually transmitted infections. Reviews report the consensus that traditional diagnostics, such as microscopy and culture, and syndromic management are not sufficient tools for diagnosing STIs, highlighting the need for rapid, accurate diagnostic tests for STIs (1–3). Yet, older methods and syndromic management continue to be used. Although POC tests have been developed to detect Chlamydia trachomatis, Neisseria gonorrhoeae, and herpes simplex virus using lateral flow assays in a POC laboratory and by RT-PCR assays, which can be done as near patient tests with results generally available within 90 minutes, these tests are not widely used in clinical practices in the United States. POC tests for syphilis, HIV and vaginal discharge etiologies (candida, bacterial vaginosis, and trichomoniasis), which can be read in 10 to 45 minutes, are FDA-approved and available to clinicians (2,3). Even though studies and systematic reviews of point of care testing for STIs report that POC testing is acceptable to providers and patients and is also demonstrated to be cost effective, (4–7), it is unclear if available POC tests for STIs are actually being used and if so, what tests and by whom. With this rapidly developing technology, which aspires to decrease overtreatment, complications, and transmission events by facilitating immediate and specific treatment of STIs, the question is: Are clinicians adopting STI POC testing strategies? In the United States over the past decade, many women are presenting to specialty practices rather than STI clinics for STI services (8). In order to determine if Obstetricians and Gynecologists are adopting STI POC tests and to determine what obstacles to POC test use may exist among current practicing reproductive health providers, we conducted a survey of members of the American College of Obstetricians and Gynecologists who were actively involved in patient care.
Methods
Sample and Study Design
Of the 1000 members of the American College of Obstetricians and Gynecologists (ACOG) selected to participate in this study, 600 were members of the Collaborative Ambulatory Research Network (CARN). CARN is a group of practicing ACOG members who voluntarily participate in survey research conducted by the ACOG Research Department (9). Part of the original impetus for the CARN was the observation that a substantial portion of information about medical care was derived from hospital-based research and surveys among active clinicians have poor representiveness due to low response rates. The CARN project was designed as a way to discern the practice trends and knowledge base of Ob-Gyns practicing in the ambulatory care setting. These members are demographically representative of ACOG members as a whole. The 600 CARN members were randomly selected from a list of over 1300 current CARN members. The 400 non-CARN respondents were selected using a proportionate stratified sample. This study was reviewed by the Johns Hopkins Institutional Review Board and the authors declare no conflicts of interest.
Participants were sent a cover letter via email with an electronic link to access the survey. Participation was voluntary with no remuneration. The survey was an online questionnaire consisting of 16 questions about point of care testing and 12 demographic questions. It was administered online through Qualtrics software, Qualtrics©, Provo, UT, between June and August of 2016. Recipients who were retired or did not wish to participate were given a link to opt out. Five email reminders were sent once a week to those who had not responded to the survey.
The survey queried participants regarding the following: demographics; practice characteristics and behaviors; use of POC tests, including pregnancy, urine dip, vaginosis, and STI diagnostic tests; and barriers to POC test use, including costs associated with POC tests, test characteristics, and impact on clinic flow.
Data Analysis
Statistical analysis was performed using IBM SPSS Statistics 24.0, IBM Corp©, Armonk, NY. Respondents who completed at least 60% of the survey were included in the analysis. For the purposes of data analysis, the responses “barrier” and “major barrier” were combined to create a dichotomous variable for whether the item is considered a barrier or not. Bivariate analyses included Chi-squared tests and independent t-tests to test for significant differences (p<.05). Logistic regression models were calculated to examine which factors, including practice location, insurance accepted, type of practice, frequency of diagnosing STIs, and POC tests used were associated with use of each POC test.
Results
Response rates
Of the 1,000 ACOG members invited to participate via email, 21 opted-out of participating and 230 did not have valid email addresses. This left a final sample of 749 respondents, of whom 288 participated in the online survey for a 39% total response rate (57% CARN, 17% non-CARN). Of the 288 participants, 251 (87%) provided completed surveys.
Comparison of CARN vs. non-CARN respondents
Assessment of CARN and non-CARN respondents found that only three variables had statistically significant differences between these groups. These variables were the ACOG districts, whether the nurse’s aide was currently responsible for reporting positive STD test results to local or state health departments, and whether the respondents used the stat rapid plasma regain (RPR) test. Of the CARN members, 5.4% stated that it was the responsibility of the nurse’s aide to report positive STD test results, compared to 14.9% of non-CARN members (p = .023). CARN members were also less likely to use the stat RPR test than non-CARN members (2% vs. 10.9%, p = .004). Responses from CARN and non-CARN participants were combined for further analyses.
Respondent demographics
Respondents were 69.7% female and 30.3% male. The average year of birth was 1965 (±11 years) and the average years in practice was 18 years (±10 years). Male respondents were older than female respondents (male, mean year of birth = 1959 ± 9 years; female, mean year of birth = 1968 ± 10 years; p < .001). Similarly, male respondents had been in practice longer than female respondents (male, mean years in practice = 23.4 years ± 9.1 years; female, mean years in practice = 16.3 years ± 9.1 years; p < .001). Additional demographics for the survey respondents are shown in Table 1. Figure 1 illustrates response distribution by state.
Table 1: Demographic Characteristics.
| % | N | ||
| Gender | |||
| Female | 69.7% | 71 | |
| Male | 30.3% | 163 | |
| Race | |||
| White | 79.2% | 183 | |
| Asian | 9.1% | 21 | |
| African American | 7.4% | 17 | |
| Hispanic | 3.9% | 9 | |
| Native Hawaiian/Other Pacific Islander | 0.4% | 1 | |
| Years since completion of residency | |||
| 30+ | 12.7% | 29 | |
| 21–30 years | 27.1% | 62 | |
| 11–20 years | 37.6% | 86 | |
| 5–10 years | 11.8% | 27 | |
| <5 | 10.9% | 25 | |
| Primary medical specialty | |||
| General Ob-Gyn | 72.1% | 168 | |
| Gynecology only | 18.5% | 43 | |
| Obstetrics only | 9.4% | 22 | |
| Type of practice | |||
| Ob-Gyn partnership/group | 42.4% | 97 | |
| University faculty and practice | 28.4% | 65 | |
| Multi-specialty/group | 12.2% | 28 | |
| Solo practice | 10.9% | 25 | |
| HMO/Military and government/Other | 6.1% | 14 | |
| Practice location | |||
| Suburban | 35.2% | 80 | |
| Urban, non-inner city | 22.0% | 50 | |
| Urban, inner city | 21.1% | 48 | |
| Mid-sized town (10,000 – 50,000) and Rural | 20.7% | 47 | |
| Military | 0.9% | 2 | |
| Patient payment method | |||
| Private Insurance | 97.4% | 221 | |
| Medicare/Medicaid | 91.2% | 207 | |
| Self-pay | 91.2% | 207 | |
| Sliding Fee | 33.5% | 76 | |
Figure 1:
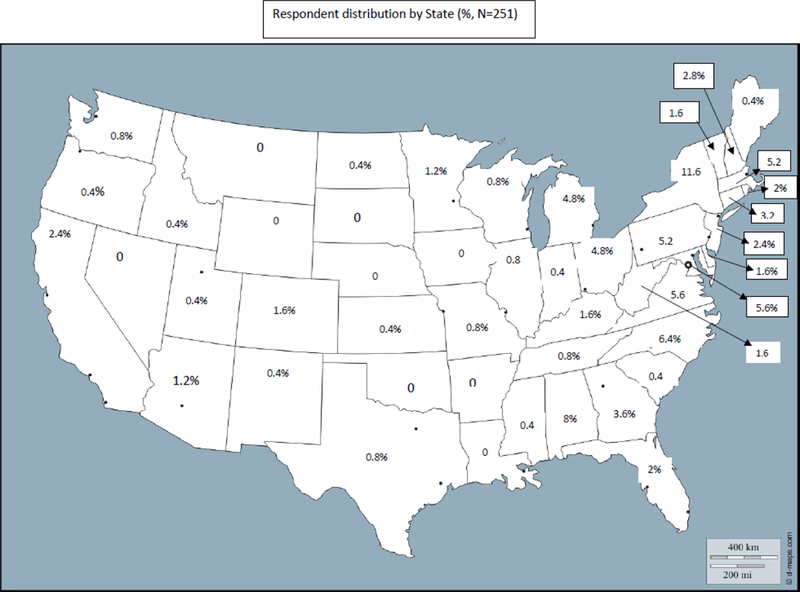
Respondent Distribution by State (%, N = 251)
Diagnosing, treatment and reporting STDs
Respondents were asked about the frequency of diagnosis and treatment of STDs within their practices. Physicians diagnosed STDs once or twice per week for 30.3% of respondents and once or twice per month for 45.0%. Almost half of the respondents indicated that they never (11.6%) or rarely (36.7%) treat STDs syndromically before they knew the laboratory test results, while one in six frequently (13.5%) or always (2.0%) do. There was no significant difference in syndromic treatment by type of practice, gender, race, years in practice, practice location, primary specialty or insurance type. Syndromic treatment by specialty type were as follows: Ob-Gyn partnership/group = 57.7%; Solo practice = 52.0%; HMO/Military and government/other = 50.0%; University faculty and practice = 43.1%; Multi-specialty/group = 42.9%, p = 0.3888.
Significant differences in frequency of diagnosing STDs were found based on primary specialty (Table 2). For physicians whose primary specialty was general obstetrics and gynecology, 35.1% diagnosed STDs once or twice per week, and 42.3% diagnosed STDs once or twice per month, while physicians whose primary specialty was gynecology only or obstetrics only diagnosed STDs 20.9% and 18.2%, respectively, once or twice per week and 48.8% and 50.0%, respectively, one or twice per month (X2 (8, N = 233) = 19.129, p = .014).
Table 2: Frequency of STDs Diagnoses.
| Every day | Once or twice per week |
Once or twice per month |
Once or twice per year |
Don’t see STDs in my patients |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | |
| Total | 10.4% | 26 | 30.3% | 76 | 45.0% | 113 | 10.4% | 26 | 4.0% | 10 |
| Primary Medical Specialty* | ||||||||||
| General Ob/Gyn | 11.9% | 20 | 35.1% | 59 | 42.3% | 71 | 9.5% | 16 | 1.2% | 2 |
| Gynecology only | 9.3% | 4 | 20.9% | 9 | 48.8% | 21 | 14.0% | 6 | 7.0% | 3 |
| Obstetrics only | 0.0% | 0 | 18.2% | 4 | 50.0% | 11 | 18.2% | 4 | 13.6% | 3 |
p < .05
The person responsible for reporting STD test results to local or state health departments is shown in Table 3. When asked who is currently responsible for reporting positive STD test results, a majority of respondents stated that it was the responsibility of the nurse (40.2%) or the laboratory (37.5%). If respondents were currently conducting a point of care test, it was most likely to be the nurse’s responsibility (33.6%). However, for point of care testing results, one in three respondents (28.3%) didn’t know who would be responsible for reporting results.
Table 3: Who is responsible for reporting STD testing results to local or state health departments.
| Clinical (MD) |
Nurse | Nurse’s Aid |
Laboratory | Admin Staff |
Don’t Know | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | % | N | |
| Currently responsible | 11.6% | 29 | 40.2% | 101 | 7.2% | 18 | 37.5% | 94 | 8.0% | 20 | 10.8% | 27 |
| Responsible if POCT conducted | 9.4% | 21 | 33.6% | 75 | 2.2% | 5 | 15.7% | 35 | 7.2% | 16 | 28.3% | 63 |
Point of care testing used
A total of 95.6% of respondents used one or more POC test in their current practice. Pregnancy test (83%), and urine dipstick (83%), were the POC tests used by most respondents, followed by the wet mount test (79%) and the vagina pH test (54.8%) (Table 4). Approximately one in five respondents used the Affirm VPIII test and one in eleven used the Rapid HIV test. Few respondents used Gram stain test (4.8%) and the stat rapid plasma regain (RPR) test (3.6%).
Table 4: Point of care tests currently used.
| % | N | |
| Pregnancy test | 83.1% | 206 |
| Urine dipstick | 83.1% | 206 |
| Wet mount test | 79.0% | 196 |
| Vagina pH | 54.8% | 136 |
| Affirm VP III | 19.0% | 47 |
| Rapid HIV test | 8.9% | 22 |
| Other | 5.6% | 14 |
| Gram Stain | 4.8% | 12 |
| None | 4.4% | 11 |
| Stat RPR | 3.6% | 9 |
Respondents who reported diagnosing STIs daily or once or twice weekly used POCTs more frequently than those who reported diagnosing STIs less frequently (once monthly or less). (Table 5)
Table 5: POCT Use by frequency of STI diagnosed.
| Test (%, N) |
Pregnancy Test |
Urine Dipstick |
Wet Mount Test |
Vagina pH | Affirm VP III |
Rapid HIV Test |
Gram Stain | Stat RPR | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | |
| Every day | 100.0% | 26 | 96.2% | 25 | 92.3% | 24 | 73.1% | 19 | 30.8% | 8 | 15.4% | 4 | 7.7% | 2 | 3.8% | 1 |
| Once or twice per week | 84.2% | 64 | 77.6% | 59 | 82.9% | 63 | 57.9% | 44 | 25.0% | 19 | 13.2% | 10 | 5.3% | 4 | 2.6% | 2 |
| Once or twice per month | 86.4% | 95 | 89.1% | 98 | 82.7% | 91 | 57.3% | 63 | 18.2% | 20 | 6.4% | 7 | 4.5% | 5 | 4.5% | 5 |
| Once or twice per year | 57.7% | 15 | 76.9% | 20 | 57.7% | 15 | 30.8% | 8 | 0.0% | 0 | 0.0% | 0 | 3.8% | 1 | 3.8% | 1 |
| Don’t see STDs in my patients | 60.0% | 6 | 40.0% | 4 | 30.0% | 3 | 20.0% | 2 | 0.0% | 0 | 10.0% | 1 | 0.0% | 0 | 0.0% | 0 |
| P-value | 0.000 | 0.000 | 0.000 | 0.005 | 0.013 | 0.165 | 0.898 | 0.930 | ||||||||
Among respondents who did not use the most common forms of point of care testing, differences in primary medical specialty and location were identified. Of respondents whose primary specialty was obstetrics only, 45.5% did not use pregnancy tests compared to 12.7% of general obstetrics and gynecology practitioners and 19% of gynecology practitioners (X2 (2, N = 230) = 15.005, p = .001); 36.4% did not use urine dipstick tests compared to 13.3% of general obstetrics and gynecology practitioners and 26.2% of gynecology practitioners (X2 (2, N = 230) = 9.537, p = .008).
Differences by location were only found among those who did not use the urine dipstick test. Respondents whose practice was located in an urban inner city (31.3%, (X2 (4, N = 225) = 9.590, p = .048) were more likely to not use the urine dipstick test than those whose practice was located in an urban non-inner city, a suburban, or a mid-sized to rural town (12.0%, 15.2%, and 13.0%, respectively).
Barriers to point of care testing
Respondents were asked about the barriers to using any point of care testing (Table 6) and the two most common barriers were the amount of reimbursement received for performing the test (61.9%) and the payment coverage from the patient (61.3%), such as insurance coverage or out-of-pocket. A majority of respondents also believed that the cost of the test from the manufacturer/distributor (59.8%), having to purchase the instruments (57.8%), and the cost to the practice/clinic (52.1%) were barriers to testing. Only one in four respondents believed that too much ambiguity in reading results (25.8%) was a barrier.
Test 6: Barriers to using Point of Care Testing.
| % | N | |
| Amount of reimbursement | 61.9% | 146 |
| Payment coverage | 61.3% | 146 |
| Cost of the test | 59.8% | 140 |
| Having to purchase the instrument | 57.8% | 133 |
| Cost to practice/clinic | 52.1% | 125 |
| Interruption of clinician work flow | 50.4% | 119 |
| Too many time-driven steps | 42.7% | 100 |
| Too many steps | 39.6% | 94 |
| Increased patient wait time | 39.5% | 93 |
| Consistent test performance regardless of environmental fluctuations | 38.6% | 91 |
| Too much ambiguity in reading results | 25.8% | 60 |
Barriers endorsed by respondents differed by accepted payment methods. Respondents who accepted Medicaid or Medicare and who accepted sliding scale fees were more likely to endorse barriers associated with cost of testing than respondents who did not accept Medicaid or sliding scale payments. Respondents who accepted public insurance were also more likely to report that the payment coverage (64.1%, X2 (1, N = 212) = 5.444, p = .020), the cost of the test from the manufacturer/distributor (61.7%, X2 (1, N = 210) = 6.718, p = .010), and the cost to the practice/clinic (55.3%, X2 (1, N = 216) = 5.853, p = .016) were barriers to testing than respondents who did not accept public insurance (36.8%, 29.4%, and 26.3%, respectively). Respondents who accepted sliding scale fees were slightly more likely to report that the amount of reimbursement received for performing the test was a barrier to using POC tests than respondents who did not accept sliding scale fees (73.5% vs. 59%, X2 (1, N = 212) = 4.200, p = .040). In addition, respondents who accepted sliding scale fees were also more likely to report that the payment coverage (75%, X2 (1, N = 214) = 7.479, p = .006), the cost of the test from the manufacturer/distributor (72.1%, X2 (1, N = 210) = 7.040, p = .008), and having to purchase the instrument (72.3%, X2 (1, N = 206) =7.215, p = .007) were barriers to testing than respondents who did not accept sliding scale fees (55.5%, 52.8%, and 52.5%, respectively).
For respondents who accepted private insurance or self-payment from patients, too many steps to the point of care test was a significant barrier. Respondents who accepted private insurance (40.6%, X2 (1, N = 213) = 4.020, p = .045) and respondents who accepted self-payment (41.8%, X2 (1, N = 210) = 4.884, p =.027) were more likely to report that too many steps were a barrier to testing than respondents who did not (0% and 15.8%, respectively).
Several other significant differences in endorsed barriers were identified based on practice location, primary specialty, and gender. Respondents who worked in a university setting (50.8%, X2 (6, N = 214) = 13.242, p = .039) were less likely to report that the amount of reimbursement received for performing the test was a barrier than respondents who worked in a solo practice, ob-gyn partnership/group, or a multi-specialty group (77.3%, 66.7%, and 76%, respectively). Respondents who worked in a university setting (46.7%, X2 (6, N = 216) = 12.480, p = .052) were also less likely to report that the amount of reimbursement received for performing the test was a barrier than respondents who worked in a solo practice, ob-gyn partnership/group, or a multi-specialty group (73.9%, 65.6%, and 70.4%, respectively). When looking at primary medical specialty, respondents whose primary specialty was obstetrics only (68.4%, X2 (2, N = 217) = 6.046, p =.049) were more likely to report that too many time-driven steps was a barrier than were respondents whose primary specialty was general obstetrics and gynecology or gynecology only (39% and 43.6%, respectively).
When comparing barriers to point of care testing by gender, male respondents were more likely than female respondents to report that the amount of reimbursement for performing the test was a barrier (75.4% of men vs. 58% of women, X2 (1, N = 219) = 6.145, p = .013). Comparing female and male respondents by age had no statistically significant effect. When comparing gender differences by whether or not respondents accepted Medicaid or Medicare, male respondents who accepted these forms of payment (75.4%, X2 (1, N = 194) = 3.467, p = .063) were more likely to report that the amount of reimbursement for performing the test was a barrier than female respondents who did (62.0%). Male respondents were more likely than female respondents to accepted Medicaid or Medicare as a form of payment (100% of men vs. 87.5% of women, X2 (1, N = 227) = 9.184, p = .002).
Few statistically significant differences were identified when comparing barriers to point of care testing with the types of tests used. Of respondents who used the stat RPR test, 22.2% reported that the amount of reimbursement received for performing the test was a barrier (X2 (1, N = 234) = 6.113, p = .013) and 11.1% reported that the cost to the practice/clinic was a barrier (X2 (1, N = 237) = 6.234, p = .013). Respondents who used this point of care test were also less likely to report that the cost of the test from the manufacturer/distributer was a barrier (22.2%, X2 (1, N = 227) = 4.836, p=.028). For respondents who used the rapid HIV test, 76.2% reported that interruption of the clinician work flow was a barrier (X2 (1, N = 233) = 6.437, p = .011).
Logistic regression modelling confirmed associations noted in bivariate analyses between practice locations, payment method accepted, type of practice, and use of each POC test. When controlling for these factors, endorsement of barriers associated with cost of POC testing were not significantly related to use of POC tests, except vaginal pH (having to purchase the instrument, B=0.155, p=.012). Endorsement of interruption of clinician workflow was associated with use of HIV and stat RPR (B=0.125, p=.001; B=−.051, p=0.04).
Discussion
Among members of ACOG who responded to this survey, 75% responded that they diagnose STDs among their patients at least once or twice per month, with 30% diagnosing STDs at least once or twice per week. Traditional POC tests, such as pregnancy test, urine dip, wet mount, and vaginal pH were used by a majority of respondents. Other FDA approved POC tests were used by fewer respondents with 19% reporting Affirm VPIII test use, 8.9% using a rapid HIV test and 3.6% using stat RPR.
Almost half of respondents indicated that they never (12%) or rarely (37%) treat STDs syndromically but wait for laboratory test results, reinforcing that there is an unmet need for rapid diagnostic tests for STDs. This delay in diagnosis and treatment while waiting for results has been reported to lead to persistent STD transmission and potential development of complications such as pelvic inflammatory disease (10–16). Half of clinicians reported treating STD syndromically, suggesting there is much room for improvement. There is no doubt that syndromic management of vaginal discharge is far from ideal, lacking sensitivity and specificity, and poorly predictive of cervical infections particularly with Neisseria gonorrhoeae or Chlamydia trachomatis (14). Continued attention to development and availability of accurate, usable POC tests is necessary.
What is deterring use of available POC tests, especially newer available tests? For the traditional POC tests, it seems intuitive that almost 46% of physicians specializing in obstetrics only would not use POC pregnancy tests, assuming that most women present already knowing they are pregnant. However, it is less clear why physicians practicing in urban inner city locations were less likely to use urine dipstick POC testing compared to those practicing in other locations. Consistent with payments accepted, practice location, and practice type being associated with use of POC tests, the two most commonly identified barriers to using POC tests were amount of reimbursement and payment coverage. Impact of POC test on clinic flow appears not to be a barrier to adopting the use of a test, but is noted as a barrier by those using the test: only 8.9% of respondents reported using rapid HIV tests, and for the respondents who used the rapid HIV test, over 75% believed that interruption of the clinician work flow was a barrier.
Reporting STD testing results to local or state health departments is currently the responsibility of either the laboratory (38%) or the practice nurse (40%). However, if a POC test is done on-sight, 28% of respondents did not know who would be responsible for reporting positive results to health departments. These responses highlight important issues with surveillance of currently reportable STDs for gonorrhea and chlamydia if future POC tests for these infections become available and adopted.
This study has several limitations. Like many email driven questionnaires, participation in an online questionnaire is never optimal. We kept the questionnaire short to maximize participation, and therefore did not ask in depth questions regarding routine testing practices (such as serologic HIV or syphilis testing). Thus, many respondents may not have used POC HIV tests since laboratory based serology is the usual practice.
In developing and marketing new and improved POC tests for STDs, therefore, it is imperative that industry consider not only the unit price of each test, but also hidden costs such as the purchase of instruments or direct cost to the practice or clinic. Insurance coverage and payments also influence adoption of POC tests for STDs. Practices accepting Medicare or Medicare identified reimbursement as a major barrier to POC test use. When money is scarce, priorities may shift. Respondents accepting private insurance or self-payment identified too many steps as a significant barrier. In this case, time is money. In either case, the argument that POC tests for STDs are cost effective by minimizing loss to follow-up, expediting treatment and improving both cost and health outcomes (17–18) is lost.
Acknowledgments
Research is supported by National Institutes of Health U54EB007958 NIBIB.
Footnotes
The authors declare no conflict of interests
References
- 1.Herbst de Cortina S, Bristow CC, Duvey DJ, Klausner JD. A systematic review of point of care testing for chlamydia trachomatis, Neisseria gonorrhoeae, and Trichomonas vaginalis. Inf Dis Ob Gynecol 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Drancourt M, Michell-Lepage A, Boyer S, Raoult D. The Point-of-Care laboratory in clinical microbiology. Clin Micro Rev 2016;29:429–446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cristillo AD, Bristow CC, Peeling R, et al. Point-ofcare sexually transmitted infection diagnostics: Proceedings of the STAR sexually transmitted infection- clinical trial group programmatic meeting. Sex Trans Dis 2017;44:211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tucker JD, Bien CH, Peeling RW. Point-of-care testing for sexually transmitted infections: Recent advances and implications for disease control. Curr Opin Infect Dis 2013;26:73–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hsieh YH, Gaydos CA, Hogan MT et al. That qualities are most important to making a point of care test desirable for clinicians and others offering sexually transmitted infection testing? PLoS One. 2011, April 29;6(4):e1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rompalo AM, Hsieh YH, Hogan T, et al. Point-of-care tests for sexually transmissible infections: what do “end users” want? Sex Health 2013;10:541–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Su WH, Tsou TS, Chen CS. Are we satisfied with the tools for the diagnosis of gonococcal infection in females? J Chin Med Assn. 2011;74:430–434. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016 Atlanta: U.S: Department of Health and Human Services; 2017. [Google Scholar]
- 9.Coleman VH, Power ML, Zinbers S, Schulkin J. Contemporary clinical issues in outpatient obstetrics and gynecology: findings of the Collaborative Ambulatory Research Network, 2001–2001:part 1. Obstet Gynecol Surv 2004;59:780–6. [DOI] [PubMed] [Google Scholar]
- 10.Ford Carleton P, Schachter S, Parrish JA et al. National Institute of Biomedical Imaging and Bioengineering point-of-care technology research network: Advancing precision medicine. IEEE J Transl Eng Health Med 2016;4:2800614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brook G the performance of non-NAAT point-of-care (POC) tests and rapid NAATS tests for chlamydia and gonorrhoea infections. AN assessment of currently available assays. Sex Trans Infect 2015;91:539–544. [DOI] [PubMed] [Google Scholar]
- 12.Reed JL, Simendinger L, Griffeth S, Kim HG, Huppert JS. Point-of-care testing for sexually transmitted infections increases awareness and short-term abstinence in adolescent women. J Adolesc health 2010;46:270–277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwebke JR, Sadler R, Sutton JM, Hook EW 3rd. Positive screening tests for gonorrhea and chlamydial infection fail to lead consistently to treatment of patients attending a sexually transmitted diseases clinic. Sex Transm Dis 1997;24:181–184. [DOI] [PubMed] [Google Scholar]
- 14.Scholes D, Stergachis A, Heidrich FE et al. Prevention of pelvic inflammatory disease by screening for cervical chlamydial infection. N Engl J Med 1996;334:1362–1366. [DOI] [PubMed] [Google Scholar]
- 15.Peeling RW, Holmes KK, Maabey D, Ronald A. Rapid tests for sexually transmitted infections (STIs): the way forward. Sex Transm Infect 2006;82: Suppl 5:v1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.World Health Organization. Global health sector strategy on sexually transmitted infections 2016–2021: Towards ending STIs. http://apps.who.int/iris/bitstream/10665/246296/1/WHO-RHR-16.09-eng.pdf?ua=1 [Google Scholar]
- 17.Turner K Round J, Hormer P et al. An early evaluation of clinical and economic costs and benefits of implementing point of care NAATS for Chlamydia trachomatis and Neisseria gonorrhoeae in genitourinary medicine clinics in England. Sex Transm Infect 2014;90:104–111.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Huang W, Gaydos CA, Barner MR, Jwett-Goheen M, Blake DD. Comparative effectiveness of a rapid point-of-care test for detection of Chlamydia trachomatis among women in a clinical setting. Sex Transm Infect 2013;89:108–114. [DOI] [PMC free article] [PubMed] [Google Scholar]


