Abstract
Medicaid patients are known to have reduced access to care compared with privately insured patients; however, quantifying this disparity with large controlled studies remains a challenge. This meta-analysis evaluates the disparity in health services accessibility of appointments between Medicaid and privately insured patients through audit studies of health care appointments and schedules. Audit studies evaluating different types of outpatient physician practices were selected. Studies were categorized based on the characteristics of the simulated patient scenario. The relative risk of appointment availability was calculated for all different types of audit scenario characteristics. As a secondary analysis, appointment availability was compared pre- versus post-Medicaid expansion. Overall, 34 audit studies were identified, which demonstrated that Medicaid insurance is associated with a 1.6-fold lower likelihood in successfully scheduling a primary care appointment and a 3.3-fold lower likelihood in successfully scheduling a specialty appointment when compared with private insurance. In this first meta-analysis comparing appointment availability between Medicaid and privately insured patients, we demonstrate Medicaid patients have greater difficulty obtaining appointments compared with privately insured patients across a variety of medical scenarios.
Keywords: appointments and schedules, health services accessibility, Medicaid, insurance, patient protection and affordable care act, healthcare disparities, primary health care, meta-analysis
What do we already know about this topic?
Medicaid patients generally have less access to care compared to patients with other insurances, and they may have more difficulty obtaining health care appointments.
How does your research contribute to the field?
The current literature has had a difficult time quantifying the reduced access to care that Medicaid patients experience in a large controlled study. Numerous small audit studies have been performed to evaluate this disparity, but currently no meta-analysis of these studies exists.
What are your research’s implications toward theory, practice, or policy?
We highlight the disparity in appointment accessibility between Medicaid and privately insured patients and hope that it may inform Medicaid reform, particularly in a post-Patient Protection and Affordable Care Act era.
Introduction
Medicaid patients experience increased barriers to care compared with privately insured patients. In a nationwide survey of primary care providers in 2015, only 45% indicated they were willing to accept new Medicaid patients while 94% were willing to accept new privately insured patients.1 This difference in insurance acceptance is attributed to Medicaid’s low reimbursement levels, disadvantaged patient population, and high administrative burden compared with other insurance.2 This lower rate of Medicaid compared with private insurance acceptance leads to disparities in care due to decreased access to health care services.
Over the years, the term access has taken on several definitions and frameworks. One widely accepted model developed by Penchansky and Thomas defines access as the degree of “fit” between the patient and the healthcare system. Integrated into this model are the concepts of affordability (the patient’s ability to pay for his or her care and whether physicians accept his or her insurance) and availability (the adequacy of the supply of medical providers, clinics, and services).3 Over the years, within the framework established by Penchansky and Thomas, the concept of affordability has been quantified by measuring the ease or difficulty associated with a patient obtaining an appointment,4 and the extent to which physicians make themselves accessible to patients.5
Patient surveys and appointment availability audit studies have been proposed as potential methods of measuring patient access to care. Recently, direct patient surveys6-9 have been used to measure the effectiveness of the Patient Protection and Affordable Care Act (PPACA) in improving patient access to care. However, these phone surveys are typically dependent on self-reported data or investigator-moderated interviews, which are subject to confirmation biases (interviewers are seeking information that supports a preconceived belief).
In contrast, appointment availability audit studies, also known as secret shopper studies, have been shown to be effective in evaluating appointment availability and the ability to receive an appointment by using simulated patients with different insurance plans to call physician offices and attempt to schedule appointments.10 Because the audit study design directly examines the obstacles patients confront when they attempt to access care and sheds light on the patient experience of obtaining care, it can be used to examine the disparity in access for Medicaid patients relative to privately insured patients. Although many accessibility audit studies have been conducted over the years, a meta-analysis has not been conducted to examine their conclusions in aggregate. Using pooled data from 34 audit studies, this meta-analysis directly evaluates the disparity between patients with private and Medicaid insurance in their ability to schedule a new patient appointment.
Methods
Search Strategy
We performed the systematic review in accordance with the PRISMA statement.11 A librarian and two independent authors conducted searches for relevant articles in Ovid Medline (1946 to January 19, 2017), Ovid Medline (In Process & Other Non-Indexed Citations), and Ovid Embase (1974 to January 19, 2017) on January 20, 2017. The databases were searched using both controlled vocabulary and free-text terms. The Yale MeSH Analyzer (http://mesh.med.yale.edu) was used in the initial stages of strategy formulation to harvest controlled vocabulary and keyword terms from highly relevant known articles. The search strategy for Ovid MEDLINE is documented in the Supplementary Appendix. In addition, we performed a hand search and screened the reference lists of selected papers for further relevant literature.
Study Selection
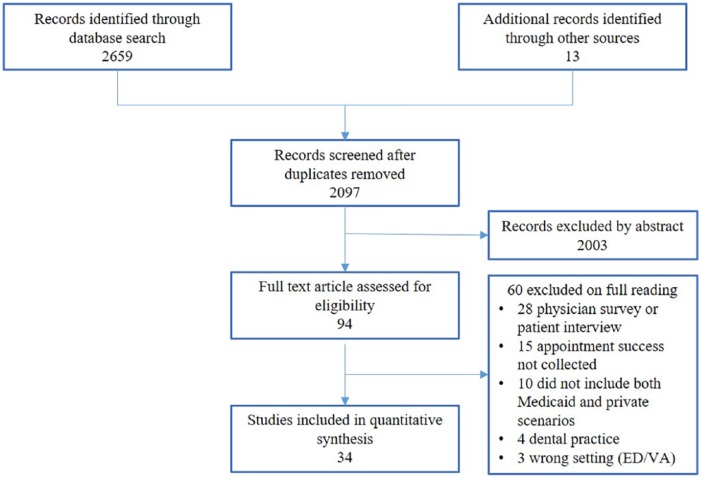
Figure 1 summarizes the study selection process. Studies were eligible for inclusion if they used an audit study methodology to compare a simulated Medicaid patient’s ability to successfully schedule a physician appointment with that of a simulated privately insured patient. All types of outpatient physician practices ranging from primary care to surgical specialties were included. We excluded any studies performed outside the United States or published before 2001. Studies that were designed as physician surveys or patient interviews were excluded. Studies that examined patient access to care in emergency departments, veteran affairs hospitals, or to dentists were also excluded. Literature from the electronic searches was imported into Covidence, a screening and data extraction tool.12 Within Covidence, two independent authors inspected the title and abstract of each study. After initial screening, full texts were retrieved and reviewers performed a second round of independent review based on their review of the entire article.
Figure 1.
Flow chart of study selection.
Source. Author’s selection of studies based on predetermined criteria, 2017.
Note. ED = emergency department; VA = veteran affairs.
Data Extraction
Two independent authors extracted data from the included studies and any disagreements were resolved by discussion with a third reviewer. Explanatory variables included year data collected, location of physician practices investigated, the type of physician practice investigated, scenario of the patient seeking an appointment, age of the patient, and the type of insurance investigated. We extracted whether the studies were conducted pre- or post-Medicaid expansion and whether the state in which the data were collected had undergone Medicaid expansion at the time of the study.
The outcome variable of interest was the number of successful appointments scheduled based on insurance type. Appointment success was defined as the ability of a patient to schedule an appointment, either within or without a specified time frame (studies ranged from 1 to 2 weeks). Requests for appointments were considered unsuccessful if the practice was not accepting new patients with the caller’s type of insurance or the scheduler did not grant an appointment due to additional practice requirements such as the requirement of a referral or preappointment chart review. Many studies did not differentiate between reasons for why Medicaid was not accepted (ie, whether the provider did not take Medicaid at all or whether the provider was not accepting new patients with Medicaid). Therefore, this outcome measure was not addressed in our analysis. Risk of bias was assessed for each study using the Cochrane Collaboration’s tool (see Supplementary Appendix).
Statistical Methods
The meta-analysis was specified to compare access with Medicaid versus private insurance. For studies that included other insurance types, notably Medicare, only the Medicaid and private insurance data were included in the analysis. The most consistently available outcome reported was the binary response to whether an appointment could be scheduled. Some studies reported on appointment availability at various time points from the call (eg, within 1 week, 2 weeks, etc). For these studies, the most permissive time point was included in the analysis.
For each study, relative risk (RR) of appointment availability based on insurance status was calculated using abstracted data. The possibility of publication bias was assessed by visual inspection of a standard funnel plot.13 We assumed a priori that substantial heterogeneity would exist between studies due to variability in the regions, practices, dates, and scenarios, among other factors, and therefore used a random effects model for meta-analysis. Studies were combined using an inverse variance approach.14 In cases of studies with no events, a standard fixed continuity correction was used. Heterogeneity between studies was evaluated using I2.15
We conducted 2 analyses. The primary analysis compared access by scenario characteristics, which included type of medical scenario (primary care and specialty scenarios), age of patient in the scenario (adult and pediatric), and timing of the scenario (urgent and nonurgent). For studies involving multiple specialties, data were extracted for each component specialty and treated as separate studies in the subgroup analysis. The secondary analysis split studies based on data collection date before and after the implementation of PPACA’s Medicaid expansion. However, the results were not categorized by scenario type due to the limited number of studies for primary care and urgent scenarios that were conducted post-Medicaid expansion. Therefore, the results were pooled to provide a suggestive trend of accessibility pre- versus post-PPACA. Data were analyzed using Stata Statistical Software: Release 13.1 (StataCorp LP).
Results
Study Characteristics
Table S1 in Supplemental Material summarizes the study characteristics of the 34 articles included in this review.16-49 In total, the 34 studies represented 21,601 calls to provider offices requesting an appointment for Medicaid and private insurance scenarios, of which 63% resulted in successful scheduling. Of 11,387 calls with private insurance, 80% of calls successfully led to appointments, while 45% of 10 214 calls with Medicaid resulted in none. The mean number of calls made per study under the private insurance and Medicaid scenario was 335 and 300, respectively (private insurance: median = 116, range = 14-5,385, SD = 906; Medicaid: median = 118, range = 14-4,352, SD = 731).
Risk of Bias
The overall quality assessment of the included studies was reported in Table S2 in Supplemental Material. Due to the nature of the audit study methodology, studies could only meet a maximum of 6 out of the 8 quality assessment domains. All studies were subject to allocation concealment bias and blinding of personnel bias. The observed effect size, presented as odds ratios, is plotted against the standard error in a typical funnel plot (Figure 2). The figure shows an abundance of smaller studies with larger effect size, with a much smaller cluster of studies showing either no or a reversed effect. This pattern is typical of publication bias in which small studies showing no effect are not present in the literature.
Figure 2.
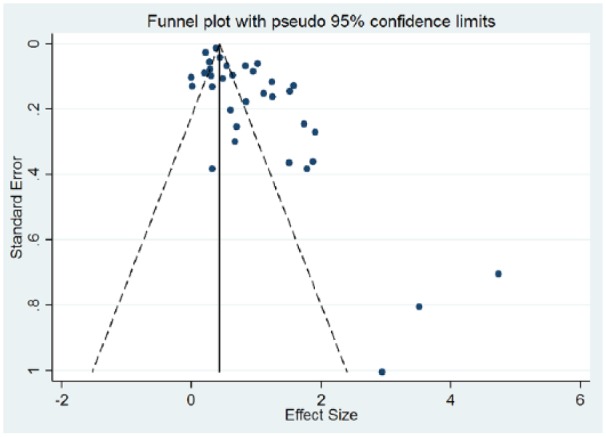
Funnel plot of selected studies.
Source. Author’s analysis of 34 audit studies, 2017.
Appointment Success by Medical Scenario
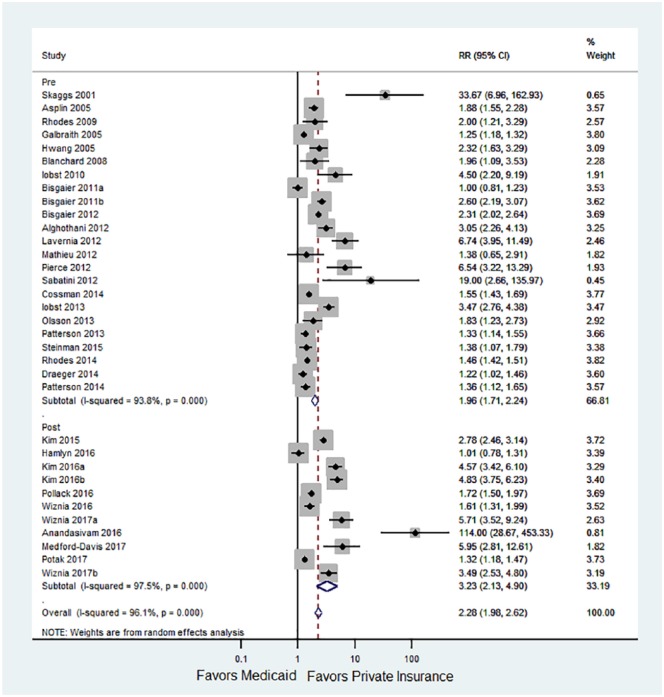
The number of successful and unsuccessful calls in each insurance group in each study is displayed in Table S3 in Supplemental Material. Figure 3 shows the RRs and confidence interval (CI) of getting an appointment with private insurance compared with Medicaid for each study. Tables 1 and 2 list the RR and CIs for appointment success based on the characteristics of each audit study’s scenario (primary care/pediatric vs specialty care scenario, adult vs pediatric scenario, urgent vs nonurgent scenarios). These scenarios were grouped regardless of whether they were conducted before or after Medicaid expansion. The RR values compare the risk of a private patient obtaining an appointment with a Medicaid patient. Privately insured patients were more likely to receive an appointment over a patient with Medicaid when seeking specialty care (RR = 3.3, 95% CI = 2.4-4.5). The advantage of private insurance over Medicaid in access to care was least in primary care/general pediatric scenarios (RR = 1.6, 95% CI = 1.4-1.9). Adult private patients had a statistically significant greater advantage in securing appointments over adult Medicaid patients (RR = 2.6, 95% CI = 2.1-3.3), and this advantage was also significant for adult private patients when compared with their pediatric counterparts (RR = 1.8, 95% CI = 1.7-1.9). Appointment availability did not differ for those with urgent versus nonurgent medical scenarios. In a sensitivity analysis with all orthopedics audit studies removed, private patients were still significantly more likely to receive an appointment over a Medicaid patient overall (RR = 1.8, 95% CI = 1.6-2.1).
Figure 3.
The RR and CI of getting an appointment with private insurance compared with Medicaid.
Source. Author’s analysis of 34 audit studies, 2017.
Note. RR = relative risk; CI = confidence interval.
Table 1.
RR of Appointment Accessibility Based on the Study Characteristic.
| RR | 95% CI | |
|---|---|---|
| Primary care/general pediatric (n = 9) | 1.6 | 1.4-1.9 |
| Specialty (n = 25) | 3.3 | 2.4-4.5 |
| Adult (n = 22) | 2.6 | 2.1-3.3 |
| Pediatric (n = 12) | 1.8 | 1.7-1.9 |
| Urgent (n = 13) | 2.4 | 1.7-3.3 |
| Nonurgent (n = 21) | 2.5 | 2.1-3.1 |
Note. RR = relative risk of a patient with private insurance receiving an appointment over a patient with Medicaid; CI = confidence interval.
Table 2.
RR of Appointment Accessibility Pre- and Post-PPACA.
| RR | 95% CI | |
|---|---|---|
| All studies (n = 34) | 2.3 | 2.0-2.6 |
| Pre-PPACA (n = 23) | 2.0 | 1.7-2.2 |
| Post-PPACA (n = 11) | 3.2 | 2.1-4.9 |
Note. PPACA = Patient Protection and Affordable Care Act; RR = relative risk of a patient with private insurance receiving an appointment over a patient with Medicaid; CI = confidence interval.
Appointment Success Pre- and Post-PPACA
Our secondary analysis demonstrates a trend of reduced appointment accessibility for Medicaid patients post-PPACA compared with pre-PPACA. In all studies prior to Medicaid expansion, Medicaid patients had a 2-fold lower likelihood of securing an appointment compared with privately insured patients. In all studies after Medicaid expansion, Medicaid patients had a 3.2-fold lower likelihood of securing an appointment compared with privately insured patients. There was marked heterogeneity between studies, with I2 of 96%, indicating that the variation in the estimate effect is due to significantly measured difference between studies rather than random error within studies.
Discussion
Appointment availability audit studies aim to define access in terms of a patient’s ability to obtain an appointment. Our comprehensive meta-analysis of audit studies examining patient access to care demonstrates that Medicaid patients have reduced access to appointment scheduling compared with their privately insured counterparts. Specifically, Medicaid patients have a more difficult time securing an appointment for specialty care compared with primary care, and appointments for adult patients are more difficult to make than appointments for pediatric patients. The urgency of a clinical scenario did not affect the difference in the reduced baseline accessibility for Medicaid patients.
Our study approached accessibility by examining the disparity in the ability to schedule new patient appointments between patients with private and Medicaid insurance to measure the tangible effects that insurance status has on appointment accessibility. Appointment availability audit studies serve as a metric to evaluate patient access to care, which can identify and quantify specific obstacles to obtaining an appointment, calculate actual physician participation rates in the treatment of Medicaid patients compared with other patients, and measure the length of time a patient must wait to be seen.5,10 Audit studies may portray patient access more accurately than direct patient surveys because the audit study design blinds appointment schedulers, greatly reducing the risk of participant bias.10 To our knowledge, this study is the first meta-analysis to examine audit studies and quantify access between Medicaid and privately insured patients using appointment accessibility.
Our results demonstrate that Medicaid patients are more likely to be excluded from the practice of their choice and may need to make considerably more effort to secure an appointment given their limited access to certain centers. However, our findings do not necessarily mean that care for Medicaid patients is worse, but Medicaid patients’ options are, de facto, reduced. Many of the audit studies in our meta-analysis do not identify the reasons physicians may reject Medicaid patients. Seemingly, such reasons could include that the provider is not taking any new patients with Medicaid, the provider does not accept Medicaid insurance, or that the provider is taking new Medicaid patients, but the wait times are untimely or unreasonable.
Some medical specialties, such as orthopedics and psychiatry, have worse patient access than others, such as primary care.50 As our meta-analysis includes a high number of orthopedic surgery audit studies, and we were worried that this weighting might bias the results, we conducted a subanalysis with the orthopedics studies removed. We found that with the orthopedic studies removed, the overall results still remain significant and follow the same direction, but with a reduced magnitude.
Because of the limited number of post-PPACA access studies, we are unable to draw a conclusion comparing appointment success pre- and post-PPACA. Future studies could follow the recently published example by Polsky et al,51 who performed a comparison of 2 appointment availability audit studies focused on primary care, one conducted before the implementation of Medicaid expansion, and a second after Medicaid expansion based on identical methods from a 2012 to 2013 baseline pre-PPACA study. Such studies should be repeated for a wide breadth of specialty and scenario types highlighted in our meta-analysis.
Recently, an issue brief by Antonisse et al6 and a systematic review by Mazurenko et al52 examining the effects of Medicaid Expansion on the PPACA concluded that patient access was positively affected. Although our study does not claim to address all measures associated with access as is covered in these 2 reviews, we are reporting on an audit methodology that we believe accurately represents a measure of access when comparing Medicaid patients and privately insured patients. Unfortunately, our meta-analysis does not have an adequate number of post-PPACA Medicaid expansion studies to draw any conclusions.
Using data from the National Health Interview Survey, Miller and Wherry53 recently demonstrated that Medicaid expansion was associated with longer wait times for appointments, indicating that problems regarding accessibility persist. Ultimately, Medicaid patients may have access to care through Federally Qualified Community Health Centers (FQHCs), academic practices, or public/nonprofit safety net hospitals that care for more uninsured and Medicaid patient populations. This hypothesis is supported by a Kaiser Family Foundation report, which demonstrated that nationally, since Medicaid expansion, federally-funded community health centers had seen a greater than 10% increase in their patient caseload, an 11% increase in insured patients, and an 8% increase in total Medicaid patients.54 Therefore, although our study demonstrates that Medicaid patients do not have the same access to certain physicians, these patients may very well have good access or even better care when seeking care in FQHCs and academic centers which dominate certain regions.
This study has several limitations beyond those already discussed. Although this meta-analysis included studies sharing the same primary outcome, there are differences in patient scenarios, physician types, and geographic regions. Although the data are from studies representing all states plus the District of Columbia, over one-third of the studies investigated 7 large states (California, Florida, New York, North Carolina, Ohio, Texas, and Massachusetts) that are influential in politics, and thus the data may not be fully reflective of the nation. In addition, there were chronological time periods in which certain specialties of interest and geographic regions were focused on. This meta-analysis cannot isolate the effect of the PPACA from potential confounders, nor can it improve on the quality of the individual studies. For example, the type of patient scenario varies widely from study to study. Our subgroup analysis aimed to minimize this variability by specialty, age, and urgency; however, other changing variables at the state level or time to adoption may affect the observed outcomes. In some geographic regions, there can be good access to care even if many practices do not accept Medicaid, particularly if academic medical centers and/or FQHCs that nearly universally do accept Medicaid are located within the region.55 Given that individual studies did not distinguish between FQHCs, academic centers, and private practices, we are unable to fully comment on how practice type affected access to care. At least 10 studies included academic medical centers and academic physicians as part of their sample. No studies stated whether FQHCs were included in the survey. However, given that audit studies are less likely to reach out to FQHCs or academic centers, it is possible that Medicaid access is better than what is portrayed in this meta-analysis because these centers are a critical part of the care delivery for Medicaid patients. The appointment availability audit study design is a real-world approach to assessing access by minimizing biases associated with surveys and interviews; however, it is a labor-intensive and imperfect process that limits sample sizes. We also could not account for Medicaid reimbursement levels, which vary considerably by state. Some states may have relatively high primary care reimbursements but poor specialty reimbursement or vice versa that may present with unique patient acceptance patterns. Finally, our study design only allows us to examine the effect of Medicaid on accessibility but did not allow us to measure the change in appointment accessibility among the uninsured population, as different studies accepted disparate definitions of uninsured patients, including those who were cash-pay or those without any insurance. These definitions make up two distinct types of patients and could confound our observed results. Future research in insurance access research should examine other insurance types like Medicare or uninsured patients, as well as changes in Medicaid insurance with corresponding changes pre- and post-PPACA.
Conclusion
In the first meta-analysis of appointment availability audit studies, we demonstrate that Medicaid patients have reduced access to appointments compared with their privately insured counterparts. Specifically, Medicaid patients have a more difficult time securing an appointment for specialty care compared with primary care. In addition, appointments for adult Medicaid patients are more difficult to schedule than appointments for pediatric Medicaid patients. Although more patients may have insurance since the implementation of Medicaid expansion, these newly insured Medicaid patients may have a relatively harder time obtaining appointments compared with privately insured patients.
Supplemental Material
Supplemental material, Supplementary_materials for Medicaid Patients Have Greater Difficulty Scheduling Health Care Appointments Compared With Private Insurance Patients: A Meta-Analysis by Walter R. Hsiang, Adam Lukasiewicz, Mark Gentry, Chang-Yeon Kim, Michael P. Leslie, Richard Pelker, Howard P. Forman and Daniel H. Wiznia in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
The authors would like to thank Cary Gross, MD, for his critical input and advice during the planning and writing of this article.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
ORCID iDs: Walter R. Hsiang  https://orcid.org/0000-0002-4718-6231
https://orcid.org/0000-0002-4718-6231
Mark Gentry  https://orcid.org/0000-0002-3542-8803
https://orcid.org/0000-0002-3542-8803
References
- 1. Boccuti C, Fields C, Casillas G, Hamel L. Primary care physicians accepting Medicare: a snapshot. https://www.kff.org/medicare/issue-brief/primary-care-physicians-accepting-medicare-a-snapshot/. Published October 2015. Accessed March 8, 2019.
- 2. Ryan J, Doty M, Hamel L, Norton M, Abrams M, Brodie M. Primary care providers’ views of recent trends in health care delivery and payment. https://www.commonwealthfund.org/publications/issue-briefs/2015/aug/primary-care-providers-views-recent-trends-health-care-delivery. Published August 2015. Accessed March 8, 2019.
- 3. Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19(2):127-140. [DOI] [PubMed] [Google Scholar]
- 4. Frenk J. Concept and measurement of accessibility. Salud Publica Mex. 1985;27(5):438-453. [PubMed] [Google Scholar]
- 5. Hall AG, Lemak CH, Steingraber H, Schaffer S. Expanding the definition of access: it isn’t just about health insurance. J Health Care Poor Underserved. 2008;19(2):625-638. [DOI] [PubMed] [Google Scholar]
- 6. Antonisse L, Garfield R, Rudowitz R, Artiga S. The effects of Medicaid expansion under the ACA: updated findings from a literature review. https://www.kff.org/medicaid/issue-brief/the-effects-of-medicaid-expansion-under-the-aca-updated-findings-from-a-literature-review-march-2018/. Published March 2018. Accessed March 8, 2019.
- 7. Collins SR, Gunja M, Doty MM, Beutel S. Americans’ experiences with ACA marketplace and Medicaid coverage: access to care and satisfaction: findings from the commonwealth fund Affordable Care Act tracking survey, February-April 2016. Issue Brief (Commonw Fund). 2016;14:1-18. [PubMed] [Google Scholar]
- 8. Kirby JB, Vistnes JP. Access to care improved for people who gained Medicaid or marketplace coverage in 2014. Health Aff (Millwood). 2016;35(10):1830-1834. [DOI] [PubMed] [Google Scholar]
- 9. Shartzer A, Long SK, Anderson N. Access to care and affordability have improved following Affordable Care Act implementation: problems remain. Health Aff (Millwood). 2016;35(1):161-168. [DOI] [PubMed] [Google Scholar]
- 10. Steinman KJ, Kelleher K, Dembe AE, Wickizer TM, Hemming T. The use of a “mystery shopper” methodology to evaluate children’s access to psychiatric services. J Behav Health Serv Res. 2012;39(3):305-313. [DOI] [PubMed] [Google Scholar]
- 11. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. PLoS Med. 2009;6(7):e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Elliot J. Covidence Systematic Review Software. Melbourne, Australia: Veritas Health Innovation; 2017. [Google Scholar]
- 13. Sterne JA, Egger M, Smith GD. Systematic reviews in health care: investigating and dealing with publication and other biases in meta-analysis. BMJ. 2001;323(7304):101-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7(3):177-188. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557-560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Alghothani L, Jacks SK, Vander Horst A, Zirwas MJ. Disparities in access to dermatologic care according to insurance type. Arch Dermatol. 2012;148(8):956-957. [DOI] [PubMed] [Google Scholar]
- 17. Anandasivam NS, Wiznia DH, Kim CY, Save AV, Grauer JN, Pelker RR. Access of patients with lumbar disc herniations to spine surgeons: the effect of insurance type under the Affordable Care Act. Spine. 2017;42:1179-1183. [DOI] [PubMed] [Google Scholar]
- 18. Asplin BR, Rhodes KV, Levy H, et al. Insurance status and access to urgent ambulatory care follow-up appointments. JAMA. 2005;294(10):1248-1254. [DOI] [PubMed] [Google Scholar]
- 19. Bisgaier J, Levinson D, Cutts DB, Rhodes KV. Access to autism evaluation appointments with developmental-behavioral and neurodevelopmental subspecialists. Arch Pediatr Adolesc Med. 2011;165(7):673-674. [DOI] [PubMed] [Google Scholar]
- 20. Bisgaier J, Polsky D, Rhodes KV. Academic medical centers and equity in specialty care access for children. Arch Pediatr Adolesc Med. 2012;166(4):304-310. [DOI] [PubMed] [Google Scholar]
- 21. Bisgaier J, Rhodes KV. Auditing access to specialty care for children with public insurance. N Engl J Med. 2011;364(24):2324-2333. [DOI] [PubMed] [Google Scholar]
- 22. Blanchard J, Ogle K, Thomas O, Lung D, Asplin B, Lurie N. Access to appointments based on insurance status in Washington, D.C. J Health Care Poor Underserved. 2008;19(3):687-696. [DOI] [PubMed] [Google Scholar]
- 23. Cossman RE, Cossman JS, Rogers S, et al. Access to primary care physicians differs by health insurance coverage in Mississippi. South Med J. 2014;107(2):87-90. [DOI] [PubMed] [Google Scholar]
- 24. Draeger RW, Patterson BM, Olsson EC, Schaffer A, Patterson JM. The influence of patient insurance status on access to outpatient orthopedic care for flexor tendon lacerations. J Hand Surg Am. 2014;39(3):527-533. [DOI] [PubMed] [Google Scholar]
- 25. Galbraith AA, Grossman DC, Koepsell TD, Heagerty PJ, Christakis DA. Medicaid acceptance and availability of timely follow-up for newborns with Medicaid. Pediatrics. 2005;116(5):1148-1154. [DOI] [PubMed] [Google Scholar]
- 26. Hamlyn GS, Hutchins KE, Johnston AL, Thomas RT, Tian J, Kamal AH. Accessibility and barriers to oncology appointments at 40 national cancer institute-designated comprehensive cancer centers: results of a mystery shopper project. J Oncol Pract. 2016;12(10):e884-e900. [DOI] [PubMed] [Google Scholar]
- 27. Hwang AH, Hwang MM, Xie HW, Hardy BE, Skaggs DL. Access to urologic care for children in California: Medicaid versus private insurance. Urology. 2005;66(1):170-173. [DOI] [PubMed] [Google Scholar]
- 28. Iobst C, King W, Baitner A, Tidwell M, Swirsky S, Skaggs DL. Access to care for children with fractures. J Pediatr Orthop. 2010;30(3):244-247. [DOI] [PubMed] [Google Scholar]
- 29. Iobst C, Arango D, Segal D, Skaggs DL. National access to care for children with fractures. J Pediatr Orthop. 2013;33(6):587-591. [DOI] [PubMed] [Google Scholar]
- 30. Kim CY, Wiznia DH, Hsiang WR, Pelker RR. The effect of insurance type on patient access to knee arthroplasty and revision under the Affordable Care Act. J Arthroplasty. 2015;30(9):1498-1501. [DOI] [PubMed] [Google Scholar]
- 31. Kim CY, Wiznia DH, Roth AS, Walls RJ, Pelker RR. Survey of patient insurance status on access to specialty foot and ankle care under the Affordable Care Act. Foot Ankle Int. 2016;37(7):776-781. [DOI] [PubMed] [Google Scholar]
- 32. Kim CY, Wiznia DH, Wang Y, et al. The effect of insurance type on patient access to carpal tunnel release under the Affordable Care Act. J Hand Surg Am. 2016;41(4):503-509.e1. [DOI] [PubMed] [Google Scholar]
- 33. Lavernia CJ, Contreras JS, Alcerro JC. Access to arthroplasty in South Florida. J Arthroplasty. 2012;27(9):1585-1588. [DOI] [PubMed] [Google Scholar]
- 34. Mathieu RP, Blanchard J, Sekaran A, Nash R, Winter L, Prideaux C. Access to urgent pediatric primary care appointments in the District of Columbia. Acad Emerg Med. 2012;19:S137. [Google Scholar]
- 35. Medford-Davis L, Lin F, Greenstein A, Rhodes KV. “I broke my ankle”: access to orthopedic follow-up care by insurance status. Acad Emerg Med. 2017;24(1):98-105. [DOI] [PubMed] [Google Scholar]
- 36. Olsson E, Lim MR, Mackinnon-Patterson B, Draeger RW. Access to outpatient care for adult lumbar disc herniation patients with private insurance versus Medicaid. Spine J. 2013;13(9):S14. [DOI] [PubMed] [Google Scholar]
- 37. Patterson BM, Draeger RW, Olsson EC, Spang JT, Lin FC, Kamath GV. A regional assessment of Medicaid access to outpatient orthopaedic care: the influence of population density and proximity to academic medical centers on patient access. J Bone Joint Surg Am. 2014;96(18):e156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Patterson BM, Spang JT, Draeger RW, Olsson EC, Creighton RA, Kamath GV. Access to outpatient care for adult rotator cuff patients with private insurance versus Medicaid in North Carolina. J Shoulder Elbow Surg. 2013;22(12):1623-1627. [DOI] [PubMed] [Google Scholar]
- 39. Pierce TR, Mehlman CT, Tamai J, Skaggs DL. Access to care for the adolescent anterior cruciate ligament patient with Medicaid versus private insurance. J Pediatr Orthop. 2012;32(3):245-248. [DOI] [PubMed] [Google Scholar]
- 40. Pollack CE, Ross ME, Armstrong K, et al. Using a mystery-caller approach to examine access to prostate cancer care in Philadelphia. PLoS One. 2016;11(10):e0164411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Potak H, Iobst C. Influence of Insurance Type on the Access to Pediatric Care for Children with Distal Radius Torus Fractures. Pediatrics. 2018;141(1):671-671. [DOI] [PubMed] [Google Scholar]
- 42. Rhodes KV, Kenney GM, Friedman AB, et al. Primary care access for new patients on the eve of health care reform. JAMA Intern Med. 2014;174(6):861-869. [DOI] [PubMed] [Google Scholar]
- 43. Rhodes KV, Vieth TL, Kushner H, Levy H, Asplin BR. Referral without access: for psychiatric services, wait for the beep. Ann Emerg Med. 2009;54(2):272-278. [DOI] [PubMed] [Google Scholar]
- 44. Sabatini CS, Skaggs KF, Kay RM, Skaggs DL. Orthopedic surgeons are less likely to see children now for fracture care compared with 10 years ago. J Pediatr. 2012;160(3):505-507. [DOI] [PubMed] [Google Scholar]
- 45. Skaggs DL, Clemens SM, Vitale MG, Femino JD, Kay RM. Access to orthopedic care for children with Medicaid versus private insurance in California. Pediatrics. 2001;107(6):1405-1408. [DOI] [PubMed] [Google Scholar]
- 46. Steinman KJ, Shoben AB, Dembe AE, Kelleher KJ. How Long Do Adolescents Wait for Psychiatry Appointments. Community Ment Health J. 2015;51:782-789. [DOI] [PubMed] [Google Scholar]
- 47. Wiznia DH, Maisano J, Kim CY, Zaki T, Lee HB, Leslie MP. The effect of insurance type on trauma patient access to psychiatric care under the Affordable Care Act. Gen Hosp Psychiatry. 2017;45:19-24. [DOI] [PubMed] [Google Scholar]
- 48. Wiznia DH, Ndon S, Kim CY, Zaki T, Leslie MP. The effect of insurance type on fragility fracture patient access to endocrinology under the Affordable Care Act. Geriatr Orthop Surg Rehabil. 2017;8(1):23-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wiznia DH, Zaki T, Maisano J, Kim CY, Halaszynski TM, Leslie MP. Influence of medical insurance under the Affordable Care Act on access to pain management of the trauma patient. Reg Anesth Pain Med. 2017;42(1):39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Bishop TF, Press MJ, Keyhani S, Pincus HA. Acceptance of insurance by psychiatrists and the implications for access to mental health care. JAMA Psychiatry. 2014;71(2):176-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Polsky D, Candon M, Saloner B, et al. Changes in primary care access between 2012 and 2016 for new patients with Medicaid and private coverage. JAMA Intern Med. 2017;177(4):588-590. [DOI] [PubMed] [Google Scholar]
- 52. Mazurenko O, Balio CP, Agarwal R, Carroll AE, Menachemi N. The effects of Medicaid expansion under the ACA: a systematic review. Health Aff (Millwood). 2018;37(6):944-950. [DOI] [PubMed] [Google Scholar]
- 53. Miller S, Wherry LR. Health and access to care during the first 2 years of the ACA Medicaid expansions. N Engl J Med. 2017;376(10):947-956. [DOI] [PubMed] [Google Scholar]
- 54. Paradise J, Rosenbaum S, Markus A, et al. Community health centers: recent growth and the role of the ACA. https://www.kff.org/medicaid/issue-brief/community-health-centers-recent-growth-and-the-role-of-the-aca/. Published January 2017. Accessed March 8, 2019.
- 55. Kaiser Family Foundation. Community health center delivery sites and patient visits. https://www.kff.org/other/state-indicator/community-health-center-sites-and-visits/?currentTimeframe=0&sortModel=%7B%22colId%22:%22Location%22,%22sort%22:%22asc%22%7D. Published 2017. Accessed March 8, 2019.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplementary_materials for Medicaid Patients Have Greater Difficulty Scheduling Health Care Appointments Compared With Private Insurance Patients: A Meta-Analysis by Walter R. Hsiang, Adam Lukasiewicz, Mark Gentry, Chang-Yeon Kim, Michael P. Leslie, Richard Pelker, Howard P. Forman and Daniel H. Wiznia in INQUIRY: The Journal of Health Care Organization, Provision, and Financing