Abstract
Background
Several epidemiological studies have investigated the association between dietary fat intake and cardiovascular disease. However, dietary recommendations based on systematic review and meta-analysis might be more credible.
Methods and results
Pubmed, Embase and Cochrane library were searched up to July 1st 2018 for cohort studies reporting associations of dietary fat intake and risk of CVDs. By comparing the highest vs. the lowest categories of fat or fatty acids intake, we found that higher dietary trans fatty acids (TFA) intake was associated with increased risk of CVDs [RR:1.14(1.08–1.21)]. However, no association was observed between total fat, monounsaturated fatty acids (MUFA), saturated fatty acids (SFA), and polyunsaturated fatty acids (PUFA), and risk of CVDs. Subgroup analysis found a cardio-protective effect of PUFA in the studies that has been followed up more than 10 years [0.95(0.91–0.99), I2 = 62.4%]. Dose-response analysis suggested that the risk of CVDs increased 16% [1.16 (1.07–1.25), Plinearity = 0.033] for an increment of 2% energy/day of TFA intake.
Conclusions
This current meta-analysis of cohort studies suggested that total fat, SFA, MUFA, and PUFA intake were not associated with the risk of cardiovascular disease. However, we found that higher TFA intake is associated with greater risk of CVDs in a dose-response fashion. Furthermore, the subgroup analysis found a cardio-protective effect of PUFA in studies followed up for more than 10 years.
Electronic supplementary material
The online version of this article (10.1186/s12944-019-1035-2) contains supplementary material, which is available to authorized users.
Keywords: Fat, Fatty acids, Cardiovascular disease, Meta-analysis, Dose-response
Backgrounds
CVDs, caused by disorders of the heart and blood vessels, are the leading cause of death globally [1]. It is estimated that 17.7 million people, which represented 31% of all global deaths, died from CVDs in 2015 [1]. Unhealthy lifestyles, especially dietary habits, are believed to play an important role in the development of heart disease [2–5]. National health institutions has traditionally recommended to reduce the intake of dietary fat to prevent CVDs [6]. In addition, the intake of trans-fat has been demonstrated to be associated with health outcomes, and it is recommended to reduce its consumption a minimum [7].
The mechanisms underlying the effects of dietary fat on CVD remain uncertain. Dietary fat might contribute to CVD via inflammatory and oxidative stress mechanisms. Polyunsaturated fatty acid (PUFA) can decrease the production of inflammatory and reactive oxygen species [8], saturated fatty acid (SFA) and trans fatty acids (TFA) can increase pro-inflammatory and oxidative stress [9, 10], excessive oxidative stress and inflammation contributes to the development of CVD [11, 12]. Several previous studies have investigated the relationship between dietary fat and cardiovascular risk [13–16], the PREvención con DIeta MEDiterránea study (PREDIMED) demonstrated that Mediterranean diets (MedDiets), which were high in polyunsaturated fatty acid (PUFA) and monounsaturated fatty acid (MUFA), low in saturated fatty acid (SFA) and trans fatty acids (TFA), were associated with reduced CVDs events compared with a low-fat control diet [13]. The Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC) Study showed that SFA intake was inversely associated with mortality from stroke [17]. However, the Lipid Research Clinics Prevalence Follow-up Study suggested that dietary MUFA and PUFA intake were associated with reduced risk of CVDs mortality and morbidity, whereas dietary intake of trans-fat and SFA were associated with increased risk of CVDs [14]. The Prospective Urban Rural Epidemiological (PURE) study found that total fat and types of fat were not associated with cardiovascular disease, or mortality, whereas saturated fat had an inverse association with stroke. Global dietary guidelines should be reconsidered in light of these findings [18]. However, in the development of guideline, recommendations should be informed by systematic review and meta-analysis of all evidences and/or large randomized clinical trials. [19].
Thus, it is warranted to conduct a meta-analysis to investigate the effect of dietary fat intake on CVDs risk. In the current study, we summarized the evidence from cohort studies of the relation of dietary fat intake and CVDs risk, and evaluated the dose-response relationship of CVDs and dietary fat intake.
Methods
Search strategy
Two members of the research team (Yonjian Zhu and Yanhua Liu) systematically searched Pubmed, Embase and Cochrane library up to July 1st 2018. The following keywords were adopted: (dietary fat OR fat OR fatty OR monounsaturated fatty acid OR polyunsaturated fatty acid OR saturated fatty acid OR trans fatty acid) AND (Cardiovascular disease OR vascular disease OR ischemic heart disease OR coronary heart disease OR Miocardial infarction OR Arrhythmia OR atrial fibrillation OR stroke OR cerebral infarction OR cerebral hemorrhage OR Heart failure OR Hypertension OR Cardiomyopathy).
Study selection
Two investigators (Yongjian Zhu and Yanhua Liu) independently reviewed all identified studies, and studies were included if they met the following criteria: (i) based on a cohort or nested case-control study design; (ii) the exposure of interest were dietary total fat or major fat subclasses (SFA, TFA, MUFA, or PUFA) intake; (iii) the outcomes of interest were CVDs and (iv) relative risk (RR) or hazard ratio (HR) with 95% confidence interval (CI) were reported (we present pooled results with HR). If data were duplicated in more than one study, the one with the most recent or with the most number of cases was included. Conflicts were resolved via a third author (Yacong Bo).
Data extraction
Two authors (Yanhua Liu and Yacong Bo) independently extracted the following information: the surname of first author, year of publication, cohort name, country, method of assessing dietary fat intake, number of participation, association between dietary fat intake and outcome (HR or RR and 95% CI); the definition of outcome; and potential confounding variables adjusted for HR (RR) with 95% CI across increasing fat intake categories were extracted preferentially or, where these data were not available, risk estimates for continuous (linear) exposures were extracted. Conflicts were resolved via a third author (Yongjian Zhu).
Statistical methods
For the highest vs. the lowest dietary fat intake and CVDs risk, we used the DerSimonian and Laird random effects model to pool RRs and its 95% CIs from the adjusted HRs or RRs. Subgroup and meta-regression analysis were also performed based on geographical location (Americas, Europe, or other); follow-up duration (< 10 years or ≥ 10 years); and whether the results were adjusted for age, sex, physical activity, energy intake, alcohol, smoking, or body mass index.
Potential publication bias was assessed by Egger’s test (P < 0.05) [20, 21]. The sensitivity analysis was performed by excluding 1 study at a time to evaluate whether the results could have been affected markedly by a single study.
For the dose-response association of dietary fat intake and incident cardiovascular disease, the method of restricted cubic splines with three knots at percentiles 25, 50, and 75% of the distribution was adopted [22]. The studies included in doses-response analysis should report the number of cases and person-years (or controls), and the RR (or HR) with the variance estimates for at least three quantitative exposure categories. If the distribution of cases or person years was not reported, we estimated them based on the quintiles definitions [23]. Moreover, we assigned the median or mean fat intake for each category to each corresponding RRs (or HRs) with 95% CI. When means and medians were not reported, the category midpoint would be used. When the lowest category was open-ended, we set zero to the lowest boundary, and when the highest category was open-ended, we set the same width of the adjacent category to it [23].
All analyses were conducted using STATA software (version 12.0; StatCorp, College Station, TX, USA) and a value of P < 0.05 was considered as statistically significant.
Patient and public involvement statement
Patients and the public sector were not directly involved in this study.
Results
Literature search and study characteristics
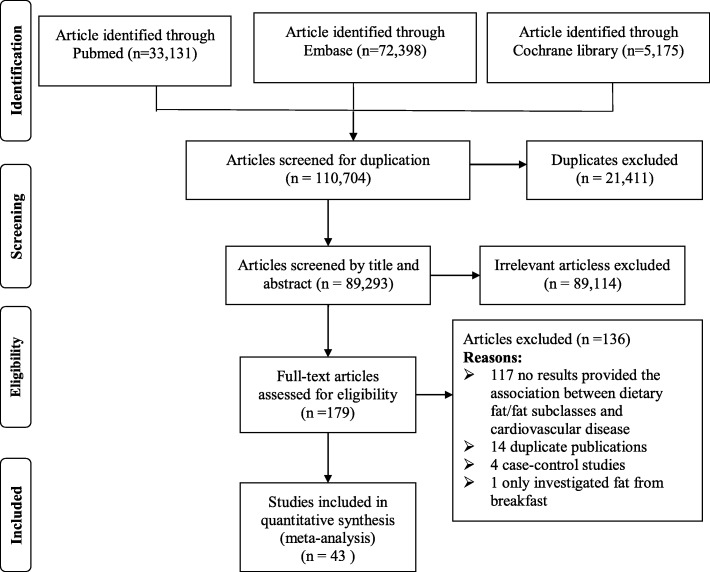
The detailed procedures of the article search and screening were presented in Fig. 1. Briefly, the search strategy retrieved 110,704 papers: 33,131 from Pubmed, 72,398 from Embase and 5175 from Cochrane library. After removing 21,411 duplicate articles, 89,293 articles were assessed. Among them, 89,114 articles were excluded after reviewing abstracts and titles, leaving 179 articles for full-text review. Of these, 136 papers were excluded due to: no results provided the association between dietary fat/fat subclasses and cardiovascular disease, duplicate publications, case-control studies, and only investigated fat from breakfast. In total, 43 publications [14, 15, 17, 18, 24–62] (63 studies, since 19 studies reported results for more than one study) that presented risk estimates for dietary total fat or major fat subclasses intake and CVDs risk were identified. The main characters of these studies are presented in Additional file 1: Table S1.
Fig. 1.
Search, screening and selection process of prospective cohort studies of dietary total fat and major fat subclasses and risk of cardiovascular disease
Total fat intake and risk of CVDs
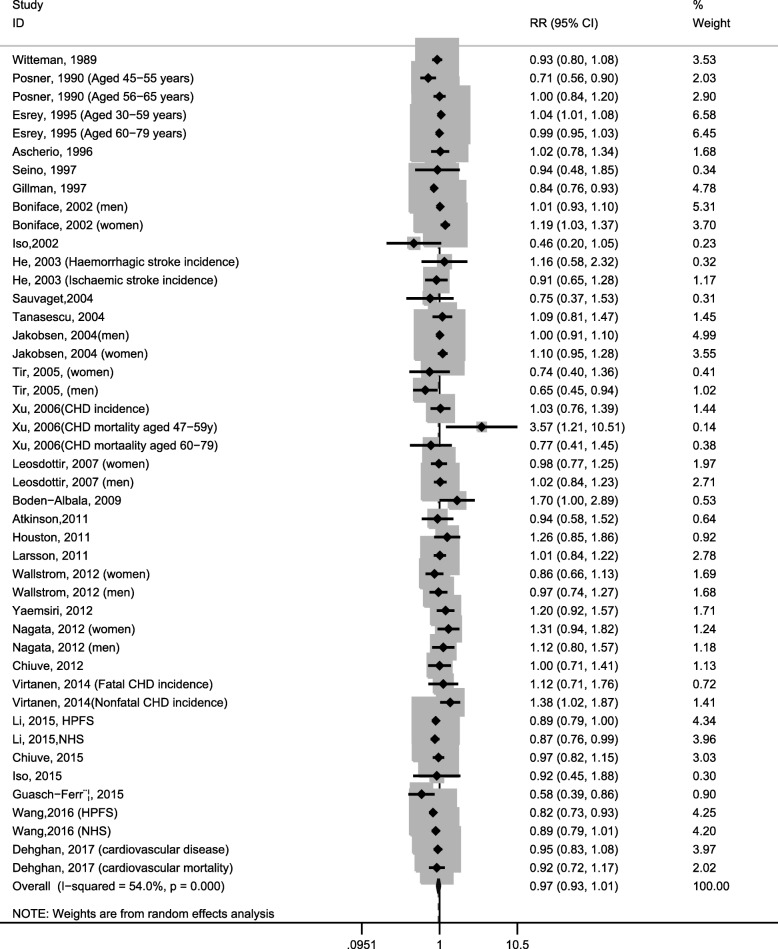
Forty-five studies reported the relationship between total dietary fat intake and CVDs risk (CVDs incidence and mortality). Highest versus lowest levels of total dietary fat were not associated with the CVDs risk [0.97(0.93–1.01), I2 = 54.0%; Fig. 2]. Sensitivity analysis showed that no individual study had an excessive influence on the pooled effect. There was evidence of significant heterogeneity (I2 = 54.0%), which was further explored in meta-regression. All covariates investigated in the meta-regression provided a poor explanation of the heterogeneity. In addition, the analysis was repeated stratified according to each covariate. The results were consistent with that observed in meta-regression.
Fig. 2.
Forest plots of cardiovascular disease for the highest versus lowest categories of dietary total fat intake
Subgroup analysis
As shown in Table 1, non-significant associations of total dietary fat intake with cardiovascular risk were detected in the subgroup analysis conducted by geographical location (Americas, Europe, or Asia); follow-up duration (< 10 years or ≥ 10 years); And whether the results were adjusted for age, sex, physical activity, energy intake, alcohol, smoking, or body mass index.
Table 1.
Subgroup analysis of dietary total fat and major fat subclasses and risk of cardiovascular disease
| Dietary total fat | Trans fat | Saturated fatty acid | Monounsaturated fatty acid | Polyunsaturated fatty acid | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | HR(95%CI) | I2 (%) | N | HR(95%CI) | I2 (%) | N | HR(95%CI) | I2 (%) | N | HR(95%CI) | I2 (%) | N | HR(95%CI) | I2 (%) | |
| Overall | 45 | 0.97 (0.93–1.01) | 54.0 | 24 | 1.14 (1.08–1.21) | 26.1 | 56 | 0.97 (0.93–1.02) | 56.8 | 43 | 0.97 (0.93–1.01) | 50.3 | 45 | 0.97 (0.93–1.00) | 55.8 |
| Follow-up duration (years) | |||||||||||||||
| < 10 | 15 | 0.97 (0.88–1.08) | 49.0 | 10 | 1.20 (1.10–1.30) | 0.0 | 19 | 0.97 (0.89–1.05) | 48.8 | 12 | 0.94 (0.81–1.08) | 51.3 | 15 | 1.03 (0.94–1.13) | 34.0 |
| ≥ 10 | 30 | 0.97 (0.93–1.01) | 57.0 | 14 | 1.11 (1.02–1.19) | 38.2 | 37 | 0.98 (0.93–1.03) | 60.9 | 31 | 0.98 (0.94–1.02) | 50.5 | 30 | 0.95 (0.91–0.99) | 62.4 |
| Geographical location | |||||||||||||||
| America | 23 | 0.95 (0.90–1.01) | 63.2 | 17 | 1.13 (1.06–1.21) | 24.2 | 24 | 1.01 (0.95–1.07) | 58.8 | 20 | 0.94 (0.88–1.02) | 59.7 | 20 | 0.93 (0.86–1.01) | 60.5 |
| Europe | 14 | 1.00 (0.93–1.08) | 50.2 | 7 | 1.16 (1.04–1.31) | 40.0 | 21 | 0.98 (0.91–1.06) | 49.5 | 16 | 1.01 (0.95–1.06) | 42.8 | 18 | 1.01 (0.98–1.05) | 27.6 |
| Asia | 6 | 1.01 (0.80–1.28) | 27.6 | 0 | – | – | 9 | 0.84 (0.73–0.97) | 42.3 | 5 | 0.90 (0.64–1.27) | 33.3 | 5 | 1.09 (0.86–1.39) | 0.0 |
| Adjust for age | |||||||||||||||
| Yes | 32 | 0.99 (0.95–1.03) | 48.4 | 16 | 1.13 (1.03–1.23) | 35.1 | 43 | 0.97 (0.92–1.02) | 57.9 | 30 | 0.99 (0.95–1.03) | 42.7 | 33 | 0.99 (0.95–1.02) | 48.9 |
| No | 13 | 0.93 (0.86–1.01) | 53.0 | 8 | 1.16 (1.06–1.28) | 9.5 | 13 | 0.99 (0.89–1.09) | 53.5 | 13 | 0.95 (0.85–1.06) | 51.2 | 12 | 0.91 (0.81–1.03) | 43.3 |
| Adjust for sex | |||||||||||||||
| Yes | 8 | 1.01 (0.93–1.09) | 61.8 | 6 | 1.07 (0.96–1.69) | 0.2 | 21 | 0.94 (0.87–1.02) | 72.6 | 13 | 0.96 (0.92–1.01) | 63.2 | 14 | 1.00 (0.94–1.05) | 9.1 |
| No | 22 | 1.00 (0.96–1.04) | 43.2 | 18 | 1.15 (1.08–1.23) | 30.4 | 35 | 1.00 (0.94–1.05) | 37.4 | 30 | 0.95 (0.86–1.06) | 42.7 | 31 | 0.96 (0.91–1.01) | 64.8 |
| Adjust for alcohol | |||||||||||||||
| Yes | 12 | 0.99 (0.92–1.07) | 59.5 | 20 | 1.13 (1.06–1.19) | 24.5 | 41 | 0.97 (0.92–1.02) | 51.7 | 29 | 0.98 (0.93–1.02) | 47.5 | 30 | 0.96 (0.92–1.01) | 64.8 |
| No | 33 | 0.97 (0.92–1.01) | 46.6 | 4 | 1.30 (1.06–1.61) | 23.2 | 15 | 0.99 (0.90–1.08) | 60.7 | 14 | 0.93 (0.85–1.02) | 58.2 | 15 | 0.99 (0.93–1.01) | 18.4 |
| Adjust for energy intake | |||||||||||||||
| Yes | 32 | 0.96 (0.92–1.01) | 62.0 | 18 | 1.16 (1.08–1.25) | 26.3 | 40 | 0.96 (0.91–1.02) | 64.5 | 30 | 0.96 (0.90–1.02) | 57.2 | 31 | 0.95 (0.89–1.01) | 54.0 |
| No | 13 | 1.00 (0.94–1.06) | 12.4 | 6 | 1.09 (1.00–1.19) | 11.1 | 16 | 1.01 (0.95–1.08) | 6.0 | 13 | 1.00 (0.97–1.03) | 12.9 | 14 | 1.01 (0.98–1.04) | 27.2 |
| Adjust for physical activity | |||||||||||||||
| Yes | 33 | 1.00 (0.93–1.08) | 56.1 | 19 | 1.14 (1.06–1.22) | 38.3 | 43 | 0.96 (0.92–1.01) | 49.8 | 31 | 0.94 (0.88–1.00) | 42.2 | 32 | 0.97 (0.91–1.03) | 59.5 |
| No | 12 | 1.02 (0.99–1.04) | 22.2 | 5 | 1.15 (1.02–1.30) | 0.0 | 13 | 1.01 (0.91–1.12) | 60.6 | 12 | 1.02 (0.98–1.06) | 41.5 | 13 | 1.01 (0.99–1.02) | 0.0 |
| Adjust for smoking | |||||||||||||||
| Yes | 41 | 0.97 (0.92–1.01) | 57.0 | 22 | 1.15 (1.08–1.23) | 28.0 | 52 | 0.97 (0.92–1.01) | 58.3 | 40 | 0.97 (0.93–1.01) | 51.8 | 42 | 0.97 (0.93–1.01) | 58.0 |
| No | 4 | 1.01 (0.94–1.08) | 0.0 | 2 | 1.08 (0.98–1.20) | 0.0 | 4 | 1.05 (0.95–1.16) | 1.0 | 3 | 1.08 (0.80–1.46) | 33.1 | 3 | 0.88 (0.67–1.15) | 0.0 |
| Adjust for body mass index | |||||||||||||||
| Yes | 35 | 0.96 (0.91–1.01) | 56.4 | 23 | 1.14 (1.07–1.21) | 29.4 | 43 | 0.97 (0.91–1.02) | 58.1 | 36 | 0.98 (0.94–1.02) | 50.3 | 37 | 0.96 (0.93–1.01) | 59.1 |
| No | 10 | 0.99 (0.93–1.06) | 48.1 | 1 | 1.14 (0.97–1.35) | – | 13 | 0.99 (0.92–1.07) | 55.6 | 7 | 0.93 (0.80–1.07) | 51.0 | 8 | 1.01 (0.87–1.17) | 39.8 |
Abbreviation: HR hazards ratio
Publication bias
Egger test showed no evidence of significant publication bias for this meta-analysis with cardiovascular risk and total fat intake (t = − 1.01, P = 0.319).
Trans fatty acids intake and risk of CVDs
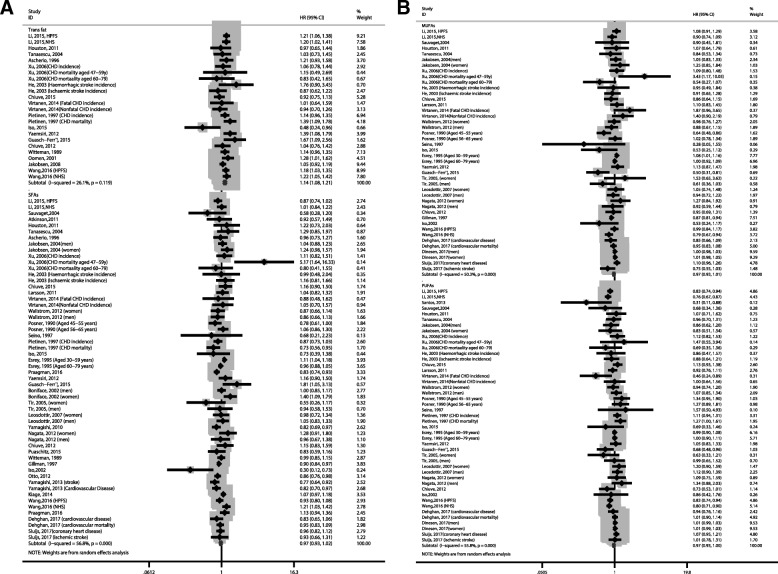
Twenty-four studies reported the effect of dietary TFA intake on CVDs risk. Highest versus lowest levels of dietary TFA were associated with increased risk of CVDs [1.14(1.08–1.21), I2 = 26.1%; Fig. 3a]. Sensitivity analysis showed that no individual study had an excessive influence on the pooled effect.
Fig. 3.
Forest plots of cardiovascular disease for the highest versus lowest categories of dietary trans fatty acids (a), saturated fatty acids (a), monounsaturated fatty acids (b), and polyunsaturated fatty acids intake (b)
Subgroup analysis
In subgroup analysis, the positive association between dietary trans fatty acids intake and CVDs risk were observed in most studies except those were not adjusted for smoking and body mass index, and studies adjusted for sex (Table 1).
Publication bias
Egger test showed no evidence of significant publication bias for this meta-analysis with cardiovascular risk and TFA intake (t = − 1.00, P = 0.330).
Saturated fatty acids intake and risk of CVDs
Fifty-six studies reported the association between dietary SFA intake and CVDs risk. Highest versus lowest levels of dietary SFA were not associated with the risk of CVDs [0.97(0.93–1.02), I2 = 56.8%; Fig. 3a]. Sensitivity analysis showed that no individual study had an excessive influence on the pooled effect. There was evidence of significant heterogeneity (I2 = 56.8%), which was further explored in meta-regression. All covariates investigated in the meta-regression provided a poor explanation of the heterogeneity. In addition, the analysis was repeated stratified according to each covariate. The results were consistent with that observed in meta-regression.
Subgroup analysis
As shown in Table 1, a significant inverse association was observed in Asia population [0.84(0.73–0.97), I2 = 42.3%] but not American and European population. No significant associations were found for subgroups by follow-up duration (< 10 years or ≥ 10 years), or whether the results were adjusted for age, sex, physical activity, energy intake, alcohol, smoking, or body mass index (P > 0.05).
Publication bias
Egger test showed no evidence of significant publication bias for this meta-analysis with cardiovascular risk and saturated fatty acids intake (t = − 0.28, P = 0.777).
Monounsaturated fatty acids intake and risk of CVDs
Forty-three studies reported the relationship between dietary MUFA intake and CVDs risk. Highest versus lowest levels of dietary MUFA were not associated with the risk of CVDs risk [0.97(0.93–1.01), I2 = 50.3%; Fig. 3b]. Sensitivity analysis showed that no individual study had an excessive influence on the pooled effect. There was evidence of significant heterogeneity (I2 = 50.3%), which was further explored in meta-regression. All covariates investigated in the meta-regression provided a poor explanation of the heterogeneity. In addition, the analysis was repeated stratified according to each covariate. The results were consistent with that observed in meta-regression.
Subgroup analysis
Non-significant associations of dietary monounsaturated fatty acids intake and cardiovascular risk were detected in the subgroup analysis conducted by geographical location (Americas, Europe, or other), follow-up duration (< 10 years or ≥ 10 years), and whether the results were adjusted for age, sex, physical activity, energy intake, alcohol, smoking, or body mass index (Table 1).
Publication bias
Egger test showed no evidence of significant publication bias for this meta-analysis with cardiovascular risk and monounsaturated fatty acids intake (t = − 1.45, P = 0.154).
Polyunsaturated fatty acids intake and risk of CVDs
Forty-five studies reported the effect of dietary PUFA intake on CVDs risk. Highest versus lowest levels of dietary PUFA were not associated with the risk of cardiovascular disease [0.97(0.93–1.004), I2 = 55.8%; Fig. 3b]. Sensitivity analysis showed that no individual study had an excessive influence on the pooled effect. There was evidence of significant heterogeneity (I2 = 55.8%), which was further explored in meta-regression. All covariates investigated in the meta-regression provided a poor explanation of the heterogeneity. In addition, the analysis was repeated stratified according to each covariate. The results were consistent with that observed in meta-regression.
Subgroup analysis
In subgroup analysis, a significant inverse association was observed in the studies that has been followed up more than 10 years [0.95(0.91–0.99), I2 = 62.4%] (Table 1). No significant associations were found for the other subgroups analysis (P > 0.05).
Publication bias
Egger test showed no evidence of significant publication bias for this meta-analysis with cardiovascular risk and polyunsaturated fatty acids intake (t = − 1.74, P = 0.088).
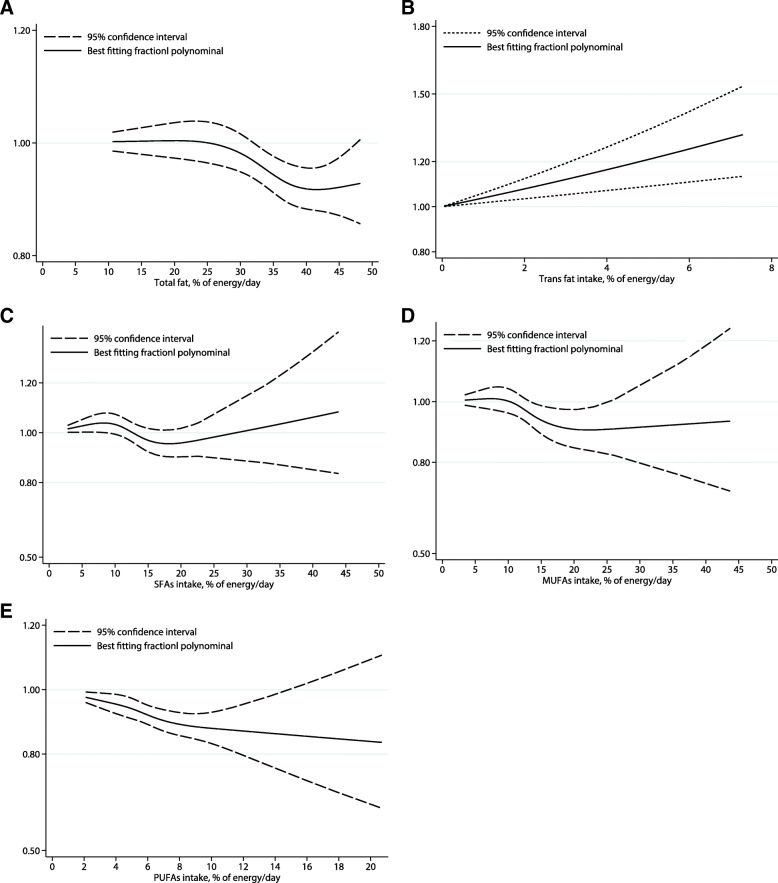
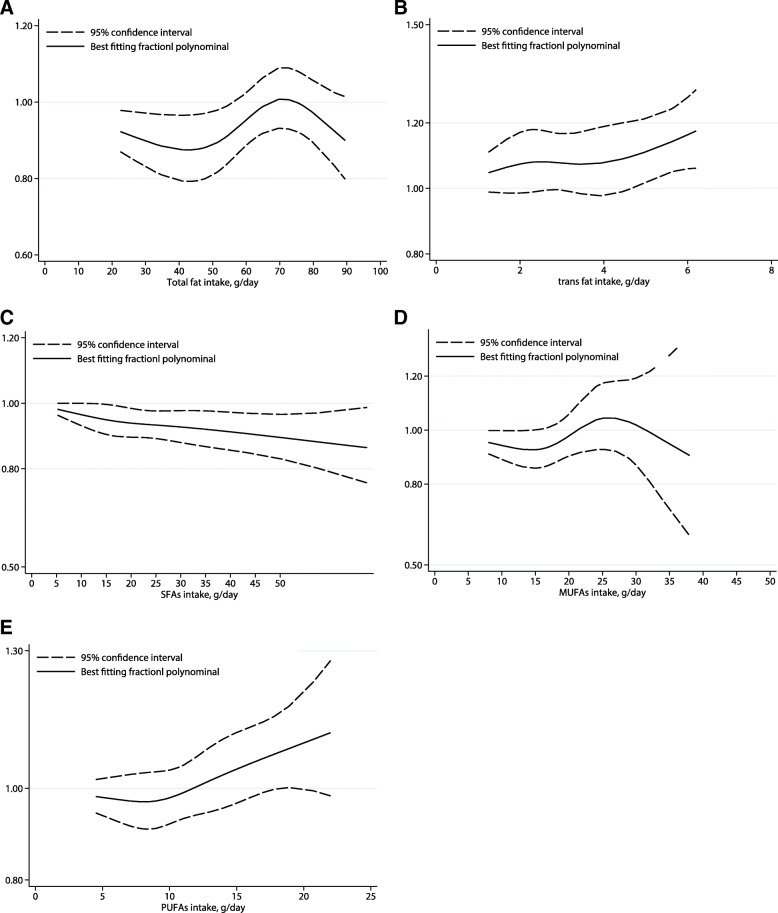
Dose-response analysis
The dose-response analysis suggested non-significant linear relationship between dietary total fat, SFA, MUFA, and PUFA and CVDs risk [0.99(0.97–1.01), Plinearity = 0.164 and 1.01(0.99–1.02), Plinearity = 0.848 for an increment of 5% energy and 5 g/day of total dietary fat, respectively; 0.99(0.95–1.04), Plinearity = 0.474 and 0.98 (0.95–1.00), Plinearity = 0.526 for an increment of 5% energy and 5 g/day of SFA, respectively; 0.96(0.91–1.02), Plinearity = 0.471 and 1.00 (0.94–1.06), Plinearity = 0.256 for an increment of 5% energy and 5 g/day of MUFA, respectively; 0.92(0.84–1.01), Plinearity = 0.757 for an increment of 5% energy of dietary PUFA intake). However, the risk of CVDs increased 16% [1.16(1.07–1.25), Plinearity = 0.033], and 4% [1.04(1.01–1.07), Plinearity = 0.030] for an increment of 2% energy of dietary TFA intake and 5 g/day dietary PUFA intake, respectively (Figs. 4, 5, Additional file 2: Figure S1, Additional file 3: Figure S2, Additional file 4: Figure S3, Additional file 5: Figure S4, and Additional file 6: Figure S5).
Fig. 4.
Dose-response analyses of the linear association between dietary total fat (a), trans fatty acids (b), saturated fatty acids (c), monounsaturated fatty acids (d), and polyunsaturated fatty acids intake (e) and the risk of cardiovascular disease (% energy/day)
Fig. 5.
Dose-response analyses of the linear association between dietary total fat (a), trans fatty acids (b), saturated fatty acids (c), monounsaturated fatty acids (d), and polyunsaturated fatty acids intake (e) and the risk of cardiovascular disease(g/d)
Discussion
This is the first study to investigate the effect of dietary total fat and fatty acid intake on CVDs risk based on dose-response meta-analysis of prospective cohort studies. Results from this meta-analysis did not detect any relationship of dietary total fat, PUFA, MUFA, and SFA intake with CVD risk. However, we found that dietary TFA intake had a dose-response association with CVDs risk. Subgroup analysis suggested inverse associations between PUFAs intake and CVDs risk among studies followed up for more than 10 years.
In contrast to popular accepted viewpoints, we did not detect a positive association between total dietary fat intake and CVDs risk. For decades, it has been believed that fat intake was a risk factor for CVDs, based on the presumption that dietary fat can increase low density lipoprotein (LDL) cholesterol and blood pressure, therefore increase CVDs risk. This viewpoint might be based on selective emphasis on some studies [25, 40, 47], but ignore other studies that do not support these conclusion [15, 36, 51]. Previous meta-analysis also suggested no association between total dietary fat intake and endometrial cancer [63], ulcerative colitis [64], and breast cancer mortality [65], adding new information to reconsider the recommendations of dietary guidelines to reduce fat intake. Even though this study does not support the popular viewpoint that dietary fat intake could increase CVDs risk, it is possible that the role of dietary fat played in the development of CVDs might be confounded by the fat sources. For instance, vegetables and fruits play protective roles in the development of CVDs. However, we could not investigate the different effects of fat from animal, vegetables and fruit separately in this current meta-analysis.
Skeaff et.al. found that dietary TFA intake can increase risk of CHD mortality and incidence [1.32 (1.08–1.61, P = 0.006) and 1.25(1.07–1.46) P = 0.007), respectively] [66], which is consistent with our meta-analysis. The potential mechanism might be via inflammation process and blood lipids [67]. A recent randomized controlled clinical (RCT) showed that the reduction in TFA intake over 1 year was significantly associated with a reduction in LDL particle number (LDL-P), a novel marker of CVD risk [68]. The meta-analysis of 7 RCTs suggested that increased TFA intake lead to an increase in total and LDL-cholesterol and a decrease in HDL-cholesterol concentrations [69]. Some studies have also demonstrated that increased TFA intake may impair insulin sensitivity [70], increase soluble tumor necrosis factor alpha receptors 1 and 2 (sTNF-R1, sTNF-R2, [71]), and C-reactive protein concentrations [72].
We found no significant association between dietary PUFA or SFA intake and CVDs risk, subgroup analysis suggested that the relative risk of CVDs in the highest compared with the lowest categories of PUFA intake was reduced by 5% in studies that has been followed up for more than 10 years, which suggested that the nonsignificant cardio-protective effect of PUFA might be ascribed to the relatively short follow up duration. The non-significant associations between PUFA and CVD risk detected by a recent research conducted by PURE [18] from five continents (mean follow up time:7.4 years) might be also ascribed to the relative short follow up time. All of these evidences demonstrated that studies with longer follow up time are needed to clarify the effect of dietary PUFA on CVDs risk.
The dose-response analysis suggested a linear relationship between dietary TFA and the risk of CVDs. However, we found no evidence for the linear effects of dietary total fat, SFA, MUFA intake on CVDs risk, supporting the validity of the main analysis results that there is no significant effect of total dietary fat, MUFA, and SFA on the risk of CVDs. What’s surprising, the dose-response analysis found a positive dose-response relationship among studies based on dietary PUFA intake as a g/day but not % of energy/day. Thus, we studied each individual study that based on dietary PUFA intake as a g/day respectively, finding only one study showed a significant association between dietary PUFA intake and CVDs risk [highest vs. lowest RR: 1.27 (1.00–1.61)], and the author suggested that the harmful effect might be ascribed the high content of mercury in local fish, a major source of PUFA. Further study adjusted mercury exposure are needed to clarify the hypothesis.
Potential limitations to this study should also be considered. As common in meta-analysis, publication bias is inevitable. However, the funnel plots and Begg’s test suggested no significant publication bias through. In addition, dietary data from most studies were collected by FFQ, which may introduce measurement errors by the over- or under-reporting of the amounts of food that they usually eaten every day. Thirdly, covariates adjustment could also influence the association between fat and CVDs risk, although we extracted the risk estimates that adjusted the greatest degree of potential confounders which varied among different studies. Forth, we found significant heterogeneity in our study. However, previous studies suggested that when there are many studies with large sample sizes, the I2 test may detect statistically significant but clinically nonsignificant heterogeneity, which may be the case in our study [73]. What’s more, we also explored potential sources of heterogeneity through subgroup and meta-regression analysis, which further proves that our findings are robust.
Our analysis has several strengths. We limited our analysis to prospective cohort studies to minimize the influence of recall and selection biases that are common in case-control studies. Moreover, we conducted a dose-response curve instead of only comparing highest vs. lowest fat consumers. The health effect of diet fat may vary among different fat types. Therefore, it is another strength to combine studies that have investigated the effect of different major dietary fat types on CVDs.
Conclusions
This current meta-analysis of cohort studies suggested that total fat, SFA, MUFA, and PUFA intake were not associated with the risk of cardiovascular disease. However, we found that higher TFA intake is associated with greater risk of CVDs in a dose-response fashion. Furthermore, the subgroup analysis found a cardio-protective effect of PUFA in studies followed up for more than 10 years. Dietary guidelines taking these findings into consideration might be more credible.
Additional files
Table S1. Characteristics of included cohort studies reporting CVDs risk and fat intake. (DOCX 82 kb)
Figure S1. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of total dietary fat and the risk of cardiovascular disease. (EPS 2101 kb)
Figure S2. Dose-response forest plot of every 2 energy/day (or 2 g/day) increased intake of dietary tans fatty acids and the risk of cardiovascular disease. (EPS 1709 kb)
Figure S3. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary saturated fatty acids and the risk of cardiovascular disease. (EPS 1904 kb)
Figure S4. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary monounsaturated fatty acids and the risk of cardiovascular disease. (EPS 48 kb)
Figure S5. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary polyunsaturated fatty acids and the risk of cardiovascular disease. (EPS 2084 kb)
Acknowledgements
Not applicable
Funding
This work was supported by the National Natural Science Foundation of China (81602852).
Availability of data and materials
All data generated or analyzed during this study are included in this article.
Abbreviations
- CVD
Cardiovascular diseases
- FFQ
Food frequency questionnaire
- HR
Hazard ratio
- JACC
Japan Collaborative Cohort Study for Evaluation of Cancer Risk
- LDL
Low density lipoprotein
- LDL-P
LDL particle number
- MedDiets
Mediterranean diets
- MUFA
Monounsaturated fatty acids
- PREDIMED
REvención con DIeta MEDiterránea study
- PUFA
Polyunsaturated fatty acids
- PURE
The Prospective Urban Rural Epidemiological
- RR
Relative risk
- SFA
Saturated fatty acids
- sTNF-R1
Soluble tumor necrosis factor alpha receptors 1
- sTNF-R2
Soluble tumor necrosis factor alpha receptors 2
- TFA
Trans fatty acids
Authors’ contributions
YZ and YB contributed to acquisition of data, analysis and interpretation of data and drafting the article. YL contributed to conception and design, revise the article critically for important intellectual content and final approval of the version to be published. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Organization WH. Cardiovascular diseases (CVDs). http://www.who.int/mediacentre/factsheets/fs317/en/. Accessed on 17 May 2017
- 2.Willett WC. Dietary fats and coronary heart disease. J Intern Med. 2012;272:13–24. doi: 10.1111/j.1365-2796.2012.02553.x. [DOI] [PubMed] [Google Scholar]
- 3.Mente A, de Koning L, Shannon HS, Anand SS. A systematic review of the evidence supporting a causal link between dietary factors and coronary heart disease. Arch Intern Med. 2009;169:659–669. doi: 10.1001/archinternmed.2009.38. [DOI] [PubMed] [Google Scholar]
- 4.Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2015;10:Cd011737. [DOI] [PubMed]
- 5.Widmer RJ, Flammer AJ, Lerman LO, Lerman A. The Mediterranean diet, its components, and cardiovascular disease. Am J Med. 2015;128:229–238. doi: 10.1016/j.amjmed.2014.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nations FaAOotU . Summary of conclusions and dietary recommendations on total fat and fatty acids in fats and fatty acids in human nutrition—report of an expert consultation. Geneva: FAO/WHO; 2010. [PubMed] [Google Scholar]
- 7.Michas G, Micha R, Zampelas A. Dietary fats and cardiovascular disease: putting together the pieces of a complicated puzzle. Atherosclerosis. 2014;234:320–328. doi: 10.1016/j.atherosclerosis.2014.03.013. [DOI] [PubMed] [Google Scholar]
- 8.Calder PC. n-3 polyunsaturated fatty acids, inflammation, and inflammatory diseases. Am J Clin Nutr. 2006;83:1505s–1519s. doi: 10.1093/ajcn/83.6.1505S. [DOI] [PubMed] [Google Scholar]
- 9.Munoz A, Costa M. Nutritionally mediated oxidative stress and inflammation. Oxidative Med Cell Longev. 2013;2013:610950. doi: 10.1155/2013/610950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Longhi R, Almeida RF, Pettenuzzo LF, Souza DG, Machado L, Quincozes-Santos A, Souza DO. Effect of a trans fatty acid-enriched diet on mitochondrial, inflammatory, and oxidative stress parameters in the cortex and hippocampus of Wistar rats. Eur J Nutr. 2018;57:1913–1924. doi: 10.1007/s00394-017-1474-3. [DOI] [PubMed] [Google Scholar]
- 11.Sverdlov AL, Elezaby A, Qin F, Behring JB, Luptak I, Calamaras TD, Siwik DA, Miller EJ, Liesa M, Shirihai OS, et al. Mitochondrial reactive oxygen species mediate cardiac structural, functional, and mitochondrial consequences of diet-induced metabolic heart disease. J Am Heart Assoc. 2016;5:e002555. doi: 10.1161/JAHA.115.002555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ruparelia N, Chai JT, Fisher EA, Choudhury RP. Inflammatory processes in cardiovascular disease: a route to targeted therapies. Nat Rev Cardiol. 2017;14:133–144. doi: 10.1038/nrcardio.2016.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, Gomez-Gracia E, Ruiz-Gutierrez V, Fiol M, Lapetra J, et al. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med. 2013;368:1279–1290. doi: 10.1056/NEJMoa1200303. [DOI] [PubMed] [Google Scholar]
- 14.Guasch-Ferre M, Babio N, Martinez-Gonzalez MA, Corella D, Ros E, Martin-Pelaez S, Estruch R, Aros F, Gomez-Gracia E, Fiol M, et al. Dietary fat intake and risk of cardiovascular disease and all-cause mortality in a population at high risk of cardiovascular disease. Am J Clin Nutr. 2015;102:1563–1573. doi: 10.3945/ajcn.115.112029. [DOI] [PubMed] [Google Scholar]
- 15.Houston DK, Ding J, Lee JS, Garcia M, Kanaya AM, Tylavsky FA, Newman AB, Visser M, Kritchevsky SB. Dietary fat and cholesterol and risk of cardiovascular disease in older adults: the health ABC study. Nutr Metab Cardiovasc Dis. 2011;21:430–437. doi: 10.1016/j.numecd.2009.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hu FB, Stampfer MJ, Rimm E, Ascherio A, Rosner BA, Spiegelman D, Willett WC. Dietary fat and coronary heart disease: a comparison of approaches for adjusting for total energy intake and modeling repeated dietary measurements. Am J Epidemiol. 1999;149:531–540. doi: 10.1093/oxfordjournals.aje.a009849. [DOI] [PubMed] [Google Scholar]
- 17.Yamagishi K, Iso H, Yatsuya H, Tanabe N, Date C, Kikuchi S, Yamamoto A, Inaba Y, Tamakoshi A. Dietary intake of saturated fatty acids and mortality from cardiovascular disease in Japanese: the Japan collaborative cohort study for evaluation of cancer risk (JACC) study. Am J Clin Nutr. 2010;92:759–765. doi: 10.3945/ajcn.2009.29146. [DOI] [PubMed] [Google Scholar]
- 18.Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, Iqbal R, Kumar R, Wentzel-Viljoen E, Rosengren A, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–2062. doi: 10.1016/S0140-6736(17)32252-3. [DOI] [PubMed] [Google Scholar]
- 19.Mann J, Meerpohl J, Nishida C, McLean R, Te Morenga L. Associations of fats and carbohydrates with cardiovascular disease and mortality-PURE and simple? Lancet. 2018;391:1676. doi: 10.1016/S0140-6736(18)30804-3. [DOI] [PubMed] [Google Scholar]
- 20.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 21.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Bmj. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Harrell FE, Jr, Lee KL, Pollock BG. Regression models in clinical studies: determining relationships between predictors and response. J Natl Cancer Inst. 1988;80:1198–1202. doi: 10.1093/jnci/80.15.1198. [DOI] [PubMed] [Google Scholar]
- 23.Threapleton DE, Greenwood DC, Evans CE, Cleghorn CL, Nykjaer C, Woodhead C, Cade JE, Gale CP, Burley VJ. Dietary fibre intake and risk of cardiovascular disease: systematic review and meta-analysis. Bmj. 2013;347:f6879. doi: 10.1136/bmj.f6879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Larsson SC, Virtamo J, Wolk A. Dietary fats and dietary cholesterol and risk of stroke in women. Atherosclerosis. 2012;221:282–286. doi: 10.1016/j.atherosclerosis.2011.12.043. [DOI] [PubMed] [Google Scholar]
- 25.Virtanen JK, Mursu J, Tuomainen TP, Voutilainen S. Dietary fatty acids and risk of coronary heart disease in men: the Kuopio ischemic heart disease risk factor study. Arterioscler Thromb Vasc Biol. 2014;34:2679–2687. doi: 10.1161/ATVBAHA.114.304082. [DOI] [PubMed] [Google Scholar]
- 26.Wallstrom P, Sonestedt E, Hlebowicz J, Ericson U, Drake I, Persson M, Gullberg B, Hedblad B, Wirfalt E. Dietary fiber and saturated fat intake associations with cardiovascular disease differ by sex in the Malmo diet and cancer cohort: a prospective study. PLoS One. 2012;7:e31637. doi: 10.1371/journal.pone.0031637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yaemsiri S, Sen S, Tinker L, Rosamond W, Wassertheil-Smoller S, He K. Trans fat, aspirin, and ischemic stroke in postmenopausal women. Ann Neurol. 2012;72:704–715. doi: 10.1002/ana.23555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.dos Santos AL, Weiss T, Duarte CK, Gross JL, de Azevedo MJ, Zelmanovitz T. Dietary fat composition and cardiac events in patients with type 2 diabetes. Atherosclerosis. 2014;236:31–38. doi: 10.1016/j.atherosclerosis.2014.06.014. [DOI] [PubMed] [Google Scholar]
- 29.Sauvaget C, Nagano J, Hayashi M, Yamada M. Animal protein, animal fat, and cholesterol intakes and risk of cerebral infarction mortality in the adult health study. Stroke. 2004;35:1531–1537. doi: 10.1161/01.STR.0000130426.52064.09. [DOI] [PubMed] [Google Scholar]
- 30.Leosdottir M, Nilsson PM, Nilsson JA, Berglund G. Cardiovascular event risk in relation to dietary fat intake in middle-aged individuals: data from the Malmo diet and cancer study. Eur J Cardiovasc Prev Rehabil. 2007;14:701–706. doi: 10.1097/HJR.0b013e3282a56c45. [DOI] [PubMed] [Google Scholar]
- 31.Nagata C, Nakamura K, Wada K, Oba S, Tsuji M, Tamai Y, Kawachi T. Total fat intake is associated with decreased mortality in Japanese men but not in women. J Nutr. 2012;142:1713–1719. doi: 10.3945/jn.112.161661. [DOI] [PubMed] [Google Scholar]
- 32.Oomen CM, Ocké MC, Feskens EJM, Erp-Baart M-AJ, Kok FJ, Kromhout D. Association between trans fatty acid intake and 10-year risk of coronary heart disease in the Zutphen elderly study: a prospective population-based study. Lancet. 2001;357:746–751. doi: 10.1016/S0140-6736(00)04166-0. [DOI] [PubMed] [Google Scholar]
- 33.Iso H. Fat and protein intakes and risk of Intraparenchymal hemorrhage among middle-aged Japanese. Am J Epidemiol. 2003;157:32–39. doi: 10.1093/aje/kwf166. [DOI] [PubMed] [Google Scholar]
- 34.Boden-Albala B, Elkind MS, White H, Szumski A, Paik MC, Sacco RL. Dietary total fat intake and ischemic stroke risk: the northern Manhattan study. Neuroepidemiology. 2009;32:296–301. doi: 10.1159/000204914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.de Oliveira Otto MC, Mozaffarian D, Kromhout D, Bertoni AG, Sibley CT, Jacobs DR, Jr, Nettleton JA. Dietary intake of saturated fat by food source and incident cardiovascular disease: the multi-ethnic study of atherosclerosis. Am J Clin Nutr. 2012;96:397–404. doi: 10.3945/ajcn.112.037770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Atkinson C, Whitley E, Ness A, Baker I. Associations between types of dietary fat and fish intake and risk of stroke in the Caerphilly prospective study (CaPS) Public Health. 2011;125:345–348. doi: 10.1016/j.puhe.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 37.Gillman MW, Cupples LA, Millen BE, Ellison RC, Wolf PA. Inverse association of dietary fat with development of ischemic stroke in men. Jama. 1997;278:2145–2150. doi: 10.1001/jama.1997.03550240035030. [DOI] [PubMed] [Google Scholar]
- 38.Witteman JC, Willett WC, Stampfer MJ, Colditz GA, Sacks FM, Speizer FE, Rosner B, Hennekens CH. A prospective study of nutritional factors and hypertension among US women. Circulation. 1989;80:1320–1327. doi: 10.1161/01.CIR.80.5.1320. [DOI] [PubMed] [Google Scholar]
- 39.Leosdottir M, Nilsson PM, Nilsson JA, Mansson H, Berglund G. Dietary fat intake and early mortality patterns--data from the Malmo diet and cancer study. J Intern Med. 2005;258:153–165. doi: 10.1111/j.1365-2796.2005.01520.x. [DOI] [PubMed] [Google Scholar]
- 40.Boniface DR, Tefft ME. Dietary fats and 16-year coronary heart disease mortality in a cohort of men and women in Great Britain. Eur J Clin Nutr. 2002;56:786. doi: 10.1038/sj.ejcn.1601509. [DOI] [PubMed] [Google Scholar]
- 41.Esrey KL, Joseph L, Grover SA. Relationship between dietary intake and coronary heart disease mortality: lipid research clinics prevalence follow-up study. J Clin Epidemiol. 1996;49:211–216. doi: 10.1016/0895-4356(95)00066-6. [DOI] [PubMed] [Google Scholar]
- 42.Iso H, Stampfer MJ, Manson JE, Rexrode K, Hu F, Hennekens CH, Colditz GA, Speizer FE, Willett WC. Prospective study of fat and protein intake and risk of intraparenchymal hemorrhage in women. Circulation. 2001;103:856–863. doi: 10.1161/01.CIR.103.6.856. [DOI] [PubMed] [Google Scholar]
- 43.Pietinen P, Ascherio A, Korhonen P, Hartman AM, Willett WC, Albanes D, Virtamo J. Intake of fatty acids and risk of coronary heart disease in a cohort of Finnish men. The alpha-tocopherol, beta-carotene cancer prevention study. Am J Epidemiol. 1997;145:876–887. doi: 10.1093/oxfordjournals.aje.a009047. [DOI] [PubMed] [Google Scholar]
- 44.Seino F, Date C, Nakayama T, Yoshiike N, Yokoyama T, Yamaguchi M, Tanaka H. Dietary lipids and incidence of cerebral infarction in a Japanese rural community. J Nutr Sci Vitaminol (Tokyo) 1997;43:83–99. doi: 10.3177/jnsv.43.83. [DOI] [PubMed] [Google Scholar]
- 45.Posner BM, Cobb JL, Belanger AJ, Cupples LA, D'Agostino RB, Stokes J., 3rd Dietary lipid predictors of coronary heart disease in men. The Framingham study. Arch Intern Med. 1991;151:1181–1187. doi: 10.1001/archinte.1991.00400060105018. [DOI] [PubMed] [Google Scholar]
- 46.He K, Merchant A, Rimm EB, Rosner BA, Stampfer MJ, Willett WC, Ascherio A. Dietary fat intake and risk of stroke in male US healthcare professionals: 14 year prospective cohort study. BMJ. 2003;327:777–782. doi: 10.1136/bmj.327.7418.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Xu J, Eilat-Adar S, Loria C, Goldbourt U, Howard BV, Fabsitz RR, Zephier EM, Mattil C, Lee ET. Dietary fat intake and risk of coronary heart disease: the strong heart study. Am J Clin Nutr. 2006;84:894–902. doi: 10.1093/ajcn/84.4.894. [DOI] [PubMed] [Google Scholar]
- 48.Wang DD, Li Y, Chiuve SE, Stampfer MJ, Manson JE, Rimm EB, Willett WC, Hu FB. Association of specific dietary fats with total and cause-specific mortality. JAMA Intern Med. 2016;176:1134–1145. doi: 10.1001/jamainternmed.2016.2417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tanasescu M, Cho E, Manson JE, Hu FB. Dietary fat and cholesterol and the risk of cardiovascular disease among women with type 2 diabetes. Am J Clin Nutr. 2004;79:999–1005. doi: 10.1093/ajcn/79.6.999. [DOI] [PubMed] [Google Scholar]
- 50.Ascherio A, Rimm EB, Giovannucci EL, Spiegelman D, Stampfer M, Willett WC. Dietary fat and risk of coronary heart disease in men: cohort follow up study in the United States. Bmj. 1996;313:84–90. doi: 10.1136/bmj.313.7049.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jakobsen MU, Overvad K, Dyerberg J, Schroll M, Heitmann BL. Dietary fat and risk of coronary heart disease: possible effect modification by gender and age. Am J Epidemiol. 2004;160:141–149. doi: 10.1093/aje/kwh193. [DOI] [PubMed] [Google Scholar]
- 52.Chiuve SE, Sandhu RK, Moorthy MV, Glynn RJ, Albert CM. Dietary fat intake is differentially associated with risk of paroxysmal compared with sustained atrial fibrillation in women. J Nutr. 2015;145:2092–2101. doi: 10.3945/jn.115.212860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Chiuve SE, Rimm EB, Sandhu RK, Bernstein AM, Rexrode KM, Manson JE, Willett WC, Albert CM. Dietary fat quality and risk of sudden cardiac death in women. Am J Clin Nutr. 2012;96:498–507. doi: 10.3945/ajcn.112.040287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Puaschitz NG, Strand E, Norekval TM, Dierkes J, Dahl L, Svingen GF, Assmus J, Schartum-Hansen H, Oyen J, Pedersen EK, et al. Dietary intake of saturated fat is not associated with risk of coronary events or mortality in patients with established coronary artery disease. J Nutr. 2015;145:299–305. doi: 10.3945/jn.114.203505. [DOI] [PubMed] [Google Scholar]
- 55.Praagman J, de Jonge EA, Kiefte-de Jong JC, Beulens JW, Sluijs I, Schoufour JD, Hofman A, van der Schouw YT, Franco OH. Dietary saturated fatty acids and coronary heart disease risk in a Dutch middle-aged and elderly population. Arterioscler Thromb Vasc Biol. 2016;36:2011–2018. doi: 10.1161/ATVBAHA.116.307578. [DOI] [PubMed] [Google Scholar]
- 56.Dinesen PT, Joensen AM, Rix TA, Tjonneland A, Schmidt EB, Lundbye-Christensen S, Overvad K. Effect of dietary intake of saturated fatty acids on the development of atrial fibrillation and the effect of replacement of saturated with monounsaturated and polyunsaturated fatty acids. Am J Cardiol. 2017;120:1129–1132. doi: 10.1016/j.amjcard.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 57.Sluijs I, Praagman J, Boer JMA, Verschuren WMM, van der Schouw YT. Fluidity of the dietary fatty acid profile and risk of coronary heart disease and ischemic stroke: results from the EPIC-Netherlands cohort study. Nutr Metab Cardiovasc Dis. 2017;27:799–805. doi: 10.1016/j.numecd.2017.06.008. [DOI] [PubMed] [Google Scholar]
- 58.Jakobsen MU, Overvad K, Dyerberg J, Heitmann BL. Intake of ruminant trans fatty acids and risk of coronary heart disease. Int J Epidemiol. 2008;37:173–182. doi: 10.1093/ije/dym243. [DOI] [PubMed] [Google Scholar]
- 59.Kiage JN, Merrill PD, Judd SE, He K, Lipworth L, Cushman M, Howard VJ, Kabagambe EK. Intake of trans fat and incidence of stroke in the REasons for geographic and racial differences in stroke (REGARDS) cohort. Am J Clin Nutr. 2014;99:1071–1076. doi: 10.3945/ajcn.113.075713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Li Y, Hruby A, Bernstein AM, Ley SH, Wang DD, Chiuve SE, Sampson L, Rexrode KM, Rimm EB, Willett WC. Saturated fats compared with unsaturated fats and sources of carbohydrates in relation to risk of coronary heart disease: a prospective cohort study. J Am Coll Cardiol. 2015;66:1538–1548. doi: 10.1016/j.jacc.2015.07.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Praagman J, Beulens JW, Alssema M, Zock PL, Wanders AJ, Sluijs I, van der Schouw YT. The association between dietary saturated fatty acids and ischemic heart disease depends on the type and source of fatty acid in the European prospective investigation into Cancer and nutrition-Netherlands cohort. Am J Clin Nutr. 2016;103:356–365. doi: 10.3945/ajcn.115.122671. [DOI] [PubMed] [Google Scholar]
- 62.Yamagishi K, Iso H, Kokubo Y, Saito I, Yatsuya H, Ishihara J, Inoue M, Tsugane S. Dietary intake of saturated fatty acids and incident stroke and coronary heart disease in Japanese communities: the JPHC study. Eur Heart J. 2013;34:1225–1232. doi: 10.1093/eurheartj/eht043. [DOI] [PubMed] [Google Scholar]
- 63.Jiang L, Hou R, Gong TT, Wu QJ. Dietary fat intake and endometrial cancer risk: dose-response meta-analysis of epidemiological studies. Sci Rep. 2015;5:16693. doi: 10.1038/srep16693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wang F, Lin X, Zhao Q, Li J. Fat intake and risk of ulcerative colitis: systematic review and dose-response meta-analysis of epidemiological studies. J Gastroenterol Hepatol. 2017;32:19–27. doi: 10.1111/jgh.13416. [DOI] [PubMed] [Google Scholar]
- 65.Brennan SF, Woodside JV, Lunny PM, Cardwell CR, Cantwell MM. Dietary fat and breast cancer mortality: a systematic review and meta-analysis. Crit Rev Food Sci Nutr. 2017;57:1999–2008. doi: 10.1080/10408398.2012.724481. [DOI] [PubMed] [Google Scholar]
- 66.Skeaff CM, Miller J. Dietary fat and coronary heart disease: summary of evidence from prospective cohort and randomised controlled trials. Ann Nutr Metab. 2009;55:173–201. doi: 10.1159/000229002. [DOI] [PubMed] [Google Scholar]
- 67.de Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, Uleryk E, Budylowski P, Schunemann H, Beyene J, Anand SS: Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ 2015, 351:h3978. [DOI] [PMC free article] [PubMed]
- 68.Garshick M, Mochari-Greenberger H, Mosca L. Reduction in dietary trans fat intake is associated with decreased LDL particle number in a primary prevention population. Nutr Metab Cardiovasc Dis. 2014;24:100–106. doi: 10.1016/j.numecd.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Aronis KN, Khan SM, Mantzoros CS. Effects of trans fatty acids on glucose homeostasis: a meta-analysis of randomized, placebo-controlled clinical trials. Am J Clin Nutr. 2012;96:1093–1099. doi: 10.3945/ajcn.112.040576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Angelieri CT, Barros CR, Siqueira-Catania A, Ferreira SR. Trans fatty acid intake is associated with insulin sensitivity but independently of inflammation. Braz J Med Biol Res. 2012;45:625–631. doi: 10.1590/S0100-879X2012007500071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mozaffarian D, Pischon T, Hankinson SE, Rifai N, Joshipura K, Willett WC, Rimm EB. Dietary intake of trans fatty acids and systemic inflammation in women. Am J Clin Nutr. 2004;79:606–612. doi: 10.1093/ajcn/79.4.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Lopez-Garcia E, Schulze MB, Meigs JB, Manson JE, Rifai N, Stampfer MJ, Willett WC, Hu FB. Consumption of trans fatty acids is related to plasma biomarkers of inflammation and endothelial dysfunction. J Nutr. 2005;135:562–566. doi: 10.1093/jn/135.3.562. [DOI] [PubMed] [Google Scholar]
- 73.Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. The Cochrane Collaboration. 2011. Available from: http://www.cochrane-handbook.org
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Characteristics of included cohort studies reporting CVDs risk and fat intake. (DOCX 82 kb)
Figure S1. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of total dietary fat and the risk of cardiovascular disease. (EPS 2101 kb)
Figure S2. Dose-response forest plot of every 2 energy/day (or 2 g/day) increased intake of dietary tans fatty acids and the risk of cardiovascular disease. (EPS 1709 kb)
Figure S3. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary saturated fatty acids and the risk of cardiovascular disease. (EPS 1904 kb)
Figure S4. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary monounsaturated fatty acids and the risk of cardiovascular disease. (EPS 48 kb)
Figure S5. Dose-response forest plot of every 5 energy/day (or 5 g/day) increased intake of dietary polyunsaturated fatty acids and the risk of cardiovascular disease. (EPS 2084 kb)
Data Availability Statement
All data generated or analyzed during this study are included in this article.