Abstract
Aims:
To evaluate the prospective association between baseline and 9-year change in alcohol consumption and long-term risk of diabetes and whether these associations might be modified by sex and/or body mass index.
Methods:
We conducted a prospective analysis of 12,042 Atherosclerosis Risk in Communities (ARIC) Study participants without prevalent diabetes (55% women, 78% white, mean age 54 years). Alcohol consumption was assessed at visit 1 (1987–1989) and visit 4 (1996–1998). We used Cox models to estimate hazard ratios for diabetes risk by baseline drinking categories and change in alcohol consumption, stratified by sex and obesity status.
Results:
During a median follow-up of 21 years, there were 3,795 incident diabetes cases. Among women, consuming 8–14 drinks/week was associated with a significantly lower risk of diabetes (HR 0.75, 95%CI, 0.58–0.96) compared to current drinkers consuming ≤1 drink/week. Among men, consuming 8–14 drinks/week was associated with a borderline significant lower risk of diabetes (HR 0.84, 95%CI 0.70–1.00) and consuming >14 drinks/week was associated with a significantly lower risk of diabetes (HR 0.81, 95%CI 0.67–0.97) (p-for-sex interaction <0.01). In both sexes, among current drinkers, there was a significant decreasing trend in diabetes risk as the alcohol consumption increased. The association was modified by body mass index (p-for-interaction=0.042 for women, p-for-interaction<0.001 for men). In women, the inverse association was only seen among overweight and obese participants. In men, the inverse association was more pronounced among obese participants. On average, drinking status did not change substantially over the 9-year period. For men with alcohol intake ≥7 drinks/week at baseline, decreasing alcohol intake was associated with higher risk of diabetes (HR per daily drink-decrease 1.12, 95%CI, 1.02–1.23).
Conclusions:
In this community-based population, there was an inverse association of alcohol consumption with diabetes risk. The amount of the alcohol consumption associated with lower risk was different in women and men, and the association was stronger among participants with higher BMI.
Keywords: diabetes, alcohol
INTRODUCTION
The incidence of diabetes has increased substantially over the past two decades [1]. Both genetic factors and environmental factors contribute to the risk of diabetes. As a modifiable behavior, alcohol consumption has been suggested to be relevant to diabetes risk. There is a large body of literature suggesting a protective effect of moderate alcohol consumption on cardiovascular risk and cardiometabolic risk factors, including diabetes [2–4], but the impact of alcohol on cardiovascular and overall population health remains controversial [5, 6]. Intervention studies have suggested that alcohol consumption might improve insulin sensitivity among women [4]. Some prior observational studies have found a protective association of moderate alcohol consumption on diabetes risk, but this association has differed by sex and adiposity in some reports [7–16]. The previous literature has shown U- or J- shaped associations between alcohol consumption and risk of future diabetes [7, 9, 11, 14, 15], with evidence in some cohorts for stronger inverse associations in women [8, 10, 13] and associations by adiposity status have been inconsistent [8, 16]. Furthermore, few prior studies have examined changes in alcohol consumption and risk of future diabetes in the general population [17].
The objective of the present study was to examine whether associations of alcohol consumption with diabetes risk might differ by sex or body mass index (BMI) in a community-based population with long-term follow-up for incident diabetes. We also undertook analyses to assess changes in alcohol consumption patterns over time with risk of diabetes.
METHODS
Study population
The Atherosclerosis Risk in Communities (ARIC) Study is a large, ongoing cohort of predominately black and white middle-aged adults from four U.S. communities. A total of 15,792 participants attended visit 1 which took place from 1987 to 1989. Subsequent visits took place in 1990–1992 (visit 2), 1993–1995 (visit 3), 1996–1998 (visit 4), and 2011–2013 (visit 5).
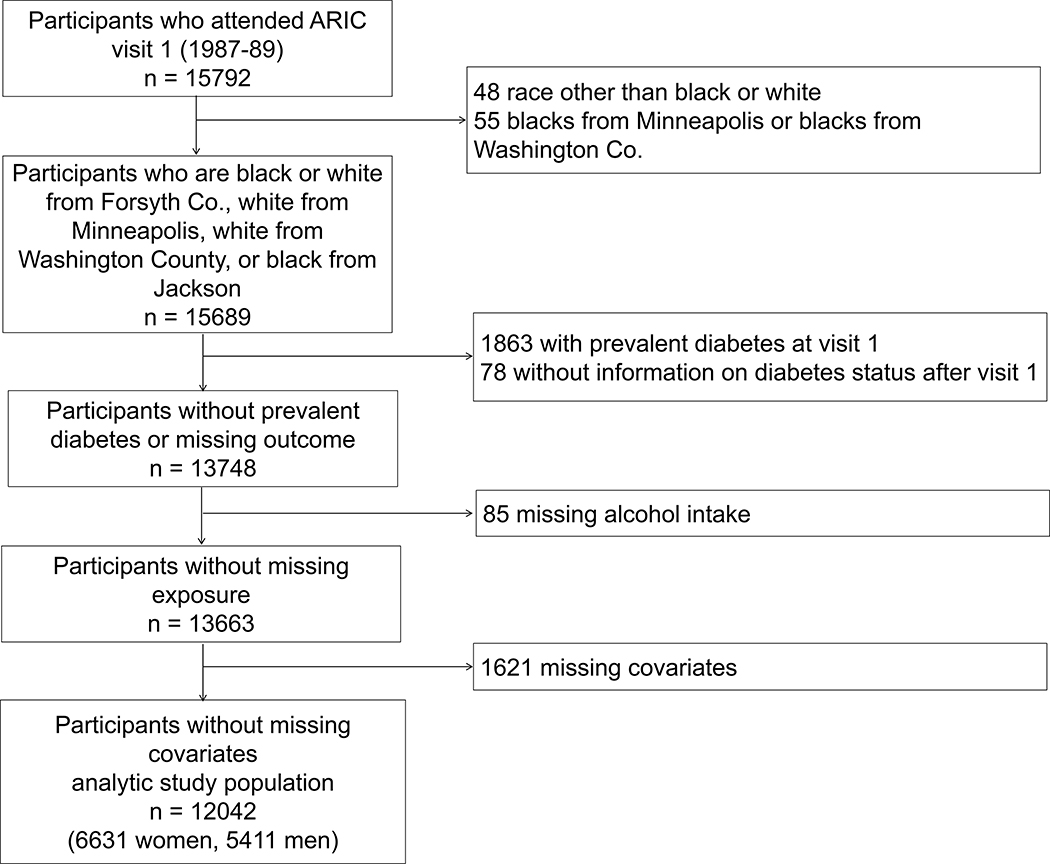
For the present study, we excluded the small number of participants with race other than black or white (n=48); blacks from Minneapolis, Minnesota (n=22); and blacks from Washington County, Maryland (n=33). We additionally excluded participants with prevalent diabetes (n=1,863), as well as those who were missing the following information: diabetes status after visit 1 (n=78), alcohol consumption (n=85), total cholesterol (n=189), fasting glucose (missing glucose or missing fasting status, n=306), education (n=19), hypertension (n=60), BMI (n=6), waist-hip ratio (n=6), smoking status (n=6), household income (n=742), coronary heart disease (n=252), or physical activity (n=35). Thus, our final analytic population included 12,042 participants, of which 6,631 were women and 5,411 were men (eFigure 1).
eFig 1.
Participants included in the study population
Assessment of alcohol intake
Information on alcohol consumption and the usual amount of alcohol consumption among current-drinkers was obtained during ARIC visit 1 (1987 to 1989) and visit 4 (1996 to 1998). We categorized baseline alcohol consumption into 6 groups according to the following questions: “Do you presently drink alcoholic beverages?” and “Have you ever consumed alcoholic beverages?”. Among participants who answered yes to the first question (current drinkers), the following questions were asked: “How many glasses of wine do you usually have per week (4-ounce glasses)?”, “How many bottles or cans of beer do you usually have per week (12-ounce bottles or cans)?”, and “How many drinks of hard liquor do you usually have per week (1.5-ounce shots)?”. We defined never drinkers as participants who answered no to the first two questions and former drinkers as participants who answered no to the first question and yes to the second. We further categorized current drinkers into 4 groups according to the last three questions. Therefore, our analysis included 6 categories: never drinkers, former drinkers, current drinkers consuming ≤1 drink/week, current drinkers consuming 2–7 drinks/week, current drinkers consuming 8–14 drinks/week, and current drinkers consuming >14 drinks/week. We also evaluated 9-year changes (visit 1 to visit 4) in alcohol consumption status with risk of diabetes (after visit 4), where the amount of alcohol consumption for non-drinkers was set to zero.
Assessment of incident diabetes
For our analyses of baseline alcohol consumption with future diabetes risk, incident diabetes was defined as a fasting glucose >126 mg/dL or a non-fasting glucose >200 mg/dL (assessed at any of the four follow-up visits), current use of diabetes medication or self-report of a physician diagnosis of diabetes (assessed at each follow-up visit and during annual telephone calls to all participants occurring following visit 4), or current use of diabetes medication assessed at visit 5.
Participants with prevalent diabetes at baseline (based on elevated glucose, self-reported diagnosis, or medication use) were excluded. We followed the participants from their first visit (1987–1989) until they developed diabetes, were lost to follow-up, or administrative censoring at December 31, 2015, whichever came first.
Covariates
Demographic covariates included age, sex, and race-center. We adjusted for race-center as a 5-category variable: whites from Forsyth County, North Carolina; whites from Minneapolis, Minnesota; whites from Washington County, Maryland; blacks from Forsyth Couty, North Carolina; and blacks from Jackson, Mississippi. Smoking status, education, household income, and parental history of diabetes were assessed during the in-person visits using standard questionnaires. Total energy intake was derived from a food frequency questionnaire, including total calorie intake from dietary and ethanol consumption, but excluding other calories from alcoholic beverages. Blood pressure was measured three times on each participant, and the mean of the second and the third readings was taken. Participants with a mean systolic blood pressure ≥140 mmHg, mean diastolic blood pressure ≥90 mmHg, or use of antihypertensive medication were classified as having hypertension. Participants with any of the following were classified as having coronary heart disease: myocardial infarction defined based on a history of myocardial infarction (self-reported or physician-reported) or using electrocardiography data, self-reported heart or arterial surgery, coronary bypass, or angioplasty of coronary artery(ies). Physical activity was assessed using the Baecke questionnaire [18]. BMI (kg/m2) and waist-hip ratio was calculated from measured weight, height, waist circumference, and hip circumference assessed during the visit.
Statistical analyses
We conducted analyses stratified by sex since the association has been reported to differ in men and women. We used multivariable Cox proportional hazards models to estimate the hazard ratios for the associations between alcohol consumption categories at baseline and risk of incident diabetes. Current-drinkers reporting ≤1 drink/week served as the reference group in the analyses. Model 1 included age, race-center, and total energy intake. Model 2 included all variables in Model 1 plus education (less than high school, high school degree or vocational school, at least some college or professional school), household income (< $25,000 per year, $25,000-$49,999 per year, ≥ $50,000 per year), parental history of diabetes (yes, no), physical activity (continuous, 1 to 5), high-density lipoprotein (HDL) cholesterol, total cholesterol, baseline fasting glucose; and time-varying BMI (normal-weight, overweight, obese), waist-hip ratio (continuous), hypertension history (yes, no), and smoking status (never smokers, former smokers, current smokers). For the missing data of these 4 time-varying covariates, we carried forward the last observation. We also tested the trend among current drinkers in the two models for both sexes, by modeling the 4 categoties of current drinkers as ordinal variables instead of nominal. We also compared the risk of diabetes in participants consuming ≥2 drinks/week to those consuming ≤1 drink/week, among current drinkers, adjusting for all variables in Model 2.
We assessed BMI as a potential effect modifier on the association between alcohol consumption and risk of diabetes. We first modeled baseline BMI as a continous variable and included the interaction terms in the regression model to test for effect modification using the likelihood ratio test. Second, we conducted analyses stratified by baseline BMI categories: normal-weight, 18.5≤ BMI <25 kg/m2; overweight, 25≤ BMI <30 kg/m2; or obese, BMI ≥30 kg/m2. Participants who were underweight (BMI<18.5 kg/m2) were excluded from this analysis, which constituted 0.9% of the study population (n=114).
Additionally, we assessed the association between the absolute changes in alcohol consumption (from visit 1 to visit 4) with incident diabetes (after visit 4). We used Cox proportional hazard models with change in alcohol consumption modeled using a linear spline with a knot at no change (absolute difference of 0 drinks/week). This analysis was stratified by sex and baseline alcohol consumption frequency: <7 drinks/week or ≥7 drinks/week.
We conducted two sensitivity analyses. First, to address reverse causation (current drinkers in poorer health may be likely to stop drinking prior to the baseline examination), we conducted our analyses after excluding the 1,468 participants with cardiovascular disease or cancer at baseline. Second, we examined the association of alcohol consumption with incident cases of diabetes defined based on self-reported diagnoses of diabetes or diabetes medication use only (ignoring cases of diabetes identified only based on glucose measurements).
Two-sided p-values <0.05 were considered statistically significant. All the analyses were performed using Stata version 14.0 (StataCorp).
RESULTS
Among the 12,042 participants (6,631 women, 5,411 men) included in the present study, 3,795 participants developed diabetes (2,059 women, 1,736 men) during a median follow-up of 21 years (maximum follow-up of 27 years). In the study population at baseline, compared to participants who consumed ≤1 drink/week, participants who consumed more alcohol were more likely to be men rather than women, had higher daily energy intake, higher HDL, higher glucose, and were current smokers (Table 1). Some baseline characteristics were associated with alcohol consumption in a U-shaped pattern. Participants who consumed a higher amount of alcohol were more likely to have attained a higher level of education, and higher family income. The heaviest drinking groups were more similar to never-drinkers or the lightest drinking groups with respect to education level and family income. Patterns of association with baseline covariates were generally similar in men and women (eTables 1 and 2).
Table 1.
Baseline characteristics a of participants without diabetes by alcohol consumption groups, the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1989
| Never drinkers (n=2802) | Former drinkers (n=2116) | ≤1 drink/week (n=2899) | 2–7 drinks/week (n=2508) | 8–14 drinks/week (n=986) | >14 drinks/week (n=731) | ||
|---|---|---|---|---|---|---|---|
| Alcoholic drinks per week, P25-P75 | - | - | 0–0 | 2–6 | 9–12 | 17–28 | |
| Age in years, mean (SD) | 54.4 (5.7) | 54.5 (5.7) | 53.6 (5.8) | 53.6 (5.7) | 53.8 (5.7) | 54.0 (5.7) | |
| Women (%) | 76.0 | 46.8 | 64.6 | 47.7 | 33.4 | 15.5 | |
| Race/center (%) | Whites, Forsyth Co. | 27.6 | 21.0 | 26.7 | 20.7 | 22.1 | 22.3 |
| Whites, Minneapolis | 4.7 | 18.7 | 37.8 | 42.1 | 40.6 | 34.3 | |
| Whites, Washington Co. | 26.7 | 32.2 | 26.8 | 21.6 | 24.7 | 25.7 | |
| Blacks, Forsyth Co. | 2.5 | 4.7 | 2.5 | 2.2 | 1.5 | 3.3 | |
| Blacks, Jackson | 38.5 | 23.3 | 6.1 | 13.4 | 11.1 | 14.4 | |
| Black (%) | 41.0 | 27.9 | 8.6 | 15.6 | 12.6 | 17.6 | |
| Total energy intake in kcal/day, mean (SD) | 1573.1 (682.5) | 1691.7 (769.2) | 1586.6 (642.1) | 1627.6 (654.5) | 1691.8 (633.0) | 1929.1 (772.8) | |
| Blood glucose level in mg/dL, mean (SD) | 97.7 (9.4) | 98.9 (9.4) | 97.7 (8.7) | 99.0 (8.9) | 100.3 (9.2) | 101.4 (10.3) | |
| HDL in mg/dl, mean (SD) | 53.6 (16.4) | 48.0 (14.9) | 51.5 (16.2) | 53.8 (18.2) | 56.0 (20.4) | 54.4 (18.3) | |
| Total cholesterol in mmol/l, mean (SD) | 5.6 (1.1) | 5.5 (1.1) | 5.5 (1.1) | 5.5 (1.0) | 5.6 (1.0) | 5.6 (1.1) | |
| Parental history of diabetes (%) | 25.4 | 23.3 | 21.3 | 21.1 | 20.3 | 20.8 | |
| Hypertension (%) | 37.4 | 34.3 | 24.9 | 26.2 | 28.9 | 35.4 | |
| Coronary heart disease (%) | 2.2 | 6.9 | 3.4 | 3.6 | 5.0 | 5.1 | |
| Body mass index in kg/(m2), mean (SD) | 28.2 (5.7) | 27.8 (5.6) | 26.9 (4.8) | 26.5 (4.3) | 26.2 (4.2) | 26.7 (4.4) | |
| Sport index, mean (SD) | 2.3 (0.7) | 2.4 (0.8) | 2.5 (0.8) | 2.6 (0.8) | 2.7 (0.8) | 2.5 (0.8) | |
| Smoking status (%) | Never | 69.9 | 28.9 | 44.8 | 32.2 | 22.0 | 12.2 |
| Former | 15.5 | 41.6 | 31.4 | 39.8 | 43.5 | 41.7 | |
| Current | 14.6 | 29.5 | 23.9 | 28.0 | 34.5 | 46.1 | |
| Waist-to-hip ratio, mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 1.0 (0.1) | |
| Family income (%) | Under $25,000 | 50.3 | 47.7 | 25.1 | 22.7 | 21.5 | 29.4 |
| $25,000-$49,999 | 36.0 | 36.1 | 42.7 | 40.2 | 36.3 | 39.0 | |
| Over $50,000 | 13.7 | 16.3 | 32.3 | 37.0 | 42.2 | 31.6 | |
| Education level (%) | Less than high school | 28.8 | 34.3 | 13.0 | 12.6 | 15.1 | 17.6 |
| High school degree or vocational school | 42.3 | 39.0 | 45.6 | 41.5 | 37.5 | 40.6 | |
| At least some college or professional school | 28.9 | 26.7 | 41.4 | 45.9 | 47.4 | 41.7 | |
Estimates are percent or mean (SD).
eTable 1.
Baseline characteristics a of women participants without diabetes by alcohol consumption groups, the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1989
| Never drinkers (n=2130) | Former drinkers (n=991) | ≤1 drink/week (n=1872) | 2–7 drinks/week (n=1196) | 8–14 drinks/week (n=329) | >14 drinks/week (n=113) | ||
|---|---|---|---|---|---|---|---|
| Alcoholic drinks per week, P25-P75 | - | - | 0–0 | 2–5 | 9–12 | 16–24 | |
| Age at visit 1, mean (SD) | 54.2 (5.8) | 53.9 (5.6) | 53.1 (5.7) | 53.2 (5.5) | 53.0 (5.7) | 53.3 (5.7) | |
| Race/center (%) | Whites, Forsyth Co. | 27.0 | 16.8 | 25.0 | 21.6 | 23.1 | 22.1 |
| Whites, Minneapolis | 3.9 | 17.4 | 40.3 | 45.2 | 42.2 | 36.3 | |
| Whites, Washington Co. | 25.7 | 33.6 | 25.9 | 19.5 | 24.3 | 28.3 | |
| Blacks, Forsyth Co. | 2.8 | 6.1 | 2.4 | 2.2 | 1.8 | 3.5 | |
| Blacks, Jackson | 40.6 | 26.2 | 6.4 | 11.6 | 8.5 | 9.7 | |
| Black (%) | 43.4 | 32.3 | 8.8 | 13.8 | 10.3 | 13.3 | |
| Total calorie intake in kcal/day, mean (SD) | 1516.5 (655.4) | 1583.1 (735.4) | 1495.5 (580.5) | 1482.4 (544.4) | 1534.9 (553.7) | 1617.6 (555.1) | |
| Blood glucose level in mg/dL, mean (SD) | 97.0 (9.4) | 97.4 (9.3) | 96.5 (8.6) | 97.3 (8.9) | 98.0 (9.6) | 97.9 (9.1) | |
| HDL in mg/dl, mean (SD) | 56.9 (16.2) | 55.3 (15.2) | 57.2 (15.7) | 63.4 (18.3) | 69.3 (21.2) | 68.0 (19.7) | |
| Total cholesterol in mmol/l, mean (SD) | 5.6 (1.1) | 5.6 (1.1) | 5.6 (1.1) | 5.6 (1.0) | 5.7 (1.1) | 5.8 (1.3) | |
| Parental history of diabetes (%) | 26.6 | 26.3 | 21.5 | 21.2 | 19.1 | 19.5 | |
| Hypertension (%) | 38.3 | 36.8 | 23.9 | 23.7 | 26.7 | 32.7 | |
| Coronary heart disease (%) | 1.6 | 3.0 | 1.3 | 0.9 | 1.2 | 1.8 | |
| Body mass index in kg/(m2), mean (SD) | 28.5 (6.1) | 28.3 (6.6) | 26.6 (5.3) | 25.8 (4.8) | 24.8 (4.3) | 25.4 (5.0) | |
| Sport index, mean (SD) | 2.2 (0.7) | 2.3 (0.8) | 2.4 (0.8) | 2.5 (0.8) | 2.5 (0.8) | 2.3 (0.8) | |
| Smoking status (%) | Never | 73.5 | 39.7 | 50.5 | 37.5 | 24.0 | 16.8 |
| Former | 11.5 | 30.1 | 24.8 | 31.3 | 29.8 | 27.4 | |
| Current | 14.9 | 30.3 | 24.6 | 31.3 | 46.2 | 55.8 | |
| Waist-to-hip ratio, mean (SD) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | 0.9 (0.1) | |
| Family income (%) | Under $25,000 | 54.6 | 56.0 | 27.6 | 26.4 | 24.0 | 35.4 |
| $25,000-$49,999 | 33.6 | 31.5 | 43.5 | 37.2 | 32.8 | 35.4 | |
| Over $50,000 | 11.8 | 12.5 | 28.9 | 36.4 | 43.2 | 29.2 | |
| Education level (%) | Less than high school | 28.7 | 33.7 | 11.8 | 10.4 | 11.2 | 15.0 |
| High school degree or vocational school | 44.4 | 41.7 | 50.4 | 46.7 | 43.8 | 46.0 | |
| At least some college or professional school | 26.9 | 24.6 | 37.8 | 43.0 | 45.0 | 38.9 | |
Estimates are percent or mean (SD).
eTable 2.
Baseline characteristics a of men participants without diabetes by alcohol consumption groups, the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1989
| Never drinkers (n=672) | Former drinkers (n=1125) | ≤1 drink/week (n=1027) | 2–7 drinks/week (n=1312) | 8–14 drinks/week (n=657) | >14 drinks/week (n=618) | ||
|---|---|---|---|---|---|---|---|
| Alcoholic drinks per week, P25-P75 | - | - | 0–1 | 3–6 | 9–12 | 18–28 | |
| Age at visit 1, mean (SD) | 55.0 (5.5) | 54.9 (5.7) | 54.3 (5.9) | 54.0 (5.8) | 54.2 (5.7) | 54.1 (5.7) | |
| Race/center (%) | Whites, Forsyth Co. | 29.6 | 25.0 | 29.9 | 20.0 | 21.6 | 22.3 |
| Whites, Minneapolis | 7.0 | 19.9 | 33.2 | 39.3 | 39.7 | 34.0 | |
| Whites, Washington Co. | 29.9 | 31.0 | 28.5 | 23.5 | 25.0 | 25.2 | |
| Blacks, Forsyth Co. | 1.5 | 3.5 | 2.7 | 2.2 | 1.4 | 3.2 | |
| Blacks, Jackson | 32.0 | 20.6 | 5.6 | 15.1 | 12.3 | 15.2 | |
| Black (%) | 33.5 | 24.1 | 8.4 | 17.3 | 13.7 | 18.4 | |
| Total calorie intake in kcal/day, mean (SD) | 1752.7 (734.2) | 1787.4 (785.7) | 1752.7 (712.2) | 1760.0 (715.7) | 1770.4 (655.6) | 1986.1 (793.5) | |
| Blood glucose level in mg/dL, mean (SD) | 99.5 (9.0) | 100.2 (9.3) | 99.8 (8.6) | 100.6 (8.7) | 101.5 (8.7) | 102.1 (10.4) | |
| HDL in mg/dl, mean (SD) | 43.4 (12.6) | 41.6 (11.3) | 41.0 (10.7) | 45.1 (12.9) | 49.3 (16.3) | 51.9 (16.9) | |
| Total cholesterol in mmol/l, mean (SD) | 5.4 (1.0) | 5.4 (1.0) | 5.4 (1.0) | 5.5 (1.0) | 5.5 (1.0) | 5.5 (1.0) | |
| Parental history of diabetes (%) | 21.6 | 20.5 | 20.9 | 21.0 | 20.9 | 21.0 | |
| Hypertension (%) | 34.7 | 32.0 | 26.6 | 28.5 | 30.0 | 35.9 | |
| Coronary heart disease (%) | 4.2 | 10.4 | 7.3 | 6.0 | 6.8 | 5.7 | |
| Body mass index in kg/(m2), mean (SD) | 27.3 (4.0) | 27.4 (4.5) | 27.4 (3.8) | 27.1 (3.7) | 27.0 (3.9) | 26.9 (4.3) | |
| Sport index, mean (SD) | 2.5 (0.8) | 2.5 (0.8) | 2.7 (0.8) | 2.7 (0.8) | 2.7 (0.8) | 2.5 (0.8) | |
| Smoking status (%) | Never | 58.3 | 19.4 | 34.3 | 27.4 | 21 | 11.3 |
| Former | 28 | 51.7 | 43.2 | 47.6 | 50.4 | 44.3 | |
| Current | 13.7 | 28.9 | 22.5 | 24.9 | 28.6 | 44.3 | |
| Waist-to-hip ratio, mean (SD) | 1.0 (0.1) | 1.0 (0.1) | 1.0 (0.1) | 1.0 (0.1) | 1.0 (0.1) | 1.0 (0.1) | |
| Family income (%) | Under $25,000 | 36.6 | 40.4 | 20.4 | 19.4 | 20.2 | 28.3 |
| $25,000-$49,999 | 43.9 | 40.1 | 41.2 | 43.0 | 38.1 | 39.6 | |
| Over $50,000 | 19.5 | 19.6 | 38.4 | 37.7 | 41.7 | 32 | |
| Education level (%) | Less than high school | 28.9 | 34.8 | 15.2 | 14.6 | 17.0 | 18.1 |
| High school degree or vocational school | 35.6 | 36.7 | 36.9 | 36.8 | 34.4 | 39.6 | |
| At least some college or professional school | 35.6 | 28.5 | 47.9 | 48.6 | 48.6 | 42.2 |
Estimates are percent or mean (SD).
Among women, in Model 2, drinking 8–14 drinks/week was associated with a lower risk of diabetes as compared to the reference group (≤1 drink/week) (HR 0.75, 95%CI, 0.58–0.96) (Table 2). Among men, there were no significant associations of alcohol consumption categories with diabetes risk in the minimally adjusted model (age, race and total energy intake). However, in Model 2, consuming 8–14 drinks/week was associated with a borderline significant lower risk of diabetes (HR 0.84, 95%CI 0.70–1.00) and consuming >14 drinks/week was associated with a significantly lower risk of diabetes (HR 0.81, 95%CI 0.67–0.97). In Model 2, the p value for interaction was <0.01 between sex and drinking status. In both sexes, among current drinkers, there was a significant decreasing trend in diabetes risk as the alcohol consumption increased in Model 2 (Table 2). Furthermore, collapsing the alcohol consumption categories among drinkers, compared to current drinkers consuming ≤1 drink/week, current drinkers consuming >1 drink/week had decreased risk (HR 0.86, 95%CI 0.75–0.99 for women; and HR 0.87, 95%CI 0.76–1.00 for men).
Table 2.
Hazard ratios (95% CIs) of incident diabetes according to baseline alcohol consumption groups and sex
| Women | Men | |||
|---|---|---|---|---|
| Model 1 a | Model 2 b | Model 1 a | Model 2 b | |
| Former-drinker | 1.10 (0.96–1.26) | 0.96 (0.84–1.11) | 1.07 (0.92–1.24) | 0.95 (0.82–1.11) |
| Never-drinker | 1.03 (0.91–1.16) | 0.98 (0.86–1.11) | 0.93 (0.78–1.11) | 0.96 (0.81–1.15) |
| ≤1 drink/week | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| 2–7 drinks/week | 0.82 (0.71–0.95) c | 0.88 (0.77–1.02) | 0.94 (0.81–1.08) | 0.93 (0.81–1.08) |
| 8–14 drinks/week | 0.71 (0.56–0.91) c | 0.75 (0.58–0.96) c | 0.89 (0.75–1.07) | 0.84 (0.70–1.00) c |
| >14 drinks/week | 0.86 (0.58–1.27) | 0.91 (0.61–1.34) | 0.92 (0.77–1.11) | 0.81 (0.67–0.97) c |
| p-trend for current drinkers | 0.001 | 0.032 | 0.261 | 0.007 |
Model 1: adjusted for age, race-center, and total energy intake
Model 2: adjusted for all variables in Model 1 plus parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
p<0.05
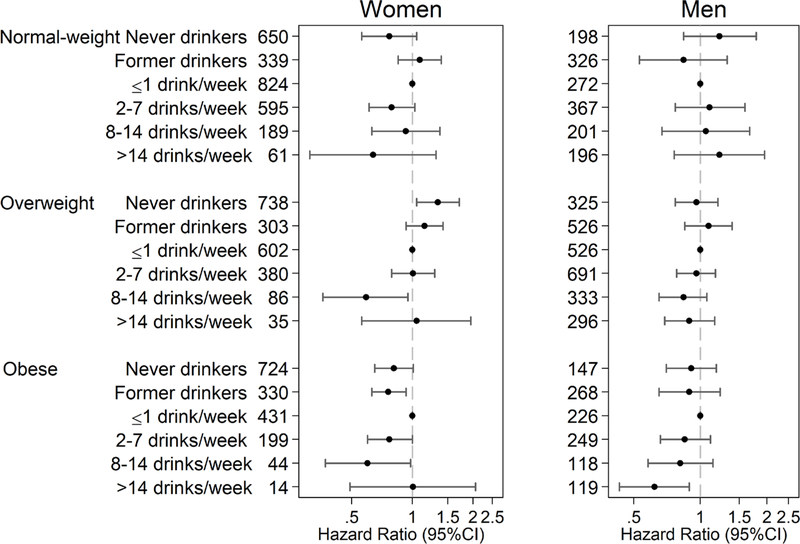
For both men and women, we found evidence for effect modification of the association of alcohol consumption and diabetes risk according to BMI (p-for-interaction=0.042 for women, p-for-interaction<0.001 for men). In women, drinking 8–14 drinks/week was associated with a decreased risk of diabetes among overweight participants (HR 0.59, 95%CI 0.36–0.95). Among women with obesity, drinking 2–14 drinks/week was also associated with lower risk for diabetes (HR 0.77, 95%CI 0.60–1.00 for 2–8 drinks/week; and HR 0.60, 95%CI 0.37–0.98 for 8–14 drinks/week). In men, an inverse association was found only among obese participants who drink >14 drinks/week (Figure 1) (HR 0.62, 95%CI 0.43–0.89).
Fig 1. Adjusted hazard ratios of incident diabetes by alcohol consumption groups and body mass index categories a and numbers of participants in each category.
a Adjust for age, race-center, total energy intake, parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
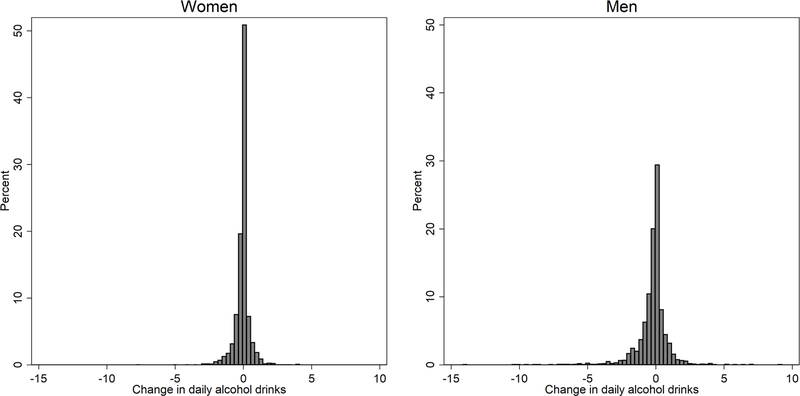
Over the 9-year period from visit 1 to visit 4 (Figure 2), changes in alcohol consumption status were observed. For women, 12.4% participants changed from current to former drinkers, and 2.9% participants changed from never to current drinkers. For men, 12.6% participants changed from current to former drinkers, and 1.1% participants changed from never to current drinkers. Drinking volume did not change substantially; the mean change in daily alcohol intake was −0.16 drinks (−0.07 drinks in women and −0.24 drinks in men). There were 1,978 incident diabetes cases (1104 in women and 874 in men) which occurred during the median of 14 years of follow-up after visit 4. For men with alcohol intake greater than 7 drinks/week at baseline, decrease in alcohol intake was associated with higher risk of diabetes (HR for per daily drink-decrease 1.12, 95%CI, 1.02–1.23) (Table 3). When we examined the risk of diabetes by changes in alcohol consumption status, compared to those who reported never drinking at both visits, no significant hazard ratios of incident diabetes were found (eTable 3).
Fig 2.
Histograms of changes in daily drinks from visit 1 to visit 4 among women and men
Table 3.
Hazard ratios of incident diabetes with 1-drink daily increase or decrease of alcohol intake from visit 1 to visit 4 a
| Women | Men | |||||
|---|---|---|---|---|---|---|
| Overall | Baseline <7 drinks/week | Baseline ≥7 drinks/week | Overall | Baseline <7 drinks/week | Baseline ≥7 drinks/week | |
| Decrease | 0.95 (0.78–1.16) | 0.78 (0.46–1.30) | 1.04 (0.76–1.41) | 1.06 (0.97–1.16) | 0.92 (0.56–1.51) | 1.12 (1.02–1.23) b |
| Increase | 0.87 (0.61–1.22) | 1.04 (0.59–1.82) | 0.75 (0.18–3.10) | 1.09 (0.95–1.25) | 1.26 (0.77–2.08) | 1.08 (0.91–1.28) |
| No change | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
Adjust for age, race-center, total energy intake, parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
p<0.05
eTable 3.
Hazard ratios of incident diabetes since visit 4 by pattern of alcohol consumption over time from visit 1 to visit 4 a
| Number of participants | Women | Number of participants | Men | |
|---|---|---|---|---|
| Never – never | 1153 | 1 (reference) | 323 | 1 (reference) |
| Never – current | 143 | 0.94 (0.54–1.66) | 42 | 2.04 (0.88–4.70) |
| Never – former | 309 | 0.71 (0.48–1.05) | 161 | 1.20 (0.68–2.11) |
| Former – former | 475 | 0.79 (0.55–1.15) | 579 | 1.24 (0.81–1.92) |
| Former – current | 104 | 1.11 (0.65–1.90) | 151 | 1.16 (0.62–2.16) |
| Current – current | 2097 | 0.89 (0.64–1.22) | 2239 | 1.36 (0.87–2.13) |
| Current – former | 607 | 0.80 (0.61–1.04) | 502 | 1.11 (0.75–1.64) |
Adjust for age, race-center, total energy intake, parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
The association between baseline drinking categories and diabetes risk were similar but somewhat weaker after excluding participants with prevalent cancer or cardiovascular disease at baseline (eTable 4) or when the diabetes outcome was defined using self-reported diagnosis or medication use (eTable 5). The somewhat weaker associations may be due to the decreased sample size and/or misclassification.
eTable 4.
Hazard ratios incident diabetes in a comparison of alcohol consumption groups among participants without baseline cancer or cardiovascular diseases
| Women | Men | |||
|---|---|---|---|---|
| Model 1 a | Model 2 b | Model 1 a | Model 2 b | |
| Former-drinker | 1.08 (0.93–1.26) | 0.99 (0.85–1.16) | 1.01 (0.86–1.18) | 0.91 (0.77–1.07) |
| Never-drinker | 1.04 (0.91–1.18) | 0.97 (0.85–1.11) | 0.91 (0.76–1.10) | 0.94 (0.78–1.13) |
| ≤1 drink/week | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| 2–7 drinks/week | 0.83 (0.71–0.96) c | 0.89 (0.76–1.04) | 0.92 (0.79–1.07) | 0.91 (0.78–1.06) |
| 8–14 drinks/week | 0.77 (0.59–0.99) c | 0.81 (0.62–1.05) | 0.89 (0.74–1.07) | 0.82 (0.68–0.99) c |
| >14 drinks/week | 0.85 (0.56–1.30) | 0.90 (0.59–1.38) | 0.92 (0.76–1.12) | 0.80 (0.65–0.97) c |
| p-trend for current drinkers | 0.007 | 0.120 | 0.293 | 0.009 |
Model 1: adjusted for age, race-center, and total energy intake
Model 2: adjusted for all variables in Model 1 plus parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
p<0.05
eTable 5.
Hazard ratios of self-reported diabetes by alcohol consumption groups and sex
| Women | Men | |||
|---|---|---|---|---|
| Model 1 a | Model 2 b | Model 1 a | Model 2 b | |
| Former-drinker | 1.13 (0.99–1.30) | 0.89 (0.77–1.02) | 1.01 (0.87–1.17) | 0.90 (0.77–1.05) |
| Never-drinker | 1.06 (0.94–1.19) | 0.92 (0.82–1.05) | 0.91 (0.76–1.08) | 0.96 (0.81–1.15) |
| ≤1 drink/week | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| 2–7 drinks/week | 0.77 (0.67–0.89) c | 0.91 (0.79–1.05) | 0.94 (0.81–1.09) | 0.94 (0.81–1.08) |
| 8–14 drinks/week | 0.65 (0.51–0.85) c | 0.80 (0.62–1.03) | 0.87 (0.73–1.04) | 0.86 (0.72–1.03) |
| >14 drinks/week | 0.78 (0.53–1.15) | 0.85 (0.57–1.27) | 0.78 (0.65–0.94) c | 0.76 (0.63–0.92) c |
| p-trend for current drinkers | <0.001 | 0.095 | 0.006 | 0.003 |
Model 1: adjusted for age, race-center, and total energy intake
Model 2: adjusted for all variables in Model 1 plus parental history of diabetes, education, family income, HDL-cholesterol, total cholesterol, baseline fasting glucose, coronary heart disease, physical activity; and time-varying BMI, smoking status (never, former, current), waist-hip ratio, and hypertension
p<0.05
DISCUSSION
In this community-based population, we observed a lower risk of diabetes in women who drank 8–14 drinks/week and men who drank more than 8 drinks/week compared to their counterparts who drank less than 1 drink per week. There was evidence for effect modification of this association by BMI, with significant inverse associations only observed among participants who were overweight or obese. For most participants, the amount of alcohol consumed did not change substantially from visit 1 to visit 4. A decrease in alcohol consumption among men consuming higher alcohol at baseline was associated with higher diabetes risk.
Evidence for how alcohol consumption is related to diabetes risk may be helpful to inform the current evidence on the long-term cardiometabolic effects of alcohol. The 2015–2020 Dietary Guidelines for Americans recommend that, if alcohol is consumed, it should be moderate (≤1 drink/day for women; ≤ 2 drinks/day for men); the guidelines do not recommend starting drinking for any reason for people who do not drink [19]. Our results suggest that any protective effect of alcohol consumption on diabetes risk is modest, may differ in men compared to women, and may differ by obesity status.
The results of our study are similar but not fully consistent with prior studies. A much earlier study on alcohol consumption and diabetes risk in the ARIC Study found no association between moderate alcohol consumption with diabetes risk, while high consumption was associated with elevated diabetes risk, but only in men [12]. This prior study, however, had a relatively short follow-up period (maximum 6 years) and many fewer events compared to our analysis. The present study had a much longer follow-up period (maximum of 27 years) and more than three times as many incident diabetes cases, giving us greater power to detect moderate associations and to compare associations across participant subgroups. A systematic review of 20 cohort studies found U-shaped associations of alcohol with diabetes risk in both sexes, with a similar dose associated with the lowest risk at 24 g/day (around 1.71 drinks/day or 12 drinks/week, risk ratio 0.60, 95% CI, 0.52–0.69) in women and 22 g/day (around 1.57 drinks/day or 11 drinks/week, risk ratio 0.87, 95% CI, 0.76–1.00) in men, respectively [7]. Another systematic review of 38 cohort studies, on the other hand, showed no reduction in diabetes risk in men, and found an inverse association among women with a summary HR 0.66, at 31 – 37 g/day (2.2 – 2.6 drinks/day) [13]. We found the lowest risk of diabetes at 1.1–2 drinks per day in women and more than 1.1 drinks per day in men. The differences in the alcohol consumption amount associated with the lowest risk among the studies may be due to variability between study populations with respect to age, race, geography, duration of follow-up, and/or adjustment variables.
It is not entirely clear why BMI may be an effect modifier of the association between alcohol intake and incident diabetes. A possible explanation for this effect modification by adiposity is that obesity-induced insulin resistance is suppressed through moderate drinking [20]. Prior studies examining this question have had inconsistent findings. Our results showed decreased risk in obese women and obese men. More research is needed to further understand the mechanisms or interplay between adiposity, alcohol, and its health effects.
Prior studies have speculated on the cardiometabolic effects of moderate alcohol consumption [2–4] and have demonstrated a protective effect of alcohol consumption on cardiovascular risk and cardiometabolic risk factors. There is evidence that moderate alcohol intake can increase HDL-cholesterol [3], which has been postulated to partially explain the inverse association of moderate alcohol consumption with cardiovascular disease [21]. It is possible that any beneficial effects on lipids may also contribute to a decreased risk of diabetes. Some investigators have suggested that the lower risk of diabetes associated with moderate alcohol consumption may be explained by improvements in insulin sensitivity [22, 23]. In a meta-analysis of 14 intervention studies, moderate alcohol consumption was found to be associated with lower fasting insulin concentrations and lower HbA1c [4]. In this meta-analysis, the alcohol dosages ranged from 10 g/day to 75 g/day, and the intervention periods varied from 2 to 12 weeks [4]. Socioeconomic status is a potent risk factor for diabetes [24] and is a complex contributor to health status. Although we adjusted for major diabetes risk factors (including education, family income, CVD history, body mass index, and physical activity), it remains possible that the inverse associations of alcohol with cardiovascular outcomes and diabetes are the result of residual confounding [25, 26].
A unique aspect of our study is that we were able to investigate changes in alcohol consumption over a 9-year time window. Evidence for the association between changes in alcohol consumption and diabetes risk is limited. A prospective cohort study of men from the Health Professionals Follow-Up Study found that increases in alcohol consumption over time were associated with a lower risk of diabetes among initially light drinkers (0–4.9 g/day) [17]. Our results showed an increased diabetes risk among men with higher baseline consumption (≥7 drinks/week) who decreased their drinking. In most participants, alcohol consumption remained stable over the 9-year period: 76% of women participants and 79% of men participants were in the same alcohol consumption status (never, former, or current drinkers) at baseline and at the 9-year follow-up visit. Our understanding of what causes lifestyle modifications such as changes in alcohol consumption in the general, middle-aged population is limited. Additional work to understand why and how adults make lifestyle changes in midlife will help inform future studies in this area.
Potential limitations of our study include the possibility of recall and/or reporting bias regarding self-reported alcohol consumption that may have resulted in misclassification of the exposure. Despite our large sample size, after stratification by sex and alcohol consumption categories, we had limited power to detect moderate associations in population subgroups including those defined by BMI categories. High alcohol consumption was low in this population and thus, we had limited ability to examine associations in this group, especially among women (only 1.7% women were in the >14 drinks/week group). Due to the small numbers of individuals who changed drinking categories, the analysis of 9-year changes were likely underpowered.
The strengths of the study include the community-based population and the long period of follow-up. We were also able to assess the effect modification by BMI of this association between alcohol consumption and diabetes risk. The wide range of rigorously measured covariates collected at baseline and later on allowed for careful adjustment of potential confounders (including time-varying covariates) and the evaluation of different adjustment models.
In conclusion, in this large, community-based cohort of black and white adults, 8–14 drinks per week for women and more than 8 drinks per week for men were associated with decreased risk of diabetes, and the associations were stronger among people with increased BMI.
RESEARCH IN CONTEXT.
Already known
Moderate alcohol consumption has been associated with lower risk for diabetes
Whether the association differs by sex or adiposity status is controversial
Evidence on the association of changes in alcohol consumption and diabetes risk is limited
Key question
What is the prospective association between baseline and 9-year change in alcohol consumption with long-term risk of diabetes and whether these associations might be modified by sex and/or body mass index
New findings
In this large, community-based cohort of black and white adults, 8–14 drinks per week for women and more than 8 drinks per week for men were associated with a moderately decreased risk of diabetes; in both sexes, among current drinkers, there was a significant decreasing trend in diabetes risk as the alcohol consumption increased
The inverse associations were stronger among people with higher body mass index
The amount of alcohol consumed was stable during the 9-year period, and among men who consumed higher amounts of alcohol at baseline, decreasing daily intake was associated with higher diabetes risk
How might it impact clinical practice
The association of alcohol consumption with diabetes may differ by sex and body mass index, suggesting that the pathways by which alcohol impacts risk is potentially complex. In our study, alcohol was only associated with a lower risk of diabetes in adults who were overweight or obese and was not associated with diabetes risk in participants of normal weight.
ACKNOWLEDGEMENTS
The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, National Institutes of Health, Department of Health and Human Services, under Contract nos. (HHSN268201700001I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I, HHSN268201700002I). The authors thank the staff and participants of the ARIC study for their important contributions.
FUNDING
Dr. Selvin was supported by NIH/NIDDK grants K24DK106414 and R01DK089174.
Dr. Rebholz is supported by a Mentored Research Scientist Development Award from the National Institute of Diabetes and Digestive and Kidney Diseases (K01 DK107782).
Abbreviations:
- ARIC study
Atherosclerosis Risk in Communities (ARIC) Study
Footnotes
DUALITY OF INTEREST
There is no conflict of interest.
Contributor Information
Xintong He, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health, xhe27@jhu.edu.
Casey M. Rebholz, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health Welch Center for Prevention, Epidemiology, and Clinical Research, crebhol1@jhu.edu.
Natalie Daya, Welch Center for Prevention, Epidemiology, and Clinical Research, ndaya1@jhu.edu.
Mariana Lazo, Division of General Internal Medicine, Johns Hopkins School of Medicine; Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health; Welch Center for Prevention, Epidemiology, and Clinical Research, mlazo@jhu.edu.
Elizabeth Selvin, Department of Epidemiology, Johns Hopkins Bloomberg School of Public Health; Welch Center for Prevention, Epidemiology, and Clinical Research, eselvin@jhu.edu.
References
- [1].Selvin E, Parrinello CM, Sacks DB, Coresh J (2014) Trends in prevalence and control of diabetes in the United States, 1988–1994 and 1999–2010. Ann Intern Med 160: 517–525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Brien SE, Ronksley PE, Turner BJ, Mukamal KJ, Ghali WA (2011) Effect of alcohol consumption on biological markers associated with risk of coronary heart disease: systematic review and meta-analysis of interventional studies. BMJ 342: d636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Rimm EB, Williams P, Fosher K, Criqui M, Stampfer MJ (1999) Moderate alcohol intake and lower risk of coronary heart disease: meta-analysis of effects on lipids and haemostatic factors. BMJ 319: 1523–1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Schrieks IC, Heil AL, Hendriks HF, Mukamal KJ, Beulens JW (2015) The effect of alcohol consumption on insulin sensitivity and glycemic status: a systematic review and meta-analysis of intervention studies. Diabetes Care 38: 723–732 [DOI] [PubMed] [Google Scholar]
- [5].Naimi TS, Stockwell T, Zhao J, et al. (2017) Selection biases in observational studies affect associations between ‘moderate’alcohol consumption and mortality. Addiction 112: 207–214 [DOI] [PubMed] [Google Scholar]
- [6].Connor J, Hall W (2018) Thresholds for safer alcohol use might need lowering. The Lancet 391: 1460–1461 [DOI] [PubMed] [Google Scholar]
- [7].Baliunas DO, Taylor BJ, Irving H, et al. (2009) Alcohol as a risk factor for type 2 diabetes: a systematic review and meta-analysis. Diabetes care 32: 2123–2132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Beulens JW, van der Schouw YT, Bergmann MM, et al. (2012) Alcohol consumption and risk of type 2 diabetes in European men and women: influence of beverage type and body size The EPIC-InterAct study. J Intern Med 272: 358–370 [DOI] [PubMed] [Google Scholar]
- [9].Djoussé L, Biggs ML, Mukamal KJ, Siscovick DS (2007) Alcohol consumption and type 2 diabetes among older adults: the Cardiovascular Health Study. Obesity 15: 1758–1765 [DOI] [PubMed] [Google Scholar]
- [10].Hodge A, English D, O’Dea K, Giles G (2006) Alcohol intake, consumption pattern and beverage type, and the risk of type 2 diabetes. Diabetic Medicine 23: 690–697 [DOI] [PubMed] [Google Scholar]
- [11].Hozawa A, Okamura T, Tanaka T, et al. (2010) Relation of Gamma-glutamyltransferase and alcohol drinking with incident diabetes: the HIPOP-OHP study. J Atheroscler Thromb 17: 195–202 [DOI] [PubMed] [Google Scholar]
- [12].Kao WH, Puddey IB, Boland LL, Watson RL, Brancati FL (2001) Alcohol consumption and the risk of type 2 diabetes mellitus: atherosclerosis risk in communities study. Am J Epidemiol 154: 748–757 [DOI] [PubMed] [Google Scholar]
- [13].Knott C, Bell S, Britton A (2015) Alcohol Consumption and the Risk of Type 2 Diabetes: A Systematic Review and Dose-Response Meta-analysis of More Than 1.9 Million Individuals From 38 Observational Studies. Diabetes Care 38: 1804–1812 [DOI] [PubMed] [Google Scholar]
- [14].Koloverou E, Panagiotakos DB, Pitsavos C, et al. (2015) Effects of alcohol consumption and the metabolic syndrome on 10-year incidence of diabetes: the ATTICA study. Diabetes Metab 41: 152–159 [DOI] [PubMed] [Google Scholar]
- [15].Liu C, Yu Z, Li H, et al. (2010) Associations of alcohol consumption with diabetes mellitus and impaired fasting glycemia among middle-aged and elderly Chinese. BMC public health 10: 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Metcalf PA, Scragg RK, Jackson R (2014) Light to moderate alcohol consumption is protective for type 2 diabetes mellitus in normal weight and overweight individuals but not the obese. Journal of obesity [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Joosten MM, Chiuve SE, Mukamal KJ, Hu FB, Hendriks HF, Rimm EB (2011) Changes in alcohol consumption and subsequent risk of type 2 diabetes in men. Diabetes 60: 74–79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Baecke JA, Burema J, Frijters JE (1982) A short questionnaire for the measurement of habitual physical activity in epidemiological studies. Am J Clin Nutr 36: 936–942 [DOI] [PubMed] [Google Scholar]
- [19].Americans DGf (2015) Dietary Guidelines 2015–2020 Appendix 9. Alcohol. Available from https://health.gov/dietaryguidelines/2015/guidelines/message/, [Google Scholar]
- [20].Wakabayashi I (2014) Light-to-moderate alcohol drinking reduces the impact of obesity on the risk of diabetes mellitus. J Stud Alcohol Drugs 75: 1032–1038 [DOI] [PubMed] [Google Scholar]
- [21].van Tol A, Hendriks HF (2001) Moderate alcohol consumption: effects on lipids and cardiovascular disease risk. Curr Opin Lipidol 12: 19–23 [DOI] [PubMed] [Google Scholar]
- [22].Furuya DT, Binsack R, Machado UF (2003) Low ethanol consumption increases insulin sensitivity in Wistar rats. Braz J Med Biol Res 36: 125–130 [DOI] [PubMed] [Google Scholar]
- [23].Hendriks HF (2007) Moderate alcohol consumption and insulin sensitivity: observations and possible mechanisms. Annals of epidemiology 17: S40–S42 [Google Scholar]
- [24].Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A (2011) Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol 40: 804–818 [DOI] [PubMed] [Google Scholar]
- [25].Criqui MH, Thomas IC (2017) Alcohol Consumption and Cardiac Disease: Where Are We Now? J Am Coll Cardiol 69: 25–27 [DOI] [PubMed] [Google Scholar]
- [26].Stockwell T, Zhao J, Panwar S, Roemer A, Naimi T, Chikritzhs T (2016) Do “moderate” drinkers have reduced mortality risk? A systematic review and meta-analysis of alcohol consumption and all-cause mortality. Journal of studies on alcohol and drugs 77: 185–198 [DOI] [PMC free article] [PubMed] [Google Scholar]