Key Clinical Message
Arteriovenous fistula is a well‐known but rarely diagnosed complication of percutaneous renal biopsy. On Doppler sonography, these fistulae are characterized by a region of high velocity shifts and random color assignment due to vibrating interfaces in the perivascular tissue. Most of them resolve spontaneously, while larger symptomatic ones need intervention.
Keywords: fistula, renal biopsy, ultrasound
1. QUIZ QUESTION: WHAT DO THE COLOR DOPPLER FINDINGS INDICATE IN THIS RENAL TRANSPLANT SONOGRAM?
A 56‐year‐old woman with a history of end‐stage renal disease secondary to diabetic nephropathy status post deceased donor kidney transplantation ~1.5 years prior, presented with acute kidney injury. Percutaneous renal allograft biopsy was consistent with acute T‐cell mediated rejection, and she was treated with pulse glucocorticoid therapy. The biopsy was performed under computed tomography (CT) guidance using a 16‐gauge needle, and three cores were obtained without any immediate complications. The serum creatinine stabilized around 1.7 mg/dL after treatment (2.3 mg/L at presentation). Four months later, an ultrasound examination of the allograft was performed because of mild elevation in serum creatinine to 2.1 mg/dL on routine labs. Doppler evaluation demonstrated prominent vascularity and turbulent flow in the lower pole of the kidney corresponding to the site of prior percutaneous biopsy suggestive of an acquired arteriovenous fistula (AVF) (Figures 1 and 2). The patient was asymptomatic, and blood pressure was stable and the urinalysis was negative for hematuria. We chose to manage her conservatively.
Figure 1.
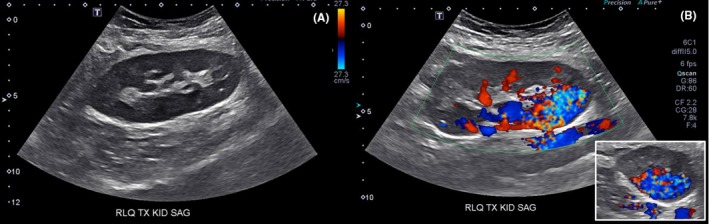
A, Gray scale renal ultrasound demonstrating normal appearing right lower quadrant renal allograft. B, Doppler ultrasound demonstrating prominent vascularity and turbulent flow in the lower pole suggestive of an arteriovenous fistula involving segmental‐interlobar vessels. Transverse view of the kidney is shown in the inset
Figure 2.
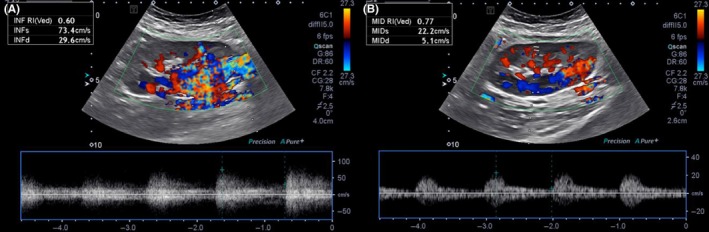
A, Pulsed wave Doppler imaging demonstrating high velocities and turbulent flow in the fistula region. B, Examination of the arcuate vessel is included for comparison, showing low velocities, and better defined systolic and diastolic flows
The incidence of AVF is estimated to be about 0.3%‐6% following native kidney biopsy and up to 10%‐16% in transplanted kidneys. However, ~70% of AVFs are asymptomatic and are resorbed spontaneously within weeks.1 Larger or symptomatic lesions require interventions such as super‐selective trans‐catheter embolization.2
CONFLICT OF INTEREST
None declared.
Informed consent: Obtained from the patient.
AUTHOR CONTRIBUTION
HB: drafted the manuscript and participated in patient care. AHS: transplant nephrologist on the case; directed patient care. AK: reviewed and revised the manuscript for critically important intellectual content and procured the images.
Bejjanki H, Santos AH, Koratala A. Postbiopsy arteriovenous fistula in renal allograft: An ultrasound case study. Clin Case Rep. 2019;7:834–835. 10.1002/ccr3.2059
REFERENCES
- 1. Lubomirova M, Krasteva R, Bogov B, Paskalev E. Incidence of A‐V Fistulas after renal biopsy of native and transplanted kidney ‐ two centers experience. Open Access Maced J Med Sci. 2015;3(2):241‐244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Loffroy R, Guiu B, Lambert A, et al. Management of post‐biopsy renal allograft arteriovenous fistulas with selective arterial embolization: immediate and long‐term outcomes. Clin Radiol. 2008;63(6):657‐665. [DOI] [PubMed] [Google Scholar]


