Abstract
Objectives
To develop and validate a model for predicting the risk of hospital admission within 1 year in the HIV population under antiretroviral treatment.
Methods
We conducted a retrospective observational study. Patients receiving antiretroviral treatment for at least 1 year who were followed by the pharmacy service in a Spanish-speaking hospital between January 2008 and December 2012 were included. Demographics, and clinical and pharmacotherapy variables, were included in the model design. To find prognostic factors for hospital admission a multivariate logistic regression model was created after performing a univariate analysis. Model validity was determined by the shrinkage method and the model discrimination by Harrell's C-index.
Results
442 patients were included in the study. The variables ‘CD4 count <200 (cells/µL)’, ‘drug/alcohol use’, ‘detectable viral load (>50 copies/mL)’, ‘number of previous admissions’, and ‘number of drugs different from antiretroviral treatment’ were the independent predictors of risk of hospital admission. Probabilities predicted by the model showed an R2=0.98 for the development sample and an R2=0.86 for the validation sample. The Harrell's C index for the development and validation data were 0.82 (95% CI 0.77 to 0.87) and 0.80 (95% CI 0.73 to 0.88), respectively.
Conclusions
The model developed in this study may be useful in daily practice for identifying HIV patients at high risk of 1-year hospital admission.
Keywords: HIV, antiretroviral treatment, predictive model, hospital admission, pharmacy
Introduction
The morbidity and mortality rates associated with HIV have been drastically reduced since the introduction of highly active antiretroviral treatment (HAART) in 1996.
Currently, HIV has become a chronic disease1 and, as a result, HIV-infected individuals are becoming older.2 It is projected that by 2015, more than half of all HIV-infected individuals in the USA will be ≥50 years of age.3
Compared with age-matched HIV-uninfected individuals and with younger HIV-infected individuals, HIV-infected people ≥50 years have a higher rate of co-morbidities and polypharmacy, possibly exacerbated by HIV infection or long-term exposure to HAART.4 The consequences of polypharmacy may include drug–drug interactions, toxicity, treatment failure or development of viral resistance to HAART. In addition, complex medication regimens are associated with poor adherence which can lead to an increase in hospital admissions.5 6
An ageing HIV population demands a new approach to the management of HIV infection. Risk prediction algorithms appear to be a good way to stratify and subsequently identify patients who need further evaluation in a multidisciplinary approach.
There are currently several methods to predict unplanned hospital admissions in patients with chronic diseases.7 8 Due to the unique characteristics of the HIV population, models to predict 30-day risk of readmission among this population have been developed.9 10 However, 30 days is not always long enough to perform medical interventions in order to prevent a hospital admission.
Therefore, the main objective of this study was to develop and validate an accurate tool for predicting risk of hospital admission within 1 year in the HIV population that is under HAART.
Methods
We conducted a retrospective observational study. Patients under HAART for at least 1 year who were followed by the pharmacy service in a Spanish-speaking hospital between January 2008 and December 2012 were included. We excluded patients enrolled in clinical trials and patients whose data were not available.
The occurrence of hospital admission in HIV patients under HAART was considered the dependent variable. We considered a hospital admission when the length of stay in the hospital was >24 h. We excluded emergency department visits.
We also collected the following independent variables: demographics, laboratory values, clinical parameters, pharmacotherapy related features, and variables related to hospital admission. The co-morbidities were classified according to the definition of Rivas Costa et al11 and Ollero et al.12 Adherence to HAART was assessed using electronic pharmacy refill records. The threshold for optimal adherence was defined at 90% and above.
The data were collected 1 year before the first hospital admission during the study period. In those patients who were not hospitalised during the study period, variables were collected 1 year before the last visit to the pharmaceutical care office. The data were obtained through outpatient electronic medical records, by reviewing the medical history of each patient, and through the patient census report from the hospital.
Statistical analysis
Quantitative variables are expressed as mean and SD. In the case of a skewed distribution variables are expressed as median and percentile P25 and 75, the difference between being the IQR. Qualitative variables are expressed as absolute numbers (n) and percentages (%).
To identify independent predictors of hospital admission, univariate logistic regression was performed. Afterwards, those variables that showed statistical significance in the univariate analysis and those with a value of p≤0.25 were included in a multivariate logistic regression.
Shrinkage method was used to evaluate the validity of the prediction model. Model discrimination was determined by calculating the Harrell’s C index. It was performed on both the original and the adjusted model. To verify the validity of the model the difference between both Harrell’s C indexes had to be <0.10.
Calibration was tested by the Hosmer-Lemeshow ‘goodness-of-fit’ test and the slope of the calibration curve.
Data analysis was carried out using the statistical package SPSS V.20.0 for Windows.
Ethical issues
The study design was approved by the local ethics committees of the participating study site (0009/13).
Results
Four hundred and forty-two patients were included in the study. Demographics and clinical characteristics are provided in table 1.
Table 1.
Baseline and clinical characteristics of the patients included in the study
| Variable | Characteristics |
|---|---|
| Age in years, median (IQR) | 45.00 (41–48) |
| Sex: male/female (% male) | 357/85 (80.8%) |
| Serum bilirubin (mg/dL), median (IQR) | 0.53 (0.37–0.84) |
| Serum creatinine (mg/dL), median (IQR) | 0.78 (0.69–0.91) |
| CD4 count <200 cells/µL, n (%) | 82 (18.6%) |
| Detectable HIV viral load (copies/mL), n (%) | 113 (25.6%) |
| HIV transmission mode, n (%) | |
| Injection drug use | 322 (72.9%) |
| Sexual | 120 (27.1%) |
| HIV/HCV co-infection, n (%) | 307 (69.5%) |
| Alcohol or drug use, n (%) | 158 (35.7%) |
| Co-morbidities, median (IQR) | 2.00 (1.00–3.00) |
| AIDS, n (%) | 297 (67.2%) |
| Type of HAART, n (%) | |
| 2 NRTI+1 NNRTI | 200 (45.2%) |
| 2 NRTI+1 PI | 238 (53.8%) |
| Others (including CCR5 antagonists or IntIn) | 44 (10.0%) |
| Adherence to HAART ≥90%, n (%) | 298 (67.4%) |
| Co-medications, median (IQR) | 2.00 (0.00–4.00) |
| Days of hospital stay, median (IQR) | 8.00 (5.00–12.75) |
| Hospital admissions the year before, minimum–maximum | 0–7 |
HAART, highly active antiretroviral treatment; IntIn, integrase inhibitor; NNRTI, non-nucleoside reverse transcriptase inhibitor; NRTI, nucleoside reverse transcriptase inhibitor; PI, protease inhibitors.
Most of the patients were men and the median age was 45 years. Regarding clinical characteristics, there was a high prevalence of HIV/hepatitis C virus (HCV) co-infected patients (69.5%). In addition, most of the patients were considered to adhere to their treatment (67.4%). Consequently, the majority of patients had an undetectable viral load (74.4%) and a CD4 count >200 cells/µL (81.2%). Considering the antiretroviral drug classes, the most common regimens were those including a combination of a nucleoside reverse transcriptase inhibitors and a protease inhibitor. In addition to HAART, the median number of co-medications was 2.
Variables that reached statistical significance in the univariate regression analysis were: demographics, adherence ≥90%, CD4 count <200 cells/µL, drug/alcohol use, detectable viral load (>50 copies/mL), AIDS, HIV transmission mode, number of co-morbidities, number of previous admissions, number of drugs different from HAART, HAART including integrase inhibitors, CCR5 receptor antagonists or non-nucleoside reverse transcriptase inhibitors. Table 2 shows the relationship between these variables and the risk of hospital admission.
Table 2.
Univariate analysis*
| Variable | HR (95% CI) |
|---|---|
| Adherence to HAART ≥90% | 0.28 (0.17 to 0.47) |
| CD4 count <200 cells/µL | 7.35 (3.45 to 15.62) |
| Alcohol or drug use | 5.91 (3.51 to 9.96) |
| Detectable HIV viral load (copies/mL) | 4.26 (2.41 to 7.54) |
| AIDS | 2.63 (1.59 to 4.36) |
| HIV transmission mode | 0.40 (0.24 to 0.68) |
| Number of co-morbilities | 1.33 (1.11 to 1.60) |
| Hospital admissions the year before | 14.70 (4.49 to 48.10) |
| Number of co-medications | 1.42 (1.26 to 1.60) |
*Only variables with a significant association with risk admission are included.
Subsequently, multivariate analysis showed that a CD4 count <200 cells/µL, drug/alcohol use, detectable viral load (>50 copies/mL), number of previous admissions, and number of drugs different from HAART were the only independent predictors of risk of hospital admission (table 3).
Table 3.
Multivariate analysis*
| Variable | HR (95% CI) |
|---|---|
| CD4 count <200 cells/µL | 3.18 (1.33 to 7.61) |
| Alcohol or drug use | 4.13 (2.30 to 7.39) |
| Detectable HIV viral load (copies/mL) | 2.11 (1.05 to 4.23) |
| Hospital admissions the year before | 6.57 (1.85 to 23.36) |
| Number of co-medications | 1.25 (1.10 to 1.42) |
*Only variables with a significant association with risk admission are included.
The mathematical model for predicting risk of hospital admission within 1 year in the HIV population is shown in box 1.
Box 1. Mathematical model for predicting risk of hospital admission within 1 year in HIV population.
Prob (risk of hospital admission within 1 year in HIV population under HAART)=1/(1+e−Z)
Z=−14 857+1744×hospital admissions the year before +02 663×number of co-medications+0771×detectable HIV viral load (copies/mL)+13 584×alcohol or drug use+11 376×CD4 count (<200 cells/µL).
In figure 1, receiver operating characteristic (ROC) curves of logistic regression for both development and validation data are plotted.
Figure 1A, B.
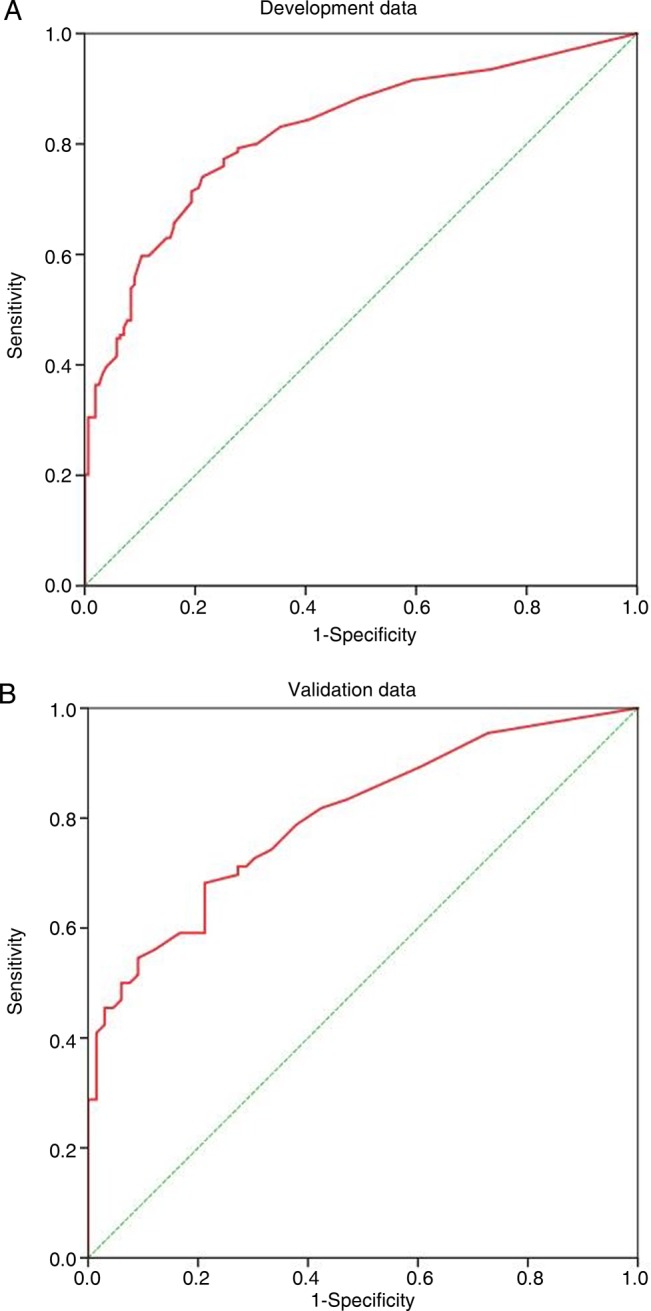
Curves of logistic regression for development and validation data.
The Harrell's C index for the development and validation data were 0.82 (95% CI 0.77 to 0.87) and 0.80 (95% CI 0.73 to 0.88), respectively. They both have values of Harrell’s C >0.75, showing good discriminatory ability. The difference between both Harrell’s C statistics was <0.10 (0.82 to 0.80=0.02) so discriminant validity is supported.
The calibration curves for development and validation data are shown in online supplementary figures 1 and 2. The slope values were R2=0.98 and R2=0.86, respectively.
Internal consistency reliability as measured by Cronbach’s α was 0.99 and 0.96 in the development and validation samples, respectively.
Finally, model calibration is graphically shown by risk deciles in online supplementary figures 3 and 4.
Discussion
Our study is the first to present a mathematical model for predicting risk of hospital admission within 1 year in an HIV population under HAART. The risk factors identified are associated with the following variables: CD4 count <200 cells/µL, detectable HIV-RNA level (>50 copies/mL), drug/alcohol use, the number of co-medications for diseases that are not HIV, and finally the number of previous admissions.
To date several risk prediction models for hospital readmission in the general population have been published. The following predictor variables were identified by some studies: demographics, type of diagnosis, and number of previous admissions.13 14 Others studies have included independent variables such as laboratory values, number of prescription drugs or socioeconomic status. Prediction models based only on one variable, such as the number of previous admissions, have little validity because they do not provide enough clinical information.15–17
In our study the type of HAART has not been shown to predict hospital admission within 1 year. Different conclusions can be drawn from other papers.6 The use of different types of HAART is probably the main cause of the differences between both studies. It is known that significant advances in antiretroviral therapy have been made recently and as a result antiretroviral agents are safer and simpler than before.
Fielden et al18 and Juday et al19 have found that adherence is a key factor in decreasing the risk of hospitalisation. In this study poor adherence to antiretroviral treatment was not an independent predictor. However, undetectable viral load was an independent variable of hospitalisation. Although it has been widely demonstrated that incorrect adherence is one of the main causes of treatment failure, it is possible that other variables such as co-infection or HIV drug resistance are associated with treatment failure.
Our study shows the number of co-medications for other chronic diseases (non-HIV drugs) predicts the risk of hospital admission. Cantudo-Cuenca et al20 reported that the use of multiple medications increases the risk of non-adherence and therefore it may increase the risk of hospital admission. Polypharmacy seems to be the next therapeutic challenge in HIV patients.21–23
Co-morbidities were related to the risk of admission only in the univariate analysis. According to Crowell et al,24 HCV and/or hepatitis B virus (HBV) co-infected patients have higher rates of admissions than HIV mono-infected patients. Despite the high rates of co-infected patients in our study, we did not find this association, possibly because we did not measure the degree of liver damage.
The number of previous hospitalisations was a predictor of readmission. Most readmissions occur within a week of discharge. Pharmaceutical interventions within the first few days would help prevent readmissions.
There is also a role for pharmacists in decreasing the errors in prescribing antiretroviral drugs during the hospitalisation. These errors can lengthen their hospital stay so a close monitoring of these patients should be a priority.25 26
Limitations
The main limitation of this study is its design. Failure to include patients from different centres may bias the results. However, given the sample size and the baseline characteristics of the study population, we believe the model is useful and can be extrapolated.27
Other factors such as variables related to health and social status could be risk factors of admission.28–30 The inclusion of these variables would have improved the predictive ability of the model. However, this information is not recorded in our database.
Knowing the risk factors of hospital admission, one important area for future research is to validate the interventions designed to prevent and reduce hospital readmissions. It would be of great interest to do a cohort study to compare the interventions in terms of health and economic outcomes. The study results would help us to determine whether the interventions are cost-effective.
Conclusion
In conclusion, the model developed in this study may be useful in daily practice for identifying HIV patients who are at high risk of hospital admission.
What this paper adds.
What is already known on this subject
An ageing HIV population demands a new approach to the management of HIV infection.
There are currently several methods to predict unplanned hospital admissions in patients with chronic diseases, but to date there is no model targeted to predict the 1-year risk of admission among the HIV population.
What this study adds
This is the first study to present a mathematical model for predicting the risk of hospital admission within 1 year in the HIV population that is under highly active antiretroviral treatment (HAART).
The predictive model for 1-year hospital admission in HIV patients appears to be a good way to stratify and subsequently identify patients who need further evaluation.
Footnotes
Competing interests: None declared.
Patient consent: Obtained.
Ethics approval: The study design was approved by the local ethics committees of the participating study site. (0009/13).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Antiretroviral Therapy Cohort Collaboration. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies. Lancet 2008;372:293–9. 10.1016/S0140-6736(08)61113-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Luther VP, Wilkin AM. HIV infection in older adults. Clin Geriatr Med 2007;23:567–83. 10.1016/j.cger.2007.02.004 [DOI] [PubMed] [Google Scholar]
- 3.Nguyen N, Holodniy M. HIV infection in the elderly. Clin Interv Aging 2008;3:453–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marzolini C, Back D, Weber R, et al. Ageing with HIV: medication use and risk for potential drug–drug interactions. J Antimicrob Chemother 2011;66:2107–11. 10.1093/jac/dkr248 [DOI] [PubMed] [Google Scholar]
- 5.Marzolini C, Elzi L, Gibbons S, et al. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antiviral Therapy 2010;15:413–2. 10.3851/IMP1540 [DOI] [PubMed] [Google Scholar]
- 6.Sax PE, Meyers JL, Mugavero M, et al. Adherence to antiretroviral treatment and correlation with risk of hospitalization among commercially insured HIV patients in the United States. PLoS One 2012;7:e31591 10.1371/journal.pone.0031591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Initial uses of the PRISM risk stratification tool in CCM Demonstrator sites: a qualitative study. June 2010. http://www.wales.nhs.uk/sitesplus/829/opendoc/161217/ (accessed 15 Aug 2015).
- 8.Daigle LA. Patient improving health care quality drives payment reform. January 2012. http://www.ashp.org/DocLibrary/Advocacy/AnalysisPaper/Improving-Health-Care-Quality -Drives-Payment-Reform.aspx/ (accessed 15 Aug 2015).
- 9.Berry SA, Fleishman JA, Yehia BR, et al. Thirty-day hospital readmission rate among adults living with HIV. AIDS 2013;27:2059–68. 10.1097/QAD.0b013e3283623d5f [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nijhawan AE, Clark C, Kaplan R, et al. An electronic medical record-based model to predict 30-day risk of readmission and death among HIV-infected inpatients. J Acquir Immune Defic Syndr 2012;61:349–58. 10.1097/QAI.0b013e31826ebc83 [DOI] [PubMed] [Google Scholar]
- 11.Rivas Costa G, Domínguez Berjon MF, Astray Mochales J, et al. Características epidemiológicas de la pluripatología y su influencia en la utilización de servicios sanitarios a partir de una encuesta de salud. Rev Esp Salud Pública 2009;83:835–46. 10.1590/S1135-57272009000600007 [DOI] [PubMed] [Google Scholar]
- 12.Ollero M, Álvarez M, Barón B. Atención a pacientes pluripatológicos: Proceso asistencial integrado. 2a ed Sevilla: Consejería de Salud de Andalucía, 2007. [Google Scholar]
- 13.McAna JF, Crawford AG, Novinger BW, et al. A predictive model of hospitalization risk among disabled Medicaid enrollees. Am J Manag Care 2013; 19:e166–74. [PubMed] [Google Scholar]
- 14.Holman CD, Preen DB, Baynham NJ, et al. A multipurpose comorbidity scoring system performed better than the Charlson index. J Clin Epidemiol 2005;58:1006–14. 10.1016/j.jclinepi.2005.01.020 [DOI] [PubMed] [Google Scholar]
- 15.Lewis G. Predictive modeling in action: how ‘virtual wards’ help high-risk patients receive hospital care at home. New York: The Commonwealth Fund, 2010. http://www.commonwealthfund.org/~/media/Files/Publications/Issue%20Brief/2010/Aug/1430_Lewis_predictive_modeling_in_action_virtual_wards_intl_brief.pdf (accessed 15 Aug 2015). [Google Scholar]
- 16.Allaudeen N, Schnipper JL, Orav EJ, et al. Inability of providers to predict unplanned readmissions. J Gen Intern Med 2011;26:771–6. 10.1007/s11606-011-1663-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Quail JM, Lix LM, Osman BA, et al. Comparing comorbidity measures for predicting mortality and hospitalization in three population-based cohorts. BMC Health Serv Res 2011;11:146 10.1186/1472-6963-11-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fielden SJ, Rusch ML, Yip B, et al. Non adherence increases the risk of hospitalization among HIV-infected antiretroviral naïve patients started on HAART. J Int Assoc Physicians AIDS Care 2008;7:238–44. 10.1177/1545109708323132 [DOI] [PubMed] [Google Scholar]
- 19.Juday T, Gupta S, Grimm K, et al. Factors associated with complete adherence to HIV combination antiretroviral therapy. HIV Clin Trials 2011;12:71–8. 10.1310/hct1202-71 [DOI] [PubMed] [Google Scholar]
- 20.Cantudo-Cuenca MR, Jiménez-Galán R, Almeida-González C, et al. Concurrent use of comedications reduces adherence to antiretroviral therapy among HIV-infected patients. J Manag Care Pharm 2014;20:844–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Edelman EJ, Gordon KS, Glover J, et al. The next therapeutic challenge in HIV: polypharmacy. Drugs Aging 2013;30:613–28. 10.1007/s40266-013-0093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holtzman C, Armon C, Tedaldi E, et al. Polypharmacy and risk of antiretroviral drug interactions among the aging HIV-infected population. J Gen Intern Med 2013;28:1302–10. 10.1007/s11606-013-2449-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gleason LJ, Luque AE, Shah K. Polypharmacy in the HIV-infected older adult population. Clin Interv Aging 2013;8:749–63. 10.2147/CIA.S37738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Crowell TA, Gebo KA, Balagopal A, et al. Impact of hepatitis coinfection on hospitalization rates and causes in a multicenter cohort of persons living with HIV. J Acquir Immune Defic Syndr 2014;65:429–37. 10.1097/QAI.0000000000000059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Commers T, Swindells S, Sayles H, et al. Antiretroviral medication prescribing errors are common with hospitalization of HIV-infected patients. J Antimicrob Chemother 2014;69:262–7. 10.1093/jac/dkt323 [DOI] [PubMed] [Google Scholar]
- 26.Traynor K. Antiretroviral stewardship program reduces drug errors. Am J Health Syst Pharm 2013;70:1964–5. 10.2146/news130075 [DOI] [PubMed] [Google Scholar]
- 27.Hasse B, Ledergerber B, Furrer H, et al. Morbidity and aging in HIV-infected persons: the Swiss HIV cohort study. Clin Infect Dis 2011; 53:1130–9. 10.1093/cid/cir626 [DOI] [PubMed] [Google Scholar]
- 28.Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA 2011;306:1688–98. 10.1001/jama.2011.1515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lemke KW, Weiner JP, Clark JM. Development and validation of a model for predicting inpatient hospitalization. Med Care 2012;50:131–9. 10.1097/MLR.0b013e3182353ceb [DOI] [PubMed] [Google Scholar]
- 30.Billings J, Georghiou T, Blunt I, et al. Choosing a model to predict hospital admission: an observational study of new variants of predictive models for case finding. BMJ Open 2013;3:e003352 10.1136/bmjopen-2013-003352 [DOI] [PMC free article] [PubMed] [Google Scholar]


