Key Clinical Message
This case emphasizes the value of cardiac MRI and genetic testing in the early phase of ARVD/C. It also emphasizes the increased risk of SCD for patients with ARVD/C participating in competitive sports, even with immediate cardiopulmonary resuscitation.
Keywords: American football, arrhythmogenic right ventricular dysplasia/cardiomyopathy, ARVC, ARVD/C, athlete, exercise, magnetic resonance imaging, sarcoidosis, sudden cardiac death, syncope
1. INTRODUCTION
An American football player presented with exercise‐related syncopes. Cardiac MRI suggested ARVD/C, whereas ECG, SAECG, and echocardiogram were not diagnostic. Against medical advice, the athlete continued competitive sports until his death. This case emphasizes the value of cardiac MRI and genetic testing. Additionally, extracardiac sarcoidosis was diagnosed.
This case deals with exercise‐related syncopes in an athlete. The diagnostic work‐up reveals the reason for the syncopes, preceding the tragic death. Autopsy additionally reveals another co‐existing pathology.
2. CASE REPORT
A 28‐year‐old male athlete (176 cm, 105 kg) presented at our outpatient clinic after two episodes of exercise‐related syncope. He reported palpitations and loss of consciousness during intensive physical activity as an American football player. Family history was unremarkable regarding sudden cardiac death or cardiac disease at early age. Clinical examination, blood testing, and 12‐lead ECG did not reveal specific findings (Figure 1A). The transthoracic echocardiogram showed enlargement of the right ventricle without evidence of dyskinesia. Exercise‐testing and signal‐averaged ECG (SAECG) were without pathological findings (Figure 1B).
Figure 1.
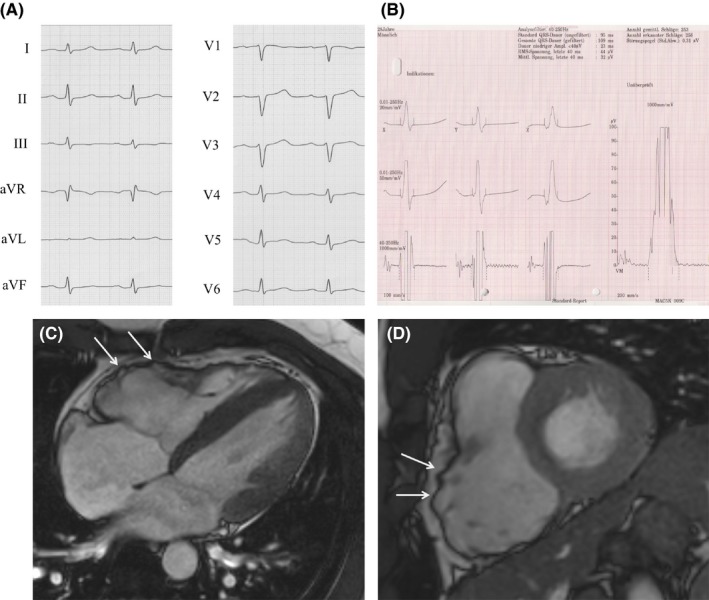
Illustrate parts of the diagnostic puzzle that finally led to the diagnosis ARVD/C and extracardiac sarcoidosis in a 28‐year‐old American football player with two exercise‐related syncopes. A, Unremarkable ECG (paper speed 50 mm/s): typical ARVD/C features as epsilon wave, T‐wave inversion or delayed terminal activation duration cannot be observed. B, Unremarkable signal‐averaged electrocardiogram (SAECG). C and D, Cardiac magnetic resonance imaging: cine images in 4‐chamber (C) and short‐axis views (D) in end‐systolic phase demonstrating a severely dilated right ventricle, ratio of RV end‐diastolic volume to BSA = 130 mL/m2 with bulging (arrows), regional dyssynchrony and moderately decreased right ventricular systolic function, RV ejection fraction = 42%. Cardiac MRI fulfilled one major criterion for ARVD/C
Cardiac magnetic resonance imaging demonstrated a severely dilated right ventricle with bulging, pronounced regional dyssynchrony, and moderately decreased right ventricular systolic function (RV ejection fraction = 42%, ratio of RV end‐diastolic volume to body surface area (BSA) = 130 mL/m2 (Figure 1C,D). Cardiac MRI fulfilled one major criterion for ARVD/C. Myocardial biopsy was refused by the patient. Genetic testing was scheduled.
We strongly advised against further intensive exercise. Against our advice, the athlete participated again in an intensive training, syncopated, walked to the paramedics, and syncopated again. The ECG showed ventricular fibrillation. Immediate electrical defibrillation was unsuccessful. The patient was then transferred to the hospital under continuous cardiopulmonary resuscitation. Defibrillation into sinus rhythm was successful after implantation of extracorporeal membrane oxygenation (ECMO). The young athlete died several hours after admission due to cerebral edema.
Postmortem genetic testing revealed a yet undescribed pathogenic plakophilin‐2 (PKP2) mutation that leads to premature truncation (NM_004572.3 c.1540_1543delAAAC). Autopsy confirmed the diagnosis of ARVD/C (Figure 2A,B). Furthermore, extracardiac sarcoidosis was revealed with epithelioid granuloma found in lungs, pleura, spleen, liver, lymph nodes, and the pelvis (Figure 2C,D). There was no evidence of cardiac involvement of sarcoidosis.
Figure 2.
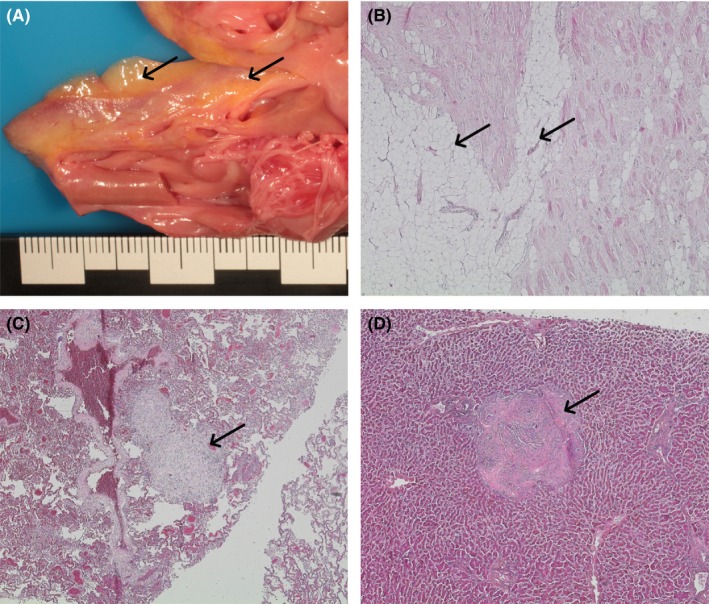
Illustrate parts of the diagnostic puzzle that finally led to the diagnosis ARVD/C and extracardiac sarcoidosis in a 28‐year‐old American football player with two exercise‐related syncopes. A, Macroscopic cross‐section of the right ventricle shows fat deposits (arrows) indicative for ARVD/C. B, Microscopic pattern of the right ventricle (stained with hematoxylin‐eosin) with typical fibrofatty replacement (arrows) of the myocardium and estimated <50% residual myocytes. C, Microscopic pattern of the lung (stained with hematoxylin‐eosin) with non‐necrotizing (non‐caseating) granulomas (arrow), typical for sarcoidosis. D, Microscopic pattern of the liver (stained with hematoxylin‐eosin) with non‐necrotizing (non‐caseating) granulomas (arrow), typical for sarcoidosis
3. DISCUSSION AND CONCLUSION
Cardiac sarcoidosis may be difficult to diagnose. As 2010 diagnostic criteria for ARVD/C have limited discrimination between cardiac sarcoidosis and ARVD/C, cardiac sarcoidosis is an important differential diagnosis.1, 2, 3 To the best of our knowledge, this is the first case being reported of an individual where both diseases could be confirmed. As ECG, SAECG, and echocardiogram were not diagnostic, this tragic case emphasizes the value of cardiac MRI and genetic testing in the early phase of ARVD/C. It also emphasizes the increased risk of SCD for patients with ARVD/C participating in competitive sports, even with immediate cardiopulmonary resuscitation.3, 4
CONFLICT OF INTEREST
None declared.
AUTHOR CONTRIBUTION
AM: involved in clinical work‐up, data collection, drafting of the manuscript. HK: involved in data collection, drafting of the manuscript. CC: involved in clinical work‐up, cardiac magnetic resonance imaging. CJ: involved in cardiac magnetic resonance imaging, revision of the manuscript. SR: involved in clinical work‐up, conceptional advice, revision of the manuscript. DH: involved in genetic counceling, revision of the manuscript. TG: involved in pathological examination, revision of the manuscript. GH: involved in conceptional advice, revision of the manuscript.
ACKNOWLEDGMENT
We presented this case as a poster at the EHRA Congress 2018 in Barcelona.4
Müssigbrodt A, Knopp H, Czimbalmos C, et al. Exercise‐related sudden cardiac death of an American football player with arrhythmogenic right ventricular dysplasia/cardiomyopathy AND sarcoidosis. Clin Case Rep. 2019;7:686–688. 10.1002/ccr3.2071
Andreas Müssigbrodt and Helge Knopp contributed equally and share first authorship.
REFERENCES
- 1. Marcus FI, McKenna WJ, Sherrill D, et al. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010;31:806‐814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Philips B, Madhavan S, James CA, et al. Arrhythmogenic right ventricular dysplasia/cardiomyopathy and cardiac sarcoidosis: distinguishing features when the diagnosis is unclear. Circ Arrhythm Electrophysiol. 2014;7:230‐236. [DOI] [PubMed] [Google Scholar]
- 3. Ruwald AC, Marcus F, Estes NA 3rd, et al. Association of competitive and recreational sport participation with cardiac events in patients with arrhythmogenic right ventricular cardiomyopathy: results from the North American multidisciplinary study of arrhythmogenic right ventricular cardiomyopathy. Eur Heart J. 2015;36:1735‐1743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Knopp H, Czimbalmos C, Jahnke C, et al. P464: Exercise‐related sudden cardiac death of an American football player with arrhythmogenic right ventricular dysplasia/cardiomyopathy and sarcoidosis. Europace. 2018;20(suppl. 1):i93. [DOI] [PMC free article] [PubMed] [Google Scholar]


