Abstract
Objectives
To investigate the reasons for the failure of uptake of shared-care arrangements for prescribing in attention deficit hyperactivity disorder.
Methods
A questionnaire was sent to 140 randomly selected general practitioners (GPs) in our local commissioning group area, and semistructured interviews were carried out with five GPs.
Results
Thirty-five questionnaires were returned, giving a response rate of 25%. The results indicate multifactorial reasons for failure to accept shared care. Three main factors were identified, namely GP concerns about the robustness of the diagnosis, lack of availability or uptake of non-pharmacological treatments and a perception that secondary-care physical monitoring was inconsistent.
Conclusions
Our recommendations for facilitating uptake of shared-care partnerships include improving documentation on how the decision to initiate medication is made, enhancing access to and communicating use of non-pharmacological treatments and ensuring communication of the results of physical monitoring and follow-up.
Keywords: PAEDIATRICS, PRIMARY CARE, QUALITATIVE RESEARCH
Introduction
Attention deficit hyperactivity disorder (ADHD) is the most commonly occurring neurobehavioural disorder in children, with a suggested prevalence of 3%–9% of children.1 Initial treatment should usually be non-pharmacological, with medication used if severe impairment or non-pharmacological treatments are refused or ineffective.1 Licensed medications for ADHD are methylphenidate, atomoxetine, dexamfetamine and lisdexamfetamine. The National Institute for Health and Clinical Excellence (NICE) recommends that these should be initiated by specialists, but that general practitioners (GPs) may take the responsibility for prescribing under shared-care arrangements.1
Within Northern Ireland, these medicines are classified as amber in the regional ‘traffic light system’ for a child over 6 years when medication doses are NICE guideline compliant and hence are appropriate for GP prescribing under shared-care arrangements.2 Regional shared-care guidelines are available to support this. Despite this, some GPs are reluctant to prescribe under a shared-care partnership. Annually, approximately 600 children suitable for a shared-care arrangement are required to have their ADHD medication dispensed by the Northern Health and Social Care Trust. This figure is in stark contrast to the rest of Northern Ireland with approximately 20 patients in all other trusts receiving amber-listed ADHD medication from secondary care (Northern Ireland Interface Pharmacists Network Specialist Medicines, personal correspondence 2013). The absolute numbers of GPs in the Northern local commissioning group (LCG) area participating in shared care is unknown, but these contrasting prescribing arrangements indicate that GP confidence for entering into shared-care arrangements in our trust catchment is poor.
The aims of this study were to examine why so many GPs in the Northern LCG area do not prescribe medicines for ADHD under shared-care arrangements and to identify required action to address this.
Method
A quantitative and qualitative questionnaire was sent to 140 randomly selected GPs, a sample size equating to 50% of the total. Question content examined personal prescribing practice, reasons for not prescribing, views on colleagues’ reasons for non-prescribing and measures that could be put in place to facilitate partnership working. A follow-up questionnaire was posted and the practice manager was phoned as a prompt if there was no response first time around. Five semistructured face-to-face interviews were conducted with three GPs who volunteered when returning their questionnaire and two who were recruited by convenience sampling. Closed questions were analysed using descriptive statistics, while responses to open questions were grouped into themes. The interviews were analysed and peer reviewed using template thematic analysis.3 The study received approval from the Research Governance Committee of the School of Medicine, Dentistry and Biomedical Sciences, Queens University Belfast.
Results
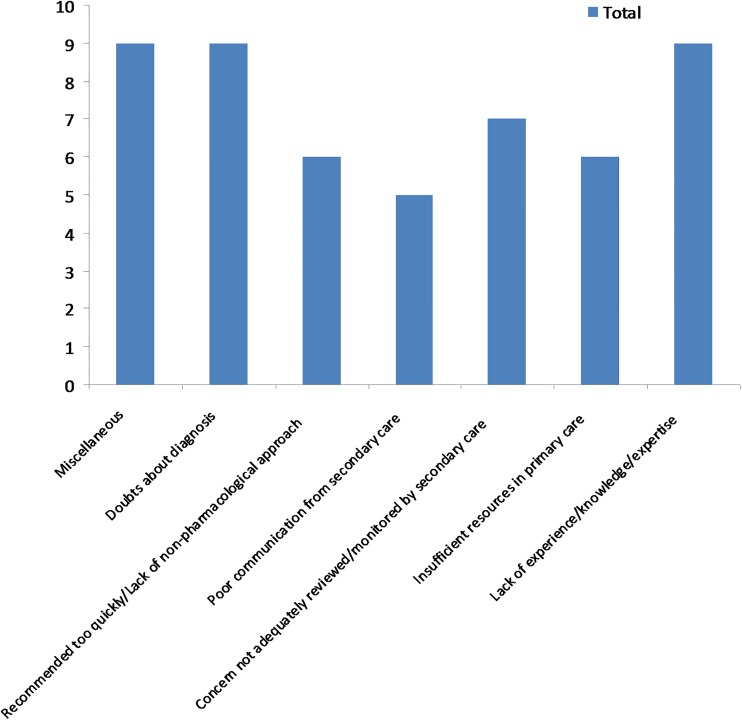
Thirty-five questionnaires were returned giving a response rate of 25%. Twenty-three (66%) GPs indicated that they had prescribed medication for ADHD in the last 3 months, though only 8 (23%) thought that prescribing should be by primary care. The main reasons, as indicated in figure 1, that GPs gave for not prescribing were doubts about the robustness of the diagnosis; lack of use of non-pharmacological treatments; concern that physical monitoring of growth, heart rate and blood pressure would not be performed adequately by secondary care; that patients would not be followed up if they failed to attend hospital appointments and that total responsibility would then default to general practice. There was also a general lack of confidence in managing ADHD related to knowledge levels, personal experience in prescribing, and a general perception that communication from secondary care had been historically poor.
Figure 1.
Results from the thematic analysis of an open-ended questionnaire question; ‘In your opinion why do you think that some GPs do not prescribe for ADHD under shared-care arrangements?’.
While the themes identified from the interviews did not differ substantially from the questionnaire results, it was possible to judge the importance of the themes from the research method used. Two important themes were identified. One concern was that the initial decision to commence medication may not be correct, reflecting the concern that the diagnosis was made too quickly, poor communication of the diagnostic process and lack of non-pharmacological treatments being offered or used. Another key theme was that secondary care may not fulfil its shared-care responsibilities including adequacy of follow-up arrangements and communication of physical monitoring results. Concern caused by GPs’ perception of having a lack of relevant knowledge and experience was also important.
Discussion
Initially, we considered the response rate to be disappointing, but the results did confirm the concern of significant non-engagement of local GPs with shared care of ADHD in children, and in this context of negativity, the 25% response rate could be viewed as relatively good.
Our literature review identified three ADHD English language reports, two from the UK, and one from Australia.4–6 In contrast to our experience, these found a general willingness by GPs to prescribe. This is probably also the situation elsewhere in Northern Ireland given the low level of amber ADHD dispensing from other Trust pharmacy departments. The reasons GPs in these studies gave for not prescribing were a lack of knowledge and experience in managing the condition, lack of non-pharmacological treatments and a perceived risk of misuse or diversion of prescribed medications. Other studies, which investigated shared care of specialist medicines in general, have highlighted concerns relating to the responsibilities for monitoring, paucity of follow-up information from secondary care and practice policies as barriers to be overcome.7–9
Our study identified a perception that medication was being over used or used too early in the diagnostic and treatment process. There were also some concerns regarding the robustness of the diagnosis. Interrogation of this latter point in the interviews suggested that this lack of confidence reflected a perception of the inadequacy of communication about how the diagnosis was reached and not necessarily the correctness of the diagnosis. There was also GP uncertainty about the availability and usage of non-pharmacological modalities. While it is possible that appropriate non-medical measures were being offered and were in place the uncertainty expressed is potentially a compounding factor in undermining confidence in the advice on usage and timing of initiation of pharmacological treatment.
Uncertainty about monitoring and follow-up arrangements was also identified. Some GPs commented that the recommended physical monitoring of patients was not actually being carried out by the hospital specialists. This perception could reflect the lack of communication of the results of growth parameters, heart rate and blood pressure monitoring and not lack of actual measurement. As our study did not examine the primary evidence, we are not in a position to comment further. There was also concern raised about the adequacy of notification to the general practice regarding failure to attend for specialist review. While we are unable to confirm the validity of these perceptions, it is not surprising that there would be reluctance to engage in a shared-care arrangement if there is a perception that monitoring will be inadequate.
Lack of GP experience and knowledge about the condition was also identified as potentially a hindrance to sharing care. While we are unable to comment on how much weight to attribute to this factor, it is probably reasonable to assume that in the presence of other uncertainties, it will contribute to a jigsaw of reasons influencing the decision not to prescribe.
The information from this study has contributed to a review of the local service based on the NICE guidance.1 10 So far, this review has resulted in the introduction of a system of triaging new referrals to ensure that arrangements are in place for comprehensive assessment. There is agreement on the assessment tools to be used and additional resources to further develop non-medical modalities for intervention have been identified. Engagement has also been commenced with the GP Local Medical Committee to review the concerns specified in respect of prescribing and monitoring arrangements. Other measures that we advise should also be undertaken include an exercise to benchmark the prevalence of pharmacological treatment in our LCG area against published standards and introduction of an education programme to meet educational objectives identified in partnership with local GPs.11
Conclusion
The reasons for the reluctance of local GPs to prescribe are probably multifactorial. Perception of poor communication was however a recurring theme that needs to be effectively addressed. Our recommendations for facilitating uptake of shared-care partnerships include improving documentation on how the decision to initiate medication is made, enhancing access to and communicating use of non-pharmacological treatments and ensuring communication of the results of physical monitoring and follow-up.
Acknowledgments
We wish to thank Dr Melissa McCullough, School of Medicine, Dentistry and Biomedical Sciences, Queens University Belfast, Northern Ireland for her support carrying out the study, and all GPs who participated.
Footnotes
Contributors: IMC led the project, devised the research questions, carried out the research and coauthored the manuscript. JMA advised on the design of the research project, interpretation of the findings and coauthored the manuscript. Both parties gave final approval of the published version.
Funding: Northern Ireland Centre for Pharmacy Learning and Development, Northern Health and Social Care Trust.
Competing interests: None declared.
Ethics approval: School of Medicine, Dentistry and Biomedical Sciences, Queens University Belfast.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: The full original research paper is available on request to the lead author.
References
- 1.National Institute for Health and Clinical Evidence. Clinical Guideline 72. Attention deficit hyperactivity disorder. Diagnosis and management of ADHD in children, young people and adults; 2008.
- 2.Northern Ireland Regional Group on Specialist Medicines. Red Amber List December 2012. [Online]. http://www.ipnsm.hscni.net/library/RedAmberList.pdf (accessed 25 Jun 2015).
- 3.King H, Horrocks C. Interviews in qualitative research. London: SAGE publications Ltd., 2010. [Google Scholar]
- 4.Salt N, Parkes E, Scammell A. GPs’ perceptions of the management of ADHD in primary care: a study of Wandsworth GPs. Prim Health Care Res Dev 2005;6:162–71. 10.1191/1463423605pc239oa [DOI] [Google Scholar]
- 5.Ball C. Attention-deficit hyperactivity disorder and the use of methylphenidate: a survey of the views of general practitioners. Psychiatr Bull 2001;25:301–4. 10.1192/pb.25.8.301 [DOI] [Google Scholar]
- 6.Shaw K, Wagner I, Eastwood H, et al. A qualitative study of Australian GPs’ attitudes and practices in the diagnosis and management of attention-deficit/hyperactivity disorder (ADHD). Fam Pract 2003;20:129–34. 10.1093/fampra/20.2.129 [DOI] [PubMed] [Google Scholar]
- 7.Horne R, Mailey E, Frost S, et al. Shared care: a qualitative study of GPs’ and hospital doctors’ views on prescribing specialist medicines. Br J Gen Pract 2001;51:187–93. [PMC free article] [PubMed] [Google Scholar]
- 8.Crowe S, Tully MP, Cantrill JA. The prescribing of specialist medicines: what factors influence GPs’ decision making? Fam Pract 2009;26:301–8. 10.1093/fampra/cmp030 [DOI] [PubMed] [Google Scholar]
- 9.Crowe S, Tully MP, Cantrill JA. Shared care arrangements for specialist drugs in the UK: the challenges facing GP adherence. Qual Saf Health Care 2010;19:e54 10.1136/qshc.2009.035857 [DOI] [PubMed] [Google Scholar]
- 10.National Institute for Health and Clinical Evidence. Attention deficit hyperactivity disorder. NICE quality standard 39. July 2013.
- 11.McCarthy S, Wilton L, Murray ML, et al. The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents and adults in UK primary care. BMC Pediatr 2012;12:78 10.1186/1471-2431-12-78 [DOI] [PMC free article] [PubMed] [Google Scholar]