Abstract
Vaginal rejuvenation procedures are increasing in popularity in terms of types of treatment offered, number of patients undergoing them, clinical studies, and in the controversy surrounding them. Both non-invasive and invasive solutions are being developed by pharmaceutical and technological companies. Radiofrequency devices and lasers are spearheading the energy-based device space, and fillers and platelet-rich plasma are used to address several concerns surrounding vaginal health. In this review, an overview of the growing field of vaginal rejuvenation is presented, as well as the authors’ personal view and analysis of this clinical space.
Introduction
Vaginal rejuvenation refers to procedures that primarily reduce the width of the vagina for reasons of function and well-being (Barbara et al., 2017). The concept is more than a thousand years old and was first described by Trotula in 1050 AD in Treatments for Women, wherein she sutured vaginal lacerations postdelivery. Since then, fueled by increased technological innovation, surgical and nonsurgical treatments have been developed.
Global awareness and changing trends
Today, with increasing life expectancy and women living longer, > 20 million women are affected by uterine prolapse, birthing injuries, and incontinence. Causes for conditions such as vaginal relaxation syndrome or vulvovaginal laxity include vaginal delivery, natural aging, and atrophy. Aside from functional consequences, these conditions also have an effect on women’s sexuality and sense of well-being. Until recently, it was a taboo topic to discuss these topics, even with a women’s health care provider. This fact is highlighted by a survey conducted by the International Urogynaecological Association in 2012, which showed that 84% of physicians believed that vaginal laxity was underreported, and 95% believed that laxity affected sexual function (Pauls et al., 2012).
Moreover, 40% of women have psychological distress from female sexual dysfunction, but only 14% consult a physician about sex during their lifetime (American College of Obstetricians and Gynecologists, Committee on Practice Bulletins-Gynecology, 2011). Today, through public awareness programs, physician education, and media sources, the barriers of communication on issues with regard to female sexual dysfunction and incontinence have been broken. Information on these conditions and treatments options are more readily available, and, as a result, the demand for such interventions is growing.
Aside from surgery, the advent of nonsurgical methods and energy sources for these indications is receiving tremendous response and patient acceptance (Karcher and Sadick, 2016). The American Society of Plastic Surgeons reported a 30% increase in the rate of vaginal rejuvenation procedures between 2005 and 2006 (Lowenstein et al., 2014), and an Indian study also showed growing trends in the demand of esthetic vaginal procedures from 3.9% in 2012 to 28.97% in 2015 (Desai and Dixit, 2018).
Clarity
Female cosmetic genital surgery (FCGS) refers to a subset of treatments that address the vaginal appearance, and the term vaginal rejuvenation has evolved into an umbrella term that covers procedures that enhance vaginal esthetics, sexuality, and functionality. Common procedures include surgical (e.g., vaginal tightening, labia minoraplasty, labia majoraplasty, clitoral hood reduction, clitoral unhooding, lipofilling, and hymen reconstruction) or nonsurgical (e.g., energy-based treatments, platelet-rich plasma [PRP], and fillers) interventions (Barbara et al., 2017).
Results interpretation
The clinical results of procedures for these indications have been assessed in terms of safety and efficacy in several peer-reviewed studies. Although objective, validated measurements and scales are still lacking, indices commonly referred to include the Female Sexual Functional Index (FSFI; Rosen et al., 2000), Millheiser Vaginal Laxity Scale (Millheiser et al., 2010), Millheiser Sexual Satisfaction Scale (Davis et al., 2006), visual analogue scale (Lukaez et al., 2004), International Consultation on Incontinence Questionnaire (Avery et al., 2004), Satisfaction Scores (Likert scale; Sullivan and Artino, 2013), and Vaginal Health Index (Bachmann, 1995).
Surgical vaginoplasty
Surgical vaginoplasty involves surgical vaginal tightening and the correction of vaginal damage or deformity. The procedure may be done under local or regional anesthesia in an office-based surgical facility and involves a full-length tightening of the vagina (i.e., not just of the introitus) whereby dissection occurs all the way up to the levators and laterally to the ischial spines. A depth of 7 to 8 cm is recommended for full-length tightening. The vagina can be resized to the exact dimension the patient desires. This procedure usually also includes perineoplasty because this requires remodeling and strengthening of the perineum. Complication rates of surgical vaginoplasty range from 2% to 3.77% and include dyspareunia, lack of lubrication, constipation, wound infection, hemorrhage, suture breakdown (mostly in the perineum), buttock pain for weeks, and rectal mucosa perforation (Pardo et al., 2006).
Various studies have addressed different aspects of surgical vaginal tightening. In a study of 53 women undergoing surgical colporrhaphy, where the vaginal diameter is decreased by two-thirds, 66% of women showed a great improvement in their sex lives, 24% a significant improvement, and 10% slight or no improvement. There were two cases of wound dehiscence (Pardo et al., 2006). Goodman et al. conducted a large multicenter study of 258 women with FCGS, including 47 cases of vaginoplasty. The researchers concluded that surgical vaginoplasty/perineoplasty showed a high rate of enhancement of sexual functioning in both women and their partners (Goodman et al., 2010).
Another study showed that the Female Sexual Function score was globally improved after colpoperineoplasty in 79 women (Abedi et al., 2014). Dyspareunia and low lubrication were reported as side effects. A recent study of 39 patients undergoing surgical vaginal tightening showed improvements in FSFI from 19.5 to 27 (Desai and Dixit, 2018). This study also showed that 81.6% of patients were very satisfied, 14.5% satisfied, and 3.9% not satisfied with the FCGS procedures.
Noninvasive modalities
Noninvasive procedures for ameliorating symptoms of genitourinary syndrome of menopause (GSM) are increasingly emerging in the form of energy-based devices and injectable agents, such as fillers and PRP (Qureshi et al., 2018).
Energy-based devices for vaginal rejuvenation harness power from radiofrequency (RF) or laser sources, such as carbon dioxide (CO2; 10,600 nm; Table 1) and erbium-YAG (2940 nm; Table 2), to induce thermal-dependent matrix remodeling (Gambacciani et al., 2015a, Gambacciani et al., 2015b). Energy-based devices stimulate type 1 collagen production in the extracellular matrix via the stimulation of fibroblasts. This process results in the contracture of elastin fibers, neovascularization, and improved vaginal lubrication. A study by Ostrzenski on CO2 laser treatment for vaginal rejuvenation included 10 patients who were treated with a continuous-mode CO2 laser with defocus, where vaporization was stopped at the endopelvic fascia. The study showed a great clinical improvement after only one treatment (Ostrzenski, 2012).
Table 1.
Clinical studies using CO2 lasers for vaginal rejuvenation
| Study | Results |
|---|---|
|
Salvatore et al., Climacteric 2015 77 patients, menopausal |
Significant improvement in FSFI scores (14.8–27.2) 17 patients inactive; normal sex life |
|
Gaspar et al., Am J Cosmet Surg 2011 CO2 + PRP + PFE |
Significant reduction in sexual discomfort |
|
Filippini et al., Photomed Laser Surg 2017 386 patients, postmenopausal |
Effective in treating vaginal epithelium and dyspareunia due to atrophy |
|
Perino et al., Maturitas 2015 48 patients, postmenopausal |
Confirmed safety, efficacy, satisfaction in reducing VVA symptoms |
|
Pieralli et al., Arch Gynecol Obstet 2016 50 patients (41–66 years) |
VHI score: 8.9–21.6 (< 15 VVA) VAS: statistics improvement in dyspareunia 52% satisfied at 11 months |
CO2, carbon dioxide; FSFI, Female Sexual Functional Index; VAS, visual analog scale; VHI, vaginal health index; VVA, vulvovaginal atrophy
Table 2.
Clinical studies using Er:YAG lasers for vaginal rejuvenation
| Study | Results |
|---|---|
| Adrian, J Lasers Health Acad 2012 | Improved tightening |
|
Gambacciani et al., 2015a, Gambacciani et al., 2015b 45 patients (postmenopausal) |
Significant decrease in vaginal dryness and dyspareunia |
| Vizintin et al., Climacteric 2015 | Effective and safe to treat vaginal laxity |
Recent RF studies showed an increase in the small nerve fiber density in the papillary dermis (Gold et al., 2018; Table 3). Posttreatment biopsy tests have demonstrated neocollagenesis and neoelastogenesis in the submucosa after RF (Leibaschoff et al., 2016; Figure). The creation of new elastin, which is relatively unique to RF, may contribute to treating vaginal laxity (Tadir et al., 2017). Several types of RF devices exist, and some have been developed with specific hand pieces for the vaginal canal (Sadick et al., 2014). Transurethral monopolar RF has also been used to treat stress urinary incontinence (SUI). Nonablative RF was used to achieve tightening of the vaginal canal (Dillon and Dmochowski, 2009, Sadick et al., 2014).
Table 3.
Clinical studies on the use of radiofrequency devices for vaginal rejuvenation
| Device | Study | No. of patients | Results | Adverse effects |
|---|---|---|---|---|
| TTCRF |
Leibaschoff et al., Surg Technol Int 2016 GSM; prospective RCT |
20 | VHI, ICIQ-UI, UDI6, IIQ7, VAS, punch biopsies Marked improvement |
None |
|
Alinsod, Prime 2015 Prospective for laxity, UI |
23 | Statistically significant: Vaginal laxity, sexual satisfaction. Improved SUI, atrophy, orgasms |
None | |
|
Alinsod, Lasers Surg Med 2016 Prospective for orgasms |
25 | Average reduced time to orgasm 50% Improved tightening, moisture, sensitivity Co-relates with histopathology |
None | |
| CMRF |
Millheiser et al., J Sex Med 2010 Prospective for laxity |
24 | 87% improved in 6 months Sexual scores: 27.6–32 Sustained improvement on SSQ at 6 months |
None |
|
Sekiguchi et al., J Womens Health 2013 Prospective for laxity |
30 | Significant FSFI: 22.4–26 | None | |
|
Kryhman et al., J Sex Med 2017 Randomized, placebo sham controlled multicenter study |
174 | Significant change in laxity 43.5% active gp v/s 19.6% | None | |
| BIPOLAR RF | Women in 50s | 14 | 64% satisfied with results | None |
| MONOPOLAR RF |
Clark, J Cosm Laser Ther 2018 Prospective for aesthetic appearance |
19 | Improvement in vulvar appearance and sexual function | None |
|
Lalji and Lozanova, J Cosmet Dermatol 2017 Mild/moderate SUI & vaginal laxity |
27 | Improvement in all evaluated areas of SUI and vaginal laxity | None |
CMRF, cryogen-cooled monopolar radiofrequency; FSFI, Female Sexual Function Index; GSM, genitourinary symptoms of menopause; ICIQ, International Consultation on Incontinence Questionnaire; RCT, randomized control trial; RF, radiofrequency; SSQ, Sexual Satisfaction Questionnaire; SUI, stress urinary incontinence; TTCRF, transcutaneous temperature controlled radiofrequency; UI, urinary incontinence; VAS, visual analogue scale; VHI, vaginal health index
Fig.
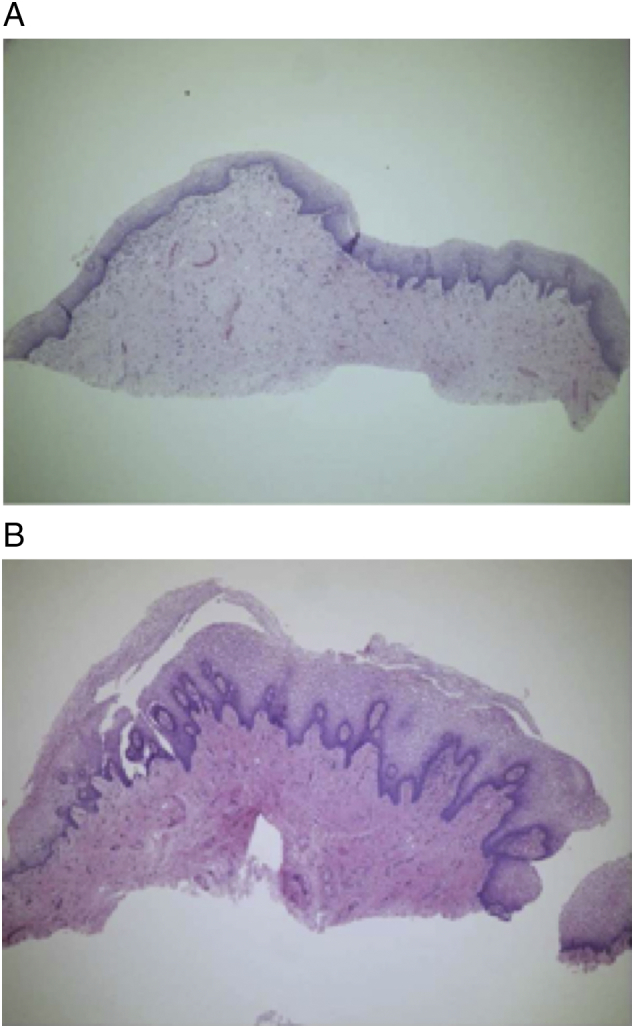
Vaginal mucosa (A) before and (B) 6 months after one treatment with the radiofrequency device ThermiVA (Thermiaesthetics, Irving, TX)
Additional clinical effects of energy-based devices include the increase of glycogen content, as documented by histopathology (Tadir et al., 2017). Energy-based vaginal rejuvenation procedures are appealing because they are noninvasive lunchtime procedures, with an average treatment time of 8 to 30 minutes depending on the indications and the method used (Table 4). The procedure is usually painless, and no anesthesia is required. Two or three sittings are advocated, spaced approximately 1 month apart. A touch-up sitting or repeat single session is done after 12 to 18 months.
Table 4.
Comparison of energy-based devices
| RF devices |
Lasers |
|||
|---|---|---|---|---|
| Monopolar | Bipolar and other RFs | CO2 | Erb:YAG | |
| Size and portability | Portable | Usually nonportable | Large and nonportable | Large and nonportable |
| Hand pieces | Disposable, small ergonomic wand | Barrel-shaped hand pieces for vagina, or small introital hand pieces | Larger, barrel-shaped hand pieces with disposable sleeves that are attached to an articular arm | Larger, barrel-shaped hand pieces with disposable sleeves that are attached to an articular arm |
| Depth of penetration | 4 mm | 0.5 mm | 0.6 mm | 0.2–0.5 mm |
| Procedure room | Outpatient room | Designated procedure room | Special room with laser-specific regulation required | Special room with laser-specific regulation required |
| Safety | No special safety gear required | No special safety gear required | User-laser protection glasses, etc | User-laser protection glasses, etc |
| Frequency of sittings | 3–4 sittings at monthly intervals | 4–6 sittings at 2–3 week intervals (bipolar), 3 sittings, each a week apart (multipolar), single Rx (patented), 2–4 times every 2–4 weeks (focused) | 3–4 sittings @ 4–6 week intervals | Protocols are different for different machines: 2 Rx at 8 weeks (Intimalaser) 3 Rx at 2 weeks (Petit Lady) |
| Anesthesia | No anesthesia | No | No | No |
| Time taken | 15–30 minutes | 10–20 minutes | 8–20 minutes | 8–20 minutes |
| Downtime | None | None | Sexual intimacy after 3 days | Sexual intimacy after 3 days |
| Pain | No pain | Introital area may be painful with pre-heated rings | Pain near introitus; hence, need to decrease energy in that area | Pain near introitus; hence, need to decrease energy in that area |
| Effects last for | 12 months | 12 months | 12 months | 12 months |
| Functional probe | Same probe can be used on vulva, in anal canal, or on the penile shaft | Separate probes for vagina and vulva | Separate probe used on vulva | Separate probe used on vulva |
| Skin lightening | ― | Separate probe for skin lightening | Separate probe for skin lightening | |
| Upgrade the machines | Newer machines with higher voltage; hence, quicker action | ― | Automated laser dispensers (robotic) arms make the procedure user independent and faster. Some machines are now adding an RF probe to work on the introital area | Robotic arms make the procedure user independent and faster. Some machines are now adding an RF probe to work on the introital area |
CO2, carbon dioxide; RF, radiofrequency; Rx, prescription
Energy-based procedures are well tolerated by most patients because they are either totally pain-free or cause slight discomfort. There is no downtime, and usual daily activities can be immediately resumed (except for sexual activity in laser treatments, after which 3 days of abstinence is recommended). Patients who benefit the most from energy-based procedures are those who have symptoms of mild-to-moderate SUI, overactive bladder, vaginal dryness, decreased lubrication, orgasmic dysfunction, grade 1 prolapse, and vaginal laxity. The indications are ever increasing, but more studies are required to evaluate the true breadth of the efficacy of energy-based devices.
In 2013, the North American Menopause Society validated energy-based devices; the society passed a position statement acknowledging that the use of lasers appeared to be an emerging therapy and may provide clinicians with other options to treat common and distressing problems of GSM (Alinsod, 2016; Gaspar et al., 2017, Leibaschoff et al., 2016, Tadir et al., 2017).
Other noninvasive modalities for vaginal rejuvenation involve the use of injectable volumizers, such as hyaluronic acid, PRP, and physical devices (e.g., Gore-Mycromesh and silicone threads). Aside from addressing laxity in the canal and dryness, some of these techniques specifically enhance the female sexuality center (e.g., amplify the G-spot).
Lipo-filling
A minimally invasive technique of vulvovaginal lipo-filling of the posterior vaginal wall was performed by Aguilar et al. in 2016. They also injected hyaluronic acid and PRP subcutaneously in the perineum (Aguilar et al., 2016).
Gore-mycromesh
In 2015, Park et al. did a study using a biocompatible compound (expanded poly-tetrafluoroethylene) as a Gore-Mycromesh on 50 women. They inserted, under local anesthesia, a 2 × 4 cm2 mesh under the posterior wall submucosa. The results showed a substantial improvement in sexual function in a year, especially for FSFI rates of satisfaction (Park and Whang, 2015).
Silicone threads
Park et al. performed a study among 180 women by inserting silicone threads under the vaginal submucosa (Park et al., 2015). They made incisions at the 3 and 9 o’clock positions and found that the FSFI significantly improved, especially for orgasms. Of their patients, 92.8% were satisfied with the vaginal width correction. Complications included implant exposure (5%), capsule contracture (3.9%), and infection (1.7%).
G-spot amplification
This procedure, which was empirically developed, makes the G spot more prominent and, hence, increases friction, which leads to better chances of vaginal orgasm. Bulking the sensitive area forward toward the vaginal lumen for greater frictional contact may lead to easier, longer, more frequent and intense orgasms. The G-spot was first described by Gräfenberg (Gräfenberg, 1950) and named by Perry and Whipple (Perry and Whipple, 1981). It is located below or inferior to the urethra, midway between the pubic bone and cervix, and is believed to be responsible for vaginal-mediated orgasms. Methods of amplification include nonpermanent fillers (e.g., hyaluronic acid) as patented by Dr. David Matlock (called the G-shot), PRP, and collagen injections. The results of the G-shot may last 3 to 5 months, but the procedure is limited by a lack of randomized controlled data.
Combination treatments
Combination treatments have increasingly been adopted for the comprehensive care of patients with esthetic and medical concerns. For vaginal rejuvenation, commonly proposed combination treatments include energy-based devices with PRP, energy-based devices after surgery, energy-based devices and fillers, and a combination of energy-based devices.
Energy-based devices with platelet-rich plasma
PRP is the most common rejuvenating injectable used in various parts of the body. Patients’ venous blood is collected in special tubes and centrifuged to obtain a supernatant of PRP. PRP acts by being very rich in and promoting growth factors with a fibrin scaffolding. PRP has been combined with energy-based devices as follows: 1) PRP is applied after microablative lasers as a rejuvenating liquid in the vagina; and 2) PRP is injected in the clitoro-urethro-vaginal space for better orgasms and better urinary control for stress urinary incontinence after use of energy-based devices (e.g., the O Shot, as patented by Runnels [Runels et al., 2014]).
Energy-based devices after surgery
With surgical vaginal tightening, the tissues are cut and resutured in layers with support that leads to structural and physical tightening. However, because energy-based devices improve the functionality of tissues, they can be offered to patients after a surgical vaginoplasty to improve elasticity and vaginal mucosa. Energy-based devices help improve symptoms of dyspareunia and lack of lubrication that are noted after surgery.
Energy-based devices and fillers
G-spot amplification can be done in combination with the third treatment of energy-based devices for vaginal orgasms.
Combination of energy-based devices
Some clinicians combine a laser device with RF and use laser in the vaginal canal and RF for the introital area and the vulva. This has prompted certain laser companies to add a separate RF device for use on the introital area.
Position of leading medical bodies
There is no federal or state legislation that currently prohibits or limits FCGS in the United States (Clinch et al., 2011). Despite the excitement of the medical and patient community about procedures to improve vaginal conditions and appearance and/or sexual health, several organizations have expressed concerns about the efficacy and safety of these procedures. Coupled with the paucity of peer-reviewed clinical trials, health care providers must tread the waters lightly so as not to run into medicolegal issues. We outlined the positions of the leading medical bodies.
American College of Obstetricians and Gynecologists
The American College of Obstetricians and Gynecologists Committee Opinion (2007, reaffirmed in 2017), indicated that FCGS is not medically indicated, and the safety and effectiveness of such procedures have not been documented. Women who ask for such procedures should be informed about the lack of data supporting their efficacy and about their potential complications, including infections, altered sensations, dyspareunia, scarring, and adhesions (American College of Obstetricians and Gynecologists, 2007).
Royal College of Obstetricians and Gynecologists
The Royal College of Obstetricians and Gynecologists stated in 2013 that “Presenting FCGS procedures as an unproblematic lifestyle choice is inappropriate” (Royal College of Obstetricians and Gynecologists, 2013).
Royal Australian and New Zealand College of Obstetricians and Gynecologists, and Society of Obstetricians and Gynecologists of Canada
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists Society of Obstetricians and Gynaecologists of Canada holds a public stand against FCGS (The Royal Australian and New Zealand College of Obstetricians and Gynaecologists RANZCOG College Statement: C-Gyn 24, 2015, Shaw et al., 2013).
U.S. Food and Drug Administration
The U.S. Food and Drug Administration recently issued a stern warning (US Food and Drug Administration, 2018) about procedures that destroy or reshape vaginal tissue using lasers or other energy-based devices, such as RF. The warning elaborates that "the full extent of the risks is unknown. But these reports indicate these procedures can cause serious harm." The U.S. Food and Drug Administration warning does not include sufficient data to address safety or efficacy, but it underscores the need for more thorough and long-term studies to be conducted.
Ongoing clinical trials
Large, blinded, randomized control trials are required to establish appropriate indications, effects, and complications for energy-based devices. Several ongoing multicenter trials use fractional CO2 lasers in GSM, often comparing their efficacy with that of a topical estrogen preparation (Cruz et al., 2018). The Vaginal Erbium Laser Academy Study for GSM and SUI is an international, multicenter trial, and the ThermiVa in Genital Hiatus Treatment trial is a multicenter Australian trial that investigates whether transcutaneous, temperature-controlled RF is an effective treatment for vaginal laxity (Dilgir, 2017).
Conclusions
Energy-based devices undoubtedly show great promise for the functional and esthetic issues of women’s intimate areas, especially vaginal rejuvenation. Larger, double-blinded, randomized control trials are required to draw definitive conclusions, including accepting these devices as standard, preventive, or first-line treatments.
Footnotes
Conflicts of interest: None.
For patient information on skin cancer in women, please click on Supplemental Material to bring you to the Patient Page. Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijwd.2019.02.003.
Appendix A. Supplementary data
Supplementary material
References
- Abedi P., Jamali S., Tadayon M., Parhizkar S., Mogharab F. Effectiveness of selective vaginal tightening on sexual function among reproductive aged women in Iran with vaginal laxity: A quasi-experimental study. J Obstet Gynaecol Res. 2014;40(2):526–531. doi: 10.1111/jog.12195. [DOI] [PubMed] [Google Scholar]
- Adrian G. Comparison of two novel laser treatments in aesthetic gynecology. J Laser Health Acad. 2012;1:S10. [Google Scholar]
- Aguilar P., Hersant B., SidAhmed-Mezi M., Bosc R., Vidal L., Meningaud J.P. Novel technique of vulvo-vaginal rejuvenation by lipofilling and injection of combined platelet-rich-plasma and hyaluronic acid: A case-report. Springerplus. 2016;5(1):1184. doi: 10.1186/s40064-016-2840-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alinsod R.M. Temperature controlled radiofrequency for vulvovaginal laxity [Internet] 2015. https://www.prime-journal.com/temperature-controlled-radiofrequency-for-vulvovaginal-laxity/ [cited 2019]. Available from:
- Alinsod R.M. Transcutaneous temperature controlled radiofrequency for orgasmic dysfunction. Lasers Surg Med. 2016;48(7):641–645. doi: 10.1002/lsm.22537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College of Obstetricians and Gynecologists Committee on Practice Bulletins-Gynecology. Practice Bulletin No. 119: Female sexual dysfunction. Obstet Gynecol. 2011;117(4):996–1007. doi: 10.1097/AOG.0b013e31821921ce. [DOI] [PubMed] [Google Scholar]
- Avery K., Donovan J., Peters T.J., Shaw C., Gotoh M., Abrams P. ICIQ: A brief and robust measure for evaluating the symptoms and impact of urinary incontinence. Neurourol Urodyn. 2004;23(4):322–330. doi: 10.1002/nau.20041. [DOI] [PubMed] [Google Scholar]
- Bachmann G. Urogenital ageing: An old problem newly recognized. Maturitas. 1995;22(s):s1–s5. doi: 10.1016/0378-5122(95)00956-6. [DOI] [PubMed] [Google Scholar]
- Barbara G., Facchin F., Buggio L., Alberico D., Frattaruolo M.P., Kustermann A. Vaginal rejuvenation: Current perspectives. Int J Women's Health. 2017;9:513–519. doi: 10.2147/IJWH.S99700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark Z. Labial tissue rejuvenation and sexual function improvement using a novel noninvasive focused monopolar radio frequency device. J Cosmet Laser Ther. 2018;20(2):66–70. doi: 10.1080/14764172.2017.1368565. [DOI] [PubMed] [Google Scholar]
- Clinch N.C., Osland A., Wang C. Legitimizing radical new medical services. J Appl Bus Econ. 2011;12(4):64–77. [Google Scholar]
- Committee on Gynecologic Practice, American College of Obstetricians and Gynecologists Committee Opinion No 378: Vaginal rejuvenation and cosmetic vaginal procedures. Obstet Gynecol. 2007;110(3):737–738. doi: 10.1097/01.AOG.0000263927.82639.9b. [DOI] [PubMed] [Google Scholar]
- Cruz V.L., Steiner M.L., Pompei L.M., Strufaldi R., Fonseca F.L.A., Santiago L.H.S. Randomized, double-blind, placebo-controlled clinical trial for evaluating the efficacy of fractional CO2 laser compared with topical estriol in the treatment of vaginal atrophy in postmenopausal women. Menopause. 2018;25(1):21–28. doi: 10.1097/GME.0000000000000955. [DOI] [PubMed] [Google Scholar]
- Davis D., Shaver P.R., Widaman K.F., Vernon M.L., Follette W.C., Beitz K. I can’t get no satisfaction: Insecure attachment, inhibited sexual communication, and sexual dissatisfaction. Pers Relatsh. 2006;13(4):465–483. [Google Scholar]
- Desai S.A., Dixit V.V. Audit of female genital aesthetic surgery: Changing trends in India. J Obstet Gynaecol India. 2018;68(3):214–220. doi: 10.1007/s13224-018-1115-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilgir S. The effectiveness of Thermiva monopolar radiofrequency device in treating symptoms of vaginal laxity in women who have had vaginal births [Internet] 2017. https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=373707 [cited xxx]. Available from:
- Dillon B., Dmochowski R. Radiofrequency for the treatment of stress urinary incontinence in women. Curr Urol Rep. 2009;10(5):369–374. doi: 10.1007/s11934-009-0058-z. [DOI] [PubMed] [Google Scholar]
- Filippini M., Del Duca E., Negosanti F., Bonciani D., Negosanti L., Sannino M. Fractional CO2 laser: From skin rejuvenation to vulvo-vaginal reshaping. Photomed Laser Surg. 2017;35(3):171–175. doi: 10.1089/pho.2016.4173. [DOI] [PubMed] [Google Scholar]
- Gambacciani M., Levancini M., Cervigni M. Vaginal erbium laser: The second-generation thermotherapy for the genitourinary syndrome of menopause. Climacteric. 2015;18(5):757–763. doi: 10.3109/13697137.2015.1045485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gambacciani M., Torelli M.G., Martella L., Bracco G.L., Casagrande A.G., Albertin E. Rationale and design for the Vaginal Erbium Laser Academy Study (VELAS): An international multicenter observational study on genitourinary syndrome of menopause and stress urinary incontinence. Climacteric. 2015;18(Suppl. 1):43–48. doi: 10.3109/13697137.2015.1071608. [DOI] [PubMed] [Google Scholar]
- Gaspar A., Addamo G., Brandi H. Vaginal fractional CO2 laser: A minimally invasive option for vaginal rejuvenation. Am J Cosmet Surg. 2011;28(3):156–162. [Google Scholar]
- Gaspar A., Brandi H., Gomez V., Luque D. Efficacy of Erbium:YAG laser treatment compared to topical estriol treatment for symptoms of genitourinary syndrome of menopause. Lasers Surg Med. 2017;49(2):160–168. doi: 10.1002/lsm.22569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gold M., Andriessen A., Bader A., Alinsod R., French E.S., Guerette N. Review and clinical experience exploring evidence, clinical efficacy, and safety regarding nonsurgical treatment of feminine rejuvenation. J Cosmet Dermatol. 2018;17(3):289–297. doi: 10.1111/jocd.12524. [DOI] [PubMed] [Google Scholar]
- Goodman M.P., Placik O.J., Benson R.H., 3rd, Miklos J.R., Moore R.D., Jason R.A. A large multicenter outcome study of female genital plastic surgery. J Sex Med. 2010;7(4 Pt 1):1565–1577. doi: 10.1111/j.1743-6109.2009.01573.x. [DOI] [PubMed] [Google Scholar]
- Gräfenberg E. The role of urethra in female orgasm. Int J Sexol. 1950;3:145–148. [Google Scholar]
- Karcher C., Sadick N. Vaginal rejuvenation using energy-based devices. Int J Womens Dermatol. 2016;2(3):85–88. doi: 10.1016/j.ijwd.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krychman M., Rowan C.G., Allan B.B., DeRogatis L., Durbin S., Yacoubian A. Effect of single-treatment, surface-cooled radiofrequency therapy on vaginal laxity and female sexual function: The VIVEVE I randomized controlled trial. J Sex Med. 2017;14(2):215–225. doi: 10.1016/j.jsxm.2016.11.322. [DOI] [PubMed] [Google Scholar]
- Lalji S., Lozanova P. Evaluation of the safety and efficacy of a monopolar nonablative radiofrequency device for the improvement of vulvo-vaginal laxity and urinary incontinence. J Cosmet Dermatol. 2017;16(2):230–234. doi: 10.1111/jocd.12348. [DOI] [PubMed] [Google Scholar]
- Leibaschoff G., Izasa P.G., Cardona J.L., Miklos J.R., Moore R.D. Transcutaneous temperature controlled radiofrequency (TTCRF) for the treatment of menopausal vaginal/genitourinary symptoms. Surg Technol Int. 2016;29:149–159. [PubMed] [Google Scholar]
- Lowenstein L., Salonia A., Shechter A., Porst H., Burri A., Reisman Y. Physicians' attitude toward female genital plastic surgery: A multinational survey. J Sex Med. 2014;11:33–39. doi: 10.1111/jsm.12254. [DOI] [PubMed] [Google Scholar]
- Lukaez E.S., Lawrence J.M., Burchette R.J., Luber K.M., Nager C.W., Buckwalter J.G. The use of visual analog scale in urogynaecologic research: A psychometric evaluation. Am J Obstet Gynecol. 2004;191:165–170. doi: 10.1016/j.ajog.2004.04.047. [DOI] [PubMed] [Google Scholar]
- Millheiser L.S., Pauls R.N., Herbst S.J., Chen B.H. Radiofrequency treatment of vaginal laxity after vaginal delivery: Non-surgical vaginal tightening. J Sex Med. 2010;7(9):3088–3095. doi: 10.1111/j.1743-6109.2010.01910.x. [DOI] [PubMed] [Google Scholar]
- Ostrzenski A. Vaginal rugation rejuvenation (restoration): A new surgical technique for an acquired sensation of wide/smooth vagina. Gynecol Obstet Investig. 2012;73(1):48–52. doi: 10.1159/000329338. [DOI] [PubMed] [Google Scholar]
- Pardo J.S., Sola V.D., Ricci P.A., Guiloff E.F., Freundlich O.K. Colpoperineoplasty in women with a sensation of a wide vagina. Acta Obstet Gynecol Scand. 2006;85(9):1125–1127. doi: 10.1080/00016340600622544. [DOI] [PubMed] [Google Scholar]
- Park T.H., Whang K.W. Vaginal rejuvenation with Gore-Mycromesh. Aesthet Plast Surg. 2015;39(4):491–494. doi: 10.1007/s00266-015-0502-z. [DOI] [PubMed] [Google Scholar]
- Park T.H., Park H.J., Whang K.W. Functional vaginal rejuvenation with elastic silicone threads: A 4-year experience with 180 patients. J Plast Surg Hand Surg. 2015;49(1):36–39. doi: 10.3109/2000656X.2014.944187. [DOI] [PubMed] [Google Scholar]
- Pauls R.N., Fellner A.N., Davila G.W. Vaginal laxity: A poorly understood quality of life problem; a survey of physician members of the International Urogynecological Association (IUGA) Int Urogynecol J. 2012;23(10):1435–1448. doi: 10.1007/s00192-012-1757-4. [DOI] [PubMed] [Google Scholar]
- Perino A., Calligaro A., Forlani F., Tiberio C., Cucinella G.A. SvelatoA, et al. Vulvo-vaginal atrophy: A new treatment modality using thermo-ablative fractional CO2 laser. Maturitas. 2015;80(3):296–301. doi: 10.1016/j.maturitas.2014.12.006. [DOI] [PubMed] [Google Scholar]
- Perry J.D., Whipple B. Pelvic muscle strength of female ejaculations: Evidence in support of a new theory of orgasm. J Sex Res. 1981;17:22–39. [Google Scholar]
- Pieralli A., Fallani M.G., Becorpi A., Bianchi C., Corioni S., Longinotti M. Fractional CO2 laser for vulvovaginal atrophy (VVA) dyspareunia relief in breast cancer survivors. Arch Gynecol Obstet. 2016;294(4):841–846. doi: 10.1007/s00404-016-4118-6. [DOI] [PubMed] [Google Scholar]
- Qureshi A.A., Tenenbaum M.M., Myckatyn T.M. Nonsurgical vulvovaginal rejuvenation with radiofrequency and laser devices: A literature review and comprehensive update for aesthetic surgeons. Aesthet Surg J. 2018;38(3):302–311. doi: 10.1093/asj/sjx138. [DOI] [PubMed] [Google Scholar]
- Rosen R., Brown C., Heiman J., Leiblum S., Meston C., Shabsigh R. The Female Sexual Function Index: A multidimensional self-report instrument for the assessment of female sexual function. J Sex Marital Ther. 2000;26(2):191–208. doi: 10.1080/009262300278597. [DOI] [PubMed] [Google Scholar]
- Royal College of Obstetricians and Gynaecologists Ethical considerations in relation to female genital cosmetic surgery (FGCS) RCOG Ethics Committee [Internet] 2013. https://www.rcog.org.uk/globalassets/documents/guidelines/ethics-issues-and-resources/rcog-fgcs-ethical-opinion-paper.pdf [cited 20 December 2018]. Available from:
- Runels C., Melnick H., Debourbon E., Roy L. A pilot study of the effect of localized injections of autologous Platelet Rich Plasma (PRP) for the treatment of sexual dysfunction. J Women’s Health Care. 2014;3:169. [Google Scholar]
- Sadick N.S., Malerich S.A., Nassar A.H., Dorizas A.S. Radiofrequency: An update on latest innovations. J Drugs Dermatol. 2014;13(11):1331–1335. [PubMed] [Google Scholar]
- Salvatore S., Nappi R.E., Parma M., Chionna R., Lagona F., Zerbinati N. Sexual function after fractional microablative CO(2) laser in women with vulvovaginal atrophy. Climacteric. 2015;18(2):219–225. doi: 10.3109/13697137.2014.975197. [DOI] [PubMed] [Google Scholar]
- Sekiguchi Y., Utsugisawa Y., Azekosi Y., Kinjo M., Song M., Kubota Y. Laxity of the vaginal introitus after childbirth: Nonsurgical outpatient procedure for vaginal tissue restoration and improved sexual satisfaction using low-energy radiofrequency thermal therapy. J Women's Health (Larchmt) 2013;22(9):775–781. doi: 10.1089/jwh.2012.4123. [DOI] [PubMed] [Google Scholar]
- Shaw D., Lefebvre G., Bouchard C., Shapiro J., Blake J., Allen L. Female genital cosmetic surgery. J Obstet Gynaecol. 2013;35(12):1108–1112. doi: 10.1016/S1701-2163(15)30762-3. [DOI] [PubMed] [Google Scholar]
- Sullivan G.M., Artino A.R., Jr. Analyzing and interpreting data from Likert-type scales. J Grad Med Edu. 2013;5(4):541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tadir Y., Gaspar A., Lev-Sagie A., Alexiades M., Alinsod R., Bader A. Light and energy based therapeutics for genitourinary syndrome of menopause: consensus and controversies. Lasers Surg Med. 2017;49(2):137–159. doi: 10.1002/lsm.22637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Royal Australian and New Zealand College of Obstetricians and Gynaecologists RANZCOG College Statement: C-Gyn 24 Vaginal rejuvenation, laser ablation for benign conditions and cosmetic vaginal procedures [Internet] 2015. https://www.ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/Women%27s%20Health/Statement%20and%20guidelines/Clinical%20-%20Gynaecology/Vaginal-rejuvenation,-laser-and-cosmetic-procedures-(C-Gyn-24)-Amended-July-2016.pdf?ext=.pdf [cited 20 December 2018]. Available from:
- U.S. Food and Drug Administration FDA warns against use of energy-based devices to perform vaginal rejuvenation or vaginal cosmetic procedures: FDA safety communication [Internet] 2018. https://www.fda.gov/medicaldevices/safety/alertsandnotices/ucm615013.htm [cited 20 December 2018]. Available from:
- Vizintin Z., Lukac M., Kazic M., Tettamanti M. Erbium laser in gynecology. Climacteric. 2015;18(Suppl. 1):4–8. doi: 10.3109/13697137.2015.1078668. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material



