Abstract
Our propose is to evaluate CT-guided biopsies in suspected spondylodiscitis with respect to puncture site, microbiology findings, histopathology findings and impact on antibiotic therapy. 86 CT-guided spine interventions in suspected spondylodiscitis comprising 201 biopsy procedures were analyzed. Medical records of all patients were screened for microbiology and histopathology reports as well as date, duration and kind of antibiotic therapy. Statistical analyses included calculation of Chi2-tests and logistic regression analyses. Locations of biopsies were intervertebral disc (48.3%), paravertebral soft-tissue (38.3%) and vertebral body (10.9%). Positive microbiological findings were found altogether in 33.8% of cases, positive histopathological findings in 53.6%. Significant associations between positive microbiological findings, positive histopathological findings and antibiotic therapy, respectively, were found. Location of biopsies did not significantly influence rate of positive findings. From the variables age, white blood cell count, serum creatinine and puncture site, none were found to be an independent predictor for a positive microbiological result. We concluded that CT-guided biopsy of intervertebral disc and paravertebral soft tissue yields positive microbiologic findings in a significant proportion of cases. Puncture site is not associated with positive results of microbiology or histopathology.
Key words: spondylodiscitis, CT guided biopsy, microbiology
Introduction
Infectious spondylodiscitis is a relatively rare disease with an estimated incidence of about 0.4 to 2.4. per 100.000 in Europe.1 Over the past years an increasing incidence has been described,2 which might be attributable to earlier and more sensitive diagnostic procedures as well as a rising proportion of immunocompromised patients in hospitals.3-5 Early diagnosis and treatment are mandatory, as the disease might be lethal in up to 17% of cases.6 Germ isolation in clinically suspected spondylodiscitis is important, as a specific antibiotic treatment based upon the antibiogram becomes possible. Ways to obtain material in order to isolate causative agents of spondylodiscitis include blood cultures, CT-guided biopsies and open surgical biopsy procedures.5,6 In patients with negative blood-cultures, CT-guided biopsy might be able to isolate causative agents of spondylodiscitis.7 The rate of positive microbiological and/or histopathological findings varies considerably in the literature. Definitive factors that might influence or predict a positive microbiological or histopathological finding are not consistently reported.7,8 The goal of our retrospective study was to evaluate a series of CT-guided biopsies in suspected spondylodiscitis in order to document rates of positive microbiological or histopathological findings in correlation to the site of CT-guided biopsy (i.e. intervertebral disc or paravertebral soft tissue) and to identify possible factors that might predict a positive microbiological result.
Materials and Methods
This retrospective study was approved by the local ethics board of our university hospital (No. 16-6866-BO).
Data acquisition
Intra-departmental review of all spine interventions from the year 2002 until 2016 was accomplished by using the radiology information system (RIS), picture archiving and communication system (PACS) and hospital information system. Furthermore, non-digitalized data was collected by sighting written patients records. All images from selected patients were reviewed by experienced radiologists. Microbiological data and histopathological data from CT-guided interventions were collected by screening of all written patient records and digital records saved in the hospital information system. Literature research was carried out with Pubmed™ and Google Scholar™.
Data editing
Data editing and preparation was accomplished by using Microsoft Excel™ comprising information about patient’s age at the time of CT guided intervention, referring department, anatomical localization of suspected spondylodiscitis, anatomical localization of puncture site, number of single biopsy procedures, size of puncture needles, post interventional complications, results of microbiological and histopathological examination, antibiotic therapy and ongoing antibiotic therapy after discharge.
Technique of CT-guided interventions
CT-guided interventions were performed under sterile conditions and under local anesthesia on multi-detector CTs of different generations. Always, co-axial technique for puncture was used with needle sizes of 16 or 18 gauge. The acquired material was sent to the departments of Microbiology and Pathology for further examination. Figures 1 and 2 illustrate CT guided biopsies from the paravertebral soft tissue and intervertebral disc.
Figure 1.
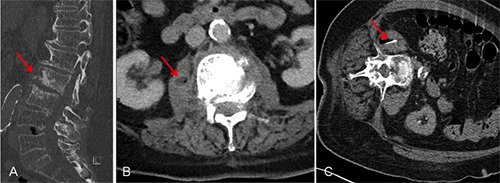
Computed tomography (CT) guided biopsy of paravertebral soft tissue in a patient with clinical and radiological signs of spondylodiscitis. A) Sagittal reformatted computed tomography in bone window illustrating partially destroyed and eroded vertebral bodies at lumbar segment 2 and 3 (arrow). B) Computed tomography in axial direction showing fluid collection with entrapped air in the right iliopsoas muscle (arrow). C) Tip of the biopsy needle (arrow) located in the paravertebral soft tissue (right ilipsoas muscle).
Statistical analysis
All statistical analyses were performed by using IBM Statistical Package for Social Science (SPSS) Version 23.0™. Testing for concordance between microbiological and histopathological results as well as between microbiological, histopathological results and antibiotic therapy was calculated with Chi-Square tests. Data of microbiological, histopathological results and antibiotic therapy were encoded as follows:
M1 = positive microbiological result
M0 = negative microbiological result
P1 = positive histopathological result
P0 = negative histopathological result
A1 = antibiotic therapy
A0 = no antibiotic therapy
Chi-Square testes were employed to test whether rates of positive microbiological and histopathological findings differed between different puncture sites.
Binary logistic regression analysis was calculated to identify possible predictive variables for a positive microbiological result. Variables included for analysis were: patient´s age at the time of biopsy, white blood cell count, serum creatinine and site of biopsy (i.e. paravertebral soft tissue or intervertebral disc).
Results
From 2002 until 2016, 380 spine interventions were performed in our institution. From these, 86 spine interventions in suspected spondylodiscitis were accomplished comprising 201 single biopsy procedures.
Patients
Altogether 78 patients (44 male, 34 female) with clinical and radiological signs of suspected spondylodiscitis were examined. Median patient age was 69.5 years with a range from 14 to 86 years (Table 1). Main referring departments were Neurosurgery and Orthopedic Surgery.
Table 1.
Demographic data and information about number of computed tomography (CT)-guided biopsies in suspected spondylodiscitis (time period of analyzed CT-guided interventions: from 2002.03.22 to 2016.02.15).
| Demographic data | N. |
|---|---|
| CT-guided interventions | 86 |
| Single biopsy procedures | 201 |
| Examined patients | 78 |
| Male | 44 |
| Female | 34 |
| Age range of patients, years | 14-86 |
| Median age | 69.5 |
| Mean age | 63.8 |
Main anatomical regions for CT guided biopsies were the lumbar spine (60.5%) and thoracic spine (27.9%). The main puncture sites at the particular anatomical regions were intervertebral disc (48.3%), paravertebral soft tissue (38.3%) and vertebral body (10.9%) (Figures 3-5).
Diagnostic yields of CT guided biopsies
Altogether 77 microbiological examinations were conducted. A positive microbiological result was obtained in 33.8% of all cases, with Staphylococcus aureus (34.6%) and Staphylococcus epidermis (23.1%) as most frequent isolated germs. Altogether 56 histopathological examinations were accomplished. A positive histopathological result with signs of inflammation was reported in 53.6%.
Testing for concordance between histopathological and microbiological findings revealed a significant but imperfect concordance (c2=6.267, P=0.012 and j=0.38).
In case of a positive microbiological result, histopathology was almost always positive as well, whereas in case of a positive histopathological finding, microbiology was positive in less than 50%.
Regarding positive histopathological results with respect to the puncture site (i.e. biopsy from the intervertebral disc vs. biopsy from paravertebral soft tissue), no significant differences could be found (c2=2.185 with P=0.138).
Impact of results from CT guided biopsy on antibiotic treatment
There was a significant concordance between positive microbiological results and antibiotic treatment, with c2=5.927 (P=0.015) and between positive histopathological result and antibiotic treatment (c2=4.056, P=0.044). These results suggest that decision for antibiotic treatment was positively influenced by the results from microbiological and histopathological analysis.
In case of a positive microbiological result from CT guided intervention, 88% of patients were treated according to the respective antibiogram.
Binary logistic regression analysis
In order to test the predictive value of different clinical variables for a positive result of microbiological analysis, we performed a binary logistic regression analysis including age, WBC, serum creatinine and site of biopsy as covariates. None of the variables provided a significant predictive value.
Discussion
Infectious spondylodiscitis is a relevant entity in clinical practice with a rising incidence in recent years.3 Isolation of the causative agent and generation of antibiograms are requirements for targeted antibiotic therapies in infectious spondylodicitis.6
In our study, we documented positive microbiological findings with isolation of the pathogenic germs in 33.8%. This result is in line with published data. For example, Rehm et al.9 showed 25% positive microbiological results in their study, which comprised altogether 86 microbiological examinations in 214 patients. Other studies report 29.4%,10 38.5%,11 36%12 and 28.4%13 positive microbiological results. In a further analysis, we investigated whether the site of the CT-guided biopsy (i.e. intervertebral disc or paravertebral soft tissue) might influence the rate of positive microbiological results. Our results demonstrate no significant difference of positive microbiological results regarding biopsy site. This result is reflected by a study of Chang et al.,14 who investigated 102 patients undergoing 122 biopsy procedures in suspected spondylodiscitis. They analyzed rates of positive microbiology results in biopsies from intervertebral discs, paravertebral soft tissue and the junction of intervertebral disc and vertebral body endplate and also found no significant differences between the different biopsy locations. Therefore, in terms of a practical guideline, biopsy specimen might be sufficient if acquired from paravertebral soft tissue, especially if targeting of intervertebral discs turns out to be technically challenging or impossible.
In addition to microbiology, we also analyzed histopathology reports of our study group. Our results demonstrate positive histopathological results in terms of verification of inflammation in 53.6% of all examined cases with suspected spondylodiscitis. Chi-Square tests proved significant concordance between microbiology and histopathology and also revealed that positive histopathological results also influenced further antibiotic treatment significantly. As already demonstrated by the microbiological results, there was also no significant coherence between location of the biopsy and positive histopathological results. Regarding the rate of positive histopathological findings in suspected spondylodiscitis, results are quite variable in the literature. Sehn et al.15 and Heyer et al.16 report of 55.8% and 74% of positive histopathological results in patients with suspected infectious spondylodiscitis, respectively, and Gasbarrini et al.11 had a comparable high rate of positive histopathological results with 69%. Corresponding to our results, also Sehn et al. and Heyer et al. did not find a significant influence of biopsy region on positive histopathological results. From a practical point of view, we recommend to always obtain specimen for pathological examination, as a positive histopathological report might influence further therapy significantly.
In order to identify possible independent variables for the prediction of a positive microbiological result, we investigated four easily accessible clinical parameters: white blood cell count, serum creatinine, patient´s age and site of biopsy. As our results demonstrate, none of the tested parameters independently predicted a positive finding of microbiological analysis. Kasalak et al.1 analyzed different clinical, radiological and laboratory parameters including leucocytes and C-reactive protein in order to find differences between culture positive and culture negative CT biopsy specimen. None of their analyzed parameters was significantly different between both groups. Ahuja et al.,8 who performed a comprehensive outcome analysis of CT-guided biopsies in spondylodiscitis with a logistic regression analysis including CRP value, white blood cell count, presence of fever or neurological deficits found CRP to be the only independent variable for prediction of isolation of the causative organism with a threshold of 50 being more likely to have a positive result from CT biopsy.
One limitation of our study is the missing analysis of CRP, which has been proven to be a strong and independent predictor of a positive microbiological result. Due to the retrospective nature of our study and to some degree incomplete patient records, especially data of CRP from the early analysis period were missing.
Conclusions
In conclusion, site of biopsy in terms of paravertebral tissue or intervertebral disc had no influence on the rate of positive microbiological or histopathological outcome. Results of microbiology significantly influence further antibiotic treatment. In case of isolation of the causative agent, antibiotic therapy is selected in a high percentage according to the antibiogram.
Figure 2.
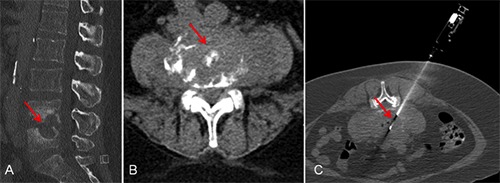
Computed tomography (CT) guided biopsy of intervertebral disc in a patient with clinical and radiological signs of spondylodiscitis at lumbar segment four and five. A) Sagittal reformatted computed tomography in bone window showing destruction of intervertebral disc and partially destroyed vertebral bodies (arrow). B) Transversal computed tomography illustrating gross inflammatory changes in lumbar segment 4/5 (arrow). C) Transversal computed tomography in bone window showing biopsy needle with co-axial technique targeting intervertebral disc (arrow).
Figure 3.
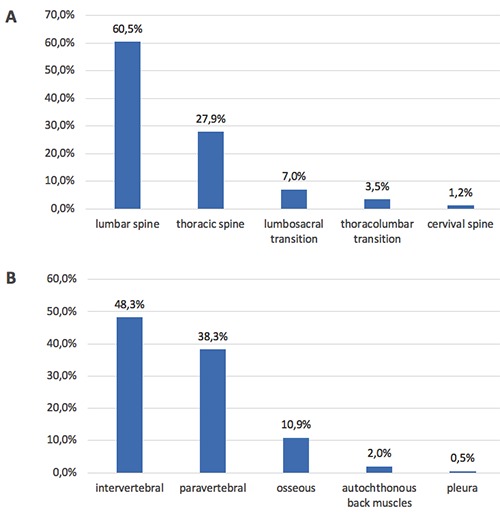
Graphical illustration of anatomical regions (A) and exact puncture sites (B) of CT-guided interventions. A) Location of puncture during CT-guided biopsies (height of vertebral column). B) Location of puncture during CT-guided biopsies (target tissue).
Figure 4.
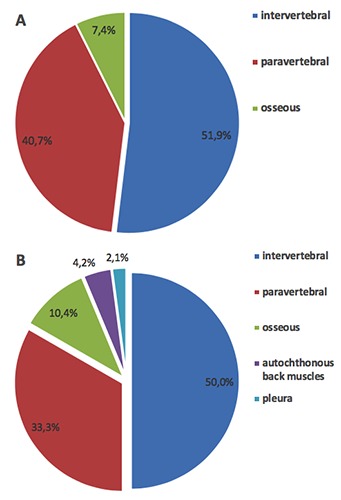
Graphical illustration of location of puncture sites and rates of positive (A) and negative (B) microbiological results. A) Location of puncture site of biopsies with positive microbiological findings. B) Location of puncture site of biopsies with negative microbiological findings.
Figure 5.
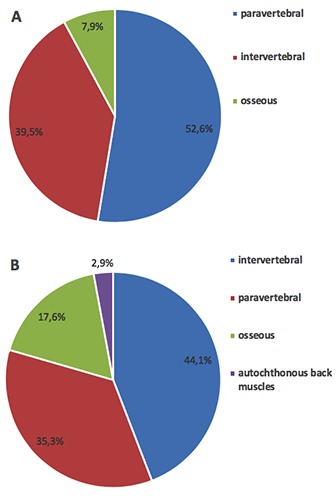
Graphical illustration of location of puncture sites and rates of positive (A) and negative (B) histopathological results. A) Location of puncture sites of biopsies with positive histopathological findings. B) Location of puncture sites of biopsies with negative histopathological findings.
Acknowledgements
Written histopathological results were provided in the digital hospital information system and patient charts by the Institute of Pathology of University Hospital Essen.
Funding Statement
Funding: none.
References
- 1.Kasalak O, Wouthuyzen-Bakker M, Adams HJA, et al. CT-guided biopsy in suspected spondylodiscitis: microbiological yield, impact on antimicrobial treatment, and relationship with outcome. Skeletal Radiol 2018;47:1383-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Frangen TM, Kälicke T, Gottwald M, et al. [Surgical management of spondylodiscitis. An analysis of 78 cases]. Unfallchirurg 2006;109:743-53. [in German] [DOI] [PubMed] [Google Scholar]
- 3.Herren C, Jung N, Pishnamaz M, et al. Spondylodiscitis: Diagnosis and Treatment Options. Dtsch Arztebl Int 2017;114:875-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cottle L, Riordan T. Infectious spondylodiscitis. J Infect 2008;56:401-12. [DOI] [PubMed] [Google Scholar]
- 5.Ahlhelm F, Kelm J, Naumann N, et al. [Spondylitis/spondylodiscitis]. Radiologe 2006;46:480-5. [in German]16609839 [Google Scholar]
- 6.Sobottke R, et al. Aktuelle Diagnostik und Therapie der Spondylodiszitis. Dtsch Arztebl 2008;105:181-7. [Google Scholar]
- 7.Czuczman GJ, Marrero DE, Huang AJ, et al. Diagnostic yield of repeat CT-guided biopsy for suspected infectious spondylodiscitis. Skeletal Radiol 2018;47:1403-10. [DOI] [PubMed] [Google Scholar]
- 8.Ahuja N, Sharma H. The effectiveness of computed tomography-guided biopsy for the diagnosis of spondylodiscitis: an analysis of variables affecting the outcome. Eur Rev Med Pharmacol Sci 2017;21:2021-6. [PubMed] [Google Scholar]
- 9.Rehm J, Veith S, Akbar M, et al. CT-Guided Percutaneous Spine Biopsy in Suspected Infection or Malignancy: A Study of 214 Patients. Rofo 2016;188: 1156-62. [DOI] [PubMed] [Google Scholar]
- 10.Spira D, Germann T, Lehner B, et al. CT-Guided Biopsy in Suspected Spondylodiscitis—The Association of Paravertebral Inflammation with Microbial Pathogen Detection. PLoS One 2016;11: e0146399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gasbarrini A, Boriani L, Salvadori C, et al. Biopsy for suspected spondylodiscitis. Eur Rev Med Pharmacol Sci 2012;16:26-34. [PubMed] [Google Scholar]
- 12.Enoch DA, Cargill JS, Laing R, et al. Value of CT-guided biopsy in the diagnosis of septic discitis. J Clin Pathol 2008;61:750-3. [DOI] [PubMed] [Google Scholar]
- 13.Foreman SC, Schwaiger BJ, Gempt J, et al. MR and CT Imaging to Optimize CT-Guided Biopsies in Suspected Spondylodiscitis. World Neurosurg 2017;99:726-34. [DOI] [PubMed] [Google Scholar]
- 14.Chang CY, Simeone FJ, Nelson SB, et al. Is Biopsying the Paravertebral Soft Tissue as Effective as Biopsying the Disk or Vertebral Endplate? 10-Year Retrospective Review of CT-Guided Biopsy of Diskitis-Osteomyelitis. AJR Am J Roentgenol 2015;205:123-9. [DOI] [PubMed] [Google Scholar]
- 15.Sehn JK, Gilula LA. Percutaneous needle biopsy in diagnosis and identification of causative organisms in cases of suspected vertebral osteomyelitis. Eur J Radiol 2012;81:940-6. [DOI] [PubMed] [Google Scholar]
- 16.Heyer CM, Al-Hadari A, Mueller KM, et al. Effectiveness of CT-guided percutaneous biopsies of the spine: an analysis of 202 examinations. Acad Radiol 2008;15:901-11. [DOI] [PubMed] [Google Scholar]


