Abstract
Objectives
Hypertension is among the leading causes of cardiovascular disease worldwide. No previous studies have examined specifically the types of drug-related problems (DRPs) in patients with hypertension, and how these problems affect blood pressure control. So, the primary aim of this study was to investigate the prevalence and nature of DRPs in outpatients with hypertension and reveal any associations between DRPs and blood pressure control in these patients.
Methods
This was a cross-sectional correlation study. A total of 200 patients who fulfilled the inclusion criteria were recruited through outpatient clinics. Patients’ data were assessed to identify DRPs using a systematic evidence-based approach.
Results
Two hundred participants were recruited in this cross-sectional study. About half of the participants (48.5%) had uncontrolled hypertension. The average number of DRPs was 6.31±2.63. The main identified DRPs affecting blood pressure control included patients’ lack of knowledge about their medications, lack of adherence to their medications, suboptimal efficacy of medications prescribed and the need for additional monitoring. Logistic regression analysis was performed to identify the most important predictors, and significant associations were found between poor blood pressure control and the above-identified variables except for knowledge about medication (p≤0.05).
Conclusion
The number of DRPs among patients with hypertension is relatively high. These DRPs were associated with poor blood pressure control. The implementation of clinical pharmacy services for all patients with hypertension is strongly recommended.
Keywords: Drug related problems, pharmaceutical care, Jordan, Outpatient
Introduction
Hypertension is among the leading causes of cardiovascular disease worldwide.1 2 Unawareness and poor control of hypertension remain important national health concerns.3–6 Although factors such as decreased access to medical care and financial barriers contribute to low control, blood pressure control is poor even in patients who can receive pharmacological treatment.7 In Jordan, the prevalence of hypertension is very high approaching 32.3%.8 Among those populations of patients with hypertension, it was found that only 39.6% of the patients had controlled blood pressure value, with the majority of patients not achieving their blood pressure goal.8
Many factors were found to be significantly associated with blood pressure control. Poor adherence to evidence-based guideline recommendations, adverse effects of blood pressure-lowering drugs, attitudes of patients in relation to disease and treatments, poor adherence to medications and lack of structured, efficient healthcare facilities are some reasons for the low rates of hypertension control.9–13
Patients with hypertension often receive multiple medications and have different comorbid chronic diseases that can lead to the occurrence of drug-related problems (DRPs).14 15 A DRP is an event or circumstance involving medication therapy that actually or potentially interferes with an optimum outcome for a specific patient.16 Although there are several studies that investigated the impact of pharmaceutical care on blood pressure control,11 17–20 none explored specifically the types of DRPs in patients with hypertension, and how these problems affect blood pressure control.
The primary aim of this study was to investigate the prevalence and nature of DRPs in outpatients with hypertension and to reveal any association between DRPs and blood pressure control in these patients.
Methods
Study design and clinical setting
This cross-sectional correlation study was approved by the Institutional Review Board at the Jordan University Hospital, and was carried out at the outpatients’ cardiac clinics at Jordan University Hospital. The study was conducted over a 3-month period.
Study subjects
During the 3 months’ study period, the outpatient cardiac clinic served 1300 patients eligible for inclusion who were diagnosed with primary hypertension. However, we were able to approach only 209 patients (15%), from which, 200 patients agreed to take part in the study (response rate 95.7%). Inclusion criteria included adult patients (≥18 years of age) with doctor diagnosis of primary hypertension for at least 6 months, receiving treatment for hypertension with no change in medication regimen for at least 1 month. Patients were excluded if they were diagnosed by the physician with secondary hypertension (such as renovascular disease, pheochromocytoma, Cushing’s syndrome and primary aldosteronism) or if they were going through hypertensive crisis (defined as systolic blood pressure >180 mm Hg or diastolic blood pressure >120 mm Hg).
Data collection
Patients visiting outpatient clinics at the Jordan University Hospital were approached for participation in the study using convenient sampling technique. Patients who responded to the researcher were offered to participate in the study, and an information leaflet was provided on acceptance. Verbal consent was sought from the respondent before study entry.
All participants had their blood pressure measured at one arm while seated, after at least 5 min of rest. Measurements were obtained by the researcher, who is also an experienced clinical pharmacist (RAF) using an auscultatory sphygmomanometer. Three previous blood pressure readings were also obtained from the patients’ files (if they were obtained within the last 3 months), and an average blood pressure reading was calculated for the patient to evaluate their blood pressure control. Hypertension is considered controlled according to Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) criteria if patient's average blood pressure was below 140/90 mm Hg or below 130/80 mm Hg in patient with diabetes or those with chronic renal failure; otherwise, patient is considered to have uncontrolled hypertension.
Patient's medical file was reviewed to collect information regarding their demographic information, clinical tests performed (fasting plasma glucose, serum creatinine, cholesterol, triglyceride, high-density lipoprotein, low-density lipoprotein and haemoglobin A1c), date of the clinical tests (whether they were taken within the last 3 months or not) and also to obtain information about the patient's diagnosed conditions, drug therapies and any other medical problems.
Patient's adherence and knowledge towards pharmacological and non-pharmacological therapies were also assessed using validated questionnaire.
Classification of DRPs
For the classification of DRPs, AbuRuz et al21 classification system was used. DRPs were divided into six main categories: (1) indication, (2) effectiveness, (3) safety, (4) knowledge, (5) adherence and (6) miscellaneous.
Identification of DRPs
All types of DRPs were identified using a systematic approach.22 DRPs affecting effectiveness were identified through comparing patients’ treatment with current evidence-based guideline recommendations. The JNC 7 recommendation was used to determine effectiveness of treatment and appropriateness of treatment.23 For patients suffering from other diseases, their treatment was evaluated using the appropriate updated evidence-based treatment guidelines for the documented diseases. Appropriateness of dosing regimen was checked by comparing doses with evidence-based guideline recommendations. The I-fact (Facts and Comparison, 2010) was used for identifying major drug–drug interactions.
Problems towards adherence to medications or lifestyle activities were assessed using a validated translation of the scale developed by Morisky et al.24 Adherence scale was first translated to Arabic and then back translated to English following a worldwide recognised approach for translation and adoption of instruments. Patient's knowledge was assessed based on ability to answer correctly the questionnaire related to their medications and lifestyle activities. All the Arabic versions of questionnaires (for both adherence and knowledge) were tested for face and content validity by the authors of the study, and questions were adjusted as appropriate.
Sample size calculation
A pilot study was conducted initially on 30 patients to estimate the average number of DRPs in patients with controlled and those with uncontrolled hypertension. The mean difference in DRPs was 2.5, and SDs were 2.3 and 1.8 in patients with controlled and uncontrolled hypertension, respectively. Setting α at 0.05 and using power of 80%, the minimum required sample size to obtain a significant difference was calculated as 12 subjects per group. A sample size of 200 was decided to be involved in the study in order to have more generalisable results.
Data analysis
Data were coded and entered into Statistical Package for Social Science V.17 (SPSS Chicago, Illinois, USA). Group differences (controlled and uncontrolled hypertension) were studied using bivariate analysis that is, independent sample Student's t test for continuous independent variables and χ2 analysis for categorical independent variables. Based on the information obtained from the bivariate analysis, a framework for the risk factors associated with uncontrolled hypertension was developed using logistic regression analysis.
Results
Demographic and clinical characteristics of the study sample
The demographic and clinical characteristics of the sample are shown in table 1. The mean age of patients was around 59.7 years (SD=10.2); males accounted for 39.5% of all the patients recruited. About half of the participants (51.5%) had controlled hypertension, with a mean value of 126/77 mm Hg.
Table 1.
Demographic and clinical characteristics of study sample (n=200)
| Parameter | |
|---|---|
| Age (mean (SD)) years | 59.7 (10.2) |
| Gender: male, n (%) | 79 (39.5) |
| Marital status, n (%) | |
| Single | 2 (1) |
| Married | 163 (81.5) |
| Widowed | 34 (17) |
| Divorced | 1 (0.5) |
| Education, n (%) | |
| Not educated | 27 (13.5) |
| Primary | 89 (44.5) |
| Secondary | 12 (6) |
| High school | 22 (11) |
| Control of hypertension, n (%) | |
| Controlled | 103 (51.5) |
| Uncontrolled | 97 (48.5) |
| Blood pressure (systolic/diastolic) mm Hg (mean (SD)) | |
| Controlled | 126/77 (9.7/6.3) |
| Uncontrolled | 150/88 (14.0/8.01) |
| Duration of hypertension (years) (mean (SD)) | |
| Controlled | 7.7 (6.2) |
| Uncontrolled | 9.1 (6.5) |
| Number of prescribed medications (mean (SD)) | |
| Controlled | 6.1 (2.5) |
| Uncontrolled | 6.8 (2.6) |
Drug-related problems
The total number of identified DRPs was 1261 (average 6.31, SD 2.63, range 0–15). Figure 1 shows the number and percentage of the different categories of the identified DRPs. DRPs affecting effectiveness were the most frequently identified DRPs among the study sample, approximating for 29.60%. Within effectiveness DRPs, drug interactions were the most common. ‘Untreated condition’ was the least frequent DRPs identified, accounting for 1.59% of the total DRPs identified in the study sample.
Figure 1.
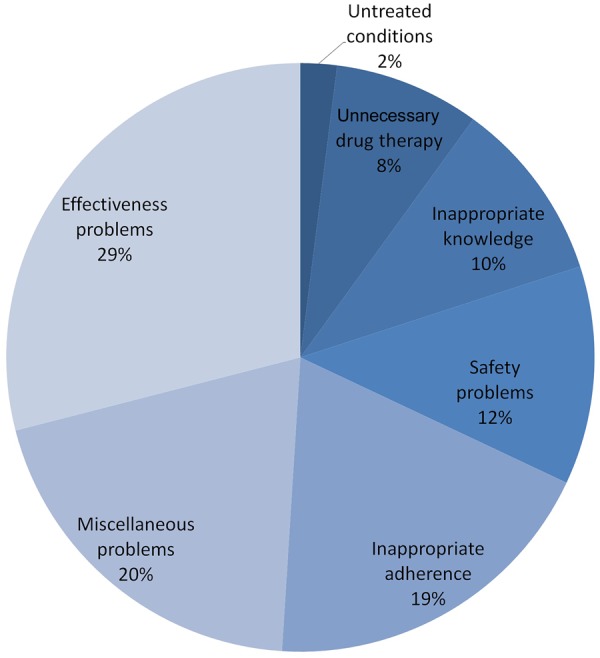
Percentage of different categories of drug-related problems identified among patient with hypertension (n=200). Total number of drug-related problems was 1261.
Effect of DRPs on blood pressure control
Initial screening of data showed a significant association between number of DRPs and poor blood pressure control (independent sample t test, p<0.05) (figure 2).
Figure 2.
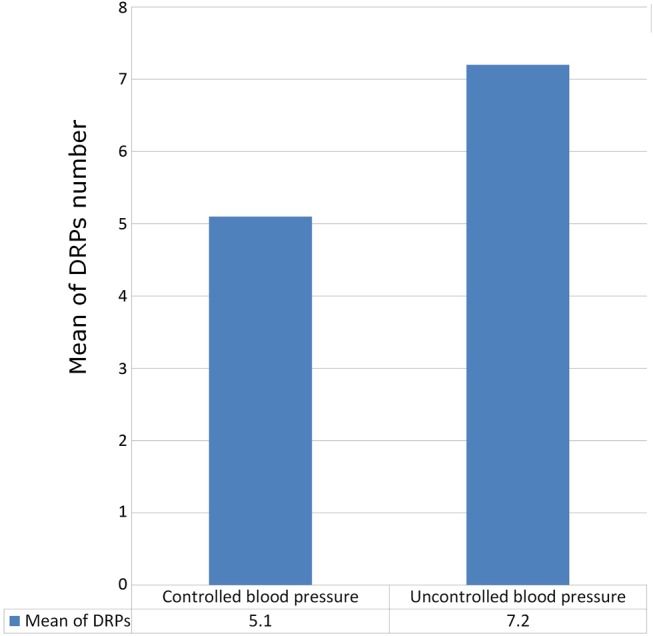
Differences among respondents with controlled and uncontrolled hypertension with regard to drug-related problems (DRPs) identified. SD for controlled and uncontrolled group was 2.2 and 2.4, respectively (*significant at 0.05 level).
A bivariate analysis was applied to determine exactly which classes of DRPs significantly affect blood pressure control. Four classes of DRPs were significantly associated with poor blood pressure control (p<0.05). These classes included knowledge about medications, adherence to medications, effectiveness DRPs and the need for additional monitoring (table 2).
Table 2.
Differences among respondents with controlled and uncontrolled hypertension with regard to specific classes of actual drug-related problems identified
| Actual drug-related problem categories | Hypertension control | |||
|---|---|---|---|---|
| Controlled (103) | Uncontrolled (97) | p Value | OR | |
| Indication drug-related problems (yes, n (%)) | 49 (47.6) | 50 (51.5) | 0.574 | 1.172 |
| Effectiveness drug-related problems (yes, n (%)) | 44 (42.7) | 78 (80.4) | 0.000* | 5.505 |
| Safety drug-related problems (yes, n (%)) | 42 (40.8) | 46 (47.4) | 0.344 | 1.310 |
| Adherence to medications (non-adherent, n (%)) | 36 (35.0) | 49 (50.5) | 0.026* | 1.900 |
| Adherence to self-care activities (non-adherent, n (%)) | 78 (75.7) | 81 (83.5) | 0.173 | 1.623 |
| Knowledge about medications (poor knowledge, n (%)) | 38 (36.9) | 56 (57.7) | 0.003* | 2.336 |
| Knowledge about self-care activities (poor knowledge, n (%)) | 17 (16.5) | 18 (18.6) | 0.703 | 1.153 |
| Miscellaneous drug-related problems (yes, n (%)) | 68 (66.0) | 84 (86.6) | 0.001* | 3.326 |
*Significant at 0.05 level, χ2 test.
Some of the identified variables may affect blood pressure as a consequence of their correlation and interaction with other variables. Therefore, logistic regression was performed to find out the factors which were independently and significantly associated with blood pressure control.
All variables identified above (table 2) were entered into logistic regression analysis to identify the most important predictors. Result revealed three of preidentified variables (adherence to medications, effectiveness DRPs and need for additional monitoring) were significantly associated with poor blood pressure control (p≤0.05) (table 3).
Table 3.
Logistic regression for actual drug-related problems identified, affecting blood pressure control
| Variables | B | SE | p Value | OR | 95% CI for OR |
|---|---|---|---|---|---|
| Indication drug-related problems (1: no; 2: yes) | −0.080 | 0.349 | 0.819 | 0.923 | 0.460 to 1.830 |
| Effectiveness drug-related problems (1: no; 2: yes) | 1.786 | 0.352 | 0.000* | 5.966 | 2.990 to 11.903 |
| Safety drug-related problems (1: no; 2: yes) | 0.120 | 0.338 | 0.722 | 1.128 | 0.582 to 2.187 |
| Adherence to medications (1: adherent; 2: non-adherent) | 0.867 | 0.356 | 0.015* | 2.379 | 1.185 to 4.777 |
| Adherence to about self-care activities (1: adherent; 2: non-adherent) | 0.724 | 0.427 | 0.090 | 2.062 | 0.893 to 4.760 |
| Knowledge about medications (1: good; 2: poor) | 0.614 | 0.353 | 0.082 | 1.848 | 0.924 to 3.693 |
| Knowledge about self-care activities (1: good; 2: poor) | −0.647 | 0.483 | 0.180 | 0.523 | 0.203 to 1.349 |
| Miscellaneous drug-related problems (1: no; 2: yes) | 1.382 | 0.448 | 0.002* | 3.982 | 1.655 to 9.577 |
*Significant at 0.05 level.
A test of the final model against a constant-only model was statistically reliable, χ2 ((degree of freedom of 8)=55.945, p<0.0005), indicating that the predictors, as a set, reliably distinguished between patients with controlled and uncontrolled hypertension. The variance in blood pressure control accounted for by the predictors was 32.5% (Nagelkerke R2).
Discussion
To our knowledge, the association between DRPs and blood pressure was not previously investigated in the literature. This is the first study to reveal the association between DRPs in patients with hypertension and its effect on their blood pressure control.
Results of this study revealed a high number of DRPs in patients with hypertension. The average number of DRPs was 6.31 per patient. To date, there has been no comparable study done specifically on DRPs in patients with hypertension both locally and globally. The number of DRPs identified was three times higher than the number detected by other study, which was conducted in patients who had diabetes mellitus with hypertension.15
Drug interactions, dose regimen issues and the need for additional therapy were the most frequent type of DRPs identified. These results were comparable with previous study, which found that drug choice problems and drug interactions were among the most frequent categories of DRPs in patients who had diabetes with hypertension.15
Non-adherence to medication was significantly associated with poor blood pressure control at both bivariate and multivariate regression. It was found that poor adherence to medication increased the risk of having uncontrolled blood pressure by 137.9% compared with adherent patients (OR 2.37). This finding was similar to previously published reports that examined the relationship of blood pressure control with an index of compliance, and found that poor blood pressure control was associated with a lower compliance index (p>0.05).25 Also another study suggested that in order to increase the effectiveness of medical care for hypertension, it is important to improve compliance with antihypertensive agents.26 These results stresses on the importance of improving compliance with antihypertensive agents in order to increase the effectiveness of medical care for patients with hypertension.
Although the impact of poor adherence to medications is well known in the literature, the effect of both effectiveness DRPs and the need for additional monitoring on blood pressure were not covered previously in the literature. Presence of effectiveness DRPs was found to increase the risk of having uncontrolled hypertension by 496.6% compared with those without effectiveness DRPs (OR 5.966). The need for additional monitoring such as ‘need for lipid profile monitoring or HBA1c monitoring’ was also found to increase the odds of being with uncontrolled hypertension by 298.2% compared with those without these problems (OR 3.982).
It is worth mentioning the main limitations of this study: (1) this study was conducted only in one centre, and therefore, may not be representative of the whole patients’ population; (2) the severity of DRPs, the proportion of self-medication and use of alternative and complementary medicines were not assessed; (3) since this study used a convenient sampling approach rather than random sampling, the results may not be representative of all patients with hypertension attending the Jordan University Hospital; (4) also, we did not study the impact of each DRP on other clinical outcomes or total healthcare costs and (5) we did not make suggestions for resolving the issue of the detected DRPs, and did not discuss the results of the review and possible solutions with the responsible physician.
Conclusion
The number of DRPs among patients with hypertension is relatively high in both patients with controlled and uncontrolled blood pressure. These DRPs were associated with poor blood pressure control. A more valid design is needed to investigate how and how much resolving identified DRPs will impact blood pressure control. Pharmaceutical care services are strongly recommended for all patients with hypertension, even those with controlled blood pressure who suffer from several DRPs. Effectiveness, adherence and monitoring DRPs should be given the highest priority.
Key messages.
What is already known on this subject?
Unawareness and poor control of hypertension remain important national health concerns.
Many factors were found to be significantly associated with blood pressure control.
What this study adds?
The number of drug-related problems (DRPs) among patients with hypertension is considered relatively high and DRPS are associated with poor hypertension control.
Pharmaceutical care services are strongly recommended for all patients with hypertension.
Effectiveness, adherence and monitoring DRPs should be given the highest priority when providing pharmaceutical care to patients with hypertension.
Footnotes
Contributors: The authors declare that all authors have substantial contributions towards the conception or design of the work, or the acquisition, analysis or interpretation of data.
Competing interests: None declared.
Ethics approval: Institutional Review Board at the Jordan University Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kearney PM, Whelton M, Reynolds K, et al. . Worldwide prevalence of hypertension: a systematic review. J Hypertens 2004;22:11–19. 10.1097/00004872-200401000-00003 [DOI] [PubMed] [Google Scholar]
- 2.Wong ND, Dede J, Chow VH, et al. . Global cardiovascular risk associated with hypertension and extent of treatment and control according to risk group. Am J Hypertens 2012;25:561–7. 10.1038/ajh.2012.2 [DOI] [PubMed] [Google Scholar]
- 3.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988–2000. JAMA 2003;290:199–206. 10.1001/jama.290.2.199 [DOI] [PubMed] [Google Scholar]
- 4.Amar J, Chamontin B, Genes N, et al. . Why is hypertension so frequently uncontrolled in secondary prevention? J Hypertens 2003;21:1199–205. 10.1097/01.hjh.0000059035.65882.ca [DOI] [PubMed] [Google Scholar]
- 5.Lang T, de Gaudemaris R, Chatellier G, et al. . Prevalence and therapeutic control of hypertension in 30 000 subjects in the workplace. Hypertension 2001;38:449–54. 10.1161/01.HYP.38.3.449 [DOI] [PubMed] [Google Scholar]
- 6.Pickering TG. Therapeutic inertia and the medicare crisis. J Clin Hypertens 2006;8:667–70. 10.1111/j.1524-6175.2006.05125.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med 2001;345:479–86. 10.1056/NEJMoa010273 [DOI] [PubMed] [Google Scholar]
- 8.Jaddou HY, Batieha AM, Khader YS, et al. . Hypertension prevalence, awareness, treatment and control, and associated factors: results from a national survey, Jordan. Int J Hypertens 2011;2011:828797 10.4061/2011/828797 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neutel JM, Smith DH. Improving patient compliance: a major goal in the management of hypertension. J Clin Hypertens (Greenwich) 2003;5:127–32. 10.1111/j.1524-6175.2003.00495.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oliveria SA, Lapuerta P, McCarthy BD, et al. . Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med 2002;162:413–20. 10.1001/archinte.162.4.413 [DOI] [PubMed] [Google Scholar]
- 11.Orozco-Beltran D, Brotons C, Moral I, et al. . [Factors affecting the control of blood pressure and lipid levels in patients with cardiovascular disease: the PREseAP Study]. Rev Esp Cardiol 2008;61:317–21. 10.1157/13116661 [DOI] [PubMed] [Google Scholar]
- 12.Ferrari P. Reasons for therapeutic inertia when managing hypertension in clinical practice in non-Western countries. J Hum Hypertens 2009;23:151–9. 10.1038/jhh.2008.117 [DOI] [PubMed] [Google Scholar]
- 13.Bulatova NR, Yousef A-M, AbuRuz SD, et al. . Hypertension management and factors associated with blood pressure control in Jordanian patients attending cardiology clinic. Trop J Pharm Res 2013;12:827–33. 10.4314/tjpr.v12i5.25 [DOI] [Google Scholar]
- 14.Munger M. Polypharmacy and combination therapy in the management of hypertension in elderly patients with co-morbid diabetes mellitus. Drugs Aging 2010;27:871–83. 10.2165/11538650-000000000-00000 [DOI] [PubMed] [Google Scholar]
- 15.Zaman Huri H, Fun Wee H. Drug related problems in type 2 diabetes patients with hypertension: a cross-sectional retrospective study. BMC Endocr Disord 2013;13:2 10.1186/1472-6823-13-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm 1990;47:533–43. [PubMed] [Google Scholar]
- 17.Garcao JA, Cabrita J. Evaluation of a pharmaceutical care program for hypertensive patients in rural Portugal. J Am Pharm Assoc (Wash) 2002;42:858–64. 10.1331/108658002762063691 [DOI] [PubMed] [Google Scholar]
- 18.Zhao P-X, Wang C, Qin L, et al. . Effect of clinical pharmacist's pharmaceutical care intervention to control hypertensive outpatients in China. Afr J Pharm Pharmacol 2012;6:48–56. 10.5897/AJPP11.633 [DOI] [Google Scholar]
- 19.de Souza WA, Yugar-Toledo JC, Bergsten-Mendes G, et al. . Effect of pharmaceutical care on blood pressure control and health-related quality of life in patients with resistant hypertension. Am J Health Syst Pharm 2007;64:1955–61. 10.2146/ajhp060547 [DOI] [PubMed] [Google Scholar]
- 20.Robinson JD, Segal R, Lopez LM, et al. . Impact of a pharmaceutical care intervention on blood pressure control in a chain pharmacy practice. Ann Pharmacother 2010;44:88–96. 10.1345/aph.1L289 [DOI] [PubMed] [Google Scholar]
- 21.AbuRuz SM, Bulatova NR, Yousef AM. Validation of a comprehensive classification tool for treatment-related problems. Pharm World Sci 2006;28:222–32. 10.1007/s11096-006-9048-0 [DOI] [PubMed] [Google Scholar]
- 22.Aburuz S. The case for evidence-based pharmaceutical care. Res Social Adm Pharm 2015;11:e146–7. 10.1016/j.sapharm.2009.06.001 [DOI] [PubMed] [Google Scholar]
- 23.Chobanian AV, Bakris GL, Black HR, et al. . The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA 2003;289:2560–72. 10.1001/jama.289.19.2560 [DOI] [PubMed] [Google Scholar]
- 24.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67–74. 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 25.Caldwell JR, Theisen V, Kaunisto CA, et al. . Psychosocial factors influence control of moderate and severe hypertension. Soc Sci Med 1983;17:773–82. 10.1016/0277-9536(83)90028-X [DOI] [PubMed] [Google Scholar]
- 26.Ren XS, Kazis LE, Lee A, et al. . Identifying patient and physician characteristics that affect compliance with antihypertensive medications. J Clin Pharm Ther 2002;27:47–56. 10.1046/j.1365-2710.2002.00387.x [DOI] [PubMed] [Google Scholar]


