Abstract
Objectives:
Over 380 million people in the world live with chronic obstructive pulmonary disease, and it is the third leading cause of death in the United States. Despite updated guidelines, there may be significant variations in diagnosis and management of chronic obstructive pulmonary disease at a primary care level. The aim of the study was to examine primary care physician management of chronic obstructive pulmonary disease in two community clinics.
Methods:
After approval from the Institutional Review Board, a retrospective chart review was done among all patients with the diagnosis of chronic obstructive pulmonary disease in two community clinics. Baseline demographics, utilization of spirometry, exacerbation history and home oxygen use were also obtained.
Results:
Chart reviews of 101 patients were completed (52 male and 49 female) in two outpatient primary care provider offices (Office A: 66 patients and Office B: 35 patients). None of the patients had validated measures of dyspnoea such as CAT or mMRC scores. Only 21% (22/101) of the patients had formal pulmonary function test testing done, and of those who had pulmonary function tests, 31.5% of patients were incorrectly diagnosed and mislabelled as chronic obstructive pulmonary disease. Pharmacotherapy for chronic obstructive pulmonary disease was not in alignment with GOLD guidelines, with only 42% of patients on an inhaler regimen that included a long-acting muscarinic antagonist.
Conclusion:
There is suboptimal use of pulmonary function test in a primary care setting for diagnosis of chronic obstructive pulmonary disease and substantial errors in diagnosis. There is virtually no use routinely of validated symptom scales for diagnosis of chronic obstructive pulmonary disease. There is substantial variance in pharmacotherapy, and regimens routinely do not follow GOLD guidelines.
Keywords: Chronic obstructive pulmonary disease, GOLD, spirometry, compliance with guidelines, obstructive lung disease
Introduction
Chronic obstructive pulmonary disease (COPD) is characterized by chronic inflammation and a slowly progressive persistent airflow obstruction, and affects more than 5% of adults in the United States.1 Despite the availability of well-established recommendations for diagnosis and management, COPD is often misdiagnosed and inappropriately treated in many patients, with approximately 50% of adults with COPD in the United States misdiagnosed or undiagnosed.2–4
Previous studies have demonstrated that despite the clear value and positive impact of clinical practice guidelines in improving the quality of care among patients with such chronic conditions as congestive heart failure, there is substantial suboptimal implementation in adherence to these guidelines in routine clinical practice.5,6 We wished to explore the adherence of Global Initiative for Chronic Obstructive Lung Disease (GOLD) guidelines for COPD among community-based primary care physicians in their management of COPD.
Methods
After approval from the Corpus Christi Medical Center (CCMC) Institutional Review Board (IRB), Corpus Christi, Texas, retrospective chart review was conducted in a primary care clinic of a community hospital for a period of 6 months. Charts reviewed were from two primary care clinics in Corpus Christi. Sequential charts were examined over a 6 months period and were included for review with a primary clinical diagnosis of COPD. Baseline demographic data, COPD exacerbations, tobacco pack year history, usage of home oxygen, availability of spirometry and the objective diagnosis of COPD were assessed. In total, 101 patient charts were reviewed, and assessments were based on GOLD standard guidelines. Once vital information (i.e. sex, race, height, weight, body mass index (BMI) and years with COPD diagnosis) and general lifestyle qualifications (annual tobacco pack usage, continuing tobacco usage and other risk factors) were assessed, further analysis of treatment with adherence to GOLD guidelines was documented. Treatment documented included CAT (COPD assessment test),7 mMRC (Modified Medical Research Centre; dyspnoea test),8 exacerbation frequency (with special focus on night exacerbations) and intubation. Furthermore, combinations of drugs administered to each patient were also recorded in survey format. Medications surveyed for included SABAs (short-acting beta agonists), combinations of SABAs and SAMAs (short-acting muscarinic antagonists), ICS (inhaled corticosteroids), LAMAs (long-acting muscarinic antagonists), combinations of ICS and LABAs (long-acting beta agonists), LAMA and LABA combinations, and LTRAs (leukotriene receptor antagonists). Pulmonary function tests (PFT) information from the preceding 12 months was reviewed and data recorded. In addition, other respiratory function tests, such as Fev1/FVC ratio (forced expiratory volume-one second/forced vital capacity), were measured to gain a better understanding of survey sample characteristics.
Smoking history was classified into three subdivisions: light (less than five cigarettes daily or 13 packs annually), heavy (one or more packs daily) or average (distribution between light and heavy). BMI and sex were included to highlight equal distribution of population among patients surveyed. Patients were further surveyed on the topic of general medication combinations (listed above) in adherence to the GOLD protocol for COPD.
Results
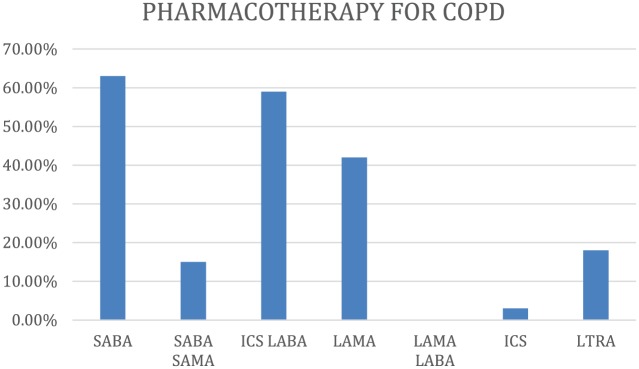
Chart reviews of 101 patients were completed (52 male and 49 female) in two outpatient primary care provider (PCP) offices (Office A: 66 patients and Office B: 35 patients). Figure 1 details a demographic overview of the sample size. 79.21% were current or former smokers. The majority of patients fell between the age distributions of 60–90 years.
Figure 1.
Demographic data.
The review indicated a glaring discrepancy in adherence to GOLD protocol in both of these clinics. Out of the 66 patients in Clinic 1 and 35 in Clinic 2 surveyed, only 28.79% and 8.57%, respectively, underwent spirometry as part of their COPD examination (Figure 2).
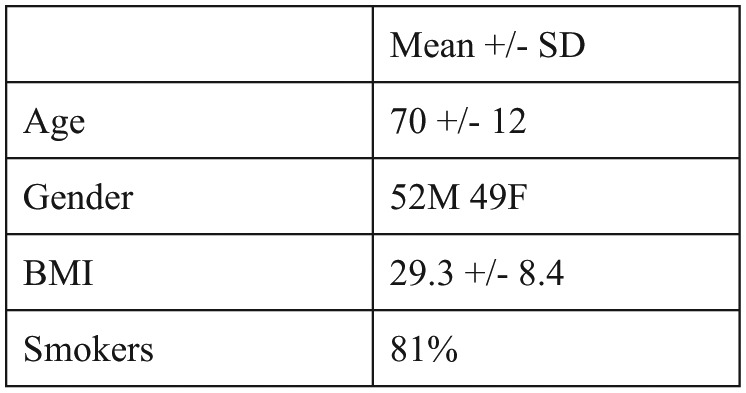
Figure 2.
Medication combination frequency of Clinic 1 COPD-afflicted patients.
Strikingly, 0% of the patients across both clinics underwent CATs or mMRC for dyspnoea testing.
Pulmonary function test (PFT) is vital to establishing the diagnosis of COPD – as per GOLD guidelines, a diagnosis of COPD requires a post-bronchodilator FEV1 of <80%. There was a paucity of PFT testing in both clinics – less than one-third of patients (only 28%) had PFTs, and in Clinic 2, a mere 8.6% had PFTs. Moreover, in the patients who actually did have PFTs, a diagnosis of COPD could be substantiated in only 69% – only 13 of the 19 patients met criteria for the diagnosis of COPD, whereas 31% of patients were incorrectly labelled as COPD.
There was also substantial variance in pharmacotherapy regimens in treatment. Only 42.42% of patients in total were given LAMAs to treat symptoms (Figure 2), whereas 62% of patients were given an inhaler regimen that included an ICS.
Discussion
The GOLD guidelines were developed and are frequently revised with the goal of standardizing care of patients with COPD. Despite the best intentions, the effectiveness of clinical practice guidelines is only as good as its implementation. This study highlights the suboptimal adherence to these guidelines in routine primary care management of COPD. This raises critical questions with regard to the relevance of these guidelines in clinical practice and measures we may implement to enhance their relevance.
Significant numbers of patients in the community clinics were either diagnosed clinically with COPD or wrongly labelled as COPD. There was significant variation seen in getting the spirometry or any attempt to accurately diagnose the patients with COPD.9
This is consistent with a previous Swiss study looking at primary care practitioners’ adherence to GOLD guidelines.10 In that study, prescription non-conformity was frequent in patients with GOLD stage I and II COPD (69% and 82% of patients, respectively) with conformity improving with more advanced COPD. 44% of the patients recruited not to have overt COPD, according to the GOLD criteria. Evaluation of subjective symptoms via CAT or mMRC in addition to exacerbation history has been the key aspect of the updated GOLD Guidelines since 2011, but in our primary care setting, a validated assessment of subjective symptoms with use of either the CAT or mMRC questionnaires was not utilized in any of the patients with the diagnosis of COPD.
Our study showed a significant underutilization of spirometry in a primary care setting in our community. A recent epidemiological survey, among more than 1.5 million members of insurance organizations, showed that only 32% of patients with a new COPD diagnosis had undergone spirometry in the previous 2 years to 6 months following diagnosis.11
The data presented demonstrated heterogeneity in pharmacotherapy for COPD and choice of inhaler use that was inconsistent with updated GOLD standards for treatment. Prescription of LAMAs was both inconsistent and suboptimal despite the latest iteration of GOLD guidelines, clearly highlighting their role in the management of COPD.
Only 42.42% of patients were treated with any type of combination which involved LAMA medication, while SABA or ICS (which are generally fast-acting) were far more prevalent as treatment options. There are critical concerns about routine use of ICS in COPD. In our study, 62% of patients with COPD were prescribed ICS usually as an ICS LABA dual therapy combination inhaler.12
GOLD guidelines specify a post-bronchodilator FEV1 as a ‘sine qua non’ of COPD diagnosis, and yet, this study illumines a significant underutilization of spirometry in diagnosing COPD in a primary care practice.
There are limitations to our study. This was a small study and involved only two sites and was a retrospective chart review. It may be hence prudent not to generalize the findings and a much larger sample size may be required to see if these results are reproduced. However, the data do appear to be consistent with earlier trials both in the US and internationally. A review of 11 studies shows significant variability in adherence to the GOLD guidelines. Barriers identified include lack of clarity, unfamiliarity with recommendations and lack of familiarity with the guidelines.
Conclusion
The best guidelines in the world do not improve treatment if they are not implemented. Our data highlight the critical need for knowledge to action framework to vigorously enhance provider education in primary care about the updated GOLD guidelines for COPD. Moreover, measures to enhance physician behaviour besides just providing education need to be implemented.
Footnotes
Author’s note: Abstract submission: the portion of this data has been presented in the CHEST meeting October 2016, Volume 150 Issue 4: 155a, 834a, 838a, 1070a.
Data availability: The raw data are available on request with the corresponding author.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval was obtained from the Corpus Christi Medical Center (CCMC) Institutional Review Board (IRB), Corpus Christi, TX, USA.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Informed consent was waived by the Institutional Review Board (IRB).
ORCID iD: Salim Surani  https://orcid.org/0000-0001-7105-4266
https://orcid.org/0000-0001-7105-4266
References
- 1. Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet 2012; 379: 1341–1351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J 2017; 49: 1700214. [DOI] [PubMed] [Google Scholar]
- 3. Miravitlles M, Soler-Cataluña JJ, Calle M, et al. Spanish COPD guidelines (GesEPOC) 2017: pharmacological treatment of stable chronic obstructive pulmonary disease. Arch Bronconeumol 2017; 53: 324–333. [DOI] [PubMed] [Google Scholar]
- 4. Wise RA, Tashkin DP. Preventing chronic obstructive pulmonary disease: what is known and what needs to be done to make a difference to the patient? Am J Med 2007; 120(8 Suppl. 1): S14–S22. [DOI] [PubMed] [Google Scholar]
- 5. Stork S, Hense HW, Zentgraf C, et al. Pharmacotherapy according to treatment guidelines is associated with lower mortality in a community-based sample of patients with chronic heart failure: a prospective cohort study. Eur J Heart Fail 2008; 10(12): 1236–1245. [DOI] [PubMed] [Google Scholar]
- 6. Calvin JE, Shanbhag S, Avery E, et al. Adherence to evidence-based guidelines for heart failure in physicians and their patients: lessons from the Heart Failure Adherence Retention Trial (HART). Congest Heart Fail 2012; 18(2): 73–78. [DOI] [PubMed] [Google Scholar]
- 7. Jones PW, Harding P, Berry P, et al. Development and first validation of the COPD assessment test. Eur Respir J 2009; 34(3): 648–654. [DOI] [PubMed] [Google Scholar]
- 8. Mahler DA, Wells CK. Evaluation of clinical methods for rating dyspnea. Chest 1988; 93(3): 580–586. [DOI] [PubMed] [Google Scholar]
- 9. Gold PM. The 2007 GOLD guidelines: a comprehensive care framework. Respir Care 2009; 54(8): 1040–1049. [PubMed] [Google Scholar]
- 10. Jochmann A, Neubauer F, Miedinger D, et al. General practitioners’ adherence to the COPD GOLD guidelines: baseline data from the Swiss COPD Cohort Study. Swiss Med Wkly 2010; 140: w13053. [DOI] [PubMed] [Google Scholar]
- 11. Han MK, Kim MG, Mardon R, et al. Spirometry utilization for COPD. How do we measure up? Chest 2007; 132(2): 403–409. [DOI] [PubMed] [Google Scholar]
- 12. Sehl J, O’Doherty J, O’Connor R, et al. Adherence to COPD management guidelines in general practice? A review of the literature. Ir J Med Sci 2018; 187(2): 403–407. [DOI] [PubMed] [Google Scholar]