Abstract
Objective
Osteoporosis is a common disease that is underdiagnosed and undertreated. A multidisciplinary intervention may improve the identification and treatment of osteoporosis and may consequently prevent secondary fractures.
Method
Retrospective, single-centre study comparing attitude to screening and treatment of patients admitted to the orthopaedic unit of the general hospital AZ Sint-Jan Brugge-Oostende AV (Belgium) before and after the implementation of a clinical pathway.
Results
A total of 172 patients (86 before and 86 after) were included in this study. The implementation of the pathway resulted in an increase in bone mineral density tests performed, an increment in the number of referrals to a specialist in the field of osteoporosis, and an increase in prevention and treatment of osteoporosis.
Conclusion
The implementation of a clinical pathway coordinated and evaluated by a clinical pharmacist improved the identification, referral and treatment of osteoporosis in patients hospitalised due to low-impact fractures.
Keywords: CLINICAL PHARMACY, PHARMACOTHERAPY, PRIMARY CARE, PREVENTIVE MEDICINE, RHEUMATOLOGY
EAHP Statement 4: Clinical Pharmacy Services
Introduction
Osteoporosis is a systemic skeletal disease characterised by low bone density and micro-architectural deterioration of bone tissue with a consequent increase in bone fragility, resulting in a higher risk of fractures, particularly of the spine, hip, wrist, humerus and pelvis.1 Hip fracture is one of the most common types of fracture and is regarded as the most devastating type of osteoporotic fracture.2
Osteoporotic fractures result in loss of independence and are associated with significant morbidity and mortality.3 They impose a huge economic burden on health services. The treatment costs of fractures lead to major expenditure, with hip fractures incurring the highest cost.4
Despite the high frequency of osteoporosis, it is still an underdiagnosed and undertreated condition.5 Mehrpour et al6 found in a survey of 515 hospitalised patients with an osteoporotic fracture, that 3.3% had a bone mineral density (BMD) appointment; 8.2% received treatment with calcium and vitamin D and only 3.5% received treatment with calcium and vitamin D in association with a bisphosphonate. Even when low-energy fractures are diagnosed, only a small percentage of patients receive pharmacological therapy.7
However, there is evidence supporting the efficacy of preventive measures and treatments for osteoporosis.3 8 Bisphosphonates combined with calcium and vitamin D are considered the most cost-effective treatment.8 Recently, other antiosteoporotic drugs have been approved for this indication.9
Early identification and treatment of osteoporosis is critical in order to prevent recurrent fractures. This can be improved by developing a clinical pathway.5 A clinical pathway standardises care processes, leading to less variation in care.10 It also optimises the care processes when needed and monitors them continuously, which enhances quality of care.11
Method
Osteoporosis clinical pathway and role of the clinical pharmacist
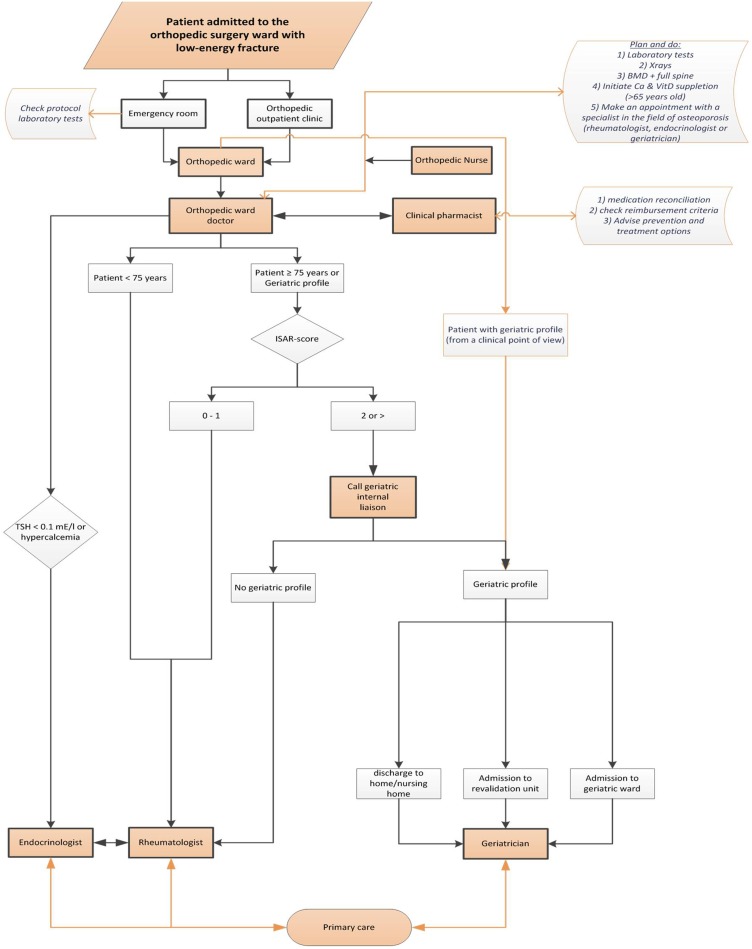
By participating in orthopaedic ward rounds, the clinical pharmacist in our hospital discovered a low prevalence and an inconsistent way of screening and treating osteoporotic fractures, which was raised at the medical staff meeting. Based on multidisciplinary discussions between orthopaedic surgeons, the orthopaedic ward doctor, geriatricians, rheumatologists, endocrinologists and the clinical pharmacist, a clinical pathway was set up in 2013 (figure 1). Adults admitted to the orthopaedic surgery unit of the general hospital with a low-energy fracture were included in the pathway. These patients had a medication reconciliation review, clinical evaluation, laboratory testing, BMD measurement and referral to a specialist in the field of osteoporosis for determination and treatment of osteoporosis. Treatment was initiated when judged appropriate by the designated specialist.
Figure 1.
Clinical pathway: ‘secondary prevention of osteoporotic fractures’. BMD, bone mineral density; ISAR, identification of senior at risk; TSH, thyroid-stimulating hormone.
The clinical pharmacist acted as a project and process manager and was responsible for the implementation, follow-up and evaluation of the clinical pathway. Patient information leaflets and posters were designed and spread throughout the hospital to make staff and patients aware about osteoporotic issues and the clinical pathway. Moreover, for every included patient, the clinical pharmacist performed a medication reconciliation review and gave advice on the intake of calcium and vitamin D preparations.
Study design
The study design was retrospective analysis of records of patients who had been admitted to the orthopaedic ward before (October through December 2010) and after (October through December 2013) implementation of the clinical pathway. Patients admitted for low-energy fractures were included. Age (continuous variable), gender and fracture type (categorical variables) were the demographic variables. The measured values were (1) the completion of BMD screening, (2) a planned consultation with a specialist in the field of osteoporosis (PCO) and (3) the initiation of antiosteoporotic therapy (calcium and vitamin D alone or calcium and vitamin D in addition to an antiosteoporotic drug) (categorical variables).
BMD screening data and T-scores were validated by manual review of the patient record. The PCOs were retrieved by questioning the consulted osteoporotic specialist or by review of the patient record. Information on prescribed medication was obtained from the patient record using the Anatomical Therapeutic Chemical (ATC) classification system codes.
Statistical analysis
All statistical analyses were performed with IBM SPSS Statistics V.20.0 software. Descriptive statistics were computed for all demographic variables. A Shapiro-Wilk test was used to verify the normality of the distribution of the continuous variables. Continuous variables were analysed using the Mann-Whitney test. Categorical variables were evaluated using the χ2 analysis and the Fisher exact test as appropriate. All the statistical tests were two sided, and p<0.05 was considered to be significant.
Results
Demographic data
This study included 86 consecutive patients before and 86 consecutive patients after implementation of the clinical pathway. Fifty patients in the second group completed the clinical pathway. Thirty-six patients did not complete the pathway: 13 were in a serious clinical condition, 6 died during hospitalisation, 10 had started osteoporotic treatment up to 3 years before the fracture, and 7 refused follow-up.
Age, gender and fracture type were similar in the two study groups (p>0.05). The median age was 79 (65–83) years in the group before implementation of the pathway and 82 (71–86) years in the group after implementation of the pathway. The two groups included 77% and 70% women, respectively. Distribution of the type of fracture (non-vertebral, hip, vertebral) was similar in the two groups.
Study results
The results are given in table 1. Before implementation of the clinical pathway, 12% of the patients had BMD screening: 90% had osteopenia (50%) or osteoporosis (40%). After implementation of the clinical pathway, BMD screening was performed in 64% of the patients (p<0.001): 81% were diagnosed with osteopenia (47%) or osteoporosis (34%). The percentage of patients who were referred to a specialist in the field of osteoporosis increased from 14% to 80% (p<0.001). Before implementation of the clinical pathway, no PCOs were performed by an orthopaedic surgeon or orthopaedic unit physician compared with 12% after implementation (p=0.002). There was an increase in PCOs by geriatricians (5% to 30%, p<0.001) and rheumatologists (9% to 38%, p<0.001) after implementation of the clinical pathway. In the group before implementation of the pathway, calcium and vitamin D supplements were started in 30% of the patients, whereas these supplements were initiated in 68% of patients in the group after implementation of the pathway (p<0.001). An additional antiosteoporotic drug was started in 11% and 38% patients, respectively, before and after the implementation of the pathway (p<0.001).
Table 1.
Results before and after implementation of the clinical pathway
| Outcome | Before implementation (n=86) | After implementation* (n=50) | p Value† |
|---|---|---|---|
| BMD tests | 10 (12) | 32 (64) | <0.001 |
| Normal bone | 1 (1) | 6 (12) | |
| Osteopenia | 5 (6) | 15 (30) | |
| Osteoporosis | 4 (5) | 11 (22) | |
| Planned osteoporotic consultation (PCO) | 12 (14) | 40 (80) | <0.001 |
| Orthopaedics | 0 | 6 (12) | 0.002 |
| Geriatrics | 4 (5) | 15 (30) | <0.001 |
| Reumatology | 8 (9) | 19 (38) | <0.001 |
| Endocrinology | 0 | 0 | N/A |
| Appropriate osteoporosis management | |||
| Calcium and vitamin D | 26 (30) | 34 (68) | <0.001 |
| Antiosteoporotic drug | 9 (11) | 19 (38) | <0.001 |
Values are n (%).
*36 patients did not complete the pathway.
†p Values from Fisher’s exact test.
BMD, bone mineral density; N/A, not applicable.
Discussion
In both groups, the most prevalent fracture was hip fracture (42% and 50%), which is in line with the literature.2 After implementation of the clinical pathway, five times more patients underwent a BMD test. Moreover, the number of patients receiving antiosteoporotic pharmacological treatment had doubled. These findings are also consistent with the literature.12–14
The literature indicates that an improvement in appropriate management (prevention and treatment) of osteoporosis minimises fracture risk.3 8
This study has several limitations. First, a clinical end point (fracture reduction or an improvement in quality of life) was not measured, which is similar to other studies.12 14 There is, however, evidence that recurrent fractures can be prevented with good identification and treatment of osteoporosis.12 14
Second, the clinical pathway is subject to selection bias. Patients with an osteoporotic fracture who were hospitalised on a non-orthopaedic unit or were outpatients were missed in this study. This may explain the low percentage of wrist and vertebral fractures. To avoid missing these patients, the clinical pathway should be extended to all hospitalisation and outpatient units.
Third, before implementation of the clinical pathway, there was no unit physician on the orthopaedic unit. At the time of implementation of the clinical pathway, a physician was present. Hence the follow-up of osteoporotic patients may also have been improved by this presence, which may have led to an overestimation of the impact of the instauration of this clinical pathway.
Fourth, patients who are hospitalised for a short time (1–2 days), especially those with a wrist fracture, are often missed from further investigations and follow-up.
Finally, the focus of the study was only on initiation, and not on continuation, of therapy. However, long-term compliance with osteoporotic treatment is particularly low.15 This is mainly due to adverse events and the absence of an immediately observable response to treatment. An improved understanding of the disease and treatment options may increase the compliance of the patient.2 This can be evaluated in further studies and could lead to further adaptation, if necessary.
Conclusion
The clinical pathway for patients with low-energy fractures produces an improvement in identification and treatment of osteoporosis. This improvement reduces the fracture risk, which may consequently result in decreased mortality, morbidity and cost. In this study, there was an increase in BMD screening, referral to a specialist in the field of osteoporosis, and initiation of calcium, vitamin D and antiosteoporotic medication. Further studies should evaluate the effect of screening programmes on fracture reduction.
A clinical pharmacist can contribute to the care of osteoporotic patients through his/her role as coordinator and evaluator in the development of a clinical pathway for the secondary prevention of osteoporotic fractures.
What this paper adds.
What is already known on this subject?
Osteoporosis is an underdiagnosed and undertreated disease associated with significant morbidity, mortality and expenditure.
There is a need for a multidisciplinary intervention to improve the identification, referral and treatment of osteoporosis.
What this study adds?
The implementation of a clinical pathway improved the identification, referral and treatment of osteoporosis in patients hospitalised due to low-impact fractures.
A clinical pharmacist can initiate and contribute to improved care of osteoporotic patients through his/her role as coordinator and evaluator in the development of a clinical pathway for the secondary prevention of osteoporotic fractures.
Footnotes
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Boyce BF, Rosenberg E,de Papp AE, et al. The osteoclast, bone remodelling and treatment of metabolic bone disease. Eur J Clin Invest 2012;42:1332–41. 10.1111/j.1365-2362.2012.02717.x [DOI] [PubMed] [Google Scholar]
- 2.Das S, Crockett JC. Osteoporosis—a current view of pharmacological prevention and treatment. Drug Des Devel Ther 2013;7:435–48. 10.2147/DDDT.S31504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Body JJ, Bergmann P, Boonen S, et al. Evidence-based guidelines for the pharmacological treatment of postmenopausal osteoporosis: a consensus document by the Belgian Bone Club. Osteoporos Int 2010;21:1657–80. 10.1007/s00198-010-1223-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bessette L, Jean S, Lapointe-Garant MP, et al. Direct medical costs attributable to peripheral fractures in Canadian post-menopausal women. Osteoporos Int 2012;23:1757–68. 10.1007/s00198-011-1785-9 [DOI] [PubMed] [Google Scholar]
- 5.Boonen S, Bischoff-Ferrari HA, Cooper C, et al. Addressing the musculoskeletal components of fracture risk with calcium and vitamin D: a review of the evidence. Calcif Tissue Int 2006;78:257–70. 10.1007/s00223-005-0009-8 [DOI] [PubMed] [Google Scholar]
- 6.Mehrpour SR, Aghamirsalim MR, Sorbi R. Are hospitalized patients with fragile fractures managed properly in relation to underlying osteoporosis? J Clin Rheumatol 2012;18:122–4. 10.1097/RHU.0b013e31824ee8af [DOI] [PubMed] [Google Scholar]
- 7.Wong PKK, Spencer DG, McElduff P, et al. Secondary screening for osteoporosis in patients admitted with minimal-trauma fracture to a major teaching hospital . J Intern Med 2003;33:505–10. 10.1046/j.1445-5994.2003.00468.x [DOI] [PubMed] [Google Scholar]
- 8.Giles M, Van Der Kallen J, Parker V, et al. A team approach: implementing a model of care for preventing osteoporosis related fractures. Osteoporos Int 2011;22:2321–8. 10.1007/s00198-010-1466-0 [DOI] [PubMed] [Google Scholar]
- 9.Miyazaki T, Tokimura F, Tanaka S. A review of denosumab for the treatment of osteoporosis. Patient Prefer Adherence 2014;8:463–71. 10.2147/PPA.S46192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vanhaecht K, Van Gerven E, Deneckere S, et al. 7-fasenmodel voor de ontwikkeling, implementatie, evaluatie en continue opvolging van zorgpaden. Ned Tijdschr Geneeskd 2011;67:473–81. [Google Scholar]
- 11.Vanhaecht K, De Witte K, Panella M, et al. Do pathways lead to better organized care processes? J Eval Clin Pract 2009;15:782–8. 10.1111/j.1365-2753.2008.01068.x [DOI] [PubMed] [Google Scholar]
- 12.Jaglal SB, Donescu OS, Bansod V, et al. Impact of a centralized osteoporosis coordinator on post-fracture osteoporosis management: a cluster randomized trial. Osteoporos Int 2012;23:87–95. 10.1007/s00198-011-1726-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Little EA, Eccles MP. A systematic review of the effectiveness of interventions to improve post-fracture investigation and management of patients at risk of osteoporosis. Implement Sci 2010;5:80 10.1186/1748-5908-5-80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leslie WD, LaBine L, Klassen P, et al. Closing the gap in postfracture care at the population level: a randomized controlled trial. CMAJ 2012;184: 290–6. 10.1503/cmaj.111158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Modi A, Sajjan S, Gandhi S. Challenges in implementing and maintaining osteoporosis therapy. Int J Womens Health 2014;6:759–69. 10.2147/IJWH.S53489 [DOI] [PMC free article] [PubMed] [Google Scholar]