Abstract
Objectives:
Pain is considered the most common and debilitating symptom reported by patients affected by cancer, and opioids are at the front line for its effective management. However, the appropriate use of opioids can be limited by healthcare professionals’ perceptions on opioids. Therefore, the aim of this study was to explore their perceptions on the use of opioids medication.
Methods:
This was a study of sequential mixed-method design conducted in Cyprus. As part of the quantitative phase of the study, the Barriers to Opioid Analgesic Availability Test questionnaire was completed by 73 physicians randomly selected. In the qualitative phase, 28 healthcare professionals working in primary and secondary healthcare centers participated in two focus groups. They were asked to express their perceptions on the use of opioid analgesics for the treatment of cancer-related pain. Data were analyzed according to Colaizzis’ seven-stage phenomenological analysis.
Results:
The quantitative analysis showed that 69.85% of physicians acknowledge opiophobia as a main barrier to appropriate pain relief but also explicitly for cancer pain which is not adequately managed (45.19%). In terms of opioids availability, physicians stated that moderate to severe problems in opioids availability were mainly caused by their reluctance to prescribe opioids (49.3%) followed by the laws/regulations in place (41.08%). The qualitative analysis yielded the following six main themes: inadequate training of healthcare professionals in the use of opioid analgesics, inadequate patient/caregivers’ awareness of opioid analgesics, opiophobia in healthcare professionals, opiophobia of patients/caregivers, poor management of opioid analgesics by healthcare professionals and patients/caregivers, and ineffective pain relief with opioids.
Conclusions:
The lack of appropriate education is a significant barrier to opioids use in Cyprus. This is compounded by the attitudes and phobias of both healthcare professionals and the general public. In addition, there are barriers to opioid availability and unsatisfactory cancer pain relief.
Keywords: Opioids, pain management, healthcare professionals, perception
Introduction
The International Association for the Study of Pain and the World Health Organization define pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Pain is the defining feature for many disease diagnoses, and it is considered among the most common, persistent, and depilating symptoms experienced by patients with malignant tumors. Moving from the status of being “the fifth vital sign,” pain has been utilized as an index of the severity and activity of an underlying condition, a prognostic indicator, and a determinant of health service use.2,3 To this end, chronic pain is no longer considered solely as a symptom, but rather a disease, classified as R 52.1 under the name of intractable disease, in the 11th Revision of the International Classification of Diseases (ICD11).4
In the early 1980s, the state of under-reliance of opioid analgesics and a resultant under-treatment of pain in Europe and North America is recorded as a world-wide phenomenon called “opiophobia.”5,6 However, since the late 1980s, the holistic pain management was formally established as the central focus of relief in a clinical setting, in education, and in research.7 The World Health Organization addressed the under-treatment of postoperative and cancer pain (CP) in 1986 with their Cancer Pain Monograph.8 This was followed by the “pain as the fifth vital sign” campaign launched by the American Pain Society (APS) in 1995, aiming to encourage proper, standardized evaluation and treatment of pain symptoms.9 Furthermore, in the United States, the Joint Commission (TJC) published standards for pain management in 2000, emphasizing the need for organizations to conduct quantitative assessments of pain as recommended by the Institute of Medicine.9
Coinciding with this shift in medical perspective in relation to pain management was the introduction and extensive marketing of oxycodone for the treatment of non-malignant pain.10 The rapid institution of strict standards for pain management in hospital systems in combination with pharmaceutical companies heavily pushing the use of opioids as a humane treatment option has contributed to the opioids epidemic.
This epidemic has triggered response in both sides of the Atlantic. The European Union Drugs Strategy 2013–2020 outlines a “five-pillar” approach to tackling drug use. The strategy promotes a balanced perspective, placing equal emphasis on two policy areas—reduction of drug demand and the reduction of drug supply. Supporting these two policy areas are three cross-cutting themes—coordination, international cooperation, and research and evaluation.11 In the United States, changes in focus to the development of new abuse deterrent opioid formulations at the US Food and Drug Administration (FDA) as well as drafting of new public standards for pain treatment were created at TJC in 2017.12
The prevalence of pain remains high despite costly, well-intentioned medical responses, which rely mainly on pharmaceuticals and high-tech interventions.13 In Europe, about 20% of the population suffers from chronic pain,14 while population-based estimates of chronic pain among US adults range from 11% to 40%.15 There have been significant advances in the management of CP with the use of opioid analgesics, and there is recognition of the need for more work in this field because healthcare professionals (HCPs) face barriers in the delivery or prescription of these drugs resulting from their own practices or other exogenous factors.16 Despite the fact that some of these barriers have been described in the context of effective pain management for patients with malignant tumors, there has not yet been a really thorough investigation of the issue from an interdisciplinary perspective.
Aim of the study
The aim was to explore the possible barriers in opioids use among HCPs.
Methods
Study design
The study utilized a sequential mixed-methods design in order to elicit the perspectives of HCPs on the barriers in the use of opioid analgesics in the management of CP. The quantitative part of the study was informed by descriptive methodology and included exploring the perspectives of physicians on the use of opioid analgesics, followed by the qualitative part which was informed by the descriptive phenomenological approach, where HCPs including physicians (medical oncologists, anesthesiologists, and palliative care specialists), cancer nurses, and psychologists participated in two focus groups in order to further explore their views on the same topic. The qualitative part of the study is reported against the Consolidated Criteria for Reporting Qualitative Studies-COREQ (Supplementary material).
Study population
In the quantitative phase of the study, the participants were solely physicians, since in Cyprus only physicians can prescribe medication. The sample consisted of 73 physicians randomly selected from the Cyprus Medical Association registry. The sample size was based on the aim of the research team to reach at least one-third of the physicians who utilize opioid prescribing within their routine clinical practice (these physicians are estimated to be 230 according to the records of the Cyprus Medical Association Registry).
The qualitative phase consisted of 28 HCPs purposively selected and divided in two equal focus groups of 14 individuals each. Only one nurse from the initially identified participants refused to take part in the study due to her absence abroad. An alternative participant was invited accordingly. The participants consisted of 9 physicians (oncologists, pain physicians, anaesthesiologist, hematologist, pediatricians), 18 nurses (oncology/hematology/pediatric oncology, outpatient surgeries, supportive, and day care), and 1 clinical psychotherapist. The physicians were selected from those that participated in the quantitative part of the study, and the other professionals were purposively chosen based on their involvement in clinical pain management practices.
Measures
Instrument
The Barriers to Opioid Analgesic Availability Test (BOAT) questionnaire was developed by the Pain and Policy Studies Group, specifically to be used in the evaluation of HCPs’ beliefs relating to the barriers which deter opioid availability.17 Access to Opioid Medication in Europe (ATOME) has adopted this instrument and advocates its use among member countries as a mean to identify barriers so that steps can be taken to develop action plans aimed at removing any obstacles which are believed to exist.
The Likert-type Scale Inventory was designed to look at the relative importance of each item, in order to reach a consensual agreement among the stakeholders regarding which barrier was likely to be the most serious.17 This original questionnaire consists of three sections: Demographics and questions related to experience in pain management; section two is divided into three parts related to pain in cancer patients, pain in AIDS/HIV, and other types of pain; and the third section examines possible barriers related to the use of opioids in various situations.
The questionnaire was originally designed for use among interdisciplinary HCPs and needed to be adjusted for use by Cypriot physicians. Approval for using and modifying the BOAT questionnaire was obtained by ATOME. With ATOME’s permission, certain changes were made to the demographics, and the age category was added aimed to examine the relationship between knowledge and physicians’ age. “Profession” was replaced by “specialty,” thus aiming to examine the relationship between the expressed respondents’ opinions and specialties.
Two independent bilingual HCPs translated the questionnaire from English to Greek and then back-translated from Greek to English. Comparison was made with the original version of BOAT in order to assess accuracy, and the Greek version was then pretested in a pilot to check for coherent fluency of the instrument. The pilot study included 15 respondents and the results showed no misconceptions or levels of ambivalence. When questioned about their understanding of the content, the respondents showed that they had clearly understood and did not require clarification on any of the questions. Therefore, questionnaire was deemed suitable for the final study.
Based on the quantitative data’s analysis, the questions constituted the basis (as identified issues related to appropriate opioid use) for the second phase of the study that included the focus groups. The research team considered that the focus groups’ participants will be able to better express and elaborate on their perspectives if the venue was outside the clinical setting. Therefore, it was decided that both focus groups to be undertaken at a venue other than the hospital (i.e. hotel). The aim was to provide a more in-depth analysis to the issues that emerged in the quantitative phase (e.g. opiophobia). The HCPs of both groups were invited to express their views on the question: “what is your opinion on the management of opioid analgesics in relieving CP in Cyprus?” Both groups were facilitated by A.C. (BSc, MSc, PhD) who is an experienced researcher and academic with a special interest in pain management. The facilitator holds specific training and expertise in qualitative studies and his work includes both quantitative and qualitative studies. Prior to participation in the focus groups, all participants were informed about the facilitator’s interest on the topic as well as the reasons for undertaking this study. Only the 28 HCPs took part in the focus groups. The focus groups were audio recorded and transcribed verbatim additionally to the field notes kept by the research team.
Statistical analysis
Quantitative data were analyzed using the R statistical package, which assisted in the calculation of frequencies and proportions of the responses to each question (Tables 1–5). The responses were then cross tabulated with the affiliation groups and significant results were displayed in Tables 6 and 7. The same procedure was then repeated for each question and various age groups (below 50 years and above 50 years)—the significant results of which are shown in Table 8. The purpose of this was to compare each variable against the other and to calculate proportions of each column to the variation as a proportion in each category (affiliations and age groups). The p value (based on Chi-square/Fisher test) was reported for each cross-tabulation and standard practice was followed; that is, the null hypothesis of no statistical dependency between two variables was rejected if the p value was close to 5% or less.
Table 1.
Distribution of responses relating to HIV/AIDS pain (distribution of physicians’ responses for each of the possible barriers to opioid use in the management of HIV-/AIDS-related pain; n = 73).
| Not a problem | Minor problem | Moderate problem | Serious problem | Do not know | No response | |
|---|---|---|---|---|---|---|
| Prescription forms | 6 (8.21%) | 4 (5.47%) | 2 (2.73%) | 6 (8.21) | 50 (68.49%) | 5 (6.84%) |
| Program licensing | 2 (2.73%) | 2 (2.73%) | 0 | 5 (6.84%) | 58 (79.45%) | 6 (6.84%) |
| Shortage of opioids | 5 (6.84%) | 6 (8.21%) | 3 (4.10%) | 2 (2.73%) | 49 (67.12%) | 8 (10.95%) |
| Physicians | 9 (12.32%) | 0 | 8 (10.95%) | 5 (6.84%) | 44 (60.27%) | 7 (9.58%) |
| Pharmacists | 1 (1.36%) | 4 (5.47%) | 3 (4.10%) | 10 (13.68%) | 49 (67.12%) | 6 (8.21%) |
| Nurses | 5 (6.84%) | 3 (4.10%) | 3 (4.10%) | 6 (8.21%) | 50 (68.49%) | 6 (8.21%) |
| Patients | 7 (9.58%) | 4 (5.47%) | 8 (10.95%) | 1 (1.36%) | 46 (63.01%) | 7 (7.58%) |
| Costs | 8 (10.95%) | 2 (2.73%) | 7 (9.58%) | 2 (2.73%) | 48 (65.75%) | 6 (8.21%) |
| Doses | 6 (8.21%) | 8 (10.95%) | 2 (2.73%) | 4 (5.47%) | 45 (61.64%) | 8 (10.95%) |
| Regulations | 4 (5.47%) | 2 (2.73%) | 6 (8.20%) | 11 (15.06%) | 44 (60.27%) | 6 (8.21%) |
| Availability for home use | 2 (2.73%) | 6 (8.21) | 3 (4.10%) | 10 (13.69%) | 45 (61.64%) | 7 (9.58%) |
| Physician licensing | 7 (9.58%) | 3 (4.10%) | 2 (2.73%) | 3 (4.10%) | 52 (71.23%) | 6 (8.21%) |
Table 2.
Merged distribution of responses relating to HIV/AIDS pain (merged distribution of physicians’ responses for each of the possible barriers to opioid use in the management of HIV-/AIDS-related pain; n = 73).
| Not a problem–minor problem | Moderate problem–serious problem | Do not know | No response | |
|---|---|---|---|---|
| Prescription forms | 10 (13.68%) | 8 (10.94%) | 50 (68.49%) | 5 (6.84%) |
| Program licensing | 4 (5.46%) | 5 (6.84%) | 58 (79.45%) | 6 (6.84%) |
| Shortage of opioids | 11 (15.05) | 5 (6.84%) | 49 (67.12%) | 8 (10.95%) |
| Physicians | 9 (12.32%) | 13 (17.79%) | 44 (60.27%) | 7 (9.58%) |
| Pharmacists | 5 (6.84%) | 13 (17.79%) | 49 (67.12%) | 6 (8.21%) |
| Nurses | 8 (10.94%) | 9 (12.31%) | 50 (68.49%) | 6 (8.21%) |
| Patients | 11 (15.05%) | 9 (12.31%) | 46 (63.01%) | 7 (7.58%) |
| Costs | 10 (13.68%) | 9 (12.32%) | 48 (65.75%) | 6 (8.21%) |
| Doses | 14 (19.16%) | 6 (8.2%) | 45 (61.64%) | 8 (10.95%) |
| Regulations | 6 (8.20%) | 17 (23.27%) | 44 (60.27%) | 6 (8.21%) |
| Availability for home use | 8 (10.94%) | 13 (17.79%) | 45 (61.64%) | 7 (9.58%) |
| Physician licensing | 10 (13.68%) | 5 (6.84%) | 52 (71.23%) | 6 (8.21%) |
Table 3.
Distribution of responses relating to other types of pain (n = 73; distribution of physicians’ responses for each of the possible barriers to opioid use in the management of other types of pain (non-cancer/non-HIV/AIDS)).
| Not a problem | Minor problem | Moderate problem | Serious problem | Do not know | No response | |
|---|---|---|---|---|---|---|
| Prescription forms | 19 (26.02%) | 10 (13.69%) | 6 (8.21%) | 7 (9.58%) | 26 (35.61%) | 5 (6.84%) |
| Program licensing | 10 (13.69%) | 10 (13.69%) | 6 (8.21%) | 9 (12.32%) | 34 (46.57%) | 4 (5.47%) |
| Shortage of opioids | 16 (21.91%) | 10 (13.69%) | 5 (6.84%) | 10 (13.69%) | 28 (38.35%) | 4 (5.47%) |
| Physicians | 13 (17.80%) | 7 (9.58%) | 14 (19.17%) | 18 (24.65%) | 17 (23.28%) | 4 (5.47%) |
| Pharmacists | 4 (5.47%) | 6 (8.21%) | 6 (8.21%) | 16 (21.91%) | 36 (49.31%) | 5 (6.84%) |
| Nurses | 8 (10.95%) | 5 (6.84%) | 13 (17.80%) | 15 (20.54%) | 28 (38.35%) | 4 (5.47%) |
| Patients | 16 (21.91%) | 7 (9.58%) | 18 (24.65%) | 8 (10.95%) | 20 (27.39%) | 4 (5.47%) |
| Costs | 11 (15.06%) | 10 (13.69%) | 10 (13.69%) | 3 (4.10%) | 35 (47.94%) | 4 (5.47%) |
| Doses | 13 (17.80) | 13 (17.80%) | 9 (12.32%) | 7 (9.58%) | 27 (36.98%) | 4 (5.47%) |
| Regulations | 3 (4.10%) | 6 (8.21%) | 14 (19.17%) | 17 (23.28%) | 29 (39.72%) | 4 (5.47%) |
| Unavailable for home use | 4 (5.47%) | 9 (12.32%) | 12 (16.43%) | 19 (26.02%) | 25 (34.24%) | 4 (5.47%) |
| Physician licensing | 11 (15.06%) | 5 (6.84%) | 8 (10.95%) | 4 (5.47%) | 39 (53.42%) | 6 (8.21%) |
Table 4.
Merged distribution responses relating to other types of pain (n = 73; merged distribution of physicians’ responses for each of the possible barriers to opioid use in the management of other types of pain (non-cancer/non-HIV/AIDS)).
| Not a problem–minor problem | Moderate problem–serious problem | Do not know | No response | |
|---|---|---|---|---|
| Prescription forms | 29 (39.71%) | 13 (17.79%) | 26 (35.61%) | 5 (6.84%) |
| Program licensing | 20 (27.38%) | 15 (20.53%) | 34 (46.57%) | 4 (5.47%) |
| Shortage of opioids | 26 (35.60%) | 15 (20.53%) | 28 (38.35%) | 4 (5.47%) |
| Physicians | 20 (27.38%) | 32 (43.82%) | 17 (23.28%) | 4 (5.47%) |
| Pharmacists | 10 (13.68%) | 22 (30.12%) | 36 (49.31%) | 5 (6.84%) |
| Nurses | 13 (17.79%) | 28 (38.34%) | 28 (38.34%) | 4 (5.47%) |
| Patients | 23 (31.49%) | 26 (35.60%) | 20 (27.39%) | 4 (5.47%) |
| Costs | 21 (28.75%) | 13 (17.79%) | 35 (47.94%) | 4 (5.47%) |
| Doses | 26 (35.60%) | 16 (21.90%) | 27 (36.98%) | 4 (5.47%) |
| Regulations | 9 (12.31%) | 31 (42.45%) | 29 (39.72%) | 4 (5.47%) |
| Unavailable for home use | 13 (17.79%) | 31 (24.45%) | 25 (34.24%) | 4 (5.47%) |
| Physician licensing | 16 (21.90%) | 12 (16.42%) | 39 (53.42%) | 6 (8.21%) |
Table 5.
Distribution of physicians’ opinions on opioid-related situations (n = 73).
| Strongly disagree | Somewhat disagree | Somewhat agree | Strongly agree | Do not know | No response | |
|---|---|---|---|---|---|---|
| CP not adequately treated | 7 (9.58%) | 17 (23.28%) | 18 (24.65%) | 15 (20.54%) | 12 (16.43%) | 4 (5.47%) |
| AIDS pain not adequately treated | 1 (1.36%) | 3 (4.10%) | 9 (12.32%) | 7 (9.58%) | 49 (67.12%) | 4 (5.47%) |
| Surgical pain not adequately treated | 17 (23.28%) | 19 (26.02%) | 15 (20.54%) | 6 (8.21%) | 13 (17.80%) | 3 (4.10%) |
| Trauma pain not adequately treated | 15 (20.54%) | 17 (23.28%) | 18 (24.65%) | 7 (9.58%) | 13 (17.80%) | 3 (4.10%) |
| Chronic non-malignant pain not adequately treated | 5 (6.84%) | 15 (20.54%) | 19 (26.02%) | 16 (21.91%) | 15 (20.54%) | 3 (4.10%) |
| Obstetric pain not adequately treated | 11 (15.06%) | 10 (13.69%) | 10 (13.69%) | 2 (2.73%) | 37 (50.68%) | 3 (4.10%) |
| No recent improvement in opioid availability | 6 (8.21%) | 14 (19.17%) | 8 (10.95%) | 9 (12.32%) | 33 (45.20%) | 3 (4.10%) |
| Opioids not available for pediatric CP | 1 (1.36%) | 3 (4.10%) | 3 (4.10%) | 6 (8.21%) | 57 (78.08%) | 3 (4.10%) |
| Opioids not available for pediatric AIDS pain | 0 | 2 (2.73%) | 1 (1.36%) | 5 (6.84%) | 61 (83.56%) | 4 (5.47%) |
| Inadequate educational opportunities | 3 (4.10%) | 5 (6.84%) | 20 (27.39%) | 36 (49.31%) | 6 (8.21%) | 3 (4.10%) |
| Fears about dependence interfere with CP management | 5 (6.84%) | 8 (10.95%) | 27 (36.98%) | 24 (32.87%) | 6 (8.21%) | 3 (4.10%) |
| Fears about dependence interfere with management of AIDS pain | 0 | 3 (4.10%) | 17 (23.28%) | 9 (12.32%) | 40 (54.79%) | 4 (5.47%) |
| Opioids are not always available out-of-hours | 4 (5.47%) | 6 (8.21%) | 20 (27.39%) | 19 (26.02%) | 20 (27.39%) | 4 (5.47%) |
| Strict controls lead to use of weaker analgesics in CP | 6 (8.21%) | 5 (6.84%) | 19 (26.02%) | 25 (34.24%) | 14 (19.17%) | 4 (5.47%) |
CP: cancer pain.
Table 6.
Attitudes of physicians in relation to affiliations where p value is less than 5% (n = 73).
| Characteristic | Private, n (%) | Public, n (%) | Other, n (%) | p value |
|---|---|---|---|---|
| Opioid shortages (cancer) | ||||
| Not a problem | 8 (28.6) | 12 (60.0) | 3 (15.0) | |
| Minor problem | 4 (14.2) | 0 (0.0) | 1 (5.0) | |
| Moderate problem | 2 (7.1) | 2 (10.0) | 2 (10.0) | |
| Serious problem | 1 (3.6) | 1 (5.0) | 1 (5.0) | |
| Do not know | 13 (46.4) | 5 (25.0) | 13 (65.0) | 0.05 |
| Physician’s reluctance to prescribe (cancer) | ||||
| Not a problem | 12 (42.9) | 3 (14.3) | 1 (5.0) | |
| Minor problem | 2 (7.1) | 2 (9.5) | 2 (10.0) | |
| Moderate problem | 10 (35.7) | 7 (33.3) | 1 (5.0) | |
| Serious problem | 2 (7.1) | 6 (28.6) | 10 (50.0) | |
| Do not know | 2 (7.1) | 3 (14.3) | 6 (30.0) | 0.0004 |
| Doses and dosages (cancer) | ||||
| Not a problem | 8 (28.6) | 8 (38.1) | 1 (4.8) | |
| Minor Problem | 4 (14.3) | 5 (23.8) | 5 (23.8) | |
| Moderate problem | 7 (25.0) | 4 (19.0) | 1 (4.8) | |
| Serious problem | 1 (3.6) | 1 (4.8) | 3 (14.3) | |
| Do not know | 8 (28.6) | 3 (14.3) | 11 (52.3) | 0.027 |
| Difficulty in obtaining for home use (cancer) | ||||
| Not a problem | 2 (7.1) | 6 (28.6) | 0 (0.0) | |
| Minor problem | 6 (21.4) | 1 (4.8) | 4 (19.0) | |
| Moderate problem | 5 (17.8) | 4 (19.0) | 2 (9.5) | |
| Serious problem | 5 (17.8) | 7 (33.3) | 6 (28.6) | |
| Do not know | 10 (35.7) | 3 (14.3) | 9 (42.9) | 0.055 |
| Physician’s reluctance to prescribe (HIV/AIDS) | ||||
| Not a problem | 7 (26.9) | 2 (10.0) | 0 (0.0) | |
| Minor problem | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Moderate problem | 2 (7.8) | 4 (20.0) | 2 (10.0) | |
| Serious problem | 0 (0.0) | 1 (5.0) | 4 (20.0) | |
| Do not know | 17 (65.4) | 13 (65.0) | 14 (70.0) | 0.026 |
| Nurse reluctance to administer (HIV/AIDS) | ||||
| Not a problem | 4 (15.4) | 1 (5.0) | 0 (0.0) | |
| Minor problem | 3 (11.5) | 0 (0.0) | 0 (0.0) | |
| Moderate problem | 1 (3.8) | 1 (5.0) | 1 (4.8) | |
| Serious problem | 0 (0.0) | 4 (20.0) | 2 (9.5) | |
| Do not know | 18 (69.3) | 14 (70.0) | 18 (85.7) | 0.048 |
| Cost prohibitive for patients (HIV/AIDS) | ||||
| Not a problem | 8 (30.8) | 0 (0.0) | 0 (0.0) | |
| Minor problem | 1 (3.8) | 0 (0.0) | 1 (4.8) | |
| Moderate problem | 1 (3.8) | 3 (15.0) | 3 (14.3) | |
| Serious problem | 0 (0.0) | 1 (5.0) | 1 (4.8) | |
| Do not know | 16 (61.6) | 16 (60.0) | 16 (76.1) | 0.006 |
Table 7.
Attitudes of physicians in relation to affiliations where p value is less than 5% (n = 73).
| Characteristics | Private, n (%) | Public, n (%) | Other, n (%) | p value |
|---|---|---|---|---|
| Prescription forms not available when needed (other) | ||||
| Not a problem | 9 (33.3) | 7 (33.3) | 3 (15.0) | |
| Minor problem | 8 (29.6) | 2 (9.5) | 0 (0.0) | |
| Moderate problem | 2 (7.4) | 4 (19.0) | 0 (0.0) | |
| Serious problem | 2 (7.4) | 2 (9.5) | 3 (15.0) | |
| Do not know | 6 (22.2) | 6 (28.6) | 14 (70.0) | 0.004 |
| Cost prohibitive for patients (other) | ||||
| Not a problem | 7 (25.9) | 3 (14.3) | 1 (4.7) | |
| Minor problem | 8 (29.6) | 0 (0.0) | 2 (9.5) | |
| Moderate problem | 2 (7.4) | 4 (19.1) | 4 (19.0) | |
| Serious problem | 0 (0.0) | 2 (9.5) | 1 (4.7) | |
| Do not know | 10 (37.0) | 12 (57.1) | 13 (61.9) | 0.019 |
| Difficulty in obtaining for home use (other) | ||||
| Not a problem | 3 (11.1) | 1 (4.8) | 0 (0.0) | |
| Minor Problem | 9 (33.3) | 0 (0.0) | 0 (0.0) | |
| Moderate problem | 2 (7.4) | 6 (28.6) | 4 (19.1) | |
| Serious problem | 6 (22.2) | 5 (23.8) | 8 (38.1) | |
| Do not know | 7 (25.9) | 9 (42.8) | 9 (42.9) | 0.004 |
| Lack of educational opportunities | ||||
| Strongly disagree | 3 (10.7) | 0 (0.0) | 0 (0.0) | |
| Somewhat disagree | 3 (10.7) | 2 (9.5) | 0 (0.0) | |
| Somewhat agree | 11(39.3) | 5 (23.8) | 4 (19.1) | |
| Strongly agree | 10 (35.7) | 14 (66.7) | 12 (57.1) | |
| Do not know | 1 (3.6) | 0 (0.0) | 5 (23.8) | 0.016 |
| Concerns about dependency (HIV/AIDS) | ||||
| Strongly disagree | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Somewhat disagree | 1 (3.6) | 2 (10.0) | 0 (0.0) | |
| Somewhat agree | 12 (42.8) | 3 (15.0) | 2 (9.5) | |
| Strongly agree | 2 (7.1) | 3 (15.0) | 4 (19.1) | |
| Do not know | 13 (46.4) | 12 (60.0) | 15 (71.4) | 0.06 |
| Opioids not always available for | ||||
| Emergencies | ||||
| Strongly disagree | 1 (3.6) | 3 (15.0) | 0 (0.0) | |
| Somewhat disagree | 4 (14.3) | 2 (10.0) | 0 (0.0) | |
| Somewhat agree | 9 (32.1) | 7 (35.0) | 4 (19.1) | |
| Strongly agree | 3 (10.7) | 6 (30.0) | 10 (47.6) | |
| Do not know | 11 (39.3) | 2 (10.0) | 7 (3.3) | 0.013 |
| Strict controls result in prescribing of weaker opioids | ||||
| Strongly disagree | 4 (14.3) | 2 (10.0) | 0 (0.0) | |
| Somewhat disagree | 5 (17.9) | 0 (0.0) | 0 (0.0) | |
| Somewhat agree | 8 (28.6) | 8 (40.0) | 3 (14.3) | |
| Strongly agree | 6 (21.4) | 9 (45.0) | 10 (47.6) | |
| Do not know | 5 (17.8 | 1 (5.0) | 8 (38.1) | 0.006 |
Table 8.
Attitudes of physicians in relation to age where p value is less than 5% (n = 73).
| Characteristic | 26–50, n (%) | 50+, n (%) | p value |
|---|---|---|---|
| Pharmacists’ reluctance to stock (cancer) | |||
| Not a problem | 7 (21.2) | 1 (2.8) | |
| Minor problem | 3 (9.1) | 1 (2.8) | |
| Moderate problem | 0 (0.0) | 6 (16.7) | |
| Serious problem | 8 (24.2) | 8 (22.2) | |
| Do not know | 15 (45.5) | 20 (55.5) | 0.011 |
| Nurses’ reluctance to administer (cancer) | |||
| Not a problem | 3 (9.1) | 10 (28.6) | |
| Minor problem | 5 (15.1) | 3 (8.6) | |
| Moderate problem | 4 (12.1) | 2 (5.7) | |
| Serious problem | 11 (33.3) | 4 (11.4) | |
| Do not know | 10 (30.3) | 16 (45.7) | 0.048 |
| Nurses’ reluctance to administer (other) | |||
| Not a problem | 2 (6.1) | 6 (17.1) | |
| Minor problem | 1 (3.0) | 3 (8.6) | |
| Moderate problem | 6 (18.2) | 7 (20.0) | |
| Serious problem | 12 (36.4) | 3 (8.6) | |
| Do not know | 12 (36.4) | 16 (45.7) | 0.054 |
| Restrictive laws (other) | |||
| Not a problem | 1 (3.0) | 2 (5.7) | |
| Minor problem | 5 (15.1) | 1 (2.8) | |
| Moderate problem | 3 (9.1) | 10 (28.6) | |
| Serious problem | 7 (21.2) | 10 (28.6) | |
| Do not know | 17 (51.5) | 12 (34.3) | 0.08 |
| Surgical pain not adequately treated | |||
| Strongly disagree | 3 (9.1) | 14 (38.9) | |
| Somewhat disagree | 11 (33.3) | 7 (19.4) | |
| Somewhat agree | 9 (27.2) | 6 (16.7) | |
| Strongly agree | 5 (15.2) | 1 (2.8) | |
| Do not know | 5 (15.2) | 8 (22.2) | 0.016 |
The analysis of the qualitative results was done through a philosophical analysis informed by Colaizzi’s descriptive phenomenological approach.18 The analysis proceeded through the following seven stages: In the first stage, each interview was read several times in order to enhance understanding of the issue. In the second stage, specific reports of participants on the use and management of opioid analgesics in Cyprus was given. In the third stage, each of the references was rendered meaningful. In the fourth stage, after the references were agreed upon, all the codes in thematic groups were categorized. In the fifth stage, a detailed description of all the issues raised took place. In the sixth stage, findings not related to the aim of the study and over-estimated opinions or theories unrelated to the subject were removed. In the seventh and final stage, the results were randomly emailed to seven participants, and the results of the focus groups were discussed in light of the quantitative findings of the previous survey and the relevant bibliography. The process of constructing the themes and subthemes was informed by the principle of data saturation and explicitly the inductive thematic saturation. In this model, saturation focuses on the identification of new codes or themes and is based on the number of such codes or themes rather than the completeness of existing theoretical categories. Each theme is accompanied by verbatim quotes which reflected the views expressed.
Ethical considerations
Ethical approvals were obtained according to national law from the Cyprus Bioethics Committee (EEBK EP 2012.01.38) and the Ministry of Health (MoH 5.34.01.7.6E). Participants were informed about the purpose of the study and the methodology. Respondents’ participation was voluntary, and they retained their right to withdraw from the study.
Results
Quantitative phase of the study
A total of 73 registered physicians completed the BOAT questionnaire. Their demographics are presented in Table 9.
Table 9.
Respondents’ age, specialty, and primary affiliation distributions.
| Age group (years) | Respondents |
|---|---|
| 26–30 | 2 |
| 31–35 | 3 |
| 36–40 | 12 |
| 41–45 | 10 |
| 46–50 | 8 |
| 51–55 | 17 |
| 56–60 | 9 |
| 61–65 | 9 |
| 66+ | 1 |
| Specialty | Respondents |
| No response | 2 |
| General medicine | 23 |
| General surgery | 3 |
| Oncology | 4 |
| Pediatrics | 6 |
| Gynecology | 6 |
| Anaesthesiology | 5 |
| Dermatology | 3 |
| Cardiology | 3 |
| Other | 16 |
| No response | 4 |
| Primary affiliation | Respondents |
| Clinic | 30 |
| Hospital | 15 |
| Hospice/palliative | 1 |
| Government | 7 |
| Other | 20 |
The results are presented in three sections that correspond to the three sections of the BOAT questionnaire. Numbers and proportions of responses to each item were calculated in order to identify major obstacles, according to the opinions of the physicians. Potential correlations between physicians’ ages and their responses as well as between the physicians’ main affiliation and the barriers which they hold responsible for the inadequate availability of opioids were also explored.
Section I
The purpose of the age group was to establish whether younger, more recently qualified physicians have better opioid-related knowledge due to more comprehensive pain management education. Physicians were asked to include information about their specialties in the hope of establishing a relationship between specialties and opioid-related knowledge. Despite the wide range of respondent specialties, the findings did not support the assumption that there are certain specialties in Cyprus which acquire more experience in pain management.
A category relating to the physicians’ primary affiliation was included in section I. As expected, not all of the options were represented due to the specificities of the Cyprus healthcare system. For example, there were no respondents who work in an “Academic Institution” due to the absence of a medical school in Cyprus at the time of the study.
For purposes of comparison, affiliations were divided into three categories consisting of the public sector (“Hospital” and “Government”), private hospitals (“Clinic”), and private non-hospital healthcare/non-governmental organization (NGOs; “Other” and “Palliative Care”).
Section II
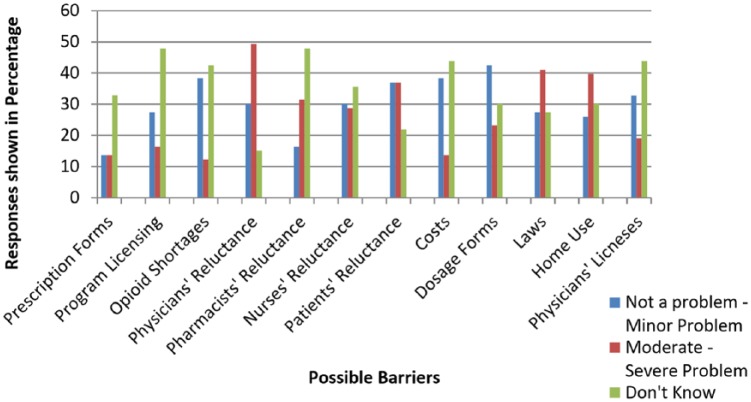
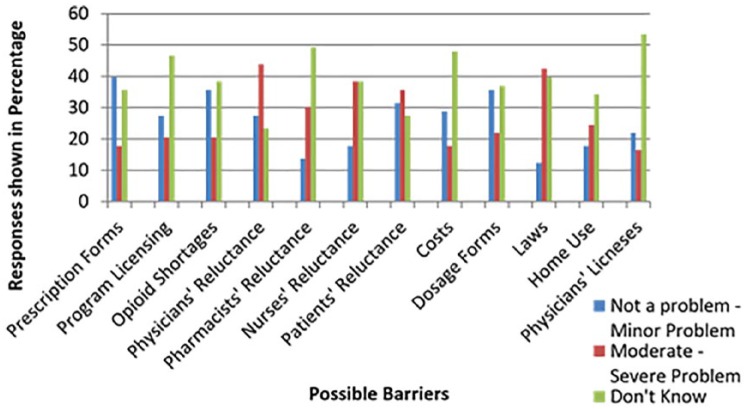
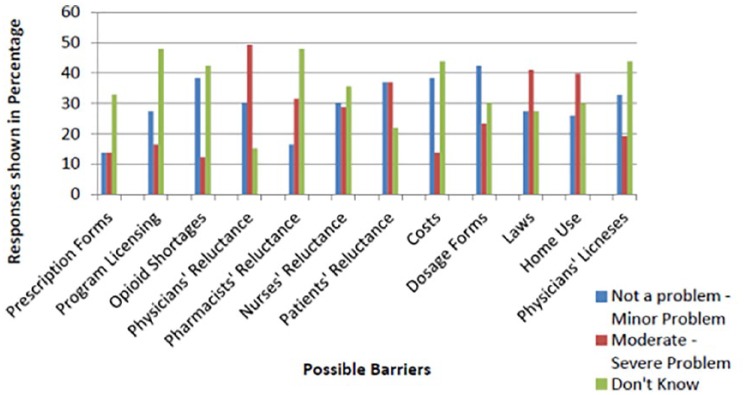
The data from responses to the second section of the questionnaire were tabulated into three parts: distribution of replies related to CP (see Table 10), AIDS/HIV pain (see Table 1), and other types of pain (non-cancer/non-AIDS; see Table 3). Columns in each table indicate how many physicians chose between “Not a Problem,” “Minor Problem,” “Moderate Problem,” “Severe Problem” and “Don’t Know.” The “No Response” column shows blank responses to particular questions. In order to assist in the comparison of barriers which were thought to cause no or minor problems and those that were thought to cause moderate to severe problems, the figures were merged in a second set of tables. Those which were not a problem were combined with those which posed a minor problem and compared with those that were thought to cause moderate-to-severe problems. This enabled a clearer distinction between the two categories and gave an indication of the barriers thought to be the most serious according to the respondents’ view. The task was performed for each of the categories related to CP (see Table 11), HIV/AIDS pain (see Table 2), and other types of pain (non-cancer/non-HIV/AIDS; see Table 4). These results were then charted in a graph in order to allow for easier comparison (see Figures 1 and 2).
Table 10.
Distribution of responses relating to CP (n = 73; distribution of physicians’ responses for each of the possible barriers to opioid use in the management of CP).
| Not a problem | Minor problem | Moderate problem | Serious problem | Do not know | No response | |
|---|---|---|---|---|---|---|
| Prescription forms | 26(35.61%) | 7 (9.58%) | 5 (6.84%) | 5 (6.84%) | 24 (32.87%) | 6 (8.21%) |
| Program licensing | 12 (16.43%) | 8 (10.95%) | 6 (8.21%) | 6 (8.21%) | 35 (47.94%) | 6 (8.21%) |
| Shortage of opioids | 23 (31.50%) | 5 (6.84%) | 6 (8.21%) | 3 (4.10%) | 31 (42.46%) | 5 (6.84%) |
| Physicians | 16 (21.91%) | 6 (8.21%) | 18 (24.65%) | 18 (24.65%) | 11 (15.06%) | 4 (5.47%) |
| Pharmacists | 8 (10.95%) | 4 (5.47%) | 6 (8.21%) | 17 (23.28%) | 35 (47.94%) | 3 (4.10%) |
| Nurses | 13 (17.80%) | 9 (12.32%) | 6 (8.21%) | 15 (20.54%) | 26 (35.61%) | 4 (5.47%) |
| Patients | 15 (20.54%) | 12 (16.43%) | 22 (30.13%) | 5 (6.84%) | 16 (21.91%) | 3 (4.10%) |
| Costs | 19 (26.02%) | 9 (12.32%) | 6 (8.21%) | 4 (5.47%) | 32 (43.83%) | 3 (4,10%) |
| Doses | 17 (23.28%) | 14 (19.17%) | 12 (16.43%) | 5 (6.84%) | 22 (30.13%) | 3 (4.10%) |
| Regulations | 8 (10.95%) | 12 (16.43%) | 11 (15.06%) | 19 (26.02%) | 20 (27.39%) | 3 (4.10%) |
| Unavailable for home use | 8 (10.95%) | 11 (15.06%) | 11 (15.06%) | 18 (24.65%) | 22 (30.13%) | 3 (4.10%) |
| Physician licensing | 13 (17.80%) | 11 (15.06%) | 7 (9.58%) | 7 (9.58%) | 32 (43.83%) | 3 (4.10%) |
CP: cancer pain.
Table 11.
Merged distribution of responses relating to CP (n = 73; distribution of physicians’ responses for each of the possible barriers to opioid use in the management of CP).
| Not a problem–minor problem | Moderate problem–serious problem | Do not know | No response | |
|---|---|---|---|---|
| Prescription forms | 33 (45.19%) | 10 (13.68%) | 24 (32.87%) | 6 (8.21%) |
| Program licensing | 20 (27.38%) | 12 (16.42%) | 35 (47.94%) | 6 (8.21%) |
| Shortage of opioids | 28 (38.34%) | 9 (12.31%) | 31 (42.46%) | 5 (6.84%) |
| Physicians | 22 (30.12%) | 36 (49.30%) | 11 (15.06%) | 4 (5.47%) |
| Pharmacists | 12 (16.42%) | 23 (31.49%) | 35 (47.94%) | 3 (4.10%) |
| Nurses | 22 (30.12%) | 21 (28.75%) | 26 (35.61%) | 4 (5.47%) |
| Patients | 27 (36.97%) | 27 (36.97%) | 16 (21.91%) | 3 (4.10%) |
| Costs | 28 (38.34%) | 10 (13.68%) | 32 (43.83%) | 3 (4.10%) |
| Doses | 31 (42.45%) | 17 (23.27%) | 22 (30.13%) | 3 (4.10%) |
| Laws | 20 (27.38%) | 30 (41.08%) | 20 (27.39%) | 3 (4.10%) |
| Availability for home use | 19 (26.01%) | 29 (39.71%) | 22 (30.13%) | 3 (4.10%) |
| Physician licensing | 24 (32.86%) | 14 (19.16%) | 32 (43.83%) | 3 (4.10%) |
CP: cancer pain.
Figure 1.
Opiophobia model.
Figure 2.
Proportion of responses relating to HIV/AIDS pain (n = 73).
CP
Figure 3 shows the distribution of responses in the CP category and indicates that the most popular choice of response was “Don’t Know” for 7 out of the 12 questions. Physicians believed that moderate-to-severe problems in opioid availability were caused primarily by “Physicians’ reluctance to prescribe opioids—49.3%, and “Laws/regulations—41.08%,” while minimal problems were primarily caused by “Prescription Forms 45.19%” and “Dosage forms and dosages 42.45%.”
Figure 3.
Proportion of responses relating to other types of pain (n = 73).
HIV-/AIDS-related pain
The majority of physicians indicated that they did not know whether these barriers can impact the use of opioids in the HIV/AIDS context (see Table 2). This was not surprising given that there are few reported cases in Cyprus and those diagnosed with HIV/AIDS attend specialist clinics. The majority of the physicians identified “Regulations” as the main barrier to opioid use followed by “Availability for home use” and “Physicians’ reluctance to prescribe opioids” (see Figure 1).
Other types of pain (non-cancer/non-HIV/AIDS)
In the context of non-cancer/non-HIV/AIDS pain, physicians predominantly identified “Physicians’ reluctance to prescribe opioids—42.82%” and “Laws/regulations—42.45%” as severe barriers to opioid use (see Tables 3 and 4). Minor barriers to opioids’ use in this context included “Prescription forms—39.71%” followed by “Opioid shortages—35.6%.” These findings revealed a similar distribution to that seen in the CP context (see Figure 2).
Section III
Section III of the questionnaire includes questions regarding physicians’ opinions on the use of opioids in selected situations. The response choices vary between “Strongly Disagree” and “Strongly Agree” and “Don’t Know.” The response distribution has been tabulated for each category, including a “No Response” column indicating choices which were left blank (see Table 5).
In categories related to various opioid-related situations, 45.19% of physicians agreed that CP is not adequately managed, while 32.87% believed that fears about dependence interfere with CP management. A high percentage of respondents (76.7%) believe that there are inadequate educational opportunities to learn about the use of opioids or further develop their knowledge on pain management. More than half of the respondents perceived that opioids are not always available to the patient for emergencies, including nights and weekends (53.41%).
The majority of respondents had no knowledge relating to opioid accessibility in various groups of patients; 45.2% of physicians did not know whether there had been recent improvement in opioid availability, while 78.08% and 83.56% did not know whether opioids were available for the treatment of pediatric CP and pediatric AIDS-related pain, respectively; 53.41% agreed that opioids are not always available during pharmacies’ out-of-hours, while the majority of respondents (60.26%) believed that strict control of morphine results in the preference of milder analgesics for the treatment of CP.
Cross tabulations
Significant results in cross tabulations (p value less than 5%) were present in some of the questions related to affiliations (see Tables 6 and 7) and age groups (see Table 8). For example, there appears to be more reluctance to prescribe opioids (p = 0.0004) and appropriate opioids dosages (p = 0.027) among private physicians compared to those working in the public sector. Furthermore, there appears to be more difficulty in obtaining opioids for home use (p = 0.004) and lack of educational opportunities (p = 0.016) in the private sector. In relation to age-related differences in physician’s beliefs, the findings showed that younger physicians (aged 25–50 years) believed that surgical pain is not adequately treated (p = 0.016) and that there is reluctance on behalf of nurses to administer opioids (p = 0.048).
It can be concluded that although sometimes small, there are affiliation and age-related differences in physicians’ beliefs and knowledge regarding barriers to opioid availability. This is not surprising given the differences between practices in the public and private sectors and the differences between the knowledge and attitudes of younger physicians compared to their more experienced colleagues.
Qualitative phase of the study
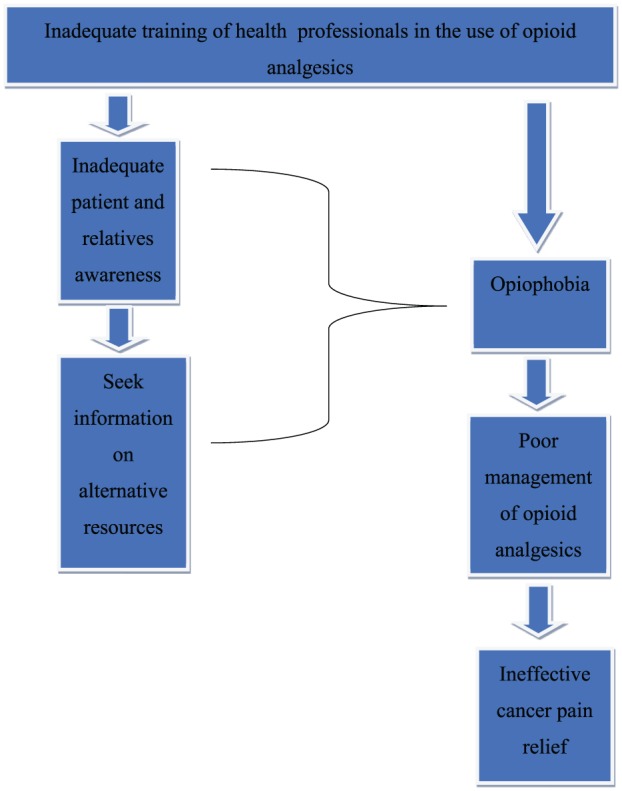
In the first stage, the focus groups transcripts (Focus group 1—1:58 recording time and Focus group 2—2:25 recording time) were read several times in order to enhance understanding of the issue, and this was followed by identifying specific reports in the transcripts that were related to the topic. This resulted in 258 reports being identified from both focus groups. In the third stage, each of the 258 references was rendered meaningful and all the codes that came up were discussed with the researchers. In the fourth stage, after the reports were agreed, all the codes were categorized into 20 thematic groups. These thematic groups were then coded again to give their general meaning. These 20 thematic groups were re-classified into categories so that the 6 main themes would eventually emerge with the consensus of all the researchers. Therefore, the following six main themes emerged: inadequate training of HCPs in the use of opioid analgesics, poor patient/caregivers’ awareness of opioid analgesics, opiophobia in HCPs, opiophobia in patients/caregivers, poor management of opioid analgesics by HCPs and patients/caregivers, and ineffective pain relief with opioids (Figure 4).
Figure 4.
Proportion of responses relating to cancer pain.
Theme 1. Inadequate training of HCPs in the use of opioid analgesics
HCPs believe that their lack of knowledge about opioid analgesics has a negative effect on patients, with employers not promoting or facilitating their staff’s training and not making the most of properly trained staff.
Subthemes
Theme 1.1
The training of HCPs is deficient in relation to opioid analgesics. Oncology specialties do not involve additional training in the use of opioid analgesics, and oncologists do not pursue further education on this topic. Nurses also find themselves in a similar situation. They feel the need to reinforce their education with special courses in the management of opioid analgesics during their basic education, as they say they are not aware of the pharmacology of morphine and are afraid of its side-effects:
… I also think that most of us physicians and nurses dealing with these medicines have empirically learned how to administer them; we have not been specifically trained on how to administer each drug and in which order, nor which medicine to administer for which pain.
Unfortunately, you do not even get any proper guidance during your oncology training … guidance in how to administer medicine. If you do not care about it yourself or do a course or a degree in it, then it just won’t happen otherwise.
Theme 1.2
HCPs’ lack of knowledge on opioids has a negative effect on the patient. This lack of sufficient knowledge creates a feeling of insecurity in patients and engenders negative feelings in them when it comes to taking them. Patients continue to suffer, and pain relief is not achieved because physicians do not use opioid analgesics appropriately. Nurses working in oncology wards report that due to their limited knowledge on the topic, they do not administer the opioids as indicated:
It is the inadequate training of staff on opioid drugs that creates a sense of insecurity which is transferred to the patient and relatives, creating the sense that everyone must move along the same path or trajectory …
Theme 1.3
The employer is responsible for allocating the necessary resources for the training of HCPs in the use of opioid analgesics. Here, HCPs report that the main cause of staff non-training is the Ministry of Health, which is mismanaging the resources, and the state must be compelled to educate its HCPs about the use of opioid analgesics:
… The state (i.e. referring to the Ministry of Health) must legislate and train …
Theme 1.4
There is a need for a multidisciplinary education of HCPs on opioids that adopts a comprehensive approach that demystifies opioids use:
An opioid-trained nurse managed to eliminate her fear of using morphine and her intervention had a positive effect on relieving the pain of her patient. An extension of the education of HCP is also what they can learn from the patients themselves and their caregivers.
… we all have (i.e. referring to the various specialties) to learn from working together to the best interest of the patient by optimising opioid use.
Theme 2. Inadequate patient and caregivers’ awareness regarding opioid analgesics
HCPs believe that the patients and their caregivers as a result to the scarcity of information and training by HCPs on the management of opioids drive them to seek information on alternative resources such as the Internet.
Subthemes
Theme 2.1
As a result of their ill preparation, patients and caregivers choose to be informed on opioid analgesics from various sources of information including unreliable ones. In the absence of evidence-based information, they are forced to seek information on the use of opioid analgesics elsewhere, mainly from the Internet, and to seek alternatives to opioids use for alleviating:
Our level of education is low and we end up searching on the Internet for everything related to opioids and because alternative treatments are often attractive to patients, as a result of opiophobia I often get the feeling that they would go for anything else apart from morphine.
Theme 2.2
There is no structured and scheduled patient/caregiver briefing for the use of opioid analgesics in relieving CP. Patients need to be informed by HCPs throughout the cancer care continuum. HCPs recognize that there is a weakness in informing patients/caregiver and that it should be done in time, before the treatment is initiated, be personalized to both the patient and the relative, and be holistic:
… This means educating your patient before, preparing him, informing him about what side effects to expect and how to deal with them.
On the other hand, you have the research nurses who can and will theoretically assume this role at least the first time you prescribe any chemotherapy drug, be it targeted or opioid the patient always needs time to understand more about its administration the first time round.
Theme 2.3
Insufficient patients’ education implies risks to their safety. HCPs recognize that the use of opioid analgesics by untrained patients/caregivers, as well as their search for information on their own, can be a threat to their safety. It is emphasized that the patient and the caregiver should have the same attention and training by HCPs in order to ensure a smooth and safe continuation of opioid use at the home setting:
… A colleague told us of her experience … it was Friday and she gave 10 patches to the daughter of the patient and took them both home without explanation, without anything, and on Sunday the daughter called and the old woman … was sleeping (She had placed all 10 patches on her). Whenever and wherever the old lady suffered pain, that’s where the daughter had patched her in order to alleviate her pain.
Theme 3. Opiophobia in HCPs
Opiophobia appears to be prominent among HCPs and this seems to be reinforced through the inadequate training on opioid analgesics. Their poor preparation to appropriately manage opioids in the clinical setting often leads to improper use, leaving the patient in unnecessary suffering.
Subthemes
Theme 3.1
HCPs fear the use of opioid analgesics. HCPs conclude that the problem of opiophobia exists and concerns all HCPs, including oncologists, physicians of other specializations, nurses, and pharmacists. Physicians fear the responsibility of administering opioid analgesics and writing down the word “morphine” in their prescriptions, associating it with addiction and death. Nurses are afraid of the drug storage cabinets, are surprised by the pain doctor’s instructions, and react to prescribing opioids, which forces physicians not to:
… write the morphine administration instruction and give it to the nurse. The nurse … (making a deep breathing sound of surprise) reluctantly replies to the physician: every two minutes? What is going on? The nurse is afraid to give the drugs out of fear of complications …
Theme 3.2
HCPs are not fully aware of the side-effects of opioids or they have misconceptions about these. Physicians consider the use of morphine to be a pain or burden which is administered to the moribund and is highly addictive. Physicians and nurses are not comfortable with giving high doses of drugs and are afraid of the frequent doses that might lead to life-threatening complications:
… And when the physician came from the Oncology Clinic and said you could give the patient morphine every 15 minutes, every 20 minutes … it was a shock … both for the doctor who was there and for the staff that was present. “It is out of the question … it is out of the question … I won’t do it…this will make the patient stop breathing …
Theme 3.3
Incorrect and ineffective use of opioids. The fear and ignorance of HCP leads to the misuse of opioids at all levels of health. Instead, they provide an alternative and ineffective painkiller because it is not morphine and which is unlike to cause life-threatening complications. Patients are in pain because physicians do not give opioids and nurses do not give the recommended dose of opioids:
I (the treating physician) give a lower dose in the evening in order to have peace of mind … and the nurses even lower … the patient this way never gets what he needs, oh I don’t know …
Theme 4. Opiophobia in patients/caregivers
There seems to be a feeling of fear among patients/caregivers about the indications of the use and effects of opioid analgesics, thus resulting in their inadequate use and/or misuse.
Subthemes
Theme 4.1. False perceptions and bias of patients/caregivers against opioids
Patients and caregivers believe that morphine is given in the final stages of the disease and they frequently associate it with death and dying:
… It’s about opiophobia when the patient comes in … that morphine has been identified as a means of therapy that indicates a terminal status. The patient asks, ‘Is this the end?’ Or the relative sees the patient attached to a drip labeled ‘morphine’ and comes next to the physician and asks, ‘Will he die?’
Theme 4.2. Fear of patients/relatives regarding opioid side-effects
Patients believe that morphine causes dependence and that they will end up becoming drug addicts, and thus, they refuse to take opioid analgesics. The parents of children with malignant tumors fear that morphine will reduce their children’s level of consciousness, and the relatives worry that the patient will be stigmatized by society if he takes opioids:
… Because they say “opioid, narcotic,” they associate it in their minds with heroin (i.e. they hear death), that is, the most well-known drug is heroin and it has known side effects. The same goes for patients and their relatives in reference to the drug use and all they are afraid of is addiction. They simply consider the two cases as one.
Theme 4.3. Lack of patients’/caregivers’ trust in what HCPs tell them and inadequate use of opioid analgesics
It has been found that people are generally negative about morphine even before there is any indication of disease or prognosis. Relatives influence the clinical decisions of nurses, and in many cases, they do not allow them to give the indicated dose of opioid. The relatives’ behavior it has been noted, distances the patient from opioid analgesics, preferring instead for the patient to continue suffering pain because they associate opioid use with a progression of the disease and subsequently death:
… The patient wants his morphine treatment, he does not want to hurt when he has cancer, but the family does not want us to give him much, so that he does not continually ask for it … so he does not become a drug addict …
It’s a lot harder when you have to deal with babies because unfortunately even when we ask a baby if it hurts, the mother responds, the baby won’t even answer … okay.
Theme 5. Poor management of opioid analgesics by HCP
There is poor management of the distribution and delivery of opioids by HCPs, mainly from pharmaceutical services, resulting in their dangerous accumulation in patients’ disposal, as well as in the lack of control in their destruction when these are not necessary (i.e. following a patient’s death).
Subthemes
Theme 5.1
Physicians who have the responsibility to prescribe them do not handle them properly. Therefore, the prescription of opioids is not made according to the patient’s needs or do not reflect the actual usage by the patients (i.e. due to poor management and control):
… I always try to provide the patient with an adequate quantity of the opioid drug, and often this means prescribing more than it is really necessary …
Theme 5.2
HCPs report that there is a large amount of opioids in patients’ homes. Excessive opioids end up in the wrong hands, especially after the patient’s death. HCPs recognize the risk of uncontrolled accumulations of opioids in domestic settings and thus try to control the amounts that patients take with them:
… At the out-patients’ clinic, once a patient came to me with 7 boxes of opioids, saying that he has far more than he really needed, I was so surprised and asked him where he got it, and he then said, but from here (i.e. clinic) of course …
Theme 5.3. Lack of appropriate organization of pharmacies in opioid management
HCPs report that pharmacists deal with the most challenges in opioid management and handling, often do not follow the pain physician’s instructions, and believe that the use of opioids does not concern them and deny their involvement in the procedure. The lack of organization of pharmacies leads to uncontrolled drug distribution and losses, failure to handle surpluses and returns, and problems of opioid availability in clinical settings:
… We send a patient at home with analgesic drugs … we prescribe for a month as we have said, suddenly the patient dies within 2 days, the family is well placed to bring the analgesics to the hospital’s pharmacy and they refuse to take them … even for disposal purposes.
Theme 5.4. Reckless destruction and wastage of opioid analgesics
There is incorrect drug destruction taking place, and expensive drugs are destroyed rather than appropriately reused. Although most HCPs are sensitive to the issue and take responsibility for receiving returns, the lack of knowledge by certain specialties results in unnecessary and inappropriate disposal of opioid drugs:
… We need to be looking into our dispensing guidelines and adopting practices on returning and reusing medications. Currently I am unable to accept any medication that was already dispensed to patients but for any reason has not been used. I simply need to waste these …
Theme 6. Ineffective CP relief with opioid analgesics
Pain is not one of the immediate priorities of HCPs, and there is a difference in its assessment and management among HCP often resulting in poor pain relief.
Subthemes
Theme 6.1
Physicians do not always prioritize CP relief. In Cyprus, there is the provision of all the means and opportunities to relieve pain, yet there are people who continue to suffer. Oncologists focus on the disease and its treatment and ignore or fail to consistently evaluate pain due lack of time:
… There may be pain and other issues. Unfortunately, we oncologists … yes … we will concentrate on the disease. He has lung cancer, we will provide him with the cure, and from then on we mistakenly believe that treatment has been given and that’s it … well, the pain will also be reduced.
Theme 6.2
HCPs do not have sufficient opioid knowledge and do not relieve pain. They do not have the same background in opioid analgesics and this creates challenges in the clinical setting:
… A patient who came out of surgery with extreme pain and who really suffered, was restricted to just getting paracetamol from the physicians or, at best, a painkiller with codeine. He was very rarely given morphine and a wrong dose of it …
Theme 6.3
There is a difference in the assessment of pain among HCP, thus resulting in ineffective pain relief. There is a difference of opinion in assessing the type and severity of pain among physicians and nurses. In major oncological wards, nurses assess and record pain in reports 24 h a day and track its specific features. These reports are not assessed in the same way by physicians. It has been reported that physicians do not adequately regulate morphine administration:
… We have a heavier burden and can usually see the whole situation as nurses because many times my colleagues and I are with the patient 24 hours a day. We have a different assessment and often the physician can contradict you, you can tell him again and again, “Doctor, the patient is in pain,” and he’ll just say, “But you gave him medicine a while ago, let him be, wait …”
Discussion
The aim of the research was to explore the perceptions of HCP regarding the use of opioid analgesics in relieving CP in Cyprus. The quantitative and qualitative parts of the research have led to the general conclusion that the main barrier to the use of opioid analgesics in Cyprus is the lack of appropriate training of HCP regarding the use of opioid analgesics. The focus groups revealed cases where the training of an HCP on opioids improved the relief of CP effectively and allowed the barriers that caused opiophobia to be overcome.
HCPs’ and patients’ perceptions
The use of opioids has also been linked to death and addiction, thus resulting in fear of using them. The ineptitude of HCP when it comes to the use and management of opioid analgesics has a negative impact on the education and information of patients and caregivers regarding treatment with opioids. Patients/caregivers are forced to find information from the Internet and other sources, which also create a sense of fear about the usage and side-effects of opioid analgesics, such as addiction, sedation, and even death. They often fail to follow the instructions of HCPs properly or even make mistakes in opioid administration, and so, their pain is not satisfactorily relieved. There appears that this area of concern is not only recorded in Cyprus. Recently, in Japan, instructions were issued to physicians who prescribed opioid analgesics in order to reduce their misuse and mismanagement by patients and physicians themselves. According to the instructions, physicians must have completed specific online training for each opioid medication, and patients must initially try out the drug in a kind of test run. A basic criterion for the continuation of analgesic therapy is patient expectation and satisfaction.19 Similarly, in the United States, the Centers for Disease Control and Prevention (CDC) has issued guidelines to all HCPs involved in opioid management indicating that they should first discuss with the patient all the possible side-effects, risks, and benefits of using these drugs to ensure the correct behavior of the patients toward their own treatment. They should focus on issues of long-term side-effects and their safe use by the patient’s family in order to avoid being exposed to danger through their potential use.20 In the United States, following the implementation of these guidelines, there was a noted improvement in patient’s behavior regarding therapy and a reduction in the risk of side-effects. In particular, HCPs have used five techniques to improve patient behavior to varying degrees, but with the same results. They focused on the patient’s autonomy, developed friendly relationships with them, took things slowly, scheduled small and frequent meetings for problem solving, and showed sympathy and interest. Patients showed cooperation as regarded their treatment and misuse and side-effects were reduced. Moreover, they also achieved better pain relief.21
HCPs’ training
The quantitative phase of the study pointed out that the main barrier to the use of opioid analgesics in Cyprus is the lack of physicians’ training. This is reinforced by the beliefs and fears of HCP and the general population around opioid analgesics. The lack of physicians’ education mentioned in the research’s general conclusion is also consistent with the results of Cicely Saunders’ model analysis of focus groups. At the top of the model is the lack of knowledge of HCPs around the management of opioid analgesics which, as described above, triggers a series of reactions resulting in ineffective pain relief. As a result of their poor educational preparation, in limited instances, physicians may behave negligently or worse in prescribing opioids often leading to opioid use disorders (OUDs). These disorders are now the second most common drug use disorder in the United States, and prevalence has increased over the last two decades.22 Many medical schools do not offer special courses in the use of opioid analgesics. Nurses find themselves in a similar situation. They feel the need to take special courses in the management of opioid analgesics at the time of their basic education, stating that they do not know the pharmacology of morphine and are afraid of its side-effects, particularly the life-threatening ones. This lack of knowledge of HCP in the use of opioid analgesics creates a feeling of insecurity in patients and leads to negativity when it comes to taking them. Patients continue to suffer pain, and optimal pain relief is not achieved because physicians do not use opioid analgesics appropriately.23
As regards nurses working in oncology wards, it is reported that due to lack of knowledge, they do not administer the opioids as indicated with the inevitable result that the patient suffers. Nurses have difficulty in recognizing the correct doses of opioids and have a problem with their administration. Their training, however, did not help them to surpass these barriers to a satisfactory degree because they could not overcome their own prejudices and beliefs.24
HCPs believe that incomplete and inadequate awareness of opioids’ use to treat CP leads patients to alternative sources of unreliable information or misinformation, creating a feeling of fear with negative consequences. Patients and their caregiver rely on HCPs to inform them about their opioid analgesic therapy. In the absence of such information, they are forced to find (often dubious) information on the use of opioid analgesics, mainly from the Internet, and to seek alternatives to pain relief other than morphine. Informing patients by the HCPs needs to include aspects of opioid use across the cancer care continuum.25 HCPs recognize that there are deficiencies in informing patients/relatives and that this should be done in good time, before the treatment is initiated. The information received should be personalized to both the patient and the relatives and be holistic.15
The issue of educating opioid HCPs seems to be a long-lasting problem and no clear-cut results are offered in comparisons of whether or not newly registered physicians, as opposed to the more experienced ones, have been better educated. The literature points out that the major challenge in the control of opioid pain is the professional training of HCP in the pharmacology, pharmacodynamics, and pharmacokinetics of morphine, as well as the optimal way for dose titration to achieve better clinical outcomes with minimum side-effects.26 The findings from the quantitative and qualitative phases of the study agree that the hierarchy and working time of HCP do not play a role in their ability to manage opioids. There is the need for a training program for all HCPs involved in pain management, regardless of their age or educational background. This will allow them to have a common code of conduct for the use of opioids and a standard measure for pain relief.
HCPs’ and patients’ opiophobia
The myths, prejudice, fears, and beliefs of HCPs and the public enhance the overall effect of the quantitative research findings, and this is also reinforced by the focus groups’ results as mentioned in the thematic units. The focus groups demonstrated that the use of morphine in Cyprus in the treatment of CP only began in the last two decades. It is commonly accepted that it will take time for the opioids to become entrenched in society as acceptable types of medication in the treatment of pain by HCPs and the general public. Currently, these are considered substances that cause fear on a large scale and are associated with addiction and poor prognosis. This is however, contradictory to the reality of opioids, based on which these are the most effective in relieving CP.27 Anxieties about addiction have been implicated in the non-relief of CP, pain in the final stages of terminal illness, and acute pain.24 The misconceptions of HCPs regarding the use and side-effects of morphine (dependency, final stages, etc.) create a barrier to opioid use by physicians and their patients. The word “morphine” alone acts a barrier to its use by the patient, but also as a medicine to be prescribed by the physician. The failure of HCPs to fully inform the patients and their caregivers about opioids is a barrier for patients to consent to their taking. This often results in caregivers blocking opioid use in the patient either by refusing to allow prescriptions or by not giving the drug to the patient. Similarly, in children with malignant tumors, the children’s parents negatively influence clinical decisions regarding the management of pain via opioids.
Opiophobia seems to be entrenched among HCPs, which is reinforced through inadequate training around opioid analgesics often leading to their ineffective use. Nurses seam to fear the responsibility of storing opioids on the ward, are often surprised by the physician’s instructions, and react negatively to the prescription of opioids, often causing physicians to reluctantly prescribe them. Physicians consider morphine to be both addictive and a nuisance and link its use to patients who are on their death beds. Physicians and nurses are not comfortable with administering high doses of drugs and are afraid of frequent doses. There appears to be a feeling of fear among patients and caregivers about the indications and the side-effects of opioid analgesics, which leads to their inadequate use or misuse. Patients believe that morphine causes addiction and prefer to endure pain rather than to take opioid analgesics. Within the pediatric oncology context, parents are afraid that morphine will reduce their child’s level of consciousness making their interaction with the environment difficult.28 Nurses’ attitudes are influenced by political factors, their culture, and their own beliefs concerning drugs.29 The physicians’ practice of prescribing drugs and their clinical decisions to relieve pain are influenced by their knowledge, personal beliefs, and attitudes.30
Barriers related to the availability and regulations of opioids
Quantitative results identify serious barriers to the availability of opioid analgesics for patients. This is due to physicians’ refusal to prescribe them, pharmacists’ refusal to stock and store them, and the procedures and regulations regarding the home use of opioids. Barriers that affect to a lesser degree physicians’ delivery of opioids is the prescription form, licensing program, opioid care and storage, costs, dosage regimens, and physicians’ licenses. Further analysis of the topic through the focus groups revealed that the inadequate training of HCP and ineffective pain assessment are also barriers for HCP themselves when it comes to handling opioid analgesics. The inadequacies in HCP drug management are passed on to patients and create a sense of insecurity, which functions as an additional barrier to opioid use.
These findings coincide to those reported in the relevant literature. The numerous barriers to the clinical management of pain with opioids use vary depending on whether they are viewed from the standpoint of the patient, the physician, or the healthcare system.31 For example, the literature mentions the main barriers to pain relief with opioid analgesics: difficult access to these drugs,32 restrictive regulatory measures for their disposal and handling,33 economic factors, and the variability in the instructions for their use among institutions.34
Physicians have many misconceptions about the laws regulating opioid use. They worry that their legitimate prescription will unintentionally induce drug trafficking and user addiction. Although addiction, tolerance, and physical dependence are clearly different phenomena with separate neurophysiological mechanisms, HCPs treat them as synonymous.30 Such concerns lead to the reduced use of opioid analgesics for the treatment of severe CP.35
Barriers related to the assessment and management strategies among HCPs in relation to opioids
The majority of physicians reported that CP (49.3%) and other types of pain (42.8%) are not satisfactorily relieved and disagree that postoperative and traumatic pain (49.3%) are not satisfactorily alleviated. It appears that HCPs in focus groups confirm that both CP and other types of pain are not relieved satisfactorily at all levels and specializations, even by the specialized pain physicians, including postoperative and traumatic pain. There is ineffective alleviation of CP through the use of opioid analgesics due to the inadequate knowledge of HCP. Pain is not in the immediate priorities of HCP, and there is a difference in its assessment and management among them (e.g. physician vs nurse). Pain is not assessed by all HCP in the same way, and there are no standardized measurements in place.
More specifically, there is a difference of opinion between physicians and nurses in evaluating the type and severity of pain. Nurses in major oncology wards record pain and trace its specific features on evaluation forms 24 h a day. These forms are not assessed by physicians in the same way. It has been reported that physicians do not adequately regulate morphine administration. A recommendation that emerged from the finding is that pain should be rated as the fifth vital sign by nurses and physicians. This is related to the APS campaign, “Pain, The Fifth Vital Sign,” and it is proposed here as a means to raise awareness among HCP of pain assessment and management. However, it should be noted here that research has triggered controversy as to the effectiveness of assessing pain as the fifth vital sign within a pain management strategy.36 Levy et al.37 also argue that the introduction of pain as the fifth vital sign contributed to the prescribed opioid epidemic that America is now experiencing. Despite this controversy, poor pain assessment has been previously identified in the literature as one of the reasons that nurses fail to appropriately alleviate pain.38
The role of nurses in the management of CP has been consistently reported in the literature. Nurses have a very important role to play in the management of pain, especially in patients receiving long-term opioid treatment. The first step is the recognition that the patient needs to change treatment from a rapid to a slow-acting opioid. Nurses perform personalized treatment to determine, through evaluation, the best route of administration and type of drug to suit each patient. Through their interventions, they assess the need to adjust the dose according to the pain felt by the patient and to prevent opioid complications and ensure the effectiveness of the treatment. They train the patient and his/her family to manage treatment, administration, and follow-up observations. They record and keep records of levels of pain, drug functionality, and unwanted side-effects and share them with all family members.29
This study has a number of limitations. The participants in the qualitative and quantitative parts of this study work in different clinical contexts which means that they have to work to different policies in relation to the utilization of opioids in clinical practice. This can result in having to deal with different barriers to utilizing opioids for pain management. The different clinical backgrounds of the HCPs also means that they take care of patients at varying stages of the disease requiring different levels of pain relief and hence opioids utilization. This might have contributed to formulating different perspectives to opioids use with those caring for patients at an earlier disease stage to express a more positive attitude to the topic (due to less barriers) compared to those in advanced disease. In terms of the quantitative phase of the study, a limitation was the relatively small number of participants who filled the BOAT questionnaire. However, to counterbalance this, the participants were randomly selected.
Conclusion
There is negativity surrounding opioid analgesics, and HCPs often avoid using them, or when they do use them, the doses are lower than the recommended ones. Based on the study’s finding, it is concluded that ignorance or inadequate knowledge are the main reasons for inappropriate use of opioids. Training and better education could improve the poor mismanagement of opioids in pain management and treatment and in time remove the prejudice and preconceptions on opioids. Improvement in the laws and organizational policies could also improve the appropriate use of opioids alongside milder analgesics according to international protocols and guidelines.
Supplemental Material
Supplemental material, COREQ_checklist for Healthcare professionals’ perceptions on the use of opioid analgesics for the treatment of cancer-related pain in Cyprus: A mixed-method study by Andreas Charalambous, Marios Zorpas, Constantina Cloconi and Yolanda Kading in SAGE Open Medicine
Acknowledgments
The authors would like to express their sincere thanks to all the healthcare professionals who took part in this study offering their valuable insight contributing to the better understanding of opiophobia within the cancer context.
Footnotes
Author contributions: The authors of this paper have directly participated in all the stages of its preparation. A.C. and Y.K. inspired and designed the study. A.C., M.Z., and Y.K. collected, analyzed, and interpreted the data and approved the final manuscript. M.Z. and C.C. prepared all the draft versions of the manuscript. A.C., M.Z., and Y.K. edited the final version of the manuscript. All authors approved the final version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from The Cyprus Bioethics Committee (EEBK EP 2012.01.38) and the Cyprus Ministry of Health (Approval Number MoH 5.34.01.7.6E).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
Supplemental material: Supplemental material for this article is available online.
ORCID iD: Andreas Charalambous  https://orcid.org/0000-0003-4050-031X
https://orcid.org/0000-0003-4050-031X
References
- 1. International Association for the Study of Pain. IASP taxonomy, https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698#Pain (accessed 18 January 2019).
- 2. Henschke N, Kamper SJ, Maher CG. The epidemiology and economic consequences of pain. Mayo Clin Proc 2015; 90(1): 139–147. [DOI] [PubMed] [Google Scholar]
- 3. Campbell JN. APS 1995 presidential address. Pain Forum 1996; 1(5): 85–88. [Google Scholar]
- 4. World Health Organization. International Classification of Diseases, 11th Revision, https://icd.who.int/ (accessed 18 January 2019).
- 5. Morgan JP. American opiophobia: customary underutilization of opioid analgesics. Adv Alcohol Subst Abuse 1985; 5(1–2): 163–173. [DOI] [PubMed] [Google Scholar]
- 6. Zenz M, Willweber-Strumpf A. Opiophobia and cancer pain in Europe. Lancet 1993; 341(8852): 1075–1076. [DOI] [PubMed] [Google Scholar]
- 7. Todd A, Akhter N, Cairns J, et al. The Pain Divide: a cross-sectional analysis of chronic pain prevalence, pain intensity and opioid utilisation in England. BMJ Open 2018; 8(7): e023391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. World Health Organization. Cancer pain relief. Geneva: World Health Organization, 1986. [Google Scholar]
- 9. Jones MR, Viswanath O, Peck J, et al. A brief history of the opioid epidemic and strategies for pain medicine. Pain Ther 2018; 7(1): 13–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Maxwell JC. The prescription drug epidemic in the United States: a perfect storm. Drug Alcohol Rev 2011; 30(3): 264–270. [DOI] [PubMed] [Google Scholar]
- 11. European Commission. Communication from the commission to the European parliament and the council parliament and the council, https://ec.europa.eu/home-affairs/sites/homeaffairs/files/what-we-do/policies/organized-crime-and-human-trafficking/drug-control/eu-response-to-drugs/20170315_evaluation_communication_en.pdf
- 12. The Joint Commission. Pain management standards—hospital, https://www.jointcommission.org/topics/pain_management.aspx (accessed 22 January 2019).
- 13. Tick H, Nielsen A, Pelletier KR, et al. Evidence-based non-pharmacologic strategies for comprehensive pain care: the Consortium Pain Task Force white paper. Explore (NY) 2018; 14(3): 177–211. [DOI] [PubMed] [Google Scholar]
- 14. Breivik H, Eisenberg E, O’Brien T. The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health 2013; 13: 1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O’Brien T, Christrup LL, Drewes AM, et al. European Pain Federation position paper on appropriate opioid use in chronic pain management. Eur J Pain 2017; 21(1): 3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Breuer B, Chang VT, Von Roenn JH, et al. How well do medical oncologists manage chronic cancer pain (CP)? A national survey. Oncologist 2015; 20(2): 202–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Manjiani D, Paul DB, Kunnumpurath S, et al. Availability and utilization of opioids for pain management: global issues. Ochsner J 2014; 14(2): 208–215 [PMC free article] [PubMed] [Google Scholar]
- 18. Shosha G. Employment of Colaizzi’s strategy in descriptive phenomenology: a reflection of a researcher. Eur Sci J 2012; 8(27): 31–43. [Google Scholar]
- 19. Onishi E, Kobayashi T, Dexter E, et al. Comparison of opioid prescribing patterns in the United States and Japan: primary care physicians’ attitudes and perceptions. J Am Board Fam Med 2017; 30(2): 248–254. [DOI] [PubMed] [Google Scholar]
- 20. Greene J, Hibbard J, Alvarez C, et al. Supporting patient behavior change: approaches used by primary care clinicians whose patients’ activation levels increased. Ann Fam Med 2016; 14(2): 148–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hero JO, McMurtry C, Benson J, et al. Discussing opioid risks with patients to reduce misuse and abuse: evidence from 2 surveys. Ann Fam Med 2016; 14(6): 575–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dineen KK, Du Bois JM. Between a rock and a hard place: can physicians prescribe opioids to treat pain adequately while avoiding legal sanction? Am J Law Med 2016; 42(1): 7–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wolfert MZ, Gilson AM, Dahl JL, et al. Opioid analgesics for pain control: Wisconsin physicians’ knowledge, beliefs, attitudes, and prescribing practices. Pain Med 2010; 11(3): 425–434. [DOI] [PubMed] [Google Scholar]
- 24. Elcigil A, Maltepe H, Eşrefgil G, et al. Nurses’ perceived barriers to assessment and management of pain in a university hospital. J Pediatr Hematol Oncol 2011; 33(Suppl. 1): 33–38. [DOI] [PubMed] [Google Scholar]
- 25. Stumbo SP, Yarborough BJH, McCarty D, et al. Patient-reported pathways to opioid use disorders and pain-related barriers to treatment engagement. J Subst Abuse Treat 2017; 73: 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Geppetti P, Benemei S. Pain treatment with opioids: achieving the minimal effective and the minimal interacting dose. Clin Drug Investig 2009; 29(Suppl. 1): 3–16. [DOI] [PubMed] [Google Scholar]
- 27. Mitra R, Jones S. Adjuvant analgesics in cancer pain: a review. Am J Hosp Palliat Care 2012; 29(1): 70–79. [DOI] [PubMed] [Google Scholar]
- 28. Drewes AM, Munkholm P, Simren M, et al. Definition, diagnosis and treatment strategies for opioid-induced bowel dysfunction—Recommendations of the Nordic Working Group. Scand J Pain 2016; 11: 111–122. [DOI] [PubMed] [Google Scholar]
- 29. Booth C. In: Kinney J, Haapala D, Booth C. (eds) Keeping families together: the homebuilders model. London; New York: Routledge, 2017, p. 13. [Google Scholar]
- 30. Upshur CC, Luckmann RS, Savageau JA. Primary care provider concerns about management of chronic pain in community clinic populations. J Gen Intern Med 2006; 21(6): 652–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Zuccaro SM, Vellucci R, Sarzi-Puttini P, et al. Barriers to pain management: focus on opioid therapy. Clin Drug Investig 2012; 32(Suppl. 1): 11–19. [DOI] [PubMed] [Google Scholar]
- 32. Maurer MA, Gilson AM, Husain SA, et al. Examining influences on the availability of and access to opioids for pain management and palliative care. J Pain Palliat Care Pharmacother 2013; 27(3): 255–260. [DOI] [PubMed] [Google Scholar]
- 33. Joranson DE, Ryan KM, Maurer M. Opioid policy, availability, and access in developing and non-industrialized countries. In: Fishman SM, Ballantyne JC, Rathmell JP. (eds) Bonica’s management of pain. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins, 2010, pp. 194–208. [Google Scholar]
- 34. Kwon JH. Overcoming barriers in cancer pain management. J Clin Oncol 2014; 32(16): 1727–1733. [DOI] [PubMed] [Google Scholar]
- 35. Dequeker S, Van Lancker A, Van Hecke A. Hospitalized patients’ vs. nurses’ assessments of pain intensity and barriers to pain management. J Adv Nurs 2018; 74(1): 160–171. [DOI] [PubMed] [Google Scholar]
- 36. Mularski RA, White-Chu F, Overbay D, et al. Measuring pain as the 5th vital sign does not improve quality of pain management. J Gen Intern Med 2006; 21(6): 607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Levy N, Sturgess J, Mills P. “Pain as the fifth vital sign” and dependence on the “numerical pain scale” is being abandoned in the US: why? Br J Anaesth 2018; 120(3): 435–438. [DOI] [PubMed] [Google Scholar]
- 38. Deldar K, Froutan R, Ebadi A. Challenges faced by nurses in using pain assessment scale in patients unable to communicate: a qualitative study. BMC Nurs 2018; 17: 11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, COREQ_checklist for Healthcare professionals’ perceptions on the use of opioid analgesics for the treatment of cancer-related pain in Cyprus: A mixed-method study by Andreas Charalambous, Marios Zorpas, Constantina Cloconi and Yolanda Kading in SAGE Open Medicine