Abstract
Background
Clinical pharmacy activities developed significantly in the last decade. The extent and organisation of these activities in Switzerland remained unknown.
Objectives
To map clinical pharmacy services (CPS) provided in Swiss hospitals and to discuss their development focusing on different cultural regions and healthcare systems.
Methods
We enrolled all chief hospital pharmacists affiliated with the Swiss Society of Public Health Administration and Hospital Pharmacists (n=47) for an online survey. We asked them to describe the extent and organisation of CPS concerning patient-related, therapy-related or process-related activities, the structural organisation and the available human resources.
Results
The survey took place from March to April 2013. It was completed by 44 chief hospital pharmacists (return rate 94%), representing the hospital landscape in Switzerland comprehensively. Thirty-three (75%) hospitals offered regular CPS and seven (16%) planned to do so. Institutions in regions without drug-dispensing physicians rather employed pharmacists assigned with clinical activities (n=20, 22% of 135.3 full-time equivalent (FTE)) than regions with partial (n=8, 7% of 35.8 FTE) or unrestricted drug dispensing by physicians (n=16, 6% of 68.1 FTE, p=0.026). Of hospitals with implemented CPS, 73% had weekly interprofessional ward rounds, and in 9.1%, clinical pharmacists daily reconciled medicines at patient discharge.
Conclusions
Our data show regional differences in the implementation and pattern of CPS. A significant correlation to drug dispensing by physicians in ambulatory care and human resources provided for CPS was found. While interprofessional ward rounds were performed periodically, seamless care activities by clinical pharmacists remained insufficiently established.
Keywords: CLINICAL PHARMACY, Pharmaceutical Care, Seamless Care, Interprofessional Collaboration, PHARMACY MANAGEMENT (PERSONNEL), PUBLIC HEALTH
Introduction
Since the publication of the concept of ‘pharmaceutical care’ by Hepler and Strand1 in 1990, great efforts have been made to establish patient-centred pharmaceutical services in outpatient and inpatient settings, especially in the Anglo-Saxon countries.2 The pharmacists’ contribution is not only limited to drug manufacture and supply, but it expands in taking increasing responsibility for the appropriate drug choice and application. Especially the pharmacist's role in patient care during the hospital stay is highly valuable since the clinical setting and related medication process is recognised as a particularly risky situation.3–5 Moreover, the transition from inpatient to outpatient care adds further challenges to patients and health professionals.6–8 As a possible approach to reduce preventable medication errors and correlated harm to the patient, around the world the concept of clinical pharmacy got successfully implemented in the hospital setting with various patient-related services.9 10
Development of structured clinical pharmacy activities in Switzerland
In 2006, the Swiss Society of Public Health Administration and Hospital Pharmacists (GSASA) organised four pioneering workshops to establish the requirements for obtaining the degree of a clinical pharmacist.11 The Swiss Pharmacy Federation approved a structured postgraduate education programme in 2008, leading to the certificate ‘Clinical Pharmacy FPH’. In 2011, the GSASA defined clinical pharmacy as “an area of pharmacy aimed at developing and promoting an appropriate, safe and cost-effective use of therapeutic products”.12 According to this definition, the clinical pharmacist is part of a multidisciplinary team and is present on the ward on a daily basis or as a regular consultant for the different services. The activities of clinical pharmacy are organised along three axes:
Patient-related axis: To collaborate in patient education and continuity of care to improve medication history, adherence to therapy; transition to the ambulatory setting and education on discharge medication (=seamless care).
Treatment-related axis: To analyse drug therapy to optimise and reduce overuse, underuse and misuse of medicines, taking into account the aspects mentioned under (1), to optimise the choice of medication after a risk/benefit analysis and cost-effectiveness; to ensure indications and completeness of treatment; to avoid contraindications according to the pathophysiological state; and to guarantee adaptation and individualisation of treatment.
Process-related axis: To consolidate the drug supply chain to ensure that the patient receives the right medication at the right time as prescribed by supporting good prescribing practices, development of guidelines on the preparation and administration of medication; development of treatment guidelines in collaboration with medical and nursing teams in the departments involved; development of computerised decision support systems for the prescription and administration of drugs; and prevention and documentation of adverse drug events on the ward.
These three axes should be completed with the following related activities, which are an integral part of the role of the clinical pharmacist: contribution in continuing education of physicians, nurses and pharmacists, as well as in research and development of new services.
Cultural and structural challenges for the development of clinical pharmacy services in Switzerland
Switzerland is characterised by its federalist political system with 26 cantons and its multilingualism (German, French, Italian and Romansh). Since the national healthcare system is independently regulated by the cantons, 26 different systems have to be considered. These heterogeneous conditions can promote innovation as well as create barriers to the development of new healthcare models. Notable for our research is the fact that in 16 cantons of Switzerland, physicians in ambulatory care are allowed to dispense drugs directly to their patients (dispensing physicians). Since lack of collaboration between competitors might be an issue in the development of clinical pharmacy practice, we were interested in the potential interference of this structural factor. Our objectives were to map the clinical pharmacy services provided in Swiss hospitals, to reflect on the aims of the definition and observed realities, and, finally, to discuss the results considering various cultural regions and the peculiarities of different healthcare systems.
Methods
Online survey
A literature search provided an overview of previously conducted surveys with comparable research questions focusing on clinical pharmacy practice.13–18 Based on these findings, general issues and topics were extracted and supplemented by country-specific elements. An expert panel with representatives from the university, postgraduate lecturers and practitioners assessed the comprehensiveness and appropriateness of the survey (content, structure and scope). To ensure an uniform understanding of clinical pharmacy activities, the GSASA definition of clinical pharmacy12 formed the main reference for this survey. The questionnaire contained 43 items and was phrased in a structured way to describe nature and extent of clinical pharmacy services (patient-related, therapy-related or process-related activities), structural organisation (extent of ward contact) and available human resources (represented as full-time equivalents (FTEs)). Thereby, FTETotPharm summed up all human resources for pharmacists’ activities in the hospital pharmacy while FTEClinPharm represented resources reserved for clinical pharmacy activities.
Data analysis
The data were transferred in Microsoft Office 2013 Excel and processed for statistical analysis with IBM SPSS Statistics 22. We also used Microsoft Office Excel 2013 and the add-in ‘GeoFlow’ to visualise our results. Analysis of possible correlations within group and scale variables was provided using the Mann–Whitney U test (nGroups=2) or the Kruskal–Wallis test (nGroups≥2). All tests were performed with a significance level of α=0.05.
Results
Conducting the survey
In a cross-sectional study, we enrolled all chief hospital pharmacists (n=47) that were affiliated with the GSASA at the index date 1 January 2013 by email. The survey took place from 21 March to 25 April 2013. In the absence of feedback, the contacts were reminded to participate by email or by phone call twice during a period of 3 weeks. The survey was completed by 44 chief hospital pharmacists (return rate 94%).
Institution characteristics
In summary, 6 institutions were affiliated with a university, 21 were independent cantonal and regional hospitals, and 7 were specialised clinics. Furthermore, 10 hospitals were organised in networks. Hospitals were categorised following their characteristics and assigned to the established categories of the Swiss federal statistical office.19 Overall, all general hospitals with central supply level 1 (university hospitals) employed a pharmacist who could provide insights into their organisation. Likewise, a majority of 80% of general hospitals with central supply level 2 and 52% of general hospitals with primary care level 3 took part in the survey. The coverage decreased in general hospitals with primary care levels 4 and 5, where in 2 of 69 listed institutions a pharmacist was present at least part time and thus surveyed (3%). This trend continued in the psychiatric, rehabilitative facilities and specialty hospitals (4%). In total, 19 trainee placements for the national accredited postgraduate degree in hospital pharmacy were provided by 17 hospitals. Nine institutions offered a total of 13 trainee placements for obtaining the certificate of proficiency in clinical pharmacy.
Extent of clinical pharmacy activities and human resources
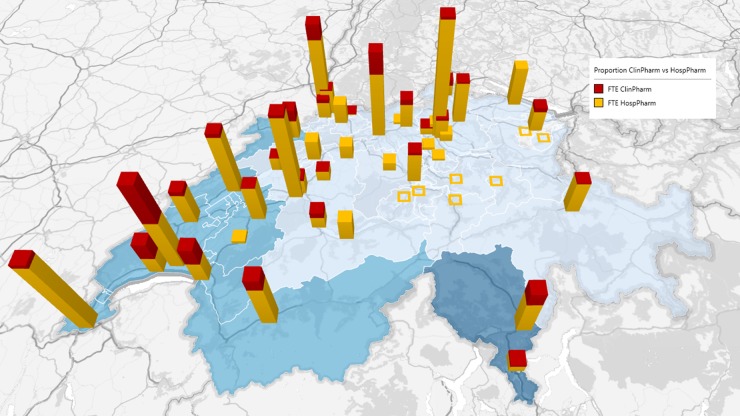
The 44 institutions reported a total of 239.2 FTETotPharm for hospital pharmacists. Of the surveyed hospitals, 33 (75%) already offered permanently implemented clinical pharmacy services (FTEClinPharm=35.9). Another seven (16%) hospitals were planning to introduce appropriate structures. The remaining four (9%) hospitals indicated offering no clinical pharmacy services in the near future. In the French-speaking part of Switzerland (11 institutions), 23.2% of the total hospital pharmacy’s human resources were assigned to clinical pharmacy services (FTEClinPharm=19.1; FTETotPharm=82.4). In the German-speaking part (31 institutions), this corresponded to 9.9% (FTEClinPharm=14.5; FTETotPharm=146.2) and in the Italian-speaking part (2 institutions) to 27.4% (FTEClinPharm=2.9; FTETotPharm=10.6). In summary, the clinical pharmacy resources differed significantly over the three language regions (p=0.032, figure 1). Median year of establishment for clinical pharmacy services were reported in the French part of Switzerland with 2002 (range: 1989–2010), in the German part with 2007 (range: 1985–2013) and in the Italian part with 2011.
Figure 1.
Ratio of clinical pharmacy practice (red) versus other hospital pharmacy activities (yellow) in the different language areas: French (blue), German (light blue) and Italian (dark blue). Hospital networks are represented as one location. Squares without filling represent areas without any pharmacy information. FTE, full-time equivalent.
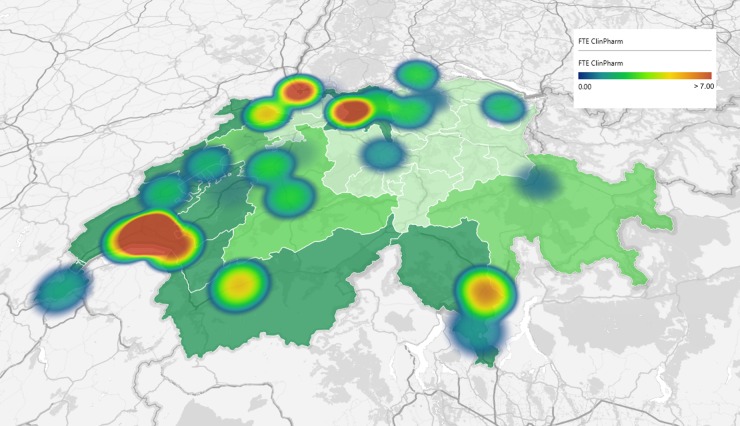
Hospitals in regions without dispensing physicians (n=20) revealed significantly more resources available for clinical pharmacy activities (22.0% of FTETotPharm=135.25) compared with regions with limited (n=8, 6.7% of FTETotPharm=35.8) or full-dispensing rights for physicians (n=16, 6.3% of FTETotPharm=68.1, p=0.026), shown in figure 2.
Figure 2.
Extent of clinical pharmacy practice (full-time equivalent (FTE) heat map, blue=low extent, red=high extent) in parts with no (dark green), partial (green) and unrestricted drug-dispensing physicians (light green).
Structural organisation of ward contact
The 33 institutions providing clinical pharmacy services had resources of 222.2 FTE, of which 35.9 were allocated to patient-centred care. In four (12%) of these institutions, pharmacists worked >50% of their time on the ward. Twenty-six (79%) hospitals mentioned part-time activities with patient contact, while three (9%) institutions reported no presence on the wards.
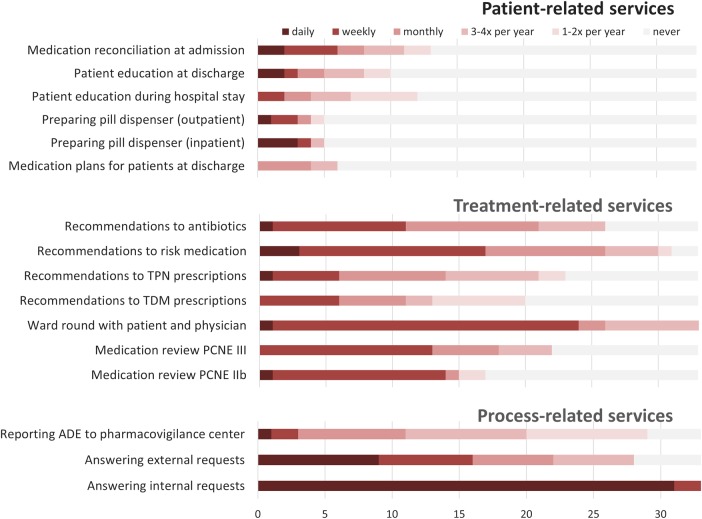
Treatment-related services were more frequent than patient-related activities (figure 3). In 73% of all hospitals with clinical pharmacy services, interdisciplinary ward rounds with pharmacists, nurses and physicians took place weekly. A proportion of 18% of the hospital pharmacists reported weekly involvement of clinical pharmacists in the medication reconciliation process at hospital admission. Meanwhile, pharmacists validated patients’ prescriptions in 9% of institutions at discharge to ambulatory care. Weekly medication reviews according Pharmaceutical Care Network Europe typology20 IIb (medication profile+clinical data) were performed in 42% and type III (medication profile+clinical data+information from physician) in 39% of institutions.
Figure 3.
Clinical pharmacy services were structured into (i) patient-related, (ii) treatment-related and (iii) process-related activities. Only responses from the institutions that provide clinical pharmacy activities were taken into account (n=33). ADE, adverse drug event; PCNE, Pharmaceutical Care Network Europe; TDM, therapeutic drug monitoring; TPN, total parenteral nutrition.
An overview of process-related services revealed ambiguous trends. One-third of all institutions (n=11) maintained a hotline to allow external professionals to ask questions (eg, community pharmacies in case of concern after hospital discharge). A majority of 81% of hospital pharmacies with according services reported daily enquiries from health professionals. Maintaining a hotline for internal professionals was an integral part of the daily routine for 31 out of 33 institutions (94%).
Discussion
To our knowledge, this is the first comprehensive national survey of the clinical pharmacy practice in Switzerland reflecting the practical implementation of a recently introduced theoretical definition. Our data indicated relevant regional differences in the implementation of clinical pharmacy services, while the presence of drug-dispensing physicians seemed to limit the development of clinical pharmacy services.
Characteristics of institutions participating in the survey
All categories of hospitals were represented in the survey. It is surprising that only 47 of 300 listed hospital institutions in Switzerland employed a chief pharmacist. In institutions without GSASA contact information (84%), it may be assumed that no structured clinical pharmacy activities take place since there is no other professional association for hospital or clinical pharmacists in Switzerland.
Interfering factors in the dissemination of clinical pharmacy practice
As a result of the cantonal regulation of the health system in Switzerland, heterogeneous conditions and structures exist and influence the implementation of new disciplines and concepts at the national level. In our study, a significant association between dispensing physicians in ambulatory care and the absence of clinical pharmacy services in hospitals of corresponding regions is shown. In primary care, collaboration between physicians and pharmacists is hampered by this keen competition, which caused multiple public votings with according local altercation between the two professional associations. Apparently this struggle in primary care influenced the collaboration in the institutions. The observed structural differences in drug supply must be clearly evaluated as a disadvantage: hospitals in regions with prevailing dispensing physicians seem to barely tolerate clinical pharmacy activities. This is not favourable in terms of patient safety and cost-effectiveness. A recent study of health insurance data revealed that prescriptions of dispensing physicians show a higher potential for drug-related problems compared with normal prescribing, non-dispensing physicians.21 In order to promote the expansion of the interprofessional collaboration, financial disincentives must be discussed critically. Thus, economic competition in primary care affects collaboration in primary care as well as in hospital care and both effects are critical in regard of patient safety.
Clinical pharmacy practice: discussing a definition's theory and observed realities in Swiss hospitals
From a total of 239.2 FTE of pharmacists in Switzerland, around 15% were assigned to the field of clinical pharmacy. Since the introduction of the certificate ‘FPH Clinical Pharmacy’, 58 pharmacists had successfully graduated until 2013.22 This may represent a first accomplished step in the right direction, leading to an improved involvement by pharmacists in patient care. However, present resources are insufficient for the adequate coverage of needs. The comprehensive and publicly available supervision by clinical pharmacists at present cannot be guaranteed in Swiss hospitals due to a lack of resources (35.9 FTEClinPharm in relation to 1.4 million hospitalisations in 2013).23
Regarding the defined axes of activities, pharmacists’ efforts seem to focus on treatment-related and process-related services. In the institutions with clinical pharmacy services, interprofessional ward rounds seemed well established since they took place regularly. Weekly performed treatment recommendations may be also considered as regular. Since they are only performed on selected wards, a large number of drug-related issues endangering patient safety remain unsolved.
The pharmacist’s competence in answering medication-related questions to hospital staff seemed to be well established and accepted. However, there were hardly any services enabling external access to valid information about a patient’s medication during his hospital stay for community pharmacies and general practitioners. This indicates a huge potential for improvement.
Participation of pharmacists in direct patient-related care was rare, probably due to a lack of resources. A crucial gap was observed in the field of ‘seamless care’. Structured discharge management (eg, medication reconciliation) involving a clinical pharmacist was implemented in <10% of the institutions. No institution reported the involvement of a clinical pharmacist in the validation process of a patient's written medication plan (eg, hand over24 25).
Current resources are not sufficient to ensure comprehensive patient care through clinical pharmacists. We propose to discuss the pattern of resource allocation that might have the highest level of efficiency. To demand a maximum of personal resources for all axes of clinical pharmacy activities at once might not be an effective strategy to maximise the clinical pharmacist’s impact. For example, an optimised medication process may prevent many interventions at the patient level. Therefore, a reasonable balance between the mentioned axes of activities, that is, direct patient contact, optimising the medication process and development of treatment guidelines, seems more reasonable and might become a topic of further investigation of clinical pharmacists’ impact on patient outcome.
Comparing Swiss resources to the international community
Compared with the human resources in North America (FTETotPharm=17.5 per 100 beds),18 Swiss hospitals showed a striking neglect of pharmaceutical expertise in hospitals. Compared with data from Europe 2010,13 Switzerland offered a similar spread of implemented clinical pharmacy services and corresponding gaps in patient-centred care. Around 40% of European institutions provided regular clinical pharmacy services on the wards. The wide range of reported extent (3.6–79.2%) indicates a heterogeneous distribution of resources, analogous to the situation in Switzerland. The European leader in the field of clinical pharmacy practice was the UK. On average, 90% of National Health Services’ institutions carried out daily clinical pharmacy visits on the hospital wards.26 Out of the 30 survey countries, Switzerland ranked on the 20th place right behind the former Yugoslav Republic of Macedonia and just ahead of the Czech Republic.13 In particular, the area of transition of care showed to be neglected in Europe: medication reconciliation supported by a clinical pharmacist took place in only 17% of European institutions upon admission and in 22% at discharge, respectively.13 It remained unclear how regularly and frequently these services were provided. In the year 2000, Canada reported seamless care services in 33% of the examined institutions reaching on average 11% of all patients treated (range: 5–50%).14 In the future, such indicators might become important target values for discussing the impact and extent of the practice of clinical pharmacy, for example, beds supplied with clinical pharmacy services instead of the total number of an institution's beds provided.
Strengths and limitations
Our study has some strengths. First, the high response rate to the survey of 94% of registered and invited chief pharmacists resulted in a comprehensive overview of the actual clinical pharmacy practices in the institutions contacted. Second, a representative sample of participating institutions was achieved by the survey (all general hospitals with central supply level 1 and 80% of general hospitals with central supply level 2). Third, since the survey took a national approach, we report data from all cultural areas of Switzerland and are able to discuss corresponding patterns of resources and influencing factors on the development of clinical pharmacy services.
The survey was designed as a self-declaration, involving several limitations. First, although the established GSASA definition for clinical pharmacy was implied as a standard reference, different perceptions for practice may persist and could not be validated by the authors. To minimise this effect, we tried to narrow the scope of individual beliefs and personal opinions with explanations and clarifications within the survey. Second, individual institutions reported on services that they have developed and established according to local needs, but that could not be divided into the categories of the survey itself. These results could not be considered in the analysis but should be pursued as an innovation in each case. Third, our results allow no statements as to the quality, efficiency and benefits of provided services on patient outcomes.
Conclusion
To our knowledge, this is the first comprehensive national survey of clinical pharmacy practice in Switzerland. Our data show important regional differences in the extent of implementation and pattern of clinical pharmacy services. A striking extent of low dissemination was observed within regions of drug-dispensing physicians in ambulatory care. While interprofessional ward rounds were performed at least periodically in hospitals, which offer clinical pharmacy services, seamless care activities by clinical pharmacists remained insufficiently established.
Key messages.
What is already known on this subject
The pharmacist's involvement in patient care during the hospital stay appears to be highly valuable since the clinical setting and related medication processes are recognised as particularly risky situations.
Around the world, the concept of clinical pharmacy was successfully implemented in the hospital setting with various specific services.
What this study adds
This is the first comprehensive survey of clinical pharmacy practice in Switzerland reflecting the practical implementation of a recently introduced theoretical definition.
Our data show important regional differences in the extent of implementation and pattern of clinical pharmacy services, highlighting a crucial gap in seamless care activities.
In particular, the regional presence of drug-dispensing physicians in the ambulatory care setting seemed to limit the development of clinical pharmacy practice in corresponding hospitals.
Acknowledgments
The authors thank all participating pharmacists for completing the survey and Dr Fabienne Boeni (University of Basel, Switzerland) for proofreading the final manuscript.
Footnotes
Contributors: MM and KAM initiated and conducted the survey. MLL and KEH helped in developing the measurement tools. MM accessed and analysed the data. He also prepared the first draft of the manuscript. KAM, KEH and MLL contributed to the discussion and reviewed the manuscript. They all approved the final version to be published.
Competing interests: None declared.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:533–43. [PubMed] [Google Scholar]
- 2.Penna RP. Pharmaceutical care: pharmacy's mission for the 1990s. Am J Hosp Pharm 1990;47:543–9. [PubMed] [Google Scholar]
- 3.Hohmann C, Neumann-Haefelin T, Klotz JM, et al. . Drug-related problems in patients with ischemic stroke in hospital. Int J Clin Pharm 2012;34:828–31. 10.1007/s11096-012-9690-7 [DOI] [PubMed] [Google Scholar]
- 4.Leendertse AJ, Van Den Bemt PM, Poolman JB, et al. . Preventable hospital admissions related to medication (HARM): cost analysis of the HARM study. Value Health 2011;14:34–40. 10.1016/j.jval.2010.10.024 [DOI] [PubMed] [Google Scholar]
- 5.Kongkaew C, Hann M, Mandal J, et al. . Risk factors for hospital admissions associated with adverse drug events. Pharmacotherapy 2013;33:827–37. 10.1002/phar.1287 [DOI] [PubMed] [Google Scholar]
- 6.Kripalani S, LeFevre F, Phillips CO, et al. . Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA 2007;297:831–41. 10.1001/jama.297.8.831 [DOI] [PubMed] [Google Scholar]
- 7.Nickerson A, MacKinnon NJ, Roberts N, et al. . Drug-therapy problems, inconsistencies and omissions identified during a medication reconciliation and seamless care service. Healthc Q 2005;8 Spec No:65–72. 10.12927/hcq..17667 [DOI] [PubMed] [Google Scholar]
- 8.Anguish I, Wick HD, Fonjallaz MH, et al. . [Hospital's discharge prescription: a challenge for continuity of care and the interprofessional collaboration]. Rev Med Suisse 2013;9:1021–5. [PubMed] [Google Scholar]
- 9.Bondesson A, Eriksson T, Kragh A, et al. . In-hospital medication reviews reduce unidentified drug-related problems. Eur J Clin Pharmacol 2013;69:647–55. 10.1007/s00228-012-1368-5 [DOI] [PubMed] [Google Scholar]
- 10.Pai AB, Boyd A, Depczynski J, et al. . Reduced drug use and hospitalization rates in patients undergoing hemodialysis who received pharmaceutical care: a 2-year, randomized, controlled study. Pharmacotherapy 2009;29:1433–40. 10.1592/phco.29.12.1433 [DOI] [PubMed] [Google Scholar]
- 11.Swiss Society of Public Health Administration and Hospital pharmacists (GSASA). GSASA 1948–2008—Jubilee edition. GSASA J 2008;111–112. [Google Scholar]
- 12.Swiss Society of Public Health Administration and Hospital pharmacists (GSASA). Definition of Clinical Pharmacy in Switzerland. In: (GSASA) SSoPHAaHp, ed. V.1, 2011. Definition of Clinical Pharmacy in Switzerland V1/2011; http://www.gsasa.ch/seiten/aktivitaeten/klinische [Google Scholar]
- 13.Frontini R, Miharija-Gala T, Sykora J. EAHP survey 2010 on hospital pharmacy in Europe: parts 4 and 5. Clinical services and patient safety. Eur J Hosp Pharm 2013;20:69–73. 10.1136/ejhpharm-2013-000285 [DOI] [Google Scholar]
- 14.Bussières J. Hospital Pharmacy in Canada > Clinical Services. Secondary Hospital Pharmacy in Canada > Clinical Services, 2000. http://www.lillyhospitalsurvey.ca/hpc2/content/rep_2000_3.asp
- 15.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration—2002. Am J Health Syst Pharm 2003;60:52–68. [DOI] [PubMed] [Google Scholar]
- 16.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration—2005. Am J Health Syst Pharm 2006;63:327–45. 10.2146/ajhp050538 [DOI] [PubMed] [Google Scholar]
- 17.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration—2008. Am J Health Syst Pharm 2009;66:926–46. 10.2146/ajhp080715 [DOI] [PubMed] [Google Scholar]
- 18.Pedersen CA, Schneider PJ, Scheckelhoff DJ. ASHP national survey of pharmacy practice in hospital settings: dispensing and administration—2011. Am J Health Syst Pharm 2012;69:768–85. 10.2146/ajhp110735 [DOI] [PubMed] [Google Scholar]
- 19.Schneider T. Key figures of Swiss hospitals, 2011. In: (BAG) BfG, ed, 2013 Statistics on health insurance, Federal Office of Public Health; 2013;7:45–349. [Google Scholar]
- 20.Pharmaceutical Care Network Euorpe (PCNE). Workshop report ‘PCNE Working Symposium 2014, Sliema, Malta / Medication review, Drug-related problems, Standards and Guidelines’. Secondary Workshop report ‘PCNE Working Symposium 2014, Sliema, Malta / Medication review, Drug-related problems, Standards and Guidelines’ 2014. http://www.pcne.org/conference/9/pcne-working-symposium-2014
- 21.Blozik E, Rapold R, Reich O. Prescription of potentially inappropriate medication in older persons in Switzerland: does the dispensing channel make a difference? Risk Manag Healthc Policy 2015;8:73–80. 10.2147/RMHP.S78179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Swiss Society of Public Health Administration and Hospital pharmacists (GSASA). 2015. http://www.gsasa.ch/seiten/bildung/fph-klinische-pharmazie/weiterbildung-klinische-pharmazie/ [Google Scholar]
- 23.Swiss Federal Statistical Office. Medical statistics of Swiss hospitals 2013—standard tables [Medizinische Statistik der Krankenhäuser 2013—Standardtabellen], 2015.
- 24.Claeys C, Dufrasne M, De Vriese C, et al. . [Information transmission to the community pharmacist after a patient's discharge from the hospital: setting up of a written medication discharge form, prospective evaluation of its impact, and survey of the information needs of the pharmacists]. J Pharm Belg 2015;97:42–54. [PubMed] [Google Scholar]
- 25.Starmer AJ, Spector ND, Srivastava R, et al. . Changes in medical errors after implementation of a handoff program. N Engl J Med 2014;371:1803–12. 10.1056/NEJMsa1405556 [DOI] [PubMed] [Google Scholar]
- 26.McLeod M, Ahmed Z, Barber N, et al. . A national survey of inpatient medication systems in English NHS hospitals. BMC Health Serv Res 2014;14:93 10.1186/1472-6963-14-93 [DOI] [PMC free article] [PubMed] [Google Scholar]