Abstract
Background
The objective of the study was to assess the efficacy of a multi-component intervention to reduce kinesiology pre-professionals’ implicit and explicit bias.
Method
A pre-post experimental design, which consisted of an experimental group (n = 42) and a control group (n = 36), was conducted to assess the efficacy of the intervention using both implicit and explicit obesity bias measures.
Results
On the pre-test, participants did not display overall explicit bias on the Anti-Fat Attitudes Test (AFAT) but had strong implicit bias and bias on the lazy/motivated semantic differential scale. Participation in the intervention reduced explicit bias on the AFAT social character disparagement and weight control/blame subscales but not implicit bias.
Conclusion
Implicit bias remains difficult to change and appears to be deep-seated in individuals’ minds. Future interventions may need methods to make sure all participants process and connect emotionally to all information.
Key Words: Service learning, Obesity bias, Intervention, Physical activity barrier
Introduction
Obesity is an increasing problem both in terms of the individual health risks that people accrue and in the cost of maintaining public health [1]. In efforts to promote active healthy lifestyles and reduce barriers to exercise, public health initiatives commonly include physical activity-related components or interventions to increase the amount of activity individuals get per week. An often overlooked physical activity barrier is obesity bias. Obesity bias is falsely assuming that all overweight or obese individuals act consistent with negative overweight stereotypes (e.g. unattractive, lazy) [2]. Not only does the general public possess bias toward overweight and obese individuals, research has also documented that allied health [3, 4] and physical activity-related professionals [5] and pre-professionals [6, 7, 8, 9] are biased as well. Professionals that are not consciously aware of a societal weight stigmatization or their own biases may unknowingly dissuade individuals from living a healthy active lifestyle [10, 11]. Implementation of strategic intervention components during undergraduate education is necessary to make pre-professionals aware of obesity bias and its potential negative ramifications toward living a healthy lifestyle.
Obesity bias can be divided into two categories: explicit and implicit bias [2]. Explicit bias is a negative conscious evaluation of the overweight, commonly measured using self-report measures such as questionnaires. On the other hand, implicit bias is the unconscious cognitions that is operating without individuals’ knowledge [12, 13]. Implicit bias is deeply engrained in ones’ minds and behaviorally manifested when critical environmental cues activate them, such as when individuals unknowingly fail to hold a door open for an overweight individual. Implicit bias is commonly measured using timed reaction time tests (e.g. Implicit Association Tests). In the literature, there has been a mixed pattern of relationships among explicit and implicit bias. In some studies there was a low positive correlation [8, 14], and in other studies there was no relationship among bias type [5, 6, 15].
Obesity bias or weight stigmatization has the potential to affect an overweight person’s psychological and emotional well-being, resulting in e.g. depression, low self-esteem and body image, especially in those that do not possess adequate coping mechanisms or are sensitive to weight-related stereotypes [16, 17]. Criticism about one’s weight or weight-related teasing can serve as a potential obstacle for living a healthy, physically active lifestyle. In a prospective study, weight-related teasing was significantly related to binge eating and loss of control in males, and in females teasing was associated with frequent dieting [18]. In physical activity settings, overweight or obese individuals who were teased or criticized had reduced physical activity levels [19, 20], decreased enjoyment [19], and embarrassment while participating [21]. Given the seriousness of the psychological and emotional ramifications, preparing professionals to possess positive attitudes and beliefs toward overweight is critical for them to create inclusive and motivating physical activity environments. Researchers suggest that a comprehensive bias reduction approach is necessary due to the resiliency and complex nature of obesity bias. This involves the use of multiple strategic intervention components and theoretical frameworks [22, 23]. Two intervention studies in pre-professional settings have used multiple strategies successfully to reduce explicit bias [7, 24]; however, no study to date has assessed the effectiveness of a multi-component intervention to reduce implicit obesity bias. To fully assess the success of obesity bias intervention, both implicit and explicit bias need to be measured.
Intervention Strategies and Frameworks
Common strategic intervention components that were investigated in this study consist of attribution theory (reducing perceptions of controllability to reduce blame), consciousness raising, and evoking empathy through perspective taking, role playing, and exposure to overweight individuals [25].
The first framework is attribution theory, which posits that individuals will exhibit bias or negative emotion toward overweight or obese individuals if they perceive that their condition is controllable (e.g., they do not exercise or eat too much) [26, 27]. Crandall et al. [28], in a study of six nations, found that bias is greater when individuals perceive controllability and devalue the condition of overweight or obese. One intervention strategy has had equivocal results, which consists of providing scientific evidence that one’s condition is not controllable. Crandall [29] provided scientific information that obesity was not controllable (i.e., caused by genetics and other physiological mechanisms), which resulted in reduced blame or explicit bias toward overweight individuals by the participants. Teachman et al. [30], however, failed to reduce both explicit and implicit bias through having individuals read a news report at a beach persuading individuals that obesity was mainly caused by genetics. Provision of information that obesity was controllable through diet and exercise to participants resulted in higher implicit bias.
Rukavina et al. [8], in a multi-strategy intervention, were able to reduce explicit obesity bias when kinesiology pre-professionals were presented with a situational perspective of obesity or that there are many physical activity barriers and multiple reasons for one to become overweight other than just diet and exercise (e.g. idea of personal responsibility). Schwartz and Brownell [31] advocate that for public health interventions to make significant environmental changes beliefs of the etiology of obesity need to be shifted from a narrow perspective of personal responsibility to an understanding of the role of the ‘toxic environment’ and a scientific accurate etiology of obesity [32]. A narrow perspective of beliefs in personal control and responsibility can lead to loss of time and money whereby environmental changes can lead to decrease in health disparities and social injustices.
One strategy that has been suggested to reduce implicit bias is consciousness raising [6, 13]. Consciousness raising involves making individuals aware of the nature of obesity bias, its pervasiveness, and the difference between explicit and implicit bias. Also, in terms of multi-strategy interventions, it has been suggested that consciousness raising be paired with other strategic intervention components so that people can make themselves aware of possible environmental critical cues that may evoke their implicit bias. Awareness is the first step to change deep-seated unconscious bias.
Another strategic intervention component involves evoking empathy toward obese individuals to reduce implicit bias [14, 30]. Teachman et al. [30] had women read a first hand account of a woman who was stigmatized for being obese and write an essay to display their feelings toward obese women in general. This intervention failed to reduce implicit bias in average weight women, but bias was reduced in women with high BMI. Wiese et al. [24], however, successfully reduced explicit bias in pre-medical students. Participants watched a video of a nurse talking about a stigmatized experience she encountered, and they engaged in two role playing exercises where they took the perspectives of the one being stigmatized.
A final set of intervention components involves exposure to overweight individuals. Pettigrew and Tropp [33], in a meta-analysis of 515 studies, reported that exposure to a stigmatized population typically results in a reduction of negative attitudes. It is hypothesized that exposure to overweight people impact negative attitudes [25]. Rukavina et al. [8] exposed pre-professionals to a population of overweight elementary children in an experiential learning situation. Participants engaged in a service learning to conduct fitness tests on elementary school students. Subsequently, participants evaluated the results, designed evaluation sheets to be sent home to parents, and wrote reflection papers on their experience. The purpose of the service learning was to create knowledge through transformation of experience usually occurring in four phases: experiencing, reflecting, generalizing, and applying [34]. Pre-professionals were able to accomplish curricular learning goals and at the same time engage in a hands-on activity to provide service to children and the community. In the reflection phase, pre-professionals were prompted to generalize their experience and knowledge from classroom discussions and make plans to use this in their future profession.
Researchers have recommended that curricular interventions be evaluated [2] that use a combination of multiple strategies to combat obesity bias [14, 23]. Implicit bias has been resilient to change; thus it is probable that a combination of strategies is important to target them. Interventions during undergraduate education are important because pre-professionals health habits are being shaped, and this critical information can help develop their future professional conduct when promoting healthy physical active lifestyles in youth and adults [35].
Researchers have called for testing of undergraduate curricula interventions [2]. Several multi-strategy studies have been successful reducing explicit obesity bias [8, 24], but it is unknown if these interventions impact implicit bias. Therefore, the purpose of the present study was to assess kinesiology pre-professionals’ both explicit and implicit bias, and then determine the efficacy of a multi-strategy intervention to reduce both kinesiology pre-professionals’ explicit and implicit bias. Several intervention components were included specifically to target both implicit and explicit biases. Thus it is expected that there be a significant reduction in both types. Creating and evaluating interventions to reduce bias is an important step in educating professionals that can successfully implement public health initiatives without the cultural barriers of obesity bias that potentially hurt more than help by dissuading overweight or obese individuals to be physically active.
Material and Methods
Participants
Participants included 78 kinesiology pre-professionals (51 male and 26 female, 1 missing; 55 European American, 20 African American, 1 Hispanic, 1 other, 1 missing) from a southern university in the USA. Ages ranged from 18 to 26 years old (mean = 21.63 years, SD = 1.49 years). The majority of participants grew up in a rural or small city childhood environment (rural/small city = 50, mid/large-sized city = 27, missing = 1) and were single at the time of the intervention (single = 70, married = 7, divorced = 0, missing = 1). The intervention was applied to a test and measurement class (n = 42), whereas the control group participants (n = 36) were recruited from several other classes in the department who had not received the intervention. Participants came from 4 main undergraduate concentrations (17 clinical exercise physiology (CLEP), 3 fitness management, 35 physical education teacher preparation, 9 sport communication, and 13 other, 1 missing). A test and measurement class was used for the intervention because all pre-professionals from the department took the class and a field experience component was available where pre-professionals would have exposure to overweight population and discuss and deal with obesity bias issues and prevent bias in an applied setting (i.e. elementary school fitness tests). Informed consent was obtained prior to start of the intervention as according to the institutions internal review board.
Measures
Demographic Questionnaire
A demographic questionnaire included questions on education, height, weight, age, sex, and race. Moreover, other yes/no items assessed social and environmental influences, for example ‘Do you have personal experience with obesity?’, ‘Do you have a family history of obesity?’, and ‘Do you believe people have personal control over obesity?’.
Explicit Ratings Tests (ERTs)
Participants’ explicit attitudes toward fat people using seven-point semantic differential scales were assessed with a self-report ERT questionnaire. Two scales were used to rate both fat and thin people ‘lazy versus motivated’ and ‘stupid versus smart’ yielding four ratings. The explicit attitude scores were computed by subtracting the ratings for thin people from those for fat people for each of the two different attributes [4, 6]. A negative score indicates an obesity bias.
Anti-Fat Attitudes Test (AFAT)
Participants’ anti-fat attitudes toward fat individuals were assessed with a self-report AFAT questionnaire, which used a five-point Likert scale ranging from ‘strongly disagree’ to ‘strongly agree’. Lewis et al. [36] used a confirmatory analysis to validate the instrument. It includes three subscales: physical/romantic attractiveness, weight control/blame, and social/character disparagement, Physical/romantic unattractiveness is the belief that overweight individuals are homely and would not make good romantic partners. Weight control/blame represents the beliefs that overweight individuals are responsible for their weight versus control from biogenetic inputs. Social/character disparagement represents the ideas that overweight people possess undesirable personality characteristics and hold low value socially. Any items that did not load on the subscales were left out of the present study.
Implicit Association Test (IAT)
The IAT is a timed word classification task used to assess implicit bias toward overweight and obese individuals. The IAT has been used in multiple populations and settings [3, 6] and has demonstrated convergent and discriminant validity [37, 38]. The test uses response latencies to assess the strength of association between concepts (e.g. thin and fat) and particular attributes (motivated and lazy). The goal of the task is to categorize the list of attributes into one of four categories. For example, one of the tests includes the categories of fat, thin, lazy, and motivated. On the first task, the categories are paired (thin/motivated, fat/lazy). On the top of the paper, thin/motivated is on the top left side of the paper, and fat/lazy is on the top right side. A list of words runs down the middle of the page. The participants begin by making a checkmark on either the left side or right side of the words in the list. On the second task, the words are reversed (thin/lazy, fat/motivated) using a similar set of words.
People generally find it easier to pair the words when the categories match their attitude (fat is paired with lazy and thin is paired with motivated) than when the words are reversed (fat paired with motivated, thin with lazy). Thus, when the category pairing is similar to their attitude, they are able to categorize more words correctly in 20-second time limit. The final score is computed by subtracting the number of words correctly classified in the incongruent task (fat paired with motivated) then correctly classified in the congruent task (fat paired with lazy). A large difference score indicates a stronger implicit association between fat people and a negative attribute than between fat people and a positive attribute. In the present study, one practice task using insects and flowers was employed in addition with the two experimental tasks (lazy/motivated, stupid/smart).
Intervention Components
The intervention included both classroom and service learning components. The classroom components were implemented before the field experience and consisted of:
i) Consciousness raising discussion. Pre-professionals were made aware of society’s biases toward overweight bias, societal influences that reinforce these biases, and that kinesiology-related professionals also have obesity bias. Also, they were made aware of the difference between implicit and explicit bias and the ramifications or potential triggers (e.g. teasing, discrimination, health care professionals’ comments) that could initiate a vicious cycle leading to unhealthy coping mechanisms and further weight gain.
ii) Perceptions of controllability. Pre-professionals discussed the scientific evidence for multi-factorial causes of obesity – genetic, environmental, cultural, psychological. This perspective was contrasted with the attitude of individual responsibility and weight control solely through diet and exercise. This component originated from Crandall [29] who had participants read about science-related reports of causes of obesity.
iii) Perspective taking. Pre-professionals heard an overweight woman with a thyroid gland problem talking about her stigmatization. In both large and small groups, the pre-professionals discussed what they learned from the tape, how the overweight women felt, and what were the implications of knowing about obesity bias were for their future careers. This component has been used by Weiss et al. [24] in a multi-component intervention with medical students.
iv) Role-playing activity on environmental cues. Pre-professionals were aware of cues in test and measurement environment that could elicit their implicit obesity bias, such as hearing a fat joke or an overweight student acting congruent to stereotypes (lazy or not performing well on fitness tests). The addition of this component was designed to provide an awareness of the automatic nature of situation-specific environmental cues so that in the service learning project they could thwart any automatic responses to be bias when working professionally in the fitness tests.
The service learning project consisted of pre-professionals administrating the FITNESSGRAM to a whole school of 4th and 5th grade children. The purpose of this component was to expose the pre-professionals to overweight children’s exercise behavior and their peer’s behavioral responses. Each pre-professional helped administer the test to 3–5 classes of students, evaluated the data, completed evaluation sheets to be sent home to parents, and wrote a reflection paper about what they learned from both classroom and service learning experience with the children. Also, they were to speculate on how they would treat overweight students or clients in the future as a result of the intervention. Pre-professionals were provided with stimulation questions, which included ‘What did you learn from this service learning project (administering the FITNESSGRAM and listening to lectures on obesity bias)?’, ‘Did you notice any environmental cues (e.g. seeing an obese child or hearing teasing) elicit an implicit obesity bias from yourself?’, ‘Describe how your attitude has or has not changed toward obese individuals as a result of the lectures and service learning project’, and ‘How do you plan to treat your clients or students in the future?’
Procedure
The obesity bias intervention was placed in a test and measurement class. The goal of the class was to learn about purposes of measurement and evaluation, basic testing procedures for children and adults, computing basic statistics, and applying concepts of reliability and validity to sport and fitness testing. After pre-professionals were introduced to the basic concepts of measurement and evaluation, the obesity bias intervention began. A package of instruments was administered pre and post intervention during their regular class time. Those in the control group were recruited from other classes in the department and filled out the questionnaire during the same time frame as the intervention group. Administrators of the survey informed pre-professionals that some of the questions might be construed as offensive, but are necessary to assess attitudes toward obesity. Pre-professionals completed the instruments in the following order: demographics, AFAT, ERTs, and IAT.
Design and Data Analysis
A pre-post experimental design with a control group as a comparison was used to assess the efficacy of the intervention using both implicit and explicit obesity bias measures. For analysis of the quantitative AFAT data (subscales are physical/romantic attractiveness, weight control/blame, and social/character disparagement), all negatively worded items were reverse-coded prior to any data analysis and internal consistency using Cronbach’s a were computed [39]. The aggregate scores for the AFAT subscales were computed by summing all responses for all items and dividing them by the number of items in the subscale. Pearson’s correlations were conducted to examine the relationships among BMI, the two ERTs, the three subscales of AFAT, and two subscales of IAT.
To examine whether participants had any explicit and implicit biases, MANOVA or ANOVAs were conducted on pre-measures. MANOVA and follow-up ANOVAs were conducted on pre-test scores of AFAT subscales to examine whether participants had any explicit obesity bias. AFAT pre-measure values were compared to a Likert value of 3, which was indicative of neutral attitude. The difference scores between the original scores and 3 were used for the data analysis, with positive difference scores indicating explicit bias. An a level of 0.017 based on a Bonferroni adjustment was used for individual ANOVA on AFAT subscales. Independent T-tests with adjusted a level of 0.006 (Bonferroni adjustment) were computed for each of the nine items from AFAT with values exceeding 3 to examine whether participants had any explicit obesity bias. ANOVA was conducted on the pre-test score of the semantic differential scale stupid/smart to examine whether participants had any explicit obesity bias. Non-parametric ANOVAs using rank orders were conducted on the semantic differential scales stupid/smart and lazy/motivated to examine whether participants had any explicit obesity bias. Two separate ANOVAs were conducted on pre-test scores of the subscales of IAT (lazy/motivated and stupid/smart) to examine whether participants had any implicit obesity bias.
Three separate 2 × 2 non-parametric ANOVAs with the factors of time (pre/post) and group (experimental group / control group) were conducted on the three AFAT subscales to examine whether participants’ explicit obesity bias was reduced over time from pre to post as a result of intervention. Two separate 2 × 2 non-parametric ANOVAs with the factors of time (pre/post) and group (experimental group / control group) were conducted to examine whether there were any significant reductions of implicit obesity bias as a result of interventions. Two separate 2 × 2 non-parametric ANOVAs with the factors of time (pre/post) and group (experimental group / control group) were conducted on motivated/lazy and stupid/smart semantic differential scales to examine whether there were any significant reductions of explicit obesity bias as a result of intervention. The non-parametric inferential tests were selected because of serious violations of normality.
Results
A relatively small frequency of pre-professionals had a family history with obesity (yes = 7, no = 70, missing = 1) or personal history with obesity (yes = 5, no = 72, missing = 1). A large number of pre-professionals advocated that obesity is under personal control (control = 68, not under personal control = 8, missing = 2) prior to the interventions. Means and standard deviations for the AFAT and IAT are presented in table 1. The AFAT subscale internal consistency reliability was acceptable; Cronbach’s a reliability coefficient ranged from 0.75 to 0.89. Correlations among obesity bias measures and BMI are in given in table 2. Of particular note is that explicit measures are significantly correlated amongst each other, suggesting those that had bias in one area have bias in another. Also, the correlations were not significant between any explicit and implicit obesity bias measure, indicating that there were no associations between implicit and explicit measures.
Pretest Analysis
AFAT
At the pretest, MANOVA indicated a significant difference from zero on AFAT subscales prior to the intervention (F(3, 73) = 163.25, p < 0.0001). The follow-up ANOVAs with adjusted a level of 0.017 indicated a significant difference from zero for social/character disparagement (F(1, 75) = 255.43, p < 0.0001, ηp2 = 0.77) and weight control/blame (F(1, 75) = 10.98, p < 0.0014, ηp2 = 0.13), but not for physical attractiveness (F(1, 75) = 1.99, p = 0.16). Inspection of the means indicates that participants overall did not have explicit bias as measured by the AFAT prior to the intervention. However, inspection of the means for individual items indicated that there were biased on specific issues. Of the nine individual AFAT items that had scores greater than 3.0 (table 3), four items were significantly different from zero using an adjusted p value of 0.006. These items were ‘Most fat people buy too much junk food’, ‘If fat people really wanted to lose weight, they could’, ‘If I were single, I would date a fat person’, and ‘Fat people should not wear revealing clothing in public’.
Table 3.
T-test results of pre-intervention means and standard deviations for items identified as greater than 3 on the AFAT
| Item | Pre-intervention | T-test |
|---|---|---|
| Most fat people buy too much junk food | 3.43 ± 0.95 | T(76) = 3.95 p < 0.0002 |
| Most fat people are lazy | 3.29 ± 1.18 | T(76) = 2.13 p < 0.0368 |
| If fat people really wanted to lose weight, they could | 3.82 ± 0.91 | T(76) = 7.86 p < 0.0001 |
| Most fat people will latch onto almost any excuse for being fat | 3.23 ± 1.00 | T(76) = 2.05 p < 0.0434 |
| If I were single, I would date a fat person | 3.70 ±1.09 | T(76) = –5.60 p < 0.0001 |
| Fat people are physically unattractive | 3.16 ± 1.19 | T(76) = 1.15 p < 0.2552 |
| Fat people should not wear revealing clothing in public | 4.18 ± 1.16 | T(76) = 8.98 p < 0.0001 |
| People who are fat have as much physical coordination as anyone* | 3.16 ± 1.12 | T(76) = –1.22 p < 0.2278 |
| Fat people should be encouraged to accept themselves the way they are* | 3.16 ± 1.05 | T(76) = –1.30 p < 0.1976 |
Items reversed scored.
IAT
The ANOVA analyses on pre-test scores of IAT indicated significant differences from zero for the motivated/lazy (F(1, 64) = 152.70, p < 0.0001, ηp2 = 0.70) and stupid/smart (F(1, 63) = 123.84, p < 0.0001, ηp2 = 0.66) scale. The results indicated that participants had implicit obesity bias toward overweight or obese people.
ERT
As indicated by ANOVA analyses prior to the intervention, pre-professionals reported explicit biases on lazy/motivated semantic differential scale (F(1, 76) = 257.78, p < 0.0001, ηp2 = 0.77), but not on stupid/smart scale (F(1, 77) = 0.78, p = 0.3812).
Pre-Post Intervention Analysis
AFAT
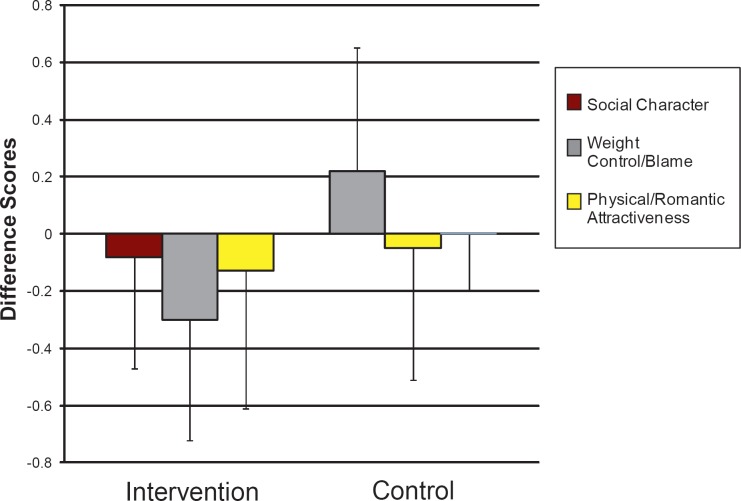
The 2 × 2 ANOVA analyses indicated that there was a significant interaction effect between time and group on the AFAT social/character disparagement subscale (F(1, 72) = 5, p < 0.03, ηp2 = 0.06). No significant time (F(1, 72) = 3.50, p = 0.07) and group effects (F(1, 72) = 1.71, p = 0.2) were observed. For the model with physical attractiveness as the dependent variable, no significant differences were observed for the interaction effect between time and group (F(1, 73) = 1.16, p = 0.29), the main time effect (F(1, 73) = 0.59, p = 0.44), and the main group effect (F(1, 73) = 0.65, p = 0.42). For the model with weight control/blame as the dependent variable, significant differences were observed for the interaction effect between time and group (F(1, 74) = 4.78, p < 0.03, ηp2 = 0.06) and the main time effect (F(1, 74) = 5, p < 0.03, ηp2 = 0.06). There was no significant main group effect (F(1, 74) = 0, p = 0.95). The results showed that participation in the intervention reduced explicit bias on the AFAT social/character disparagement and weight control/blame subscales but not on the physical attractiveness subscale. Evaluation of the means indicates a reduction in explicit bias for weight control/blame and social/character disparagement for intervention groups and an increase in explicit bias for control group on the social/character disparagement subscale (fig. 1).
Fig. 1.
AFAT subscale difference scores for intervention and control groups.
IAT
The 2 × 2 ANOVA analyses indicated that there were a non-significant interaction effect between time and group (F(1, 63) = 0.07, p = 0.79) as well as non-significant main effects of time (F(1, 63) = 0.13, p = 0.72) and group (F(1, 63) = 0.52, p = 0 .48) on the motivated/lazy IAT implicit anti-fat bias. The 2 × 2 ANOVA analyses also indicated that there were a non-significant interaction effect between time and group (F(1, 64) = 0.50, p = 0.48) as well as non-significant main effects of time (F(1, 64) = 0.55, p = 0.46) and group (F(1, 64) = 3.57, p = 0.06) on the stupid/smart IAT implicit anti-fat bias.
ERT
The 2 × 2 ANOVA analyses with the factors of time and groups revealed a non-significant interaction effect between time and group (F(1, 75) = 0.05, p = 0.83) as well as non-significant main effects of time (F(1, 75) = 0.04, p = 0.84) and groups (F(1, 75) = 0.15, p = 0.7) on the stupid/smart explicit rating. The 2 × 2 ANOVA analyses with the factors of time and groups revealed a non-significant interaction effect between time and group (F(1, 75) = 0.05, p = 0.82) as well as non-significant main effects of time (F(1, 75) = 0.04, p = 0.84) and groups (F(1, 75) = 3.9, p = 0.05) on the motivated/lazy explicit rating.
Discussion
The purpose of the present study was to describe kinesiology pre-professionals’ obesity bias and assess the efficacy of a multi-strategy intervention to reduce their explicit and implicit obesity bias. A multi-strategy intervention is necessary to impact the deep-seated nature of implicit biases and variety of negative stereotypes that exist. Particular intervention components were specifically designed to debunk particular stereotypes and create empathy through increased awareness of the psychological and emotional consequences as a result of being stigmatized. These intervention components were strategically situated adjacent to a service learning project that gave kinesiology pre-professionals a chance to apply the knowledge learned in the classroom and reflect on the negative implications of obesity bias in their future careers.
In the present study, kinesiology pre-professionals reported strong implicit anti-fat bias (stupid/smart, motivated/lazy) before the intervention, which is consistent with IAT results of fitness professionals and exercisers [5], another group of kinesiology pre-professionals [6], and other health-related professionals [4]. Moreover and similar to other studies [6, 8], the pre-professionals did not display overall explicit obesity bias (AFAT subscales of weight/control blame, social/character disparagement, and sexual attractiveness). Interestingly, the correlations among explicit bias AFAT measurements were significant, indicating that those who were biased in one area were also biased in other areas and vice versa for those that were not biased. On the other hand, the implicit bias measurements were not correlated to each other or to any of the explicit bias measurements, as already shown by Chambliss et al. [6]. This lack of correlation is consistent with further data from the literature, showing little or no association among implicit and explicit measures. The pattern of association has been explained by differences in age, moderators, and type of obesity bias assessments [40].
Similar to other studies [6, 8, 10], the pre-professionals, however, endorsed individual stereotypes related to individual control of lifestyle behavior and outward appearance, measured by several measurements, i.e., individual items on the AFAT, demographic measure of individual control, and measure of the semantic differential explicit measure of lazy/motivated. These results suggest that pre-professionals value living a healthy active lifestyle and that they assume that overweight individuals are not taking responsibility for maintaining a normal weight, learning motor skills, or making an attempt to improve their appearance. Individuals that believe in high personal control are linked to higher levels of obesity bias [5, 6, 41].
In an effort to reduce the endorsement of these stereotypes, a multiple strategy intervention to reduce kinesiology pre-professionals’ obesity bias was implemented. The strategic intervention components were grounded in theory but differed as a function of this unique pre-professional situation. In the present study, individuals became aware of the multi-factorial nature of obesity, of the differences between implicit and explicit bias, and of the negative ramifications in their career field that arise from both. The addition of these components is a departure from Rukavina et al. [8] where components only addressed issues related to explicit bias. To further address issues related to implicit bias, pre-professionals listened to an audio tape, similar to Weiss et al. [24], to evoke empathy toward overweight individuals. Last, a role playing activity was added to make pre-professionals aware of the situation-specific environmental cues that could activate their implicit bias in the service learning component. Earlier studies had not attempted to facilitate reflective work with pre-professionals to deal with implicit bias.
The intervention achieved partial success. Mean values in the AFAT blame/personal control subscale were siginificantly reduced. Both multi-component intervention [8] and psychologically based studies [29] have shown significant reductions of weight control/blame. This result of the present study is consistent with attribution theory and is not surprising given that the several intervention components were strategically focused to reduce blame.
In the present study, during the classroom instruction, pre-professionals were introduced to situational perspective (i.e., there are multiple reasons for one’s level of fatness such as genetics, social, or psychological reasons), and this was reinforced when the pre-professionals heard the tape of the woman talking about her hyperthyroidism (genetics) and the witnessed resultant stigmatized interaction of the children (social). There was a significant change in the AFAT measure of social/character disparagement or the degree pre-professionals prejudge individuals in that they have low social value or possess undesirable personality characteristics because of their body shape and size. The strategic intervention component of hearing the overweight women talk about her life was designed to evoke empathy through perspective taking. Pre-professionals were supposed to imagine the stigmatization and what it felt like to be a second class citizen. In the discussions after hearing the tape of the stigmatized woman, some pre-professionals were shocked of the negative treatment and argued that people are individuals and people are not better than others just because of their body size. Phrases that were introduced in the discussions after hearing the tape were ‘everybody has the same size heart’ or ‘work with people as if they are individuals instead of stereotypical obese persons’.
The intervention did not yield a significant change in pre-professionals implicit bias pre and post intervention for either the lazy/motivated or the stupid/smart IAT scales. This non-significant result is similar to other single intervention component studies [22, 30]. To reduce the implicit bias in the present study, pre-professionals were made aware of their bias (consciousness raising), encouraged to take the perspective of an overweight woman who was stigmatized, exposed to the behavior of overweight children, and primed to notice if their implicit bias was being activated during the service learning project. One possible reason for the lack of the reduction, based on theories of attitude change [42], is that pre-professionals were in the beginning stages of attitude change and still processing or trying to resolve the dissonance created by the intervention. Until they resolve the internal conflict among themselves and make a conscious effect to de-link the automatic evaluation with the environmental cue, the implicit bias will persist.
To reduce bias, it is likely that key concepts need to be introduced early and reinforced throughout the curriculum, and not singly placed within one class near the end of the professional preparation. O’Brien et al. [9] found that pre-service teachers increased their implicit bias from year 1 to year 3 and had greater degree of implicit bias than psychology majors. Departments need to evaluate pre-professionals’ conceptions and ensure they are not providing competing messages or promoting misconceptions of scientific information. For example, one common misconception occurs when pre-professionals assume a cause and effect relationship between obesity and health risks. One implication they miss is that one can be overweight and still be healthy. Thus, departments need to promote the correct etiology of obesity (multiple reasons for obesity beyond diet and exercise) across the curriculum and, at the same time, promote diversity and size acceptance (healthy lifestyles for all body shapes and sizes).
Surprisingly, a testing effect occurred in the control group (did not receive the intervention but took the pre- and postassessments); there was a significant increase in the mean value of the social/character disparagement subscale from pre- to post-intervention. It is possible that the pre-test increased their awareness or primed the pre-professionals to notice the negative character of overweight individuals between pre- and post-measurements. Also, it is interesting to note that other explicit measures or implicit measures did not increase. For future interventions, researchers need to be aware that providing an obesity bias assessment may activate participants’ attitudes and the treatment may have to be more powerful to reduce bias than if no pre-assessment was provided. Future studies need to look at multiple universities and compare freshmen to senior attitudes.
Before future intervention studies, a comprehensive study of beliefs and attitudes across curriculum needs to be accomplished. Future interventions need to address the sexual attractiveness aspect of obesity bias beyond a superficial discussion; it is likely that beliefs of the ideal body shape and size could be a rate limiter in changing implicit bias and endorsing a size acceptance view. Discussions could include the education on the importance of matching one’s values in relationships, but not superficial items like hair color or body size; the danger of dieting to achieve body types that are not attainable; airbrushing of photos presented in the media to create body shapes and sizes that are not attainable; the positive nature of diversity; and the benefits of having a large size body for particular physical performances.
There were limitations in the present study that affect the generalization of the study to other settings. The study used a convenience sample of one class of kinesiology pre-professionals from a southern university in the USA and the control group volunteer pre-professionals from other classes in the same department. The use of non-random sampling for both groups can possibly create initial differences group differences that could impact their bias reduction. Also, these pre-professionals may not be representative of the population of pre-professionals. However, the results are consistent with other studies of other health and physical activity fields [5, 6]. Also, the explicit bias measure results may have been influenced from social desirability since the participants knew they were being studied. However, the present study took a large step forward in implementing multi-component intervention studies with pre-professionals. Interventions at this stage in their careers are vital given in that they are forming their attitudes for their careers and in that they will be ‘working in the trenches’ to promote a healthy active lifestyle. First, the study was the first multi-component intervention to test the effects using implicit bias and a comparison group (control). Second, the intervention lasted over 1 month and was specific to the careers of the pre-professionals.
Conclusion
In the present study, the intervention was partially successful at reducing pre-professionals’ obesity bias. However, the effects were relatively small as reflected from the effect sizes. Pre-professionals’ perceptions of controllability and blame and social/character disparagement were reduced. However, it is likely that participants need time and/or to be guided through attitudinal change process for a meaningful reduction in implicit bias to occur. Moreover, as evidenced by the inductive analysis of pre-professionals’ reflections, the participants had some similar experiences and perceptions, but it was apparent that each pre-professional experienced the intervention uniquely. It is possible that some key information was not processed by the pre-professionals because they were focused on particular aspects of the intervention, and not on others. More information is needed on pre-professionals’ beliefs and attitudes and how they process this particular information. This is essential to design better strategic components so that pre-professionals can process more information and become more emotionally involved with each of the intervention components.
Disclosure
The authors declared no financial interest.
Table 1.
Means and standard deviations for dependent measures
| Intervention group |
Control group |
|||
|---|---|---|---|---|
| pre-test | post-test | pre-test | post-test | |
|
AFAT Weight control/blame Social/character disparagement Physical/romantic attractiveness |
2.88 ± 0.55 2.04 ± 0.54 3.01 ± 0.70 |
2.58 ± 0.54 1.97 ± 0.55 2.88 ± 0.62 |
2.76 ± 0.56 2.08 ± 0.65 2.83 ± 0.71 |
2.70 ± 0.59 2.23 ± 0.61 2.08 ± 0.65 |
|
IAT Stupid/smart Lazy/motivated |
–8.51 ± 5.54 –8.74 ± 5.85 | –8.49 ± 5.61 –9.33 ± 6.12 |
–6.74 ±5.83 –8.23 ± 5.22 |
–5.70 ± 5.40 –8.31 ± 4.78 |
|
ERT Stupid/smart Lazy/motivated |
0.19 ± 0.77 2.00 ± 1.43 |
0 ± 0.31 1.02 ± 1.09 |
–0.03 ± 1.03 1.11 ± 1.39 |
0.06 ± 0.59 0.71 ± 1.20 |
Table 2.
Means, standard deviations, and correlation coefficients for AFAT and ERT measures
| WC | SC | PR | IATSS | IATML | BMI | SDSS | SDML | |
|---|---|---|---|---|---|---|---|---|
| WC | 1 | 0.68 | 0.73 | 0.08 | –0.13 | –0.33 | 0.36 | 0.50 |
| 0.0001 | 0.0001 | 0.4634 | 0.2699 | 0.0042 | 0.0013 | <0.0001 | ||
| n = 76 | n = 77 | n = 77 | n = 77 | n = 76 | n = 77 | n = 77 | ||
| SC | 1 | 0.76 | –0.00 | –0.13 | –0.16 | 0.43 | 0.33 | |
| 0.0001 | 0.9697 | 0.2484 | 0.1744 | 0.0001 | 0.0036 | |||
| n = 76 | n = 77 | n = 76 | n = 75 | n = 76 | n = 76 | |||
| PR | 1 | 0.04 | –0.17 | –0.28 | 0.48 | 0.45 | ||
| 0.7120 | 0.1464 | 0.0162 | 0.0001 | 0.0001 | ||||
| n = 77 | n = 77 | n = 76 | n = 77 | n = 77 | ||||
| IATSS | 1 | 0.04 | –0.07 | –0.16 | 0.14 | |||
| 0.7459 | 0.5508 | 0.1750 | 0.2076 | |||||
| n = 78 | n = 77 | n = 78 | n = 78 | |||||
| IATML | 1 | –0.14 | 0.09 | –0.02 | ||||
| 0.2359 | 0.4170 | 0.8592 | ||||||
| n = 77 | n = 78 | n = 78 | ||||||
| BMI | 1 | –0.23 | –0.19 | |||||
| 0.0401 | 0.0898 | |||||||
| n = 77 | n = 77 | |||||||
| SDSS | 1 | 0.18 | ||||||
| 0.1049 | ||||||||
| n = 78 | ||||||||
| SDML | 1 |
WC = AFAT (weight control/blame); SC = AFAT (social/character disparagement); PR =AFAT (physical/romantic attractiveness); IATSS = IAT (stupid/smart); IATML = IAT (motivated/lazy); SDSS = ERT (stupid/smart); SDML = ERT (lazy/motivated).
References
- 1.Ratzan SC. Silent threat: non-communicable disease and obesity. J Health Commun. 2004;9:1–2. doi: 10.1080/10810730490436833. [DOI] [PubMed] [Google Scholar]
- 2.Puhl R, Brownell Bias. KD discrimination, and obesity. Obes Res. 2001;9:788–805. doi: 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 3.Teachman BA, Brownell KD. Implicit anti-fat bias among health professionals: is anyone immune? Int J Obes Relat Metab Disord. 2001;25:1525–1531. doi: 10.1038/sj.ijo.0801745. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz MBChambliss HOBrownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–1039. doi: 10.1038/oby.2003.142. [DOI] [PubMed] [Google Scholar]
- 5.Robertson NVohora RFitness vs fatness. implicit bias towards obesity fitness professionals and regular exercisers. Psychol Sport Exerc. 2008;9:547–557. [Google Scholar]
- 6.Chambliss HOFinley CE, Blair SN. Attitudes toward obese individuals among exercise science students. Med Sci Sports Exerc. 2004;36:468–474. doi: 10.1249/01.mss.0000117115.94062.e4. [DOI] [PubMed] [Google Scholar]
- 7.Greenleaf C, Martin B, Rhea D. Fighting fat: how do fat stereotypes influence beliefs about physical education? Obesity (Silver Spring) 2008;16((suppl 2)):S53–S59. doi: 10.1038/oby.2008.454. [DOI] [PubMed] [Google Scholar]
- 8.Rukavina PB, Li W, Rowell MB. A service learning based intervention to change attitudes toward obese individuals in kinesiology pre-professionals. Soc Psych Educ. 2008;11:95–112. [Google Scholar]
- 9.O’Brien KS, Hunter JA, Banks M. Implicit anti-fat bias in physical educators: physical attributesideology and socialization. Int J Obes. 2007;31:308–314. doi: 10.1038/sj.ijo.0803398. [DOI] [PubMed] [Google Scholar]
- 10.Greenleaf C, Weiller K. Perceptions of youth obesity among physical educators. Soc Psych Educ. 2005;8:407–423. [Google Scholar]
- 11.Irwin CCSymons CW, Kerr DL. The dilemmas of obesity: How can physical educators help? JOPERD. 2003;74:33–39. [Google Scholar]
- 12.Blair IVMa JELenton AP. Imagining stereotypes away: the moderation of automatic stereotypes through mental imagery. J Pers Soc Psychol. 2001;81:828–841. doi: 10.1037//0022-3514.81.5.828. [DOI] [PubMed] [Google Scholar]
- 13.Greenwald AGBanaji MRImplicit social cognition. attitudesself-esteem, and stereotypes. Psychol Rev. 1995;102:4–27. doi: 10.1037/0033-295x.102.1.4. [DOI] [PubMed] [Google Scholar]
- 14.Gapinski KD, Schwartz MB, Brownell KD. Can television change anti-fat attitudes and behavior? J Appl Biobehav Res. 2006;11:1–28. [Google Scholar]
- 15.Brochu PMMorrison MAImplicit and explicit prejudice toward overweight and average-weight men and women. testing their correspondence and relation to behavioral intentions. J Soc Psychol. 2007;147:681–706. doi: 10.3200/SOCP.147.6.681-706. [DOI] [PubMed] [Google Scholar]
- 16.Libbey HPStory MT, Neumark-Sztainer DR. Boutelle Teasing KN disordered eating behaviors and psychological morbidities among overweight adolescents. Obesity (Silver Spring) 2008;16((suppl 2)):S24–SS. doi: 10.1038/oby.2008.455. [DOI] [PubMed] [Google Scholar]
- 17.Haines J, Neumark-Sztainer D, Wall M, Story M. Personal behavioral, and environmental risk and protective factors for adolescent overweight. Obesity (Silver Spring) 2007;15:2748–2760. doi: 10.1038/oby.2007.327. [DOI] [PubMed] [Google Scholar]
- 18.Haines J, Neumark-Sztainer D, Eisenberg ME, Hannan PJ. Weight-related teasing and disordered eating behaviors in adolescents: longitudinal findings from project EAT (eating among teens) Pediatrics. 2006;117:209–215. doi: 10.1542/peds.2005-1242. [DOI] [PubMed] [Google Scholar]
- 19.Faith MSLeone MA, Ayers TS, Heo M, Pietrobelli A. Weight criticism during physical activitycoping skills and reported physical activity in children. Pediatrics. 2002;110:e23. doi: 10.1542/peds.110.2.e23. [DOI] [PubMed] [Google Scholar]
- 20.Storch EA, Milsom VA, Debraganza N, Lewin AB, Geffken GR, Silverstein JH. Peer victimizationpsychosocial adjustment and physical activity in overweight and at-risk-for-overweight youth. J Pediatr Psychol. 2007;32:80–89. doi: 10.1093/jpepsy/jsj113. [DOI] [PubMed] [Google Scholar]
- 21.Pierce JW, Wardle J. Cause and effect beliefs and self-esteem of overweight children. J Child Psychol Psychiatry. 1997;38:645–650. doi: 10.1111/j.1469-7610.1997.tb01691.x. [DOI] [PubMed] [Google Scholar]
- 22.Gapinski KD, Schwartz MB, Brownell KD. Can television change anti-fat attitudes and behavior? J Appl Biobehav Res. 2006;11:1–28. [Google Scholar]
- 23.Puhl RM, Schwarz MB, Brownell KD. Impact of perceived consensus on stereotypes about obese people: A new approach for reducing bias. Health Psychol. 2005;24:517–525. doi: 10.1037/0278-6133.24.5.517. [DOI] [PubMed] [Google Scholar]
- 24.Wiese HJCWilson JF, Jones RA, Neises M. Obesity stigma reduction in medical students. Int J Obes Relat Metab Disord. 1992;16:859–868. [PubMed] [Google Scholar]
- 25.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: Toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–227. doi: 10.1046/j.1467-789x.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 26.Weiner B. Judgments of Responsibility: A Foundation for a Theory of Social Conduct. New York Guilford. 1995 [Google Scholar]
- 27.Weiner B, Perry RP, Magnusson J. An attributional analysis of reactions to stigma. J Pers Soc Psychol. 1988;55:738–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]
- 28.Crandall CSD’Anello S, Sakalli N, Lazarus E, Nejtardt GW, Feather NT. An attribution-value model of prejudice: anti-fat attitudes in six nations. Pers Soc Psychol Bull. 2001;27:30–37. [Google Scholar]
- 29.Crandall CS. Prejudice against fat people: ideology and self-interest. J Pers Soc Psychol. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- 30.Teachman BAGapinski KD, Brownwell KD, Rawlins M. Demonstrations of implicit anti-fat bias: the impact of providing causal information and evoking empathy. Health Psychol. 2003;22:68–78. doi: 10.1037//0278-6133.22.1.68. [DOI] [PubMed] [Google Scholar]
- 31.Schwartz MBBrownell, KD. Actions necessary to prevent childhood obesity: creating the climate for change. J Law Med Ethics. 2007;35:78–89. doi: 10.1111/j.1748-720X.2007.00114.x. [DOI] [PubMed] [Google Scholar]
- 32.Maffeis C. Aetiology of overweight and obesity in children and adolescents. Eur J Pediatr. 2000;159((suppl 1)):S35–SS. doi: 10.1007/pl00014361. [DOI] [PubMed] [Google Scholar]
- 33.Pettigrew TF, Tropp LR. A meta-analytic test of intergroup contact theory. J Pers Soc Psychol. 2006;90:751–783. doi: 10.1037/0022-3514.90.5.751. [DOI] [PubMed] [Google Scholar]
- 34.Kolb DA. Experiential Learning: Experience as the Source of Learning and Development. New JerseyPrentice Hall. 1984 [Google Scholar]
- 35.Ottenritter NW. Service learningsocial justice and campus health. J Am Coll Health. 2004;52:189–191. doi: 10.3200/JACH.52.4.189-192. [DOI] [PubMed] [Google Scholar]
- 36.Lewis RJ, Cash TF, Jacobi L, Bubb-Lewis C. Prejudice toward fat people: the development and validation of the anti-fat attitudes test. Obes Res. 1997;5:297–307. doi: 10.1002/j.1550-8528.1997.tb00555.x. [DOI] [PubMed] [Google Scholar]
- 37.Gawronski B. What does the Implicit Association Test measure? A test of the convergent and discriminant validity of prejudice-related IATs. Exp Psychol. 2002;49:171–180. doi: 10.1026//1618-3169.49.3.171. [DOI] [PubMed] [Google Scholar]
- 38.Greenwald AG, McGhee DE, Schwartz JLK. Measuring individual differences in implicit cognition: the Implicit Association Test. J Pers Soc Psychol. 1998;74:1464–1480. doi: 10.1037//0022-3514.74.6.1464. [DOI] [PubMed] [Google Scholar]
- 39.Cronbach LJ. Coefficient alpha and the internal structure of tests. Psychometrika. 1951;16:297–334. [Google Scholar]
- 40.Hofmann WGawronski B, Gschwender T, Le H, Schmitt M. A meta-analysis on the correlation between the implicit association test and explicit self-report measures. Pers Soc Psychol Bull. 2005;31:1369–1385. doi: 10.1177/0146167205275613. [DOI] [PubMed] [Google Scholar]
- 41.Hilbert ARief W, Braehler E. Stigmatizing attitudes toward obesity in a representative population-based sample. Obesity (Silver Spring) 2008;16:1529–1534. doi: 10.1038/oby.2008.263. [DOI] [PubMed] [Google Scholar]
- 42.Suedfeld P. Attitude Change: The Competing Views. EdisonAldine Transaction. 2007 [Google Scholar]